Cost–Benefit and Cost–Utility Analyses to Demonstrate the Potential Value-for-Money of Supermarket Shelf Tags Promoting Healthier Packaged Products in Australia
Abstract
:1. Introduction
2. Materials and Methods
2.1. The Intervention
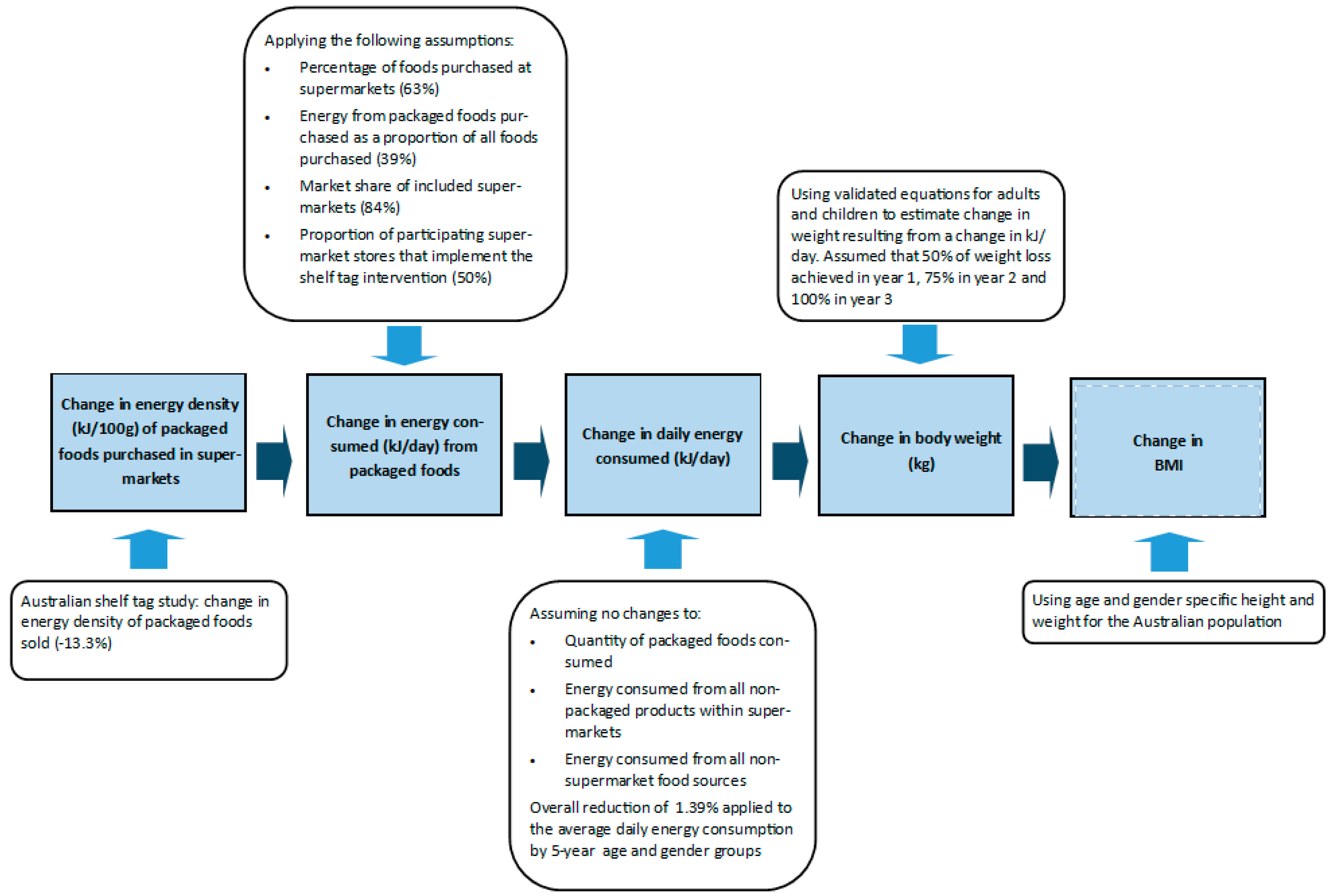
2.2. Modelling the Intervention Impact on Population Energy Intake and Weight
2.3. Modelling the Cost of the Intervention
2.3.1. Supermarket Costs
2.3.2. Government Costs
2.4. Overview of Cost-Effectiveness Modelling
2.4.1. Cost–Benefit Analysis Modelling
2.4.2. Cost–Utility Analysis Modelling
2.4.3. Sensitivity Analyses
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Australian Institute of Health and Welfare. Overwight and Obesity: An Interactive Insight. Cat No. PHE 251. Available online: https://www.aihw.gov.au/reports/overweight-obesity/overweight-and-obesity-an-interactive-insight (accessed on 25 November 2020).
- Australian Institute of health and Welfare. A Picture of Overweight and Obesity in Australia; AIHW: Canberra, Australia, 2017. [Google Scholar]
- Swinburn, B.A.; Sacks, G.; Hall, K.D.; McPherson, K.; Finegood, D.T.; Moodie, M.L.; Gortmaker, S.L. The global obesity pandemic: Shaped by global drivers and local environments. Lancet 2011, 378, 804–814. [Google Scholar] [CrossRef]
- Dawson, J. Retailer activity in shaping food choice. Food Qual. Prefer. 2013, 28, 339–347. [Google Scholar] [CrossRef]
- Department of Agriculture Fisheries and Forestry. FOODmap. An Analysis of the Australian Food Supply Chain; Department of Agriculture Fisheries and Forestry: Canberra, Australia, 2012; ISBN 978-1-921575-46-4. [Google Scholar]
- Adam, A.; Jensen, J.D. What is the effectiveness of obesity related interventions at retail grocery stores and supermarkets?—A systematic review. BMC Public Health 2016, 16, 1247. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cameron, A.J.; Charlton, E.; Ngan, W.W.; Sacks, G. A Systematic Review of the Effectiveness of Supermarket-Based Interventions Involving Product, Promotion, or Place on the Healthiness of Consumer Purchases. Curr. Nutr. Rep. 2016, 5, 129–138. [Google Scholar] [CrossRef]
- Cawley, J.; Sweeney, M.J.; Sobal, J.; Just, D.R.; Kaiser, H.M.; Schulze, W.D.; Wansink, B.; Wethington, E. The impact of a supermarket nutrition rating system on purchases of nutritious and less nutritious foods. Public Health Nutr. 2015, 18, 8–14. [Google Scholar] [CrossRef] [Green Version]
- Epstein, L.H.; Finkelstein, E.A.; Katz, D.L.; Jankowiak, N.; Pudlewski, C.; Paluch, R.A. Effects of nutrient profiling and price changes based on NuVal® scores on food purchasing in an online experimental supermarket. Public Health Nutr. 2016, 19, 2157–2164. [Google Scholar] [CrossRef] [Green Version]
- Finkelstein, E.A.; Li, W.; Melo, G.; Strombotne, K.; Zhen, C. Identifying the effect of shelf nutrition labels on consumer purchases: Results of a natural experiment and consumer survey. Am. J. Clin. Nutr. 2018, 107, 647–651. [Google Scholar] [CrossRef]
- Hobin, E.; Bollinger, B.; Sacco, J.; Liebman, E.L.I.; Vanderlee, L.; Zuo, F.E.I.; Rosella, L.; L’Abbe, M.; Manson, H.; Hammond, D. Consumers’ Response to an On-Shelf Nutrition Labelling System in Supermarkets: Evidence to Inform Policy and Practice. Milbank Q. 2017, 95, 494–534. [Google Scholar] [CrossRef]
- Melo, G.; Zhen, C.; Colson, G. Does Point-of-Sale Nutrition Information Improve the Nutritional Quality of Food Choices? Econ. Hum. Biol. 2019, 35, 133–143. [Google Scholar] [CrossRef]
- Nikolova, H.D.; Inman, J.J. Healthy Choice: The Effect of Simplified Point-of-Sale Nutritional Information on Consumer Food Choice Behavior. J. Mark. Res. (JMR) 2015, 52, 817–835. [Google Scholar] [CrossRef]
- Sutherland, L.A.; Kaley, L.A.; Fischer, L. Guiding stars: The effect of a nutrition navigation program on consumer purchases at the supermarket. Am. J. Clin. Nutr. 2010, 91, 1090S–1094S. [Google Scholar] [CrossRef] [PubMed]
- Vandevijvere, S.; Berger, N. The impact of shelf tags with Nutri-Score on consumer purchases: A difference-in-difference analysis of a natural experiment in supermarkets of a major retailer in Belgium. Int. J. Behav. Nutr. Phys. Act. 2021, 18, 150. [Google Scholar] [CrossRef] [PubMed]
- Department of Health. About Health Star Ratings. Available online: http://www.healthstarrating.gov.au/internet/healthstarrating/publishing.nsf/Content/About-health-stars (accessed on 25 November 2020).
- Jones, A.; Shahid, M.; Neal, B. Uptake of Australia’s Health Star Rating System. Nutrients 2018, 10, 997. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shahid, M.; Neal, B.; Jones, A. Uptake of Australia’s Health Star Rating System 2014–2019. Nutrients 2020, 12, 1791. [Google Scholar] [CrossRef] [PubMed]
- Cameron, A.J.; Brown, A.; Orellana, L.; Marshall, J.; Crino, M.; Charlton, E.; Ngan, W.; Ananthapavan, A.; Lindsay, J.; Blake, M.; et al. Health Star Ratings on supermarket shelf tags to promote sales of healthy packaged foods store-wide. Nutrients 2022. Submitted. [Google Scholar]
- Ananthapavan, J.; Sacks, G.; Moodie, M.; Carter, R. Economics of obesity--learning from the past to contribute to a better future. Int. J. Environ. Res. Public Health 2014, 11, 4007–4025. [Google Scholar] [CrossRef]
- Department of Health. Guidelines for Preparing a Submission to the Pharmaceutical Benefits Advisory Committee. Version 5.0; Department of Health: Canberra, Australia, 2016. [Google Scholar]
- Department of Health. Technical Guidelines for Preparing Assessment Reports for the Medical Services Advisory Committee–Service Type: Investigative (Version 3.0); Department of Health: Canberra, Australia, 2017. [Google Scholar]
- McIntosh, E.; Baba, C.; Botha, W. Applied Health Economics for Public Health Practice and Research. In Cost–Benefit Analysis for Applied Public Health Economic Evaluation; Oxford University Press: Oxford, UK, 2019. [Google Scholar]
- Weatherly, H.; Drummond, M.; Claxton, K.; Cookson, R.; Ferguson, B.; Godfrey, C.; Rice, N.; Sculpher, M.; Sowden, A. Methods for assessing the cost-effectiveness of public health interventions: Key challenges and recommendations. Health Policy 2009, 93, 85–92. [Google Scholar] [CrossRef]
- Kim, D.D.; Silver, M.C.; Kunst, N.; Cohen, J.T.; Ollendorf, D.A.; Neumann, P.J. Perspective and Costing in Cost-Effectiveness Analysis, 1974–2018. Pharmacoeconomics 2020, 38, 1135–1145. [Google Scholar] [CrossRef]
- Fattore, G.; Federici, C.; Drummond, M.; Mazzocchi, M.; Detzel, P.; Hutton, Z.V.; Shankar, B. Economic evaluation of nutrition interventions: Does one size fit all? Health Policy 2021, 125, 1238–1246. [Google Scholar] [CrossRef]
- Buchanan, J.; Wordsworth, S. Welfarism versus extra-welfarism: Can the choice of economic evaluation approach impact on the adoption decisions recommended by economic evaluation studies? Pharmacoeconomics 2015, 33, 571–579. [Google Scholar] [CrossRef]
- McIntosh, E.; Clarke, P.; Frew, E.; Louviere, J. Applied Methods of Cost-Benefit Analysis in Health Care; Oxford University Press, Incorporated: Oxford, UK, 2010. [Google Scholar]
- Blake, M.R.; Sacks, G.; Marshall, J.; Brown, A.K.; Cameron, A.J. A successful intervention research collaboration between a supermarket chain, the local government, a non-government or-ganisation, and academic researchers: The Eat Well @ IGA healthy supermarket partnership. In The Handbook of Health Promotion Research; Jourdan, D.P.L., Ed.; Springer: Cham, Switzerland, 2022. [Google Scholar]
- Dunford, E.; Trevena, H.; Goodsell, C.; Ng, K.H.; Webster, J.; Millis, A.; Goldstein, S.; Hugueniot, O.; Neal, B. FoodSwitch: A Mobile Phone App to Enable Consumers to Make Healthier Food Choices and Crowdsourcing of National Food Composition Data. JMIR mHealth uHealth 2014, 2, e37. [Google Scholar] [CrossRef] [PubMed]
- Food Standards Australia and New Zealand. AUSNUT 2011–2013. Available online: https://www.foodstandards.gov.au/science/monitoringnutrients/ausnut/pages/default.aspx (accessed on 4 June 2020).
- IBISWorld. Industry Report G4111 Supermarkets and Grocery Stores in Australia; G4111 February 2018; IBISWorld: Los Angeles, CA, USA, 2018. [Google Scholar]
- ABS 43640DO001_20112012; Australian Health Survey: Nutrition First Results–Foods and Nutrients, 2011–2012—Australia. Australian Bureau of Statistics: Canberra, Australia, 2014.
- Hall, K.D.; Sacks, G.; Chandramohan, D.; Chow, C.C.; Wang, Y.C.; Gortmaker, S.L.; Swinburn, B.A. Quantification of the effect of energy imbalance on bodyweight. Lancet 2011, 378, 826–837. [Google Scholar] [CrossRef] [Green Version]
- Hall, K.D.; Butte, N.F.; Swinburn, B.A.; Chow, C.C. Dynamics of childhood growth and obesity: Development and validation of a quantitative mathematical model. Lancet Diabetes Endocrinol. 2013, 1, 97–105. [Google Scholar] [CrossRef] [Green Version]
- 4364055001DO008_20172018; National Health Survey: First Results, 2017–2018—Australia. Table 8.1 Body Mass Index, Waist circumference, Height and Weight(a)(b), Persons. Australian Bureau of Statistics: Canberra, Australian, 2018.
- 4364055001DO016_20172018; National Health Survey: First Results, 2017–2018—Australia. Table 16.1 Children’s Body Mass Index, Waist Circumference, Height and Weight(a)(b), Persons. Australian Bureau of Statistics: Canberra, Australian, 2018.
- Euromonitor International. Retailing in Australia; Euromonitor International: London, UK, 2018. [Google Scholar]
- NSW Food Authority. Review of Fast-Food Labelling Requirements (“Fast Choices”); NSW Government: Sydney, Australia, 2012. [Google Scholar]
- Australian Bureau of Statistics. Labour Costs; Australian Bureau of Statistics: Canberra, Australia, 2017. [Google Scholar]
- Fair Work Ombudsman. Payment for Annual Leave. Available online: https://www.fairwork.gov.au/leave/annual-leave/payment-for-annual-leave# (accessed on 25 November 2020).
- Australian Institute of Health and Welfare. Health expenditure Australia 2018–19; Australian Institute of Health and Welfare, Ed.; Australian Institute of Health and Welfare: Canberra, Australia, 2020; Volume HWE 80. [Google Scholar]
- Australian Bureau of Statistics. Wage Price Index, Australia. Table 1. Total Hourly Rates of Pay Excluding Bonuses: Sector, Original, Seasonally Adjusted and Trend; Australian Bureau of Statistics: Canberra, Australian, 2021. [Google Scholar]
- TABLES 3 and 4. CPI: Groups, Weighted Average of Eight Capital Cities, Index Numbers and Percentage Changes; Australian Bureau of Statistics: Canberra, Australia, 2022.
- Ananthapavan, J.; Moodie, M.; Milat, A.; Veerman, L.; Whittaker, E.; Carter, R. A cost–benefit analysis framework for preventive health interventions to aid decision-making in Australian governments. Health Res. Policy Syst. 2021, 19, 147. [Google Scholar] [CrossRef]
- Ananthapavan, J.; Nguyen, P.K.; Bowe, S.J.; Sacks, G.; Mantilla Herrera, A.M.; Swinburn, B.; Brown, V.; Sweeney, R.; Lal, A.; Strugnell, C.; et al. Cost-effectiveness of community-based childhood obesity prevention interventions in Australia. Int. J. Obes. 2019, 43, 1102–1112. [Google Scholar] [CrossRef]
- Ananthapavan, J.; Sacks, G.; Brown, V.; Moodie, M.; Nguyen, P.; Veerman, L.; Mantilla Herrera, A.M.; Lal, A.; Peeters, A.; Carter, R. Priority-setting for obesity prevention—The Assessing Cost-Effectiveness of obesity prevention policies in Australia (ACE-Obesity Policy) study. PLoS ONE 2020, 15, e0234804. [Google Scholar] [CrossRef]
- 31010do002_202003 National; State and Territory Population. Australian Bureau of Statistics: Canberra, Australian, 2020.
- Murray, C.J.; Atkinson, C.; Bhalla, K.; Birbeck, G.; Burstein, R.; Chou, D.; Dellavalle, R.; Danaei, G.; Ezzati, M.; Fahimi, A.; et al. The state of US health, 1990-2010: Burden of diseases, injuries, and risk factors. JAMA 2013, 310, 591–608. [Google Scholar] [CrossRef] [Green Version]
- Global Burden of Disease Collaborative Network. Global Burden of Disease Study 2017 (GBD 2017) Disability Weights; Global Burden of Disease Collaborative Network: Washington, DC, USA, 2018. [Google Scholar]
- Vos, T.; Carter, R.; Barendregt, J.; Mihalopoulos, C.; Veerman, L.; Magnus, A.; Cobiac, L.; Bertram, M.; Wallace, A.; ACE-Prevention Team. Assessing Cost-Effectiveness in Prevention (ACE–Prevention): Final Report; University of Queensland and Deakin University: Brisbane, Australia; Melbourne, Australia, 2010. [Google Scholar]
- Nguyen, P.; Ananthapavan, J.; Tan, E.J.; Crosland, P.; Bowe, S.J.; Gao, L.; Dunstan, D.W.; Moodie, M. Modelling the potential health and economic benefits of reducing population sitting time in Australia. Int. J. Behav. Nutr. Phys. Act. 2022, 19, 28. [Google Scholar] [CrossRef]
- Australian Institute of Health and Welfare. Health Expenditure Australia 2014–15; Australian Institute of Health and Welfare: Canberra, Australia, 2016; Volume HWE 67. [Google Scholar]
- Husereau, D.; Drummond, M.; Petrou, S.; Carswell, C.; Moher, D.; Greenberg, D.; Augustovski, F.; Briggs, A.H.; Mauskopf, J.; Loder, E. Consolidated Health Economic Evaluation Reporting Standards (CHEERS) statement. BMJ Br. Med. J. 2013, 346, f1049. [Google Scholar] [CrossRef] [Green Version]
- Ananthapavan, J.; Moodie, M.; Milat, A.J.; Carter, R. Systematic Review to Update ‘Value of a Statistical Life’ Estimates for Australia. Int. J. Environ. Res. Public Health 2021, 18, 6168. [Google Scholar] [CrossRef]
- Gregori, D.; Ballali, S.; Vögele, C.; Galasso, F.; Widhalm, K.; Berchialla, P.; Baldi, I. What Is the Value Given by Consumers to Nutritional Label Information? Results from a Large Investigation in Europe. J. Am. Coll. Nutr. 2015, 34, 120–125. [Google Scholar] [CrossRef] [PubMed]
- Loureiro, M.L.; Gracia, A.; Nayga, R.M., Jr. Do consumers value nutritional labels? Eur. Rev. Agric. Econ. 2006, 33, 249–268. [Google Scholar] [CrossRef]
- Cooper, S.L.; Butcher, L.M.; Scagnelli, S.D.; Lo, J.; Ryan, M.M.; Devine, A.; O’Sullivan, T.A. Australian Consumers Are Willing to Pay for the Health Star Rating Front-of-Pack Nutrition Label. Nutrients 2020, 12, 3876. [Google Scholar] [CrossRef] [PubMed]
- Birot, M. What Is the Average Grocery Bill? Available online: https://www.canstarblue.com.au/groceries/average-grocery-bill/ (accessed on 28 October 2021).
- Blake, M.R.; Backholer, K.; Lancsar, E.; Boelsen-Robinson, T.; Mah, C.; Brimblecombe, J.; Zorbas, C.; Billich, N.; Peeters, A. Investigating business outcomes of healthy food retail strategies: A systematic scoping review. Obes. Rev. 2019, 20, 1384–1399. [Google Scholar] [CrossRef] [PubMed]
- Gupta, A.; Alston, L.; Needham, C.; Robinson, E.; Marshall, J.; Boelsen-Robinson, T.; Blake, M.R.; Huggins, C.E.; Peeters, A. Factors Influencing Implementation, Sustainability and Scalability of Healthy Food Retail Interventions: A Systematic Review of Reviews. Nutrients 2022, 14, 294. [Google Scholar] [CrossRef] [PubMed]
- Houghtaling, B.; Serrano, E.L.; Kraak, V.I.; Harden, S.M.; Davis, G.C.; Misyak, S.A. A systematic review of factors that influence food store owner and manager decision making and ability or willingness to use choice architecture and marketing mix strategies to encourage healthy consumer purchases in the United States, 2005–2017. Int. J. Behav. Nutr. Phys. Act. 2019, 16, 5. [Google Scholar] [CrossRef] [Green Version]
- Blake, M.R.; Sacks, G.; Zorbas, C.; Marshall, J.; Orellana, L.; Brown, A.K.; Moodie, M.; Ni Mhurchu, C.; Ananthapavan, J.; Etilé, F.; et al. The ‘Eat Well @ IGA’ healthy supermarket randomised controlled trial: Process evaluation. Int. J. Behav. Nutr. Phys. Act. 2021, 18, 36. [Google Scholar] [CrossRef]
- George, B.; Harris, A.; Mitchell, A. Cost-effectiveness analysis and the consistency of decision making: Evidence from Pharmaceutical Reimbursement in Australia (1991 to 1996). Pharmacoeconomics 2001, 19, 1103–1109. [Google Scholar] [CrossRef]
- Neumann, P.J.; Sanders, G.D.; Russell, L.B.; Siegel, J.E.; Ganiats, T.G. Cost-Effectiveness in Health and Medicine, 2nd ed.; Oxford University Press: New York, NY, USA, 2017. [Google Scholar]
- Epigear International. Ersatz. Available online: http://www.epigear.com/index_files/ersatz.html (accessed on 3 February 2022).
- Fouad, A.M.; Waheed, A.; Gamal, A.; Amer, S.A.; Abdellah, R.F.; Shebl, F.M. Effect of Chronic Diseases on Work Productivity: A Propensity Score Analysis. J. Occup. Environ. Med. 2017, 59, 480–485. [Google Scholar] [CrossRef]
- Schofield, D.; Shrestha, R.N.; Cunich, M.M.; Tanton, R.; Veerman, L.; Kelly, S.J.; Passey, M.E. Economic costs of chronic disease through lost productive life years (PLYs) among Australians aged 45–64 years from 2015 to 2030: Results from a microsimulation model. BMJ Open 2016, 6, e011151. [Google Scholar] [CrossRef] [Green Version]
- Australian Institute of Health and Welfare. Health Expenditure Australia 2019-2020; Australian Institute of Health and Welfare: Canberra, Australia, 2021; Volume HWE 87. [Google Scholar]
- Tran, H.N.Q.; McMahon, E.; Moodie, M.; Ananthapavan, J. A Systematic Review of Economic Evaluations of Health-Promoting Food Retail-Based Interventions. Int. J. Environ. Res. Public Health 2021, 18, 1356. [Google Scholar] [CrossRef] [PubMed]
- Health Ministers Meeting. National Obesity Strategy 2022–2032. Enabling Australians to Eat Well and be Active. 2022. Available online: https://www.health.gov.au/sites/default/files/documents/2022/03/national-obesity-strategy-2022-2032_0.pdf (accessed on 7 March 2022).
- Department of Premier and Cabinet. Guidelines for Cabinet Submissions; Department of Premier and Cabinet: Sydney, Australia, 2017. [Google Scholar]
- State Government of Victoria. Cabinet Handbook; State Government of Victoria: Victoria, Australia, 2019. [Google Scholar]
- Cubi-Molla, P.; Buxton, M.; Devlin, N. Allocating Public Spending Efficiently: Is There a Need for a Better Mechanism to Inform Decisions in the UK and Elsewhere? Appl. Health Econ. Health Policy 2021, 19, 635–644. [Google Scholar] [CrossRef] [PubMed]
- Mpconsulting. Health Star Rating System Five Year Review Report; Commonwealth of Australia: Canberra, Australia, 2019. [Google Scholar]
- Lenzen, M.; Malik, A.; Li, M.; Fry, J.; Weisz, H.; Pichler, P.-P.; Chaves, L.S.M.; Capon, A.; Pencheon, D. The environmental footprint of health care: A global assessment. Lancet Planet. Health 2020, 4, e271–e279. [Google Scholar] [CrossRef]
- Just Food. UK Grocer Morrisons under Fire over Healthy Food Strategy; Just Food: London, UK, 2021. [Google Scholar]
- Williams, H.; Santillo, E. Tesco Expands Junk Food Pledge after Pressure from Investors. It comes amid calls to help tackle the UK’s obesity crisis. 5 May 2021. Available online: https://www.walesonline.co.uk/whats-on/shopping/tesco-expands-junk-food-pledge-20524597 (accessed on 10 April 2022).
- Food Standards Australia and New Zealand. Australian Branded Food Database. Available online: https://www.foodstandards.gov.au/science/monitoringnutrients/Pages/Branded-food-database.aspx (accessed on 25 March 2022).
- Ball, K.; McNaughton, S.A.; Le, H.N.D.; Abbott, G.; Stephens, L.D.; Crawford, D.A. ShopSmart 4 Health: Results of a randomized controlled trial of a behavioral intervention promoting fruit and vegetable consumption among socioeconomically disadvantaged women. Am. J. Clin. Nutr. 2016, 104, 436–445. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cobiac, L.J.; Vos, T.; Veerman, J.L. Cost-Effectiveness of Interventions to Promote Fruit and Vegetable Consumption. PLoS ONE 2010, 5, e14148. [Google Scholar] [CrossRef] [PubMed]
- Dobes, L.; Leung, J.; Argyrous, G. Social Cost-Benefit Analysis in Australia and New Zealand: The State of Current Practice and What Needs to Be Done; ANU Press: Canberra, Australian, 2016. [Google Scholar]
- Le, H.N.D.; Gold, L.; Abbott, G.; Crawford, D.; McNaughton, S.A.; Mhurchu, C.N.; Pollard, C.; Ball, K. Economic evaluation of price discounts and skill-building strategies on purchase and consumption of healthy food and beverages: The SHELf randomized controlled trial. Soc. Sci. Med. 2016, 159, 83–91. [Google Scholar] [CrossRef] [PubMed]
- Australian Bureau of Statistics. 6302.0 Average Weekly Earnings, Australia. May 2019; TABLE 10H. Average Weekly Earnings, Industry, Australia (Dollars)-Original-Persons, Full Time Adult Total Earnings Canberra: ABS; 2022. Available online: https://www.abs.gov.au/statistics/labour/earnings-and-work-hours/average-weekly-earnings-australia/latest-release (accessed on 25 February 2022).
- Department of Prime Minister and Cabinet. Best Practice Regulation Guidance Note Value of Statistical Life; Department of Prime Minister and Cabinet, Ed.; Commonwealth of Australia: Canberra, Australia, 2021. [Google Scholar]
- Australian Bureau of Statistics. Household and Family Projections, Australia; Australian Bureau of Statistics, Ed.; ABS: Canberra, Australia, 2019. [Google Scholar]
- Lal, A.; Mantilla-Herrera, A.M.; Veerman, L.; Backholer, K.; Sacks, G.; Moodie, M.; Siahpush, M.; Carter, R.; Peeters, A. Modelled health benefits of a sugar-sweetened beverage tax across different socioeconomic groups in Australia: A cost-effectiveness and equity analysis. PLoS Med. 2017, 14, e1002326. [Google Scholar] [CrossRef] [Green Version]
- Chronic Disease Prevention Directorate. Healthy Food and Drink School Principal Survey Report 2019; Western Australian Department of Health, Ed.; Western Australian Department of Health: Canberra, Australia, 2021. [Google Scholar]

| CBA Primary Analysis | CUA Primary Analysis | |
|---|---|---|
| Perspective and Referent Group | Societal, Australian population | Healthcare system |
| Comparator/Base Case | Status quo—no shelf tag intervention | |
| Options for Appraisal | Shelf tag intervention—3-year intervention and duration of effect | |
| Time Horizon | Lifetime account of healthcare costs and health impacts | |
| Discount Rate | 3% (recommended by CBA framework [45]) | 5% (recommended by PBAC [21]) |
| Costs Included | Supermarket industry, government | Government—health sector |
| Benefits Included | HALYs valued using VSLY Healthcare cost-savings Consumer surplus (WTP for HSR) Benefits to supermarkets (assessed qualitatively) | HALYs gained Healthcare cost-savings |
| Decision Rules | NPV/BCR | ICER: AUD per HALY gained |
| Sensitivity Analyses * | Univariate and multivariate sensitivity analyses (see Table 2) | |
| Distributional Impacts and Other Considerations | Equity and distributional impacts and other considerations described (qualitatively) | |
| Reporting | Disaggregate costs and benefits across subgroups (retailers, individuals, government, and various healthcare payers (e.g., state and federal governments, individuals and private health insurers). | Overall findings |
| Cost–Benefit Analysis | Cost–Utility Analysis | |
|---|---|---|
| SA 1: Varied Discount Rate | 0%, 5%, 7%, 10% | 0%, 3.5% |
| SA 2: Lower Duration of Intervention Implementation and Effect | 1 year of intervention duration, 8 weeks of intervention effect (duration of the initial study) | |
| SA 3: Limited Uptake by Supermarket Chains | Only 50% of IGA stores implement the intervention, no implementation in other supermarket chains | |
| SA 4: Exclude Consumer Surplus | Remove consumer surplus benefit | No change |
| SA 5: Shorter Time Horizon | 30 years | No change |
| SA 6: Varied Monetary Valuation of Health Gains | HALY gained: AUD 50,000; AUD 92,114; AUD 329,981 Life years gained: AUD 317,230 | No change |
| SA 7: Specifications of the Second Panel on Cost-Effectiveness in Health and Medicine [65] | No change | Societal perspective—include implementation costs accrued by retailers. 3% discount rate. |
| SA 8: Mandatory Intervention | Cost of passing legislation in each state/territory. Increased implementation of 80% in all major supermarket chain stores. Implementation and monitoring costs and intervention effect for 20 years. Consumer surplus benefit was assumed to last for 3 years. | |
| Cost–Benefit Analysis | Cost–Utility Analysis | |
|---|---|---|
| Population Change in Body Weight (kg) | −1.09 (−2.22; −0.21) | |
| Population Change in BMI (kg/m2) | −0.41 (−0.82; −0.08) | |
| Total HALYs Gained | 50,923 (11,499; 101,399) | 36,930 (7527; 70,817) |
| Total Intervention Costs | AUD 29.8 M (18.5 M; 44.1 M) | AUD 0.7 M (0.4 M; 1.1 M) |
| Government Costs | AUD 0.7 M (0.4 M; 1.1 M) | AUD 0.7 M (0.4 M; 1.1 M) |
| Supermarket Costs | AUD 29.1 M (17.8 M; 43.5 M) | N/A |
| Total Monetary Benefits | AUD 16.8 B (3.9 B; 33.6 B) | N/A |
| Total Healthcare Cost-Savings | AUD 542.5 M (121.6 M; 1.1 B) | AUD 406.5 M (81.5 M; 787.4 M) |
| Consumer Surplus (Information Benefits of HSR) | AUD 139.8 M (8.5 M; 670.4 M) | N/A |
| Value of health gains | AUD 16.2 B (3.6 B; 32.2 B) | N/A |
| Net Costs for CUA * | N/A | − AUD 405.6 M (−786.8 M; −80.6 M) |
| Net Present Value (NPV) | AUD 16.8 B (3.8 B; 33.6 B) | N/A |
| Benefit–Cost Ratio (BCR) | 591 (118; 1278) | N/A |
| Mean Incremental Cost–Effectiveness Ratio (ICER) | N/A | Dominant (Dominant to Dominant) |
| Probability Intervention has Positive NPV/is Cost-Effectiveβ | 99.6% | 99.2% |
| Stakeholder Group | Costs, Mean (95% UI) | Benefits |
|---|---|---|
| Supermarket Industry | Total: AUD 29.1 M (17.8 M; 43.5 M) Design and matching: AUD 5.4 M (2.6 M; 8.9 M) Printing and installation: AUD 10.3 M (5.0 M; 17.8 M) Monitoring: AUD 13.4 M (6.4 M; 23.9 M) | Customer perceptions: The majority of customers exposed to healthy food retail interventions in supermarkets and grocery stores reported positive reactions to the intervention [60]. In the shelf tag study, 58% of surveyed customers who noticed the shelf tags reported that the shelf tags influenced their purchases [19]. Commercial viability: 84% of healthy food retail strategies in supermarkets and grocery stores either had a neutral or positive impact on measures of sales, revenue and profitability [60]. Retailer perspectives: In the shelf tag study, staff were positive about the intervention, and noted there was little work for the retailer. Retailers reported that the intervention was perceived positively by supplier representatives [29]. However, there were also reports that the shelf tags fell off easily [63]. Other potential benefits: Productivity gains from improved health of workforce * [67] See Supplementary Materials, Table S7 for details. |
| Australian Federal Government (Healthcare Sector) | AUD 0 | Healthcare costs-saving: AUD 231.7 M Improved health from reduced chronic illness is predicted to improve productivity of the workforce resulting in increased taxes and reductions in welfare payments [68]. |
| Australian State Governments (Healthcare Sector) | AUD 0.7 M (0.4 M; 1.1 M) | Healthcare costs-saving: AUD 150.3 M |
| Private Health Insurers | AUD 0 | Healthcare costs-saving: AUD 44.5 M |
| Individuals/Households | AUD 0 | Healthcare costs-saving: AUD 79.8 M Health benefits: AUD 16.2 B Consumer surplus (information value of HSR): AUD 139.8 M |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ananthapavan, J.; Sacks, G.; Orellana, L.; Marshall, J.; Robinson, E.; Moodie, M.; Blake, M.; Brown, A.; Carter, R.; Cameron, A.J. Cost–Benefit and Cost–Utility Analyses to Demonstrate the Potential Value-for-Money of Supermarket Shelf Tags Promoting Healthier Packaged Products in Australia. Nutrients 2022, 14, 1919. https://doi.org/10.3390/nu14091919
Ananthapavan J, Sacks G, Orellana L, Marshall J, Robinson E, Moodie M, Blake M, Brown A, Carter R, Cameron AJ. Cost–Benefit and Cost–Utility Analyses to Demonstrate the Potential Value-for-Money of Supermarket Shelf Tags Promoting Healthier Packaged Products in Australia. Nutrients. 2022; 14(9):1919. https://doi.org/10.3390/nu14091919
Chicago/Turabian StyleAnanthapavan, Jaithri, Gary Sacks, Liliana Orellana, Josephine Marshall, Ella Robinson, Marj Moodie, Miranda Blake, Amy Brown, Rob Carter, and Adrian J. Cameron. 2022. "Cost–Benefit and Cost–Utility Analyses to Demonstrate the Potential Value-for-Money of Supermarket Shelf Tags Promoting Healthier Packaged Products in Australia" Nutrients 14, no. 9: 1919. https://doi.org/10.3390/nu14091919
APA StyleAnanthapavan, J., Sacks, G., Orellana, L., Marshall, J., Robinson, E., Moodie, M., Blake, M., Brown, A., Carter, R., & Cameron, A. J. (2022). Cost–Benefit and Cost–Utility Analyses to Demonstrate the Potential Value-for-Money of Supermarket Shelf Tags Promoting Healthier Packaged Products in Australia. Nutrients, 14(9), 1919. https://doi.org/10.3390/nu14091919







