Effects of Dietary Diversity on Growth Outcomes of Children Aged 6 to 23 Months in India: Evidence from National Family and Health Survey
Abstract
1. Introduction
2. Methods
2.1. Study Design and Sample
2.2. Study Participants
2.3. Growth Outcomes Calculation
2.4. Dietary Diversity Calculation
2.5. Other Covariates
2.6. Statistical Analyses
3. Results
3.1. Characteristics of the Children Aged 6–23 Months
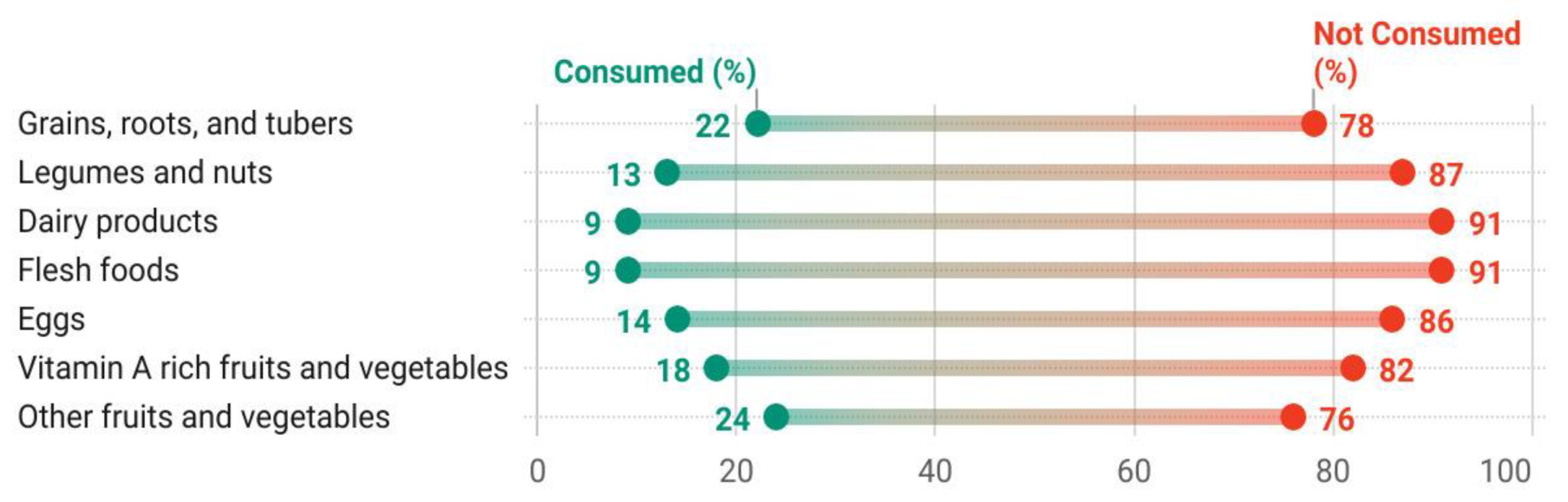
3.2. Dietary Diversity of Children Aged 6 to 23 Months in India
3.3. Association between Dietary Diversity and Undernutrition
3.4. Association between Dietary Diversity and Severe Undernutrition
3.5. Association between Specific Food Groups and Undernutrition
3.6. Association between Specific Food Groups and Severe Undernutrition
4. Discussion
Limitations of the Study
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- WHO. Malnutrition. 2021. Available online: https://www.who.int/news-room/fact-sheets/detail/malnutrition (accessed on 26 October 2022).
- Quamme, S.H.; Iversen, P.O. Prevalence of child stunting in Sub-Saharan Africa and its risk factors. Clin. Nutr. Open Sci. 2022, 42, 49–61. [Google Scholar] [CrossRef]
- Lu, C.; Black, M.M.; Richter, L.M. Risk of poor development in young children in low-income and middle-income countries: An estimation and analysis at the global, regional, and country level. Lancet Glob. Heal. 2016, 4, e916–e922. [Google Scholar] [CrossRef] [PubMed]
- Micha, R.; Mannar, V.; Afshin, A.; Allemandi, L.; Baker, P.; Battersby, J.; Bhutta, Z.; Chen, K.; Corvalan, C.; Di Cesare, M.; et al. 2020 Global Nutrition Report: Action on Equity to End Malnutrition; Development Initiatives: Bristol, UK, 2020. [Google Scholar]
- UNICEF. The State of the World’s Children 2008 Child Survival; UNICEF: New York, NY, USA, 2007; Available online: https://www.unicef.org/reports/state-worlds-children-2008 (accessed on 7 November 2022).
- UNICEF. From the First Hour of Life: A New Report on Infant and Young Child Feeding—UNICEF DATA; UNICEF: New York, NY, USA, 2016. [Google Scholar]
- IIPS; ICF. National Family Health Survey (NFHS-5) 2019–2021; IIPS: Mumbai, India, 2021. [Google Scholar]
- Khan, N.; Mozumdar, A.; Kaur, S. 2019, undefined Dietary adequacy among young children in India: Improvement or stagnation? An investigation from the National Family Health Survey. Food Nutr. Bull. 2019, 40, 471–487. [Google Scholar] [CrossRef] [PubMed]
- International Institute for Population Sciences (IIPS). ICF National Family Health Survey—4: 2015–2016. Available online: http://rchiips.org/nfhs/ (accessed on 8 September 2022).
- World Health Organization. Guidance on Ending the Inappropriate Promotion of Foods for Infants and Young Children: Implementation Manual; World Health Organization: Geneva, Switzerland, 2017.
- IIPS; MoHFW. India—Summary Report—National Family Health Survey 1992–1993; IIPS: Mumbai, India, 1993. [Google Scholar]
- Petrikova, I. The role of complementary feeding in India’s enigma of high child malnutrition rates: Findings from a comprehensive national study. Res. Sq. 2020. [Google Scholar] [CrossRef]
- Russell, A.L.; Hentschel, E.; Fulcher, I.; Ravà, M.S.; Abdulkarim, G.; Abdalla, O.; Said, S.; Khamis, H.; Hedt-Gauthier, B.; Wilson, K. Caregiver parenting practices, dietary diversity knowledge, and association with early childhood development outcomes among children aged 18–29 months in Zanzibar, Tanzania: A cross-sectional survey. BMC Public Health 2022, 22, 762. [Google Scholar] [CrossRef] [PubMed]
- Borkotoky, K.; Unisa, S.; Gupta, A.K. State-level dietary diversity as a contextual determinant of nutritional status of children in India: A multilevel approach. J. Biosoc. Sci. 2017, 50, 26–52. [Google Scholar] [CrossRef]
- Khan, J.; Das, S.K. The burden of anthropometric failure and child mortality in India. Sci. Rep. 2020, 10, 20991. [Google Scholar] [CrossRef]
- Wagnew, F.; Dessie, G.; Takele, W.W.; Tadesse, A.; Islam, S.M.S.; Mulugeta, H.; Haile, D.; Negesse, A.; Abajobir, A.A. A meta-analysis of inpatient treatment outcomes of severe acute malnutrition and predictors of mortality among under-five children in Ethiopia. BMC Public Health 2019, 19, 1175. [Google Scholar] [CrossRef]
- Irshad, M.; Hayat, M.; Ahmad, A.; Khalil, B.; Hussain, M. Case fatality rate and etiological factors of malnutrition in children less than 5 years of age. JPMI J. Postgrad. Med. Inst. 2014, 28, 42–48. [Google Scholar]
- Dafursa, K.; Gebremedhin, S. Dietary diversity among children aged 6–23 months in Aleta Wondo District, Southern Ethiopia. J. Nutr. Metab. 2019, 2019, 2869424. [Google Scholar] [CrossRef]
- Abeshu, M.A.; Lelisa, A.; Geleta, B. Complementary Feeding: Review of Recommendations, Feeding Practices, and Adequacy of Homemade Complementary Food Preparations in Developing Countries–Lessons from Ethiopia. Front. Nutr. 2016, 3, 41. [Google Scholar] [CrossRef] [PubMed]
- WHO. Global Health Risks: Mortality and Burden of Disease Attributable to Selected Major Risks; World Health Organization: Geneva, Switzerland, 2009; ISBN 9789241563871.
- Masuke, R.; Msuya, S.E.; Mahande, J.M.; Diarz, E.J.; Stray-Pedersen, B.; Jahanpour, O.; Mgongo, M. Effect of inappropriate complementary feeding practices on the nutritional status of children aged 6–24 months in urban Moshi, Northern Tanzania: Cohort study. PLoS ONE 2021, 16, e0250562. [Google Scholar] [CrossRef] [PubMed]
- Aboagye, R.G.; Seidu, A.-A.; Ahinkorah, B.O.; Arthur-Holmes, F.; Cadri, A.; Kobina Dadzie, L.; Hagan, J.E.; Eyawo, O.; Yaya, S.; Fernandez, L. Dietary Diversity and Undernutrition in Children Aged 6–23 Months in Sub-Saharan Africa. Nutrients 2021, 13, 3431. [Google Scholar] [CrossRef]
- Kennedy, G.L.; Pedro, M.R.; Seghieri, C.; Nantel, G.; Brouwer, I. Dietary diversity score is a useful indicator of micronutrient intake in non-breast-feeding Filipino children. J. Nutr. 2007, 137, 472–477. [Google Scholar] [CrossRef] [PubMed]
- McDonald, C.M.; Olofin, I.; Flaxman, S.; Fawzi, W.W.; Spiegelman, D.; Caulfield, L.E.; Black, R.E.; Ezzati, M.; Danaei, G.; Study, N.M. The effect of multiple anthropometric deficits on child mortality: Meta-analysis of individual data in 10 prospective studies from developing countries. Am. J. Clin. Nutr. 2013, 97, 896–901. [Google Scholar] [CrossRef]
- Molla, W.; Adem, D.A.; Tilahun, R.; Shumye, S.; Kabthymer, R.H.; Kebede, D.; Mengistu, N.; Ayele, G.M.; Assefa, D.G. Dietary diversity and associated factors among children (6–23 months) in Gedeo zone, Ethiopia: Cross-sectional study. Ital. J. Pediatr. 2021, 47, 233. [Google Scholar] [CrossRef]
- Solomon, D.; Aderaw, Z.; Tegegne, T.K. Minimum dietary diversity and associated factors among children aged 6–23 months in Addis Ababa, Ethiopia. Int. J. Equity Health 2017, 16, 181. [Google Scholar] [CrossRef]
- WHO. Indicators for Assessing Infant and Young Child Feeding Practices: Part 1: Definitions: Conclusions of A Consensus Meeting Held 6–8 November 2007 in Washington DC, USA; World Health Organization: Geneva, Switzerland, 2008. [Google Scholar]
- WHO. Indicators for Assessing Infant and Young Child Feeding Practices Part 3: Country Profiles; World Health Organization: Geneva, Switzerland, 2010; pp. 1–59. Available online: https://apps.who.int/iris/bitstream/handle/10665/44368/9789241599757_eng.pdf (accessed on 8 September 2022).
- Worku, T.; Gonete, K.A.; Muhammad, E.A.; Atnafu, A. Sustainable under nutrition reduction program and dietary diversity among children’s aged 6–23 months, Northwest Ethiopia: Comparative cross-sectional study. Int. J. Equity Health 2020, 19, 14. [Google Scholar] [CrossRef]
- FAO; ECA; AUC. Africa—Regional Overview of Food Security and Nutrition 2021; FAO: Rome, Italy, 2021. [Google Scholar]
- Temesgen, H.; Negesse, A.; Woyraw, W.; Mekonnen, N. Dietary diversity feeding practice and its associated factors among children age 6–23 months in Ethiopia from 2011 up to 2018: A systematic review and meta-analysis 11 Medical and Health Sciences 1117 Public Health and Health Services. Ital. J. Pediatr. 2018, 44, 109. [Google Scholar] [CrossRef]
- Agrawal, S.; Kim, R.; Gausman, J.; Sharma, S.; Sankar, R.; Joe, W.; Subramanian, S.V. Socio-economic patterning of food consumption and dietary diversity among Indian children: Evidence from NFHS-4. Eur. J. Clin. Nutr. 2019, 73, 1361–1372. [Google Scholar] [CrossRef]
- Jain, A.; Wang, W.; James, K.S.; Sarwal, R.; Kim, R.; Subramanian, S.V. Small Area Variations in Dietary Diversity Among Children in India: A Multilevel Analysis of 6–23-Month-Old Children. Front. Nutr. 2021, 8, 791509. [Google Scholar] [CrossRef] [PubMed]
- Rai, R.; Kumar, S.; Kumar, C. Factors associated with minimum dietary diversity failure among Indian children. J. Nutr. Sci. 2022, 11, E4. [Google Scholar] [CrossRef] [PubMed]
- Ahmad, I.; Khalique, N.; Khalil1, S.; Maroof, M. Dietary diversity and stunting among infants and young children: A cross-sectional study in Aligarh. Indian J. Community Med. 2018, 43, 34. [Google Scholar] [CrossRef]
- IIPS; ICF. National Family Health Survey—4: 2015–2016; IIPS: Mumbai, India, 2017. [Google Scholar]
- WHO. WHO Child Growth Standards: Length/Height-for-Age, Weight-for-Age, Weight-for-Length, Weight-for-Height and Body Mass Index-for-Age: Methods and Development; World Health Organization: Geneva, Switzerland, 2006.
- Nie, P.; Rammohan, A.; Gwozdz, W.; Sousa-Poza, A. Changes in child nutrition in India: A decomposition approach. Int. J. Environ. Res. Public Health 2019, 16, 1815. [Google Scholar] [CrossRef] [PubMed]
- Rakotonirainy, N.H.; Razafindratovo, V.; Remonja, C.R.; Rasoloarijaona, R.; Piola, P.; Raharintsoa, C.; Randremanana, R.V. Dietary diversity of 6- to 59-month-old children in rural areas of Moramanga and Morondava districts, Madagascar. PLoS ONE 2018, 13, e0200235. [Google Scholar] [CrossRef] [PubMed]
- WHO. Indicators for Assessing Infant and Young Child Feeding Practices: Part 2: Measurement; World Health Organization: Geneva, Switzerland, 2010.
- Ghosh, S.; Varerkar, S.A. Undernutrition among tribal children in Palghar district, Maharashtra, India. PLoS ONE 2019, 14, e0212560. [Google Scholar] [CrossRef]
- George, C.M.; Coglianese, N.; Bauler, S.; Perin, J.; Kuhl, J.; Williams, C.; Kang, Y.; Thomas, E.D.; François, R.; Ng, A.; et al. Low dietary diversity is associated with linear growth faltering and subsequent adverse child developmental outcomes in rural Democratic Republic of the Congo (REDUCE program). Matern. Child Nutr. 2022, 18, e13340. [Google Scholar] [CrossRef]
- Khamis, A.G.; Mwanri, A.W.; Ntwenya, J.E.; Kreppel, K. The influence of dietary diversity on the nutritional status of children between 6 and 23 months of age in Tanzania. BMC Pediatr. 2019, 19, 518. [Google Scholar] [CrossRef]
- Bukania, Z.N.; Mwangi, M.; Karanja, R.M.; Mutisya, R.; Kombe, Y.; Kaduka, L.U.; Johns, T. Food insecurity and not dietary diversity is a predictor of nutrition status in children within semiarid agro-ecological zones in eastern Kenya. J. Nutr. Metab. 2014, 2014, 907153. [Google Scholar] [CrossRef] [PubMed]
- Marriott, B.P.; White, A.; Hadden, L.; Davies, J.C.; Wallingford, J.C. World Health Organization (WHO) infant and young child feeding indicators: Associations with growth measures in 14 low-income countries. Matern. Child Nutr. 2012, 8, 354–370. [Google Scholar] [CrossRef]
- Srivastava, S.; Kumar, S. Does socio-economic inequality exist in micro-nutrients supplementation among children aged 6–59 months in India? Evidence from National Family Health Survey 2005–06 and 2015–16. BMC Public Health 2021, 21, 545. [Google Scholar] [CrossRef] [PubMed]
- MoHFW; Government of India; UNICEF; Population Council. Comprehensive National Nutrition Survey: 2016–2018; MoHFW: New Delhi, India, 2019; Available online: https://knowledgecommons.popcouncil.org/cgi/viewcontent.cgi?article=2541&context=departments_sbsr-rh (accessed on 5 November 2022).
- Sari, M.; De Pee, S.; Bloem, M.W.; Sun, K.; Thorne-Lyman, A.L.; Akhter, R.M.-P.N.; Kraemer, K.; Semba, R.D. Higher household expenditure on animal-source and nongrain foods lowers the risk of stunting among children 0–59 months old in Indonesia: Implications of rising. J. Nutr. 2010, 140, 195S–200S. [Google Scholar] [CrossRef] [PubMed]
- Neumann, C.G.; Bwibo, N.O.; Murphy, S.P.; Sigman, M.; Whaley, S.; Allen, L.H.; Guthrie, D.; Weiss, R.E.; Demment, M.W. Animal source foods improve dietary quality, micronutrient status, growth and cognitive function in Kenyan school children: Background, study design and baseline. J. Nutr. 2003, 133, 3941S–3949S. [Google Scholar] [CrossRef]
- Mehranfar, S.; Jalilpiran, Y.; Surkan, P.J.; Azadbakht, L. Association between protein-rich dietary patterns and anthropometric measurements among children aged 6 years. Nutr. Diet. 2020, 77, 359–367. [Google Scholar] [CrossRef]
- Darapheak, C.; Takano, T.; Kizuki, M.; Nakamura, K.; Seino, K. Consumption of animal source foods and dietary diversity reduce stunting in children in Cambodia. Int. Arch. Med. 2013, 6, 1–11. [Google Scholar] [CrossRef]
- Bohrer, B.M. Nutrient density and nutritional value of meat products and non-meat foods high in protein. Trends Food Sci. Technol. 2017, 65, 103–112. [Google Scholar] [CrossRef]
- Pandey, S.; Kashima, S. Effects of dairy intake on anthropometric failure in children ages 6 to 23 mo consuming vegetarian diets and fulfilling minimum dietary diversity in India. Nutrition 2021, 91, 111446. [Google Scholar] [CrossRef]
- Gil, Á.; Ortega, R.M. Introduction and executive summary of the supplement, role of milk and dairy products in health and prevention of noncommunicable chronic diseases: A series of. Adv. Nutr. 2019, 10, S67–S73. [Google Scholar] [CrossRef]


| Characteristics | Mean (SD) and Frequency (%) | |
| Age of Children in Months | 14.4 (SD = 5.2 Months) | |
| Growth outcomes | ||
| Prevalence of undernutrition | ||
| Stunting (HAZ < −2 SD) | 35.9 | 24,157 |
| Wasting (WHZ < −2 SD) | 23.8 | 15,254 |
| Underweight (WAZ < −2 SD) | 32.8 | 21,325 |
| Prevalence of severe undernutrition | ||
| Severely stunting (HAZ < −3 SD) | 16.2 | 10,954 |
| Severely wasting (WHZ < −3 SD) | 8.5 | 5601 |
| Severely underweight (WAZ < −3 SD) | 10.4 | 6881 |
| Sex of Child | ||
| Male | 51.9 | 34,915 |
| Female | 48.1 | 32,363 |
| Child’s birthplace | ||
| At Home | 17.6 | 13,908 |
| Institution/health facility | 82.2 | 53,199 |
| Other places | 0.2 | 171 |
| Size of the child at birth | ||
| Larger | 19.6 | 11,617 |
| Average | 67.5 | 46,557 |
| Smaller | 11.8 | 7940 |
| Not reported | 1.2 | 1164 |
| Currently breastfeeding | ||
| No | 15.2 | 9598 |
| Yes | 84.8 | 57,680 |
| Diarrhea in the last 2 weeks | ||
| Yes | 14.7 | 9666 |
| No | 85.3 | 57,562 |
| Not reported | 0.06 | 50 |
| Fever in last 2 weeks | ||
| Yes | 17.5 | 11,721 |
| No | 82.4 | 55,522 |
| Not reported | 0.04 | 35 |
| Dietary Diversity Score (DDS) | Growth Outcomes | ||||||||
| Stunting (HAZ < −2 SD) | Wasting (WHZ < −2 SD) | Underweight (WAZ < −2 SD) | |||||||
| Frequency (%) | OR (95% CI) | AOR a (95% CI) | Frequency (%) | OR (95% CI) | AOR a (95% CI) | Frequency (%) | OR (95% CI) | AOR a (95% CI) | |
| Score 0 | 12,460 (34.8) | ® | ® | 8764 (25.5) | ® | ® | 11,903 (34.2) | ® | ® |
| Score 1 | 4904 (38.2) | 1.2 *** (1.05–1.15) | 0.92 *** (0.88–0.96) | 2801 (22.6) | 0.83 *** (0.79–0.87) | 0.86 *** (0.82–0.91) | 4157 (33.4) | 0.92 *** (0.88–0.96) | 0.85 *** (0.81–0.89) |
| Score 2 | 2791 (38.4) | 1.09 *** (1.04–1.15) | 0.88 *** (0.84–0.93) | 1542 (22.3) | 0.79 *** (0.74–0.84) | 0.83 *** (0.78–0.89) | 2268 (32.6) | 0.86 *** (0.81–0.90) | 0.78 *** (0.74–0.83) |
| Score 3 | 1577 (35.6) | 1.02 (0.95–1.09) | 0.80 *** (0.75–0.86) | 896 (20.5) | 0.77 *** (0.71–0.83) | 0.83 *** (0.77–0.89) | 1236 (27.6) | 0.76 *** (0.71–0.82) | 0.70 *** (0.65–0.75) |
| Score 4 | 946 (37.2) | 1.06 (0.98–1.16) | 0.84 *** (0.77–0.91) | 487 (20.8) | 0.71 *** (0.64–0.78) | 0.75 *** (0.68–0.84) | 707 (29.5) | 0.74 *** (0.68–0.81) | 0.68 *** (0.62–0.74) |
| Score 5 | 613 (33.2) | 0.99 (0.89–1.09) | 0.76 *** (0.68–0.84) | 301 (20.4) | 0.63 *** (0.55–0.71) | 0.68 *** (0.60–0.78) | 427 (26.0) | 0.63 *** (0.57–0.71) | 0.57 *** (0.52–0.64) |
| Score 6 | 378 (34) | 0.93 (0.82–1.05) | 0.71 *** (0.63–0.81) | 185 (17.3) | 0.59 *** (0.51–0.70) | 0.66 *** (0.56–0.77) | 290 (29.4) | 0.68 *** (0.60–0.78) | 0.63 *** (0.55–0.72) |
| Score 7 | 447 (33.9) | 0.9 * (0.80–1.01) | 0.69 *** (0.62–0.79) | 252 (22.6) | 0.69 *** (0.6–0.76) | 0.76 *** (0.66–0.87) | 306 (23.6) | 0.57 *** (0.50–0.65) | 0.53 *** (0.46–0.60) |
| Minimum dietary diversity (MDD) | Frequency (%) | OR (95% CI) | AOR a (95% CI) | Frequency (%) | OR (95% CI) | AOR a (95% CI) | Frequency (%) | OR (95% CI) | AOR a (95% CI) |
| ≥4 food groups | 2384 (35.1) | ® | ® | 1225 (20.4) | ® | ® | 1730 (27.6) | ® | ® |
| <4 food groups | 21,732 (36) | 1.05 * (0.99–1.10) | 1.23 *** (1.17–1.30) | 14,003 (24.1) | 1.38 *** (1.29–1.47) | 1.29 *** (1.21–1.38) | 19,564 (33.3) | 1.41 *** (1.33–1.5) | 1.47 *** (1.39–1.56) |
| Dietary Diversity Score (DDS) | Growth Outcomes | ||||||||
| Severely Stunting (HAZ < −3 SD) | Severely Wasting (WHZ < −3 SD) | Severely Underweight (WAZ < −3 SD) | |||||||
| Frequency (%) | OR (95% CI) | AOR a (95% CI | Frequency (%) | OR (95% CI) | AOR a (95% CI) | Frequency (%) | OR (95% CI) | AOR a (95% CI | |
| Score 0 | 5808 (16) | ® | ® | 3295 (9.5) | ® | ® | 3918 (11.1) | ® | ® |
| Score 1 | 2189 (17.2) | 1.02 (0.97–1.08) | 0.89 *** (0.84–0.94) | 989 (7.7) | 0.79 *** (0.74–0.86) | 0.84 *** (0.78–0.91) | 1272 (10) | 0.85 *** (0.79–0.91) | 0.79 *** (0.74–0.85) |
| Score 2 | 1262 (17.2) | 1.03 (0.97–1.10) | 0.87 *** (0.81–0.93) | 532 (7.3) | 0.75 *** (0.68–0.82) | 0.8 *** (0.72–0.88) | 681 (10.1) | 0.79 *** (0.72–0.86) | 0.76 *** (0.67–0.79) |
| Score 3 | 661 (14.9) | 0.89 ** (0.82–0.98) | 0.74 *** (0.69–0.81) | 337 (7.1) | 0.80 *** (0.71–0.9) | 0.87 ** (0.78–0.98) | 405 (8.8) | 0.79 *** (0.71–0.88) | 0.73 *** (0.69–0.82) |
| Score 4 | 410 (16.6) | 0.96 (0.86–1.07) | 0.79 *** (0.71–0.89) | 196 (8.2) | 0.80 *** (0.69–0.93) | 0.87 * (0.75–1.01) | 223 (8.8) | 0.75 *** (0.65–0.86) | 0.69 *** (0.6–0.8) |
| Score 5 | 254 (14) | 0.86 ** (0.75–0.99) | 0.7 *** (0.61–0.8) | 98 (5.4) | 0.58 *** (0.47–0.71) | 0.64 *** (0.52–0.79) | 130 (8.3) | 0.63 *** (0.53–0.76) | 0.58 *** (0.48–0.7) |
| Score 6 | 154 (12.1) | 0.803 ** (0.68–0.95) | 0.655 *** (0.55–0.78) | 65 (5.2) | 0.59 *** (0.46–0.77) | 0.67 *** (0.52–0.86) | 73 (6.5) | 0.55 *** (0.43–0.69) | 0.51 *** (0.40–0.65) |
| Score 7 | 199 (16.2) | 0.87 * (0.75–1.02) | 0.72 *** (0.62–0.84) | 84 (7) | 0.64 *** (0.51–0.8) | 0.72 *** (0.57–0.9) | 104 (8.6) | 0.65 *** (0.53–0.8) | 0.61 *** (0.5–0.75) |
| Minimum dietary diversity (MDD) | Frequency (%) | OR (95% CI) | AOR a (95% CI) | Frequency (%) | OR (95% CI) | AOR a (95% CI | Frequency (%) | OR (95% CI) | AOR a (95% CI |
| ≥4 food groups | 1017 (15.1) | ® | ® | 443 (6.7) | ® | ® | 530 (8.3) | ® | ® |
| < 4 food groups | 9920 (16.3) | 1.12 *** (1.05–1.2) | 1.27 *** (1.18–1.36) | 5153 (8.7) | 1.34 *** (1.22–1.49) | 1.24 *** (1.12–1.37) | 6339 (10.6) | 1.39 *** (1.27–1.53) | 1.44 *** (1.31–1.58) |
| Characteristics | Growth Outcomes | |||||
|---|---|---|---|---|---|---|
| Stunting (HAZ < −2 SD) | Wasting (WHZ < −2 SD) | Underweight (WAZ < −2 SD) | ||||
| Crude OR (95% CI) | Model a AOR (95% CI) | Crude OR (95% CI) | Model a AOR (95% CI) | Crude OR (95% CI) | Model a AOR (95% CI) | |
| Food Groups Grains, roots, and tubers | ||||||
| Yes | ® | ® | ® | ® | ® | ® |
| No | 0.87 *** (0.84–0.91) | 0.92 *** (0.88–0.96) | 1.16 *** (1.11–1.22) | 1 (0.95–1.05) | 1.06 *** (1.02–1.10) | 0.95 ** (0.91–0.99) |
| Legumes and nuts | ||||||
| Yes | ® | ® | ® | ® | ® | ® |
| No | 0.99 (0.95–1.04) | 1 (0.95–1.06) | 1.29 *** (1.22–1.36) | 1.07 ** (1–1.14) | 1.25 *** (1.19–1.31) | 1.06 * (1–1.12) |
| Dairy products | ||||||
| Yes | ® | ® | ® | ® | ® | ® |
| No | 1.13 *** (1.07–1.19) | 1.15 *** (1.08–1.22) | 1.37 *** (1.28–1.46) | 1.14 *** (1.06–1.23) | 1.46 *** (1.38–1.55) | 1.23 *** (1.16–1.32) |
| Flesh foods | ||||||
| Yes | ® | ® | ® | ® | ® | ® |
| No | 1.11 *** (1.05–1.16) | 1.14 *** (1.07–1.21) | 1.44 *** (1.35–1.54) | 1.18 *** (1.08–1.27) | 1.5 *** (1.42–1.59) | 1.24 *** (1.16–1.33) |
| Eggs | ||||||
| Yes | ® | ® | ® | ® | ® | ® |
| No | 1.08 *** (1.04–1.13) | 1.13 *** (1.07–1.2) | 1.37 *** (1.3–1.45) | 1.13 *** (1.05–1.2) | 1.44 *** (1.37–1.52) | 1.24 *** (1.17–1.32) |
| Vitamin A-rich fruits and vegetables | ||||||
| Yes | ® | ® | ® | ® | ® | ® |
| No | 0.97 (0.9–1.01) | 1 (0.95–1.05) | 1.15 *** (1.1–1.20) | 0.93 *** (0.88–0.98) | 1.13 *** (1.08–1.18) | 0.93 *** (0.89–0.98) |
| Other fruits and vegetables | ||||||
| Yes | ® | ® | ® | ® | ® | ® |
| No | 1.02 (0.98–1.06) | 1.12 *** (1.07–1.17) | 1.26 *** (1.21–1.32) | 1.1 *** (1.04–1.16) | 1.29 *** (1.24–1.34) | 1.20 *** (1.15–1.26) |
| Characteristics | Growth Outcomes | |||||
|---|---|---|---|---|---|---|
| Severely Stunting (HAZ < −3 SD) | Severely Wasting (WHZ < −3 SD) | Severely Underweight (WAZ < −3 SD) | ||||
| Crude OR (95% CI) | Model a AOR (95% CI) | Crude OR (95% CI) | Model a AOR (95% CI) | Crude OR (95% CI) | Model a AOR (95% CI) | |
| Food groups | ||||||
| Grains, roots, and tubers | ||||||
| Yes | ® | ® | ® | ® | ® | ® |
| No | 0.93 *** (0.89–0.98) | 0.93 ** (0.89–0.99) | 1.16 *** (1.09–1.24) | 0.99 (0.92–1.07) | 1.07 ** (1.01–1.14) | 0.97 (0.91–1.04) |
| Legumes and nuts | ||||||
| Yes | ® | ® | ® | ® | ® | ® |
| No | 1.05 * (0.99–1.12) | 1.01 (0.95–1.09) | 1.34 *** (1.23–1.46) | 1.12 ** (1.01–1.23) | 1.27 *** (1.18–1.38) | 1.07 (0.98–1.17) |
| Dairy products | ||||||
| Yes | ® | ® | ® | ® | ® | ® |
| No | 1.21 *** (1.12–1.3) | 1.16 *** (1.07–1.26) | 1.38 *** (1.25–1.53) | 1.15 ** (1.03–1.29) | 1.48 *** (1.34–1.63) | 1.24 *** (1.12–1.38) |
| Flesh foods | ||||||
| Yes | ® | ® | ® | ® | ® | ® |
| No | 1.15 *** (1.07–1.23) | 1.08 * (1–1.18) | 1.44 *** (1.3–1.59) | 1.17 ** (1.03–1.32) | 1.47 *** (1.34–1.61) | 1.18 *** (1.06–1.31) |
| Eggs | ||||||
| Yes | ® | ® | ® | ® | ® | ® |
| No | 1.18 *** (1.11–1.25) | 1.19 *** (1.10–1.28) | 1.36 *** (1.25–1.48) | 1.11 * (1–1.23) | 1.49 *** (1.38–1.62) | 1.3 *** (1.18–1.43) |
| Vitamin A-rich fruits and vegetables | ||||||
| Yes | ® | ® | ® | ® | ® | ® |
| No | 1.06 ** (1–1.11) | 1.05 (0.99–1.12) | 1.15 *** (1.07–1.24) | 0.93 * (0.85–1.01) | 1.12 *** (1.05–1.19) | 0.92 ** (0.85–0.99) |
| Other fruits and vegetables | ||||||
| Yes | ® | ® | ® | ® | ® | ® |
| No | 1.07 ** (1.02–1.12) | 1.1 *** (1.04–1.17) | 1.25 *** (1.18–1.34) | 1.08 * (0.99–1.16) | 1.29 *** (1.22–1.38) | 1.20 *** (1.12–1.29) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Saha, J.; Chouhan, P.; Malik, N.I.; Ghosh, T.; Das, P.; Shahid, M.; Ahmed, F.; Tang, K. Effects of Dietary Diversity on Growth Outcomes of Children Aged 6 to 23 Months in India: Evidence from National Family and Health Survey. Nutrients 2023, 15, 159. https://doi.org/10.3390/nu15010159
Saha J, Chouhan P, Malik NI, Ghosh T, Das P, Shahid M, Ahmed F, Tang K. Effects of Dietary Diversity on Growth Outcomes of Children Aged 6 to 23 Months in India: Evidence from National Family and Health Survey. Nutrients. 2023; 15(1):159. https://doi.org/10.3390/nu15010159
Chicago/Turabian StyleSaha, Jay, Pradip Chouhan, Najma Iqbal Malik, Tanmoy Ghosh, Puja Das, Muhammad Shahid, Farooq Ahmed, and Kun Tang. 2023. "Effects of Dietary Diversity on Growth Outcomes of Children Aged 6 to 23 Months in India: Evidence from National Family and Health Survey" Nutrients 15, no. 1: 159. https://doi.org/10.3390/nu15010159
APA StyleSaha, J., Chouhan, P., Malik, N. I., Ghosh, T., Das, P., Shahid, M., Ahmed, F., & Tang, K. (2023). Effects of Dietary Diversity on Growth Outcomes of Children Aged 6 to 23 Months in India: Evidence from National Family and Health Survey. Nutrients, 15(1), 159. https://doi.org/10.3390/nu15010159













