Nutrition Therapy by Nutrition Support Team: A Comparison of Multi-Chamber Bag and Customized Parenteral Nutrition in Hospitalized Patients
Abstract
1. Introduction
2. Materials and Methods
2.1. Data Source
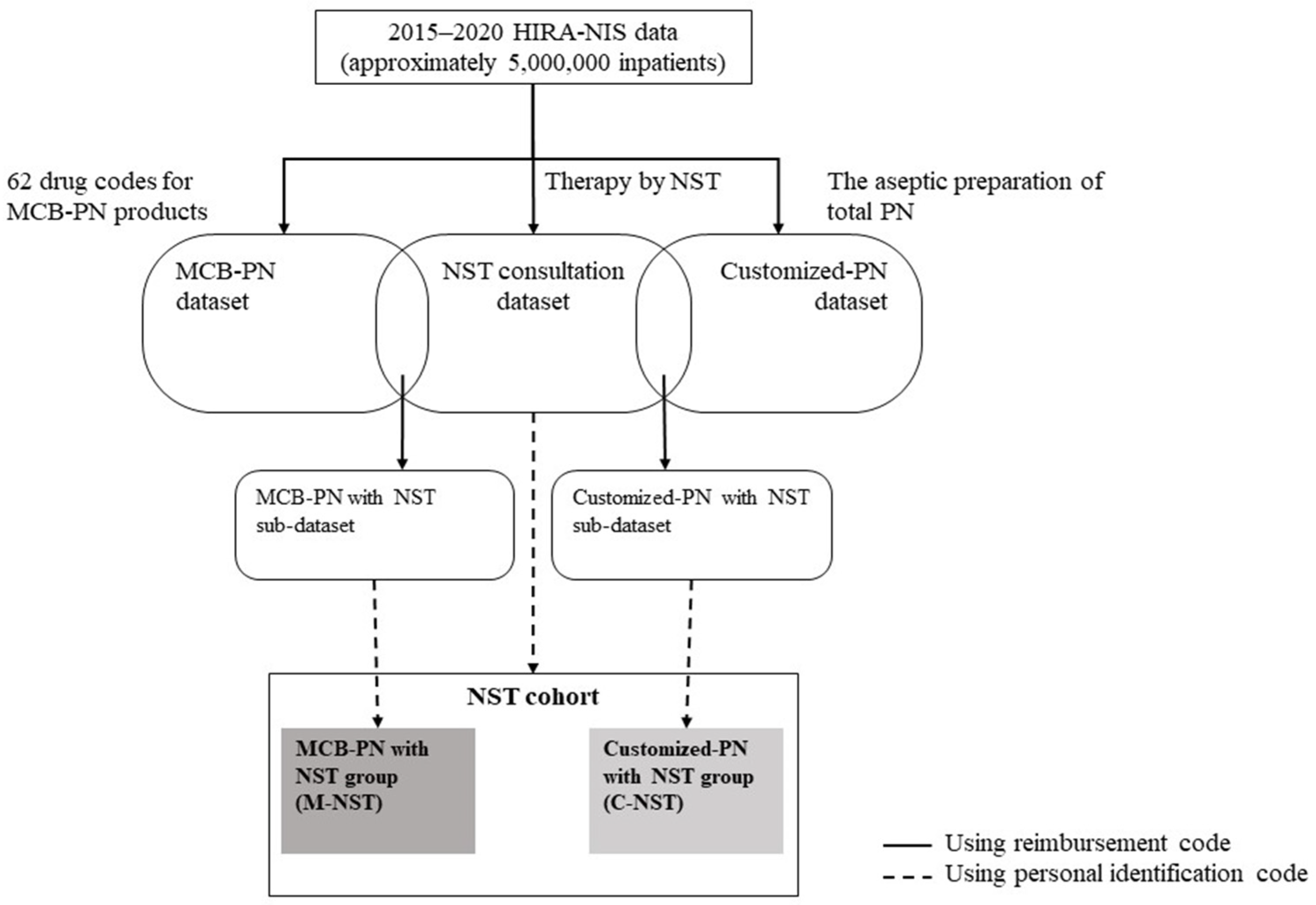
2.2. Dataset and Cohort Construction
2.3. Study Variables and Analysis
3. Results
3.1. NST Consultation Dataset and NST Cohort
3.2. MCB-PN Dataset and M-NST
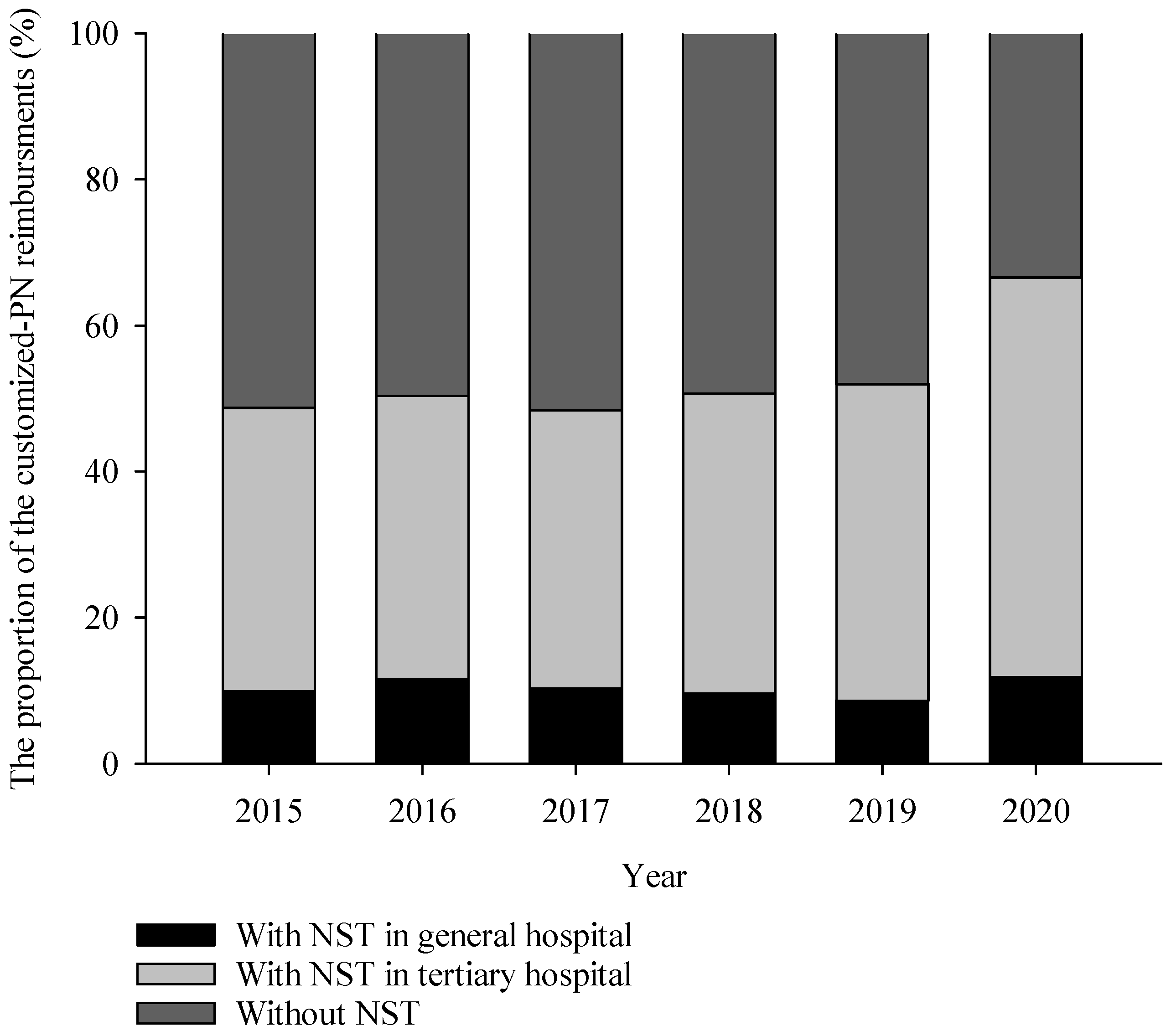
3.3. Customized-PN Dataset and C-NST
3.4. Subgroup Comparison: M-NST vs. C-NST
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Lin, A.; Micic, D. Nutrition Considerations in Inflammatory Bowel Disease. Nutr. Clin. Pract. 2021, 36, 298–311. [Google Scholar] [CrossRef] [PubMed]
- D’Almeida, C.A.; Peres, W.A.F.; de Pinho, N.B.; Martucci, R.B.; Rodrigues, V.D.; Ramalho, A. Prevalence of Malnutrition in Older Hospitalized Cancer Patients: A Multicenter and Multiregional Study. J. Nutr. Health Aging 2020, 24, 166–171. [Google Scholar] [CrossRef] [PubMed]
- Ghimire, S.; Baral, B.K.; Pokhrel, B.R.; Pokhrel, A.; Acharya, A.; Amatya, D.; Amatya, P.; Mishra, S.R. Depression, malnutrition, and health-related quality of life among Nepali older patients. BMC Geriatr. 2018, 18, 191. [Google Scholar] [CrossRef]
- Dempsey, D.; Mullen, J.; Buzby, G.P. The link between nutritional status and clinical outcome: Can nutritional intervention modify it? Am. J. Clin. Nutr. 1988, 47, 352–356. [Google Scholar] [CrossRef] [PubMed]
- Alberda, C.; Gramlich, L.; Jones, N.; Jeejeebhoy, K.; Day, A.G.; Dhaliwal, R.; Heyland, D.K. The relationship between nutritional intake and clinical outcomes in critically ill patients: Results of an international multicenter observational study. J. Intensive Care Med. 2009, 35, 1728–1737. [Google Scholar] [CrossRef] [PubMed]
- Agarwal, E.; Ferguson, M.; Banks, M.; Batterham, M.; Bauer, J.; Capra, S.; Isenring, E. Malnutrition and poor food intake are associated with prolonged hospital stay, frequent readmissions, and greater in-hospital mortality: Results from the Nutrition Care Day Survey 2010. Clin. Nutr. 2013, 32, 737–745. [Google Scholar] [CrossRef]
- Norman, K.; Pichard, C.; Lochs, H.; Pirlich, M. Prognostic impact of disease-related malnutrition. Clin. Nutr. 2008, 27, 5–15. [Google Scholar] [CrossRef]
- Braun, K.; Utech, A.; Velez, M.E.; Walker, R. Parenteral Nutrition Electrolyte Abnormalities and Associated Factors Before and After Nutrition Support Team Initiation. J. Parenter. Enter. Nutr. 2018, 42, 387–392. [Google Scholar] [CrossRef]
- Reber, E.; Strahm, R.; Bally, L.; Schuetz, P.; Stanga, Z. Efficacy and efficiency of nutritional support teams. J. Clin. Med. 2019, 8, 1281. [Google Scholar] [CrossRef]
- Gonzalez-Granda, A.; Schollenberger, A.; Thorsteinsson, R.; Haap, M.; Bischoff, S.C. Impact of an interdisciplinary nutrition support team (NST) on the clinical outcome of critically ill patients. A pre/post NST intervention study. Clin. Nutr. ESPEN 2021, 45, 486–491. [Google Scholar] [CrossRef]
- Traeger, S.M.; Williams, G.B.; Milliren, G.; Young, D.S.; Fisher, M.; Haug, M.T., III. Total Parenteral Nutrition by a Nutrition Support Team: Improved Quality of Care. J. Parenter. Enter. Nutr. 1986, 10, 408–412. [Google Scholar] [CrossRef] [PubMed]
- Vlug, L.E.; Nagelkerke, S.C.J.; Jonkers-Schuitema, C.F.; Rings, E.H.H.M.; Tabbers, M.M. The Role of a Nutrition Support Team in the Management of Intestinal Failure Patients. Nutrients 2020, 12, 172. [Google Scholar] [CrossRef] [PubMed]
- Seol, E.M.; Suh, Y.S.; Ju, D.L.; Bae, H.J.; Kim, E.; Lee, H.J. Nutrition Support Team Reconsultation During Nutrition Therapy in Korea. J. Parenter. Enter. Nutr. 2021, 45, 357–365. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.; Ock, M.; Lee, S.; Kim, J.T. Nutrition support team service in hospitalized patients in Korea. Clin. Nutr. 2018, 37, S132. [Google Scholar] [CrossRef]
- Oh, E.; Shim, H.; Yon, H.J.; Moon, J.S.; Kang, D.R.; Jang, J.Y.; Care, C. Effectiveness of a multidisciplinary team for nutrition support in a trauma intensive care unit. Acute Crit. Care 2020, 35, 142–148. [Google Scholar] [CrossRef]
- Park, H.J.; Oh, S.-H.; Kim, J.T.; Bae, H.J.; Nam, J.H.; Sung, Y.W.; Kim, S.H.; Jung, M.J.; Chung, J.E. Report on the Current Trend of Nutrition Support Team Consultation Fee and Fee for Aseptic Preparation of Parenteral Nutrition in Korea: 2014~2020. J. Korean Soc. Health-Syst. Pharm. 2022, 39, 69–80. [Google Scholar] [CrossRef]
- Christensen, M.L.; Ayers, P.; Boullata, J.I.; Guenter, P.; Gura, K.M.; Holcombe, B.; Seres, D.S.; Sacks, G.S.; ASPEN PN Safety Committee. Lipid Injectable Emulsion Survey With Gap Analysis. Nutr. Clin. Pract. 2017, 32, 694–702. [Google Scholar] [CrossRef]
- Stidham, M.A.; Douglas, J.W. Nutrition Support Team Oversight and Appropriateness of Parenteral Nutrition in Hospitalized Adults: A Systematic Review. J. Parenter. Enter. Nutr. 2020, 44, 1447–1460. [Google Scholar] [CrossRef]
- Berger, M.M.; Pichard, C.; Bao, J. When is parenteral nutrition indicated? J. Intensive Med. 2022, 2, 22–28. [Google Scholar] [CrossRef]
- Braga, M.; Ljungqvist, O.; Soeters, P.; Fearon, K.; Weimann, A.; Bozzetti, F. ESPEN Guidelines on Parenteral Nutrition: Surgery. Clin. Nutr. 2009, 28, 378–386. [Google Scholar] [CrossRef]
- Prathik, B.H.; Aradhya, A.S.; Sahoo, T.; Saini, S.S. Neonatal Total Parenteral Nutrition: Clinical Implications From Recent NICE Guidelines. Indian Pediatr. 2021, 58, 67–70. [Google Scholar] [CrossRef] [PubMed]
- Worthington, P.; Balint, J.; Bechtold, M.; Bingham, A.; Chan, L.-N.; Durfee, S.; Jevenn, A.K.; Malone, A.; Mascarenhas, M.; Robinson, D.T.; et al. When Is Parenteral Nutrition Appropriate? J. Parenter. Enter. Nutr. 2017, 41, 324–377. [Google Scholar] [CrossRef] [PubMed]
- Jeejeebhoy, K.N. Enteral nutrition versus parenteral nutrition—The risks and benefits. Nat. Clin. Pract. Gastroenterol. Hepatol. 2007, 4, 260–265. [Google Scholar] [CrossRef] [PubMed]
- Bischoff, S.C.; Kester, L.; Meier, R.; Radziwill, R.; Schwab, D.; Thul, P.; Working group for developing the guidelines for parenteral nutrition of The German Association for Nutrition Medicine. Organisation, regulations, preparation and logistics of parenteral nutrition in hospitals and homes; the role of the nutrition support team–Guidelines on Parenteral Nutrition, Chapter 8. Ger. Med. Sci. 2009, 7. [Google Scholar] [CrossRef]
- Mistiaen, P.; Van den Heede, K. Nutrition Support Teams: A Systematic Review. J. Parenter. Enter. Nutr. 2020, 44, 1004–1020. [Google Scholar] [CrossRef]
- Eriksen, M.K.; Crooks, B.; Baunwall, S.M.D.; Rud, C.L.; Lal, S.; Hvas, C.L. Systematic review with meta-analysis: Effects of implementing a nutrition support team for in-hospital parenteral nutrition. Aliment. Pharmacol. Ther. 2021, 54, 560–570. [Google Scholar] [CrossRef]
- Lee, J.S.; Kim, S.; Sung, S.-Y.; Kim, Y.H.; Lee, H.W.; Hong, J.H.; Ko, Y.H. Treatment Outcomes of 9994 Patients with Extensive-Disease Small-Cell Lung Cancer from a Retrospective Nationwide Population-Based Cohort in the Korean HIRA Database. Front. Oncol. 2021, 11, 546672. [Google Scholar] [CrossRef]
- Kim, S.; Kim, M.S.; You, S.H.; Jung, S.Y. Conducting and Reporting a Clinical Research Using Korean Healthcare Claims Database. Korean J. Fam. Med. 2023, 41, 146–152. [Google Scholar] [CrossRef]
- Chazard, E.; Focheur, G.; Beuscart, J.-B.; Preda, C. How to Compare the Length of Stay of Two Samples of Inpatients? A Simulation Study to Compare Type I and Type II Errors of 12 Statistical Tests. Value Health 2017, 20, 992–998. [Google Scholar] [CrossRef]
- Plauth, M.; Bernal, W.; Dasarathy, S.; Merli, M.; Plank, L.D.; Schütz, T.; Bischoff, S.C. ESPEN guideline on clinical nutrition in liver disease. Clin. Nutr. 2019, 38, 485–521. [Google Scholar] [CrossRef]
- Volkert, D.; Beck, A.M.; Cederholm, T.; Cruz-Jentoft, A.; Goisser, S.; Hooper, L.; Kiesswetter, E.; Maggio, M.; Raynaud-Simon, A.; Sieber, C.C.; et al. ESPEN guideline on clinical nutrition and hydration in geriatrics. Clin. Nutr. 2019, 38, 10–47. [Google Scholar] [CrossRef] [PubMed]
- Moore, F.A.; Feliciano, D.V.; Andrassy, R.J.; McArdle, A.H.; Booth, F.V.; Morgenstein-Wagner, T.B.; Kellum, J.M., Jr.; Welling, R.E.; Moore, E.E. Early enteral feeding, compared with parenteral, reduces postoperative septic complications. The results of a meta-analysis. Ann. Surg. 1992, 216, 172–183. [Google Scholar] [CrossRef] [PubMed]
- Gramlich, L.; Kichian, K.; Pinilla, J.; Rodych, N.J.; Dhaliwal, R.; Heyland, D.K. Does enteral nutrition compared to parenteral nutrition result in better outcomes in critically ill adult patients? A systematic review of the literature. Nutrition 2004, 20, 843–848. [Google Scholar] [CrossRef] [PubMed]
- Dissanaike, S.; Shelton, M.; Warner, K.; O’Keefe, G.E. The risk for bloodstream infections is associated with increased parenteral caloric intake in patients receiving parenteral nutrition. Crit. Care 2007, 11, R114. [Google Scholar] [CrossRef]
- Elke, G.; van Zanten, A.R.H.; Lemieux, M.; McCall, M.; Jeejeebhoy, K.N.; Kott, M.; Jiang, X.; Day, A.G.; Heyland, D.K. Enteral versus parenteral nutrition in critically ill patients: An updated systematic review and meta-analysis of randomized controlled trials. Crit. Care 2016, 20, 117. [Google Scholar] [CrossRef]
- Reignier, J.; Boisramé-Helms, J.; Brisard, L.; Lascarrou, J.-B.; Ait Hssain, A.; Anguel, N.; Argaud, L.; Asehnoune, K.; Asfar, P.; Bellec, F.; et al. Enteral versus parenteral early nutrition in ventilated adults with shock: A randomised, controlled, multicentre, open-label, parallel-group study (NUTRIREA-2). Lancet 2018, 391, 133–143. [Google Scholar] [CrossRef]
- Goh, R.J.L.; Li, H.; Cheah, M.C.C.; Salazar, E. The use of standardized commercially available parenteral nutrition as a bridge to customized compounded bag in the acute hospital setting is safe and feasible. Clin. Nutr. ESPEN 2022, 47, 321–324. [Google Scholar] [CrossRef]
- Banko, D.; Rosenthal, N.; Chung, J.; Lomax, C.; Washesky, P.F. Comparing the risk of bloodstream infections by type of parenteral nutrition preparation method: A large retrospective, observational study. Clin. Nutr. ESPEN 2019, 30, 100–106. [Google Scholar] [CrossRef]
- Hall, J.W. Safety, Cost, and Clinical Considerations for the Use of Premixed Parenteral Nutrition. Nutr. Clin. Pract. 2015, 30, 325–330. [Google Scholar] [CrossRef]
- Turpin, R.S.; Canada, T.; Rosenthal, V.D.; Nitzki-George, D.; Liu, F.X.; Mercaldi, C.J.; Pontes-Arruda, A. Bloodstream Infections Associated With Parenteral Nutrition Preparation Methods in the United States. J. Parenter. Enter. Nutr. 2012, 36, 169–176. [Google Scholar] [CrossRef]
- Mundi, M.S.; Klek, S.; Martindale, R.G. Use of Lipids in Adult Patients Requiring Parenteral Nutrition in the Home Setting. J. Parenter. Enter. Nutr. 2020, 44, S39–S44. [Google Scholar] [CrossRef]
- Mundi, M.S.; Pattinson, A.; McMahon, M.T.; Davidson, J.; Hurt, R.T. Prevalence of Home Parenteral and Enteral Nutrition in the United States. Nutr. Clin. Pract. 2017, 32, 799–805. [Google Scholar] [CrossRef]
- Choe, J.H.; Baek, J.H.; Jo, Y.H.; Cho, Y.S. Infection Control in Parenteral Nutrition Preparation and Compounding. J. Clin. Nutr. 2018, 10, 31–37. [Google Scholar] [CrossRef]
- Maisonneuve, N.; Raguso, C.A.; Paoloni-Giacobino, A.; Mühlebach, S.; Corriol, O.; Saubion, J.L.; Hecq, J.D.; Bailly, A.; Berger, M.; Pichard, C. Parenteral nutrition practices in hospital pharmacies in Switzerland, France, and Belgium. Nutrition 2004, 20, 528–535. [Google Scholar] [CrossRef] [PubMed]
- Shafiekhani, M.; Nikoupour, H.; Mirjalili, M. The experience and outcomes of multidisciplinary clinical pharmacist-led parenteral nutrition service for individuals with intestinal failure in a center without home parenteral nutrition. Eur. J. Clin. Nutr. 2022, 76, 841–847. [Google Scholar] [CrossRef] [PubMed]
- Stettler, N.; Sentongo, T.A.; Carroll, M.; Schears, G.J.; Mascarenhas, M.R. Impact of Customized Parenteral Nutrition in a Pediatric Hospital. Nutr. Clin. Pract. 2001, 16, 345–348. [Google Scholar] [CrossRef]
- Smolkin, T.; Diab, G.; Shohat, I.; Jubran, H.; Blazer, S.; Rozen, G.S.; Makhoul, I.R. Standardized versus individualized parenteral nutrition in very low birth weight infants: A comparative study. Neonatology 2010, 98, 170–178. [Google Scholar] [CrossRef]
- Boscarino, G.; Conti, M.G.; Gasparini, C.; Onestà, E.; Faccioli, F.; Dito, L.; Regoli, D.; Spalice, A.; Parisi, P.; Terrin, G. Neonatal Hyperglycemia Related to Parenteral Nutrition Affects Long-Term Neurodevelopment in Preterm Newborn: A Prospective Cohort Study. Nutrients 2021, 13, 1930. [Google Scholar] [CrossRef]
- Terrin, G.; Boscarino, G.; Gasparini, C.; Di Chiara, M.; Faccioli, F.; Onestà, E.; Parisi, P.; Spalice, A.; De Nardo, M.C.; Dito, L.; et al. Energy-enhanced parenteral nutrition and neurodevelopment of preterm newborns: A cohort study. Nutrition 2021, 89, 111219. [Google Scholar] [CrossRef]
- Vos, T.; Lim, S.S.; Abbafati, C.; Abbas, K.M.; Abbasi, M.; Abbasifard, M.; Abbasi-Kangevari, M.; Abbastabar, H.; Abd-Allah, F.; Abdelalim, A.; et al. Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: A systematic analysis for the Global Burden of Disease Study 2019. Lancet 2020, 396, 1204–1222. [Google Scholar] [CrossRef]
- Ostermann, S.; Morel, P.; Chalé, J.-J.; Bucher, P.; Konrad, B.; Meier, R.P.H.; Ris, F.; Schiffer, E.R.C. Randomized Controlled Trial of Enhanced Recovery Program Dedicated to Elderly Patients After Colorectal Surgery. Dis. Colon Rectum 2019, 62, 1105–1116. [Google Scholar] [CrossRef] [PubMed]
- Guenter, P.; Blackmer, A.; Malone, A.; Mirtallo, J.M.; Phillips, W.; Tyler, R.; Barrocas, A.; Resnick, H.E.; Anthony, P.; Abdelhadi, R. Update on use of enteral and parenteral nutrition in hospitalized patients with a diagnosis of malnutrition in the United States. Nutr. Clin. Pract. 2022, 37, 94–101. [Google Scholar] [CrossRef] [PubMed]
- Sabbouh, T.; Torbey, M.T. Malnutrition in Stroke Patients: Risk Factors, Assessment, and Management. Neurocritical Care 2018, 29, 374–384. [Google Scholar] [CrossRef]
- Chen, B.; Liu, W.; Chen, Y.; She, Q.; Li, M.; Zhao, H.; Zhao, W.; Peng, Z.; Wu, J. Effect of Poor Nutritional Status and Comorbidities on the Occurrence and Outcome of Pneumonia in Elderly Adults. Front. Med. 2021, 8, 719530. [Google Scholar] [CrossRef]
- Yeo, H.J.; Byun, K.S.; Han, J.; Kim, J.H.; Lee, S.E.; Yoon, S.H.; Jeon, D.; Kim, Y.S.; Cho, W.H. Prognostic significance of malnutrition for long-term mortality in community-acquired pneumonia: A propensity score matched analysis. Korean J. Intern. Med. 2019, 34, 841–849. [Google Scholar] [CrossRef]
- Gomes, F.; Emery, P.W.; Weekes, C.E. Risk of Malnutrition Is an Independent Predictor of Mortality, Length of Hospital Stay, and Hospitalization Costs in Stroke Patients. J. Stroke Cerebrovasc. Dis. 2016, 25, 799–806. [Google Scholar] [CrossRef] [PubMed]
- Cogle, S.V.; Martindale, R.G.; Ramos, M.; Roberti, G.J.; Roberts, P.R.; Taylor, K.; Sacks, G.S. Multicenter Prospective Evaluation of Parenteral Nutrition Preparation Time and Resource Utilization: 3-Chamber Bags Compared with Hospital Pharmacy–Compounded Bags. J. Parenter. Enter. Nutr. 2021, 45, 1552–1558. [Google Scholar] [CrossRef]
- Berlana, D.; Almendral, M.A.; Abad, M.R.; Fernández, A.; Torralba, A.; Cervera-Peris, M.; Piñeiro, G.; Romero-Jiménez, R.; Vázquez, A.; Ramírez, E.; et al. Cost, Time, and Error Assessment During Preparation of Parenteral Nutrition: Multichamber Bags versus Hospital-Compounded Bags. J. Parenter. Enter. Nutr. 2019, 43, 557–565. [Google Scholar] [CrossRef]
- Tucker, A.; Ybarra, J.; Bingham, A.; Blackmer, A.; Curtis, C.; Mattox, T.; Miller, C.; Ward, C.; Williams, N.T.; Standards of Practice for Nutrition Support Pharmacists Task Force; et al. American Society for Parenteral and Enteral Nutrition (A.S.P.E.N.) Standards of Practice for Nutrition Support Pharmacists. Nutr. Clin. Pract. 2015, 30, 139–146. [Google Scholar] [CrossRef]
- Katoue, M.G. Role of pharmacists in providing parenteral nutrition support: Current insights and future directions. Integr. Pharm. Res. Pract. 2018, 7, 125–140. [Google Scholar] [CrossRef]

| NST Cohort n (%) | Comparative Analysis of Subgroups | ||||
|---|---|---|---|---|---|
| M-NST n (%) | C-NST n (%) | p-Value | |||
| No. of patients | 70,665 | 50,010 | 7591 | - | |
| No. of patients per 1000 inpatients | 14.13 | 10.00 | 1.52 | - | |
| Gender | Male | 40,190 (56.9) | 28,796 (57.6) | 4383 (57.7) | p < 0.001 |
| Female | 30,475 (43.1) | 21,214 (42.4) | 3208 (42.3) | ||
| Age | <5 | 4995 (7.1) | 262 (0.5) | 3208 (42.3) | p < 0.001 |
| 5–9 | 390 (0.6) | 158 (0.3) | 67 (0.9) | ||
| 10–14 | 367 (0.5) | 205 (0.4) | 47 (0.6) | ||
| 15–19 | 590 (0.8) | 419 (0.8) | 76 (1.0) | ||
| 20–24 | 636 (0.9) | 485 (1.0) | 48 (0.6) | ||
| 25–29 | 635 (0.9) | 516 (1.0) | 34 (0.4) | ||
| 30–34 | 965 (1.4) | 746 (1.5) | 60 (0.8) | ||
| 35–39 | 1235 (1.7) | 955 (1.9) | 108 (1.4) | ||
| 40–44 | 1830 (2.6) | 1397 (2.8) | 150 (2.0) | ||
| 45–49 | 3045 (4.3) | 2299 (4.6) | 222 (2.9) | ||
| 50–54 | 4228 (6.0) | 3270 (6.5) | 312 (4.1) | ||
| 55–59 | 6048 (8.6) | 4718 (9.4) | 455 (6.0) | ||
| 60–64 | 6636 (9.4) | 5167 (10.3) | 547 (7.2) | ||
| 65–69 | 6945 (9.8) | 5337 (10.7) | 560 (7.4) | ||
| 70–74 | 8323 (11.8) | 6348 (12.7) | 572 (7.5) | ||
| ≥75 | 23,797 (33.7) | 17,728 (35.4) | 1125 (14.8) | ||
| No. of reimbursements | 91,384 | 60,916 | 9343 | - | |
| No. of reimbursements per 1000 inpatients | 18.28 | 12.18 | 1.87 | - | |
| Medical department | Internal medicine | 44,978 (49.2) | 33,395 (54.8) | 2807 (30.0) | p < 0.001 |
| Gastroenterology | 11,659 (12.8) | 9205 (15.1) | 812 (8.7) | ||
| Cardiology | 3364 (3.7) | 1927 (3.2) | 165 (1.8) | ||
| Pulmonology | 11,888 (13.0) | 8627 (14.2) | 544 (5.8) | ||
| Nephrology | 4175 (4.6) | 2765 (4.5) | 170 (1.8) | ||
| Hemato-oncology | 9254 (10.1) | 7954 (13.1) | 868 (9.3) | ||
| Infection | 2439 (2.7) | 1619 (2.7) | 89 (1.0) | ||
| Other IMs | 2199 (2.4) | 1298 (2.1) | 159 (1.7) | ||
| Neuropsychiatry | 4851 (5.3) | 2462 (4.0) | 124 (1.3) | ||
| General surgery | 12,628 (13.8) | 10,699 (17.6) | 1304 (14.0) | ||
| Neurosurgery | 8998 (9.8) | 6114 (10.0) | 233 (2.5) | ||
| Chest surgery | 2455 (2.7) | 1692 (2.8) | 360 (3.9) | ||
| Pediatrics | 8076 (8.8) | 991 (1.6) | 3997 (42.8) | ||
| Others | 9398 (10.3) | 5563 (9.1) | 518 (5.5) | ||
| Admission route | Outpatients | 37,074 (40.6) | 23,477 (38.5) | 5086 (54.4) | p < 0.001 |
| Emergency | 50,847 (55.6) | 34,871 (57.2) | 3980 (42.6) | ||
| Transfer from other institutions | 3463 (3.8) | 2568 (4.2) | 277 (3.0) | ||
| Clinical outcomes | Continuation | 26,863 (29.4) | 17,163 (28.2) | 3553 (38.0) | p < 0.001 |
| Death | 9429 (10.3) | 7683 (12.6) | 891 (9.5) | ||
| Discharge | 49,059 (53.7) | 32,411 (53.2) | 4507 (48.2) | ||
| Others | 6033 (6.6) | 3659 (6.0) | 392 (4.2) | ||
| Days of hospitalization (mean ± SD) | 20.8 ± 15.0 | 21.2 ± 15.0 | 26.2 ± 17.3 | p < 0.001 | |
| Days of care (mean ± SD) | 28.7 ± 18.7 | 28.5 ± 18.0 | 32.4 ± 20.6 | p < 0.001 | |
| ICD-10 Classification | NST Cohort n (%) | M-NST * n (%) | C-NST * n (%) | |
|---|---|---|---|---|
| A00–B99 | Certain infectious and parasitic disease | 1740 (2.5) | 1287 (2.6) | 90 (1.2) |
| C00–D48 | Neoplasms | 19,149 (27.1) | 16,683 (33.4) | 2142 (28.2) |
| D50–D89 | Diseases of the blood and blood-forming organs and certain disorders involving the immune mechanism | 264 (0.4) | 142 (0.3) | 14 (0.2) |
| E00–E90 | Endocrine, nutritional, and metabolic diseases | 815 (1.2) | 426 (0.9) | 44 (0.6) |
| F00–F99 | Mental and behavioral disorders | 284 (0.4) | 178 (0.4) | 11 (0.1) |
| G00–G99 | Diseases of the nervous system | 1815 (2.6) | 960 (1.9) | 108 (1.4) |
| H00–H95 | Diseases of the eye and adnexa and diseases of the ear and mastoid process | 71 (0.1) | 34 (0.1) | 3 (0.0) |
| I00–I99 | Diseases of the circulatory system | 11,303 (16.0) | 7093 (14.2) | 433 (5.7) |
| J00–J99 | Diseases of the respiratory system | 7667 (10.8) | 5604 (11.2) | 381 (5.0) |
| K00–K93 | Diseases of the digestive system | 8174 (11.6) | 6634 (13.3) | 612 (8.1) |
| L00–L99 | Diseases of the skin and subcutaneous tissue | 268 (0.4) | 145 (0.3) | 18 (0.2) |
| M00–M99 | Diseases of the musculoskeletal system and connective tissue | 958 (1.4) | 583 (1.2) | 47 (0.6) |
| N00–N99 | Diseases of the genitourinary system | 3124 (4.4) | 2070 (4.1) | 137 (1.8) |
| O00–O99 | Pregnancy, childbirth, and the puerperium | 44 (0.1) | 26 (0.1) | 2 (0.0) |
| P00–P96 | Certain conditions originating in the perinatal period | 3144 (4.4) | 65 (0.1) | 2260 (29.8) |
| Q00–Q99 | Congenital malformations, deformations, and chromosomal abnormalities | 587 (0.8) | 65 (0.1) | 337 (4.4) |
| R00–R99 | Symptoms, signs, and abnormal clinical and laboratory findings, not elsewhere classified | 1210 (1.7) | 759 (1.5) | 73 (1.0) |
| S00–T98 | Injury, poisoning, and certain other consequences of external causes | 4416 (6.2) | 3089 (6.2) | 215 (2.8) |
| U00–U85 | Codes for special purposes | 79 (0.1) | 63 (0.1) | 8 (0.1) |
| V01–Y98 | External causes of morbidity and mortality | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Z00–Z99 | Factors influencing health status and contact with health services | 1365 (1.9) | 995 (2.0) | 111 (1.5) |
| Not specified # | 4188 (5.9) | 3109 (6.2) | 545 (7.2) | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cheon, S.; Oh, S.-H.; Kim, J.-T.; Choi, H.-G.; Park, H.; Chung, J.-E. Nutrition Therapy by Nutrition Support Team: A Comparison of Multi-Chamber Bag and Customized Parenteral Nutrition in Hospitalized Patients. Nutrients 2023, 15, 2531. https://doi.org/10.3390/nu15112531
Cheon S, Oh S-H, Kim J-T, Choi H-G, Park H, Chung J-E. Nutrition Therapy by Nutrition Support Team: A Comparison of Multi-Chamber Bag and Customized Parenteral Nutrition in Hospitalized Patients. Nutrients. 2023; 15(11):2531. https://doi.org/10.3390/nu15112531
Chicago/Turabian StyleCheon, Seunghyun, Sang-Hyeon Oh, Jung-Tae Kim, Han-Gon Choi, Hyojung Park, and Jee-Eun Chung. 2023. "Nutrition Therapy by Nutrition Support Team: A Comparison of Multi-Chamber Bag and Customized Parenteral Nutrition in Hospitalized Patients" Nutrients 15, no. 11: 2531. https://doi.org/10.3390/nu15112531
APA StyleCheon, S., Oh, S.-H., Kim, J.-T., Choi, H.-G., Park, H., & Chung, J.-E. (2023). Nutrition Therapy by Nutrition Support Team: A Comparison of Multi-Chamber Bag and Customized Parenteral Nutrition in Hospitalized Patients. Nutrients, 15(11), 2531. https://doi.org/10.3390/nu15112531





