Development and Validation of a Food and Nutrition Literacy Questionnaire for Chinese Adults
Abstract
:1. Introduction
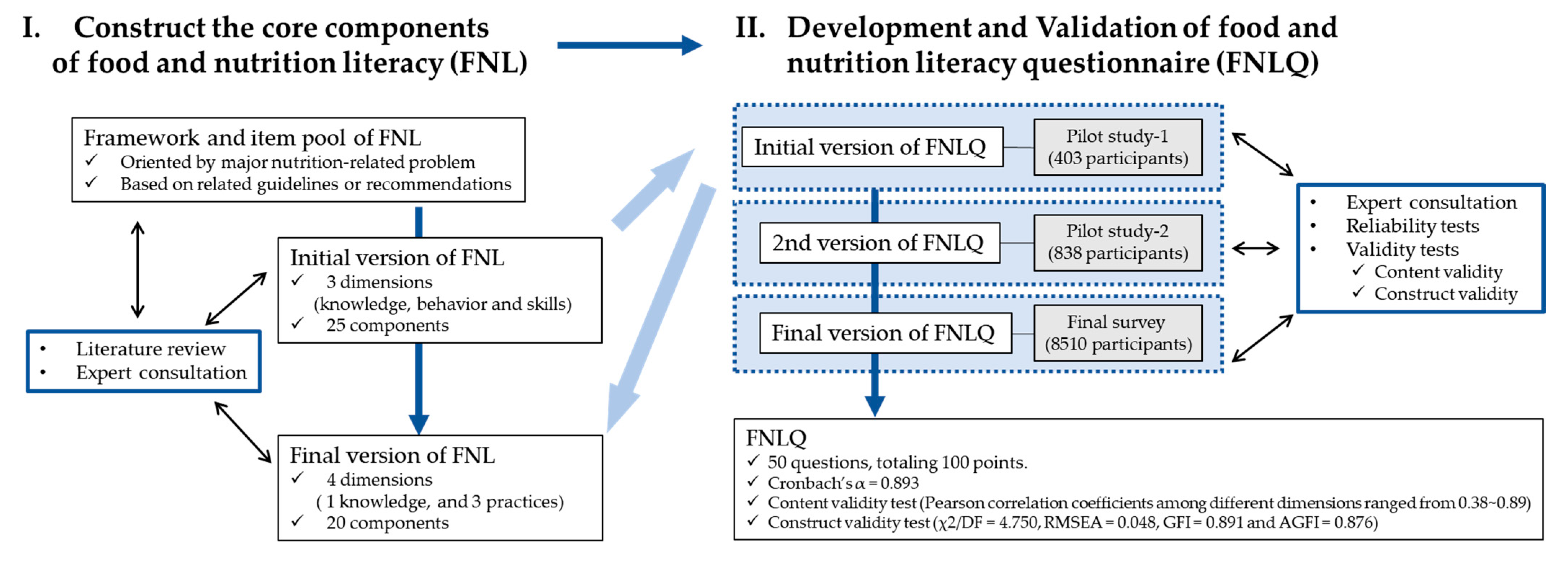
2. Materials and Methods
2.1. Development of Questionnaire
- Stage 1: construct the core components of Food and Nutrition Literacy
- Stage 2: Develop the FNLQ
2.2. Validation of Questionnaire
2.2.1. Data Collection
2.2.2. Reliability Tests
2.2.3. Validity Tests
2.3. Statistical Analysis
3. Results
3.1. Core Components of Food and Nutrition Literacy
3.2. Demographic Characteristics of Participants
3.3. Reliability
3.4. Construct Validity
3.5. Content Validity
3.6. Assessing Food and Nutrition Literacy and Its Related Factors
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Acknowledgments
Conflicts of Interest
References
- GBD 2017 Diet Collaborators. Health effects of dietary risks in 195 countries, 1990–2017: A systematic analysis for the Global Burden of Disease Study 2017. Lancet 2019, 393, 1958–1972. [Google Scholar] [CrossRef]
- FAO; IFAD; UNICEF; WFP; WHO. The State of Food Security and Nutrition in the World 2019. In Safeguarding against Economic Slowdowns and Downturns; FAO: Rome, Italy, 2019. [Google Scholar]
- National Health and Family Planning Commission Disease Control and Prevention Bureau. Report on the Nutrition and Chronic Disease Status of Chinese Residents (2020). Acta Nutr. Sin. 2020, 42, 521. [Google Scholar]
- Yuxuan, G.; Yansu, H.; Shahmir, H.A.; Kaitlyn, H.; Hengjin, D.; Joel, G. Fruit and Vegetable Intake and All-Cause Mortality in a Chinese Population: The China Health and Nutrition Survey. Int. J. Environ. Res. Public Health 2021, 18, 342. [Google Scholar]
- Lina, H.; Huijun, W.; Zhihong, W.; Jiguo, Z.; Bing, Z.; Gangqiang, D. Regional Disparities in the Association between Cereal Consumption and Metabolic Syndrome: Results from the China Health and Nutrition Survey. Nutrients 2019, 11, 764. [Google Scholar]
- Liu, T.; Su, X.; Li, N.; Sun, J.; Ma, G.; Zhu, W. Development and validation of a food and nutrition literacy questionnaire for Chinese schoolage children. PLoS ONE 2021, 16, e0244197. [Google Scholar]
- Carbone, E.T.; Zoellner, J.M. Nutrition and health literacy: A systematic review to inform nutrition research and practice. J. Acad. Nutr. Diet 2012, 112, 254–265. [Google Scholar] [CrossRef]
- Xia, J.; Wu, P.; Deng, Q.; Yan, R.; Yang, R.; Lv, B.; Wang, J.; Yu, J. Relationship between health literacy and quality of life among cancer survivors in China: A cross-sectional study. BMJ Open 2019, 9, e028458. [Google Scholar] [CrossRef]
- Finbråten, H.S.; Guttersrud, Ø.; Nordström, G.; Pettersen, K.S.; Trollvik, A.; Wilde-Larsson, B. Explaining variance in health literacy among people with type 2 diabetes: The association between health literacy and health behaviour and empowerment. BMC Public Health 2020, 20, 161. [Google Scholar] [CrossRef]
- Taylor, M.K.; Sullivan, D.K.; Ellerbeck, E.F.; Gajewski, B.J.; Gibbs, H.D. Nutrition literacy predicts adherence to healthy/unhealthy diet patterns in adults with a nutrition-related chronic condition. Public Health Nutr. 2019, 22, 2157–2169. [Google Scholar] [CrossRef]
- Gazmararian, J.A.; Kripalani, S.; Miller, M.J.; Echt, K.V.; Ren, J.; Rask, K. Factors associated with medication refill adherence in cardiovascular-related diseases: A focus on health literacy. J. Gen. Intern. Med. 2006, 21, 1215–1221. [Google Scholar] [CrossRef]
- Parmenter, K.; Waller, J.; Wardle, J. Demographic variation in nutrition knowledge in England. Health Educ. Res. 2000, 15, 163–174. [Google Scholar] [CrossRef] [PubMed]
- Zoellner, J.; Connell, C.; Bounds, W.; Crook, L.; Yadrick, K. Nutrition literacy status and preferred nutrition communication channels among adults in the Lower Mississippi Delta. Prev. Chronic. Dis. 2009, 6, A128. [Google Scholar] [PubMed]
- Silk, K.J.; Sherry, J.; Winn, B.; Keesecker, N.; Horodynski, M.A.; Sayir, A. Increasing nutrition literacy: Testing the effectiveness of print, web site, and game modalities. J. Nutr. Educ. Behav. 2008, 40, 3–10. [Google Scholar] [CrossRef] [PubMed]
- Doustmohammadian, A.; Omidvar, N.; Keshavarz-Mohammadi, N.; Abdollahi, M.; Amini, M.; Eini-Zinab, H. Developing and validating a scale to measure Food and Nutrition Literacy (FNLIT) in elementary school children in Iran. PLoS ONE 2017, 12, e0179196. [Google Scholar] [CrossRef]
- Carbone, E.T.; Gibbs, H.D. Measuring Nutrition Literacy: Problems and Potential Solutions. J. Nutr. Disord. Ther. 2012, 3, e105. [Google Scholar] [CrossRef]
- Parekh, N.; Jiang, J.; Buchan, M.; Meyers, M.; Gibbs, H.; Krebs, P. Nutrition Literacy among Cancer Survivors: Feasibility Results from the Healthy Eating and Living Against Breast Cancer (HEAL-BCa) Study: A Pilot Randomized Controlled Trial. J. Cancer Educ. 2017, 33, 1239–1249. [Google Scholar] [CrossRef]
- Fraser, S.D.; Roderick, P.J.; Casey, M.; Taal, M.; Yuen, H.M.; Nutbeam, D. Prevalence and associations of limited health literacy in chronic kidney disease: A systematic review. Nephrol. Dial. Transpl. 2013, 28, 129–137. [Google Scholar] [CrossRef]
- Park, Y.-H.; Song, M.; Cho, B.-L.; Lim, J.-Y.; Song, W.; Kim, S.-H. The effects of an integrated health education and exercise program in community-dwelling older adults with hypertension: A randomized controlled trial. Patient Educ. Couns. 2011, 82, 133–137. [Google Scholar] [CrossRef]
- Gibbs, H.D. Nutrition Literacy: Foundations and Development of an Instrument for Assessment. 2012. Available online: https://www.ideals.illinois.edu/handle/2142/31202 (accessed on 20 February 2022).
- Diamond, J.J. Development of a reliable and construct valid measure of nutritional literacy in adults. Nutr. J. 2007, 6, 5. [Google Scholar] [CrossRef]
- Guttersrud, O.; Dalane, J.Ø.; Pettersen, S. Improving measurement in nutrition literacy research using Rasch modelling: Examining construct validity of stage-specific ’critical nutrition literacy’ scales. Public Health Nutr. 2014, 17, 877–883. [Google Scholar] [CrossRef]
- Weiss, B.D.; Mays, M.Z.; Martz, W.; Castro, K.M.; DeWalt, D.A.; Pignone, M.P.; Mockbee, J.; Hale, F.A. Quick assessment of literacy in primary care: The Newest Vital Sign. Ann. Fam. Med. 2005, 3, 514–522. [Google Scholar] [CrossRef] [PubMed]
- Polit, D.F.; Beck, C.T.; Owen, S.V. Is the CVI an acceptable indicator of content validity? Appraisal and recommendations. Res. Nurs. Health 2007, 30, 459–467. [Google Scholar] [CrossRef] [PubMed]
- Zhang, J.; Sun, H. Application of Knowledge-Attitude-Practice Model Nursing Intervention in Early Rehabilitation of Stroke Patients. Chin. J. Pract. Neurol. Dis. 2012, 15, 88–89. [Google Scholar]
- Sakane, Y.; Yamaguchi, M.; Yokoi, N.; Uchino, M.; Dogru, M.; Oishi, T.; Ohashi, Y.; Ohashi, Y. Development and validation of the dry eye-related quality-of-life score questionnaire. JAMA Ophthalmol. 2013, 131, 1331–1338. [Google Scholar] [CrossRef]
- Wang, S.S.; Lay, S.; Yu, H.N.; Shen, S.R. Dietary Guidelines for Chinese Residents (2016): Comments and comparisons. J. Zhejiang Univ. Sci. B 2016, 17, 649–656. [Google Scholar] [CrossRef]
- Mozaffarian, D. Dietary and policy priorities for cardiovascular disease, diabetes, and obesity: A comprehensive review. Circulation 2016, 133, 187–225. [Google Scholar] [CrossRef]
- Gibbs, H.D.; Ellerbeck, E.F.; Gajewski, B.; Zhang, C.; Sullivan, D.K. The Nutrition Literacy Assessment Instrument is a Valid and Reliable Measure of Nutrition Literacy in Adults with Chronic Disease. J. Nutr. Edu. Behav. 2018, 50, 247–257. [Google Scholar] [CrossRef]
- Vidgen, H.A.; Gallegos, D. Defining food literacy and its components. Appetite 2014, 76, 50–59. [Google Scholar] [CrossRef]
- Tessy, B.; Nele, S.; Joke, V.; Astrid, V.; Charlotte, D.B.; Peter, Y.; Christophe, M. A Mixed-Method Approach to Develop and Validate an Integrated Food Literacy Tool for Personalized Food Literacy Guidance. Front. Nutr. 2022, 8, 760493. [Google Scholar]
- Taylor, R.S.; Brown, A.; Ebrahim, S.; Jolliffe, J.; Noorani, H.; Rees, K.; Skidmore, B.; Stone, J.A.; Thompson, D.R.; Oldridge, N. Exercise-based rehabilitation for patients with coronary heart disease: Systematic review and meta-analysis of randomized controlled trials. Am. J. Med. 2004, 116, 682–692. [Google Scholar] [CrossRef]
- Indrani, K. The impact of nutrition literacy on the food habits among young adults in Turkey. Nutr. Res. Pract. 2019, 13, 352–357. [Google Scholar]
- Maria, L.S.; Laura, G.; Anna, S.; Laura, R. Relationship Between Nutrition Knowledge and Dietary Intake: An Assessment Among a Sample of Italian Adults. Front. Nutr. 2021, 8, 714493. [Google Scholar]
- Queenie, P.S.L.; Alice, H.Y.Y.; Joanne, W.Y.C. Chinese adults′ nutrition label literacy in Hong Kong: Implications for nurses. Nurs. Health Sci. 2019, 21, 171–177. [Google Scholar]
- Mónica, M.; Tatiana, F.; Cíntia, F. Nutrition Literacy of Portuguese Adults-A Pilot Study. Int. J. Environ. Res. Public Health 2021, 18, 3177. [Google Scholar]
| Domain | Dimension | Components | The Second Round Consultation | ||||
|---|---|---|---|---|---|---|---|
| N # | I-CVI | Pc | K * | S-CVI | |||
| Knowledge | Food and nutrition Knowledge |
| 12 | 1.00 | 0.0002 | 1.00 | 0.98 |
| 12 | 1.00 | 0.0002 | 1.00 | |||
| 12 | 1.00 | 0.0002 | 1.00 | |||
| 11 | 0.92 | 0.0029 | 0.92 | |||
| Practices | Access to and planning and selecting for food |
| 10 | 0.83 | 0.0161 | 0.83 | 0.93 |
| 10 | 0.83 | 0.0161 | 0.83 | |||
| 11 | 0.92 | 0.0029 | 0.92 | |||
| 12 | 1.00 | 0.0002 | 1.00 | |||
| 12 | 1.00 | 0.0002 | 1.00 | |||
| 12 | 1.00 | 0.0002 | 1.00 | |||
| Preparing and marking food |
| 12 | 1.00 | 0.0002 | 1.00 | 1.00 | |
| 12 | 1.00 | 0.0002 | 1.00 | |||
| 12 | 1.00 | 0.0002 | 1.00 | |||
| Eating |
| 12 | 1.00 | 0.0002 | 1.00 | 0.93 | |
| 11 | 0.92 | 0.0029 | 0.92 | |||
| 12 | 1.00 | 0.0002 | 1.00 | |||
| 11 | 0.92 | 0.0029 | 0.92 | |||
| 10 | 0.83 | 0.0161 | 0.83 | |||
| 10 | 0.83 | 0.0161 | 0.83 | |||
| 12 | 1.00 | 0.0002 | 1.00 | |||
| Characteristics | Total (N = 8510) | Reliability and Validity Tests |
|---|---|---|
| (N = 841) | ||
| Age (mean ± SD) | 34.47 ± 7.41 | 33.88 ± 7.38 |
| BMI (mean ± SD) | 21.57 ± 2.92 | 21.37 ± 2.80 |
| Gender | ||
| Male (n, %) | 4577 (53.8%) | 438 (52.1%) |
| Female (n, %) | 3933 (46.2%) | 403 (47.9%) |
| Education level | ||
| Junior high school degree or below | 382 (4.5%) | 40 (4.8%) |
| Senior high school degree | 2986 (35.1%) | 285 (33.9%) |
| Bachelor’s/Technical degree or above | 5142 (60.4%) | 516 (61.4%) |
| Marriage status | ||
| Never married | 1406 (16.5%) | 150 (17.8%) |
| Married | 6276 (73.7%) | 614 (73.0%) |
| Divorced | 765 (9%) | 69 (8.2%) |
| Other | 63 (0.7%) | 8 (1.0%) |
| Healthcare related work experience | ||
| Yes | 4395 (51.6%) | 441 (52.4%) |
| No | 4115 (48.4%) | 400 (47.6%) |
| Family income * | ||
| ≤5000 CNY/month | 784 (9.2%) | 66 (7.8%) |
| 5000~8000 CNY/month | 1461 (17.2%) | 156 (18.5%) |
| 8000~13,000 CNY/month | 2429 (28.5%) | 232 (27.6%) |
| 13,000~17,000 CNY/month | 1752 (20.6%) | 170 (20.2%) |
| 17,000~24,000 CNY/month | 1241 (14.6%) | 119 (14.1%) |
| >24,000 CNY/month | 843 (9.9%) | 98 (11.7%) |
| Chronic diseases | ||
| None | 5331 (62.6%) | 540 (64.2%) |
| Single disease | 811 (9.5%) | 70 (8.3%) |
| Multimorbidity & | 2368 (27.8%) | 231 (27.5%) |
| Dimensions | Knowledge (8′) | Selecting Food (30′) | Preparing Food (22′) | Eating (40′) | Total (100′) |
|---|---|---|---|---|---|
| Knowledge | -- | 0.439 ** | 0.375 ** | 0.668 ** | 0.665 ** |
| Selecting food | 0.439 ** | -- | 0.797 ** | 0.480 ** | 0.887 ** |
| Preparing food | 0.375 ** | 0.797 ** | -- | 0.391 ** | 0.834 ** |
| Eating | 0.668 ** | 0.480 ** | 0.391 ** | -- | 0.782 ** |
| Variables | Total (100′) | Knowledge (8′) | Selecting Food (30′) | Preparing Food (22′) | Eating (40′) |
|---|---|---|---|---|---|
| Total | 64.08 ± 12.77 | 5.84 ± 1.32 | 16.53 ± 4.99 | 12.91 ± 4.25 | 28.79 ± 4.89 |
| Age | |||||
| 15~30 | 63.93 ± 12.31 | 5.87 ± 1.31 | 16.59 ± 4.93 | 12.79 ± 4.07 | 28.68 ± 4.83 |
| 31~45 | 64.26 ± 12.89 | 5.83 ± 1.29 | 16.55 ± 5.02 | 12.99 ± 4.29 | 28.89 ± 4.90 |
| 46~60 | 63.18 ± 13.39 | 5.85 ± 1.52 | 16.18 ± 4.96 | 12.70 ± 4.53 | 28.45 ± 4.96 |
| Gender | |||||
| Male | 61.56 ± 12.44 | 5.68 ± 1.35 | 15.57 ± 4.80 | 11.99 ± 4.03 | 28.30 ± 5.07 |
| Female | 67.02 ± 12.50 a | 6.03 ± 1.26 a | 17.65 ± 4.98 a | 13.98 ± 4.26 a | 29.36 ± 4.59 a |
| Education level | |||||
| Junior high school degree | 52.63 ± 10.65 | 4.85 ± 1.67 | 12.45 ± 3.45 | 9.59 ± 2.83 | 25.74 ± 5.98 |
| Senior high school degree | 59.27 ± 12.18 a | 5.49 ± 1.46 a | 14.61 ± 4.48 a | 11.40 ± 3.92 a | 27.77 ± 5.32 a |
| Bachelor’s/Technical degree or above | 67.72 ± 11.79 a,b | 6.13 ± 1.10 a,b | 17.95 ± 4.83 a,b | 14.04 ± 4.13 a,b | 29.61 ± 4.30 a,b |
| Marriage status | |||||
| Never married | 65.96 ± 11.58 | 6.11 ± 1.25 | 17.35 ± 4.79 | 13.58 ± 4.01 | 28.92 ± 4.54 |
| Married | 65.09 ± 12.62 a | 5.90 ± 1.23 a | 16.87 ± 4.98 a | 13.21 ± 4.26 a | 29.11 ± 4.71 a |
| Divorced | 53.20 ± 10.17 a | 4.99 ± 1.63 a,b | 12.50 ± 3.24 a,b | 9.46 ± 2.72 a,b | 26.25 ± 5.84 a,b |
| Other | 53.26 ± 13.64 b,c | 4.58 ± 1.85 a,b | 13.25 ± 4.50 a,b | 10.29 ± 3.67 a,b | 25.14 ± 6.13 a,b |
| Healthcare related work experience | |||||
| Yes | 60.91 ± 12.56 | 5.68 ± 1.39 | 15.22 ± 4.81 | 11.66 ± 3.97 | 28.35 ± 5.18 |
| No | 67.46 ± 12.11 a | 6.02 ± 1.21 a | 17.93 ± 4.79 a | 14.25 ± 4.13 a | 29.26 ± 4.51 a |
| Family income * | |||||
| ≤5000 CNY/month | 66.79 ± 10.65 | 6.27 ± 1.28 | 17.62 ± 4.35 | 14.10 ± 3.76 | 28.80 ± 4.30 |
| 5000~8000 CNY/month | 65.30 ± 12.44 a | 5.90 ± 1.25 a | 16.90 ± 4.93 a | 13.60 ± 4.23 a | 28.91 ± 4.68 |
| 8000~13,000 CNY/month | 61.06 ± 12.43 a,b | 5.65 ± 1.32 a,b | 15.32 ± 4.79 a,b | 11.85 ± 4.09 a,b | 28.24 ± 4.97 a,b |
| 13,000~17,000 CNY/month | 61.82 ± 12.40 a,b | 5.68 ± 1.32 a,b | 15.65 ± 4.81 a,b | 11.99 ± 4.02 a,b | 28.50 ± 4.99 b |
| 17,000~24,000 CNY/month | 65.44 ± 13.36 a,b,c,d | 5.94 ± 1.41 a,b | 17.18 ± 5.09 a,c,d | 13.36 ± 4.36 a,b,d | 28.95 ± 5.04 b |
| >24,000 CNY/month | 70.83 ± 12.31 a,c,d,e | 6.14 ± 1.15 a,c,d,e | 19.26 ± 4.95 a,c,d,e | 14.93 ± 4.16 a,c,d,e | 30.50 ± 4.67 a,b,c,d,e |
| Chronic diseases | |||||
| None | 67.10 ± 12.51 | 6.02 ± 1.27 | 17.77 ± 4.94 | 13.99 ± 4.18 | 29.32 ± 4.71 |
| Single disease | 64.21 ± 13.21 a,c | 5.79 ± 1.43 a,c | 16.87 ± 4.85 a,c | 13.54 ± 4.17 a,c | 28.01 ± 5.09 a,c |
| Multimorbidity & | 57.22 ± 10.30 a,b | 5.74 ± 1.30 a,b | 13.63 ± 3.83 a,b | 10.26 ± 3.14 a,b | 27.87 ± 5.04 a |
| BMI | |||||
| 18.5~23.9 | 64.71 ± 12.70 | 5.88 ± 1.27 | 16.73 ± 4.99 | 13.06 ± 4.25 | 29.03 ± 4.85 |
| <18.5 or ≥24.0 | 62.74 ± 12.79 a | 5.76 ± 1.40 a | 16.10 ± 4.95 a | 12.59 ± 4.23 a | 28.28 ± 4.92 a |
| Variables * | β | SE | B | T | p |
|---|---|---|---|---|---|
| (Constant) | 56.09 | 0.75 | 74.94 | 0.00 | |
| Gender (Female) | 3.16 | 0.24 | 0.12 | 13.15 | 0.00 |
| Education level | |||||
| Junior high school degree or below | -- | ||||
| Senior high school degree | 4.18 | 0.59 | 0.16 | 7.06 | 0.00 |
| Bachelor’s/Technical degree or above | 9.70 | 0.59 | 0.37 | 16.38 | 0.00 |
| Marriage status | |||||
| Never married | -- | ||||
| Married | 0.90 | 0.32 | 0.03 | 2.77 | 0.01 |
| Divorced | −5.35 | 0.51 | −0.12 | −10.41 | 0.00 |
| Other | −7.27 | 1.40 | −0.05 | −5.20 | 0.00 |
| Healthcare related work experience (YES) | 3.34 | 0.25 | 0.13 | 13.54 | 0.00 |
| Family income | |||||
| ≤5000 RMB/month | -- | ||||
| 5000~8000 RMB/month | −0.01 | 0.48 | −0.00 | −0.03 | 0.98 |
| 8000~13,000 RMB/month | −2.87 | 0.45 | −0.10 | −6.34 | 0.00 |
| 13,000~17,000 RMB/month | −1.79 | 0.47 | −0.06 | −3.77 | 0.00 |
| 17,000~24,000 RMB/month | −0.06 | 0.50 | −0.00 | −0.11 | 0.91 |
| >24,000 RMB/month | 3.89 | 0.54 | 0.09 | 7.15 | 0.00 |
| Chronic diseases | |||||
| None | -- | ||||
| Single disease | −2.34 | 0.41 | −0.05 | −5.74 | 0.00 |
| Multimorbidity & | −5.40 | 0.29 | −0.19 | −18.70 | 0.00 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zhang, Y.; Zhang, Z.; Xu, M.; Aihemaitijiang, S.; Ye, C.; Zhu, W.; Ma, G. Development and Validation of a Food and Nutrition Literacy Questionnaire for Chinese Adults. Nutrients 2022, 14, 1933. https://doi.org/10.3390/nu14091933
Zhang Y, Zhang Z, Xu M, Aihemaitijiang S, Ye C, Zhu W, Ma G. Development and Validation of a Food and Nutrition Literacy Questionnaire for Chinese Adults. Nutrients. 2022; 14(9):1933. https://doi.org/10.3390/nu14091933
Chicago/Turabian StyleZhang, Yaqin, Zhaofeng Zhang, Meihong Xu, Sumiya Aihemaitijiang, Chen Ye, Wenli Zhu, and Guansheng Ma. 2022. "Development and Validation of a Food and Nutrition Literacy Questionnaire for Chinese Adults" Nutrients 14, no. 9: 1933. https://doi.org/10.3390/nu14091933
APA StyleZhang, Y., Zhang, Z., Xu, M., Aihemaitijiang, S., Ye, C., Zhu, W., & Ma, G. (2022). Development and Validation of a Food and Nutrition Literacy Questionnaire for Chinese Adults. Nutrients, 14(9), 1933. https://doi.org/10.3390/nu14091933










