Association between Dysphagia and Frailty in Older Adults: A Systematic Review and Meta-Analysis
Abstract
:1. Introduction
2. Materials and Methods
2.1. Data Sources and Searches
2.2. Study Selection and Data Extraction
2.3. Risk-of Bias Assessment
2.4. Data Synthesis and Analysis
3. Results
3.1. Study Selection and Baseline Characteristics
3.2. Studies with Cross-Sectional Data
3.3. Dysphagia and Incident Frailty in One Longitudinal Study
3.4. Meta-Analysis of Dysphagia and Frailty
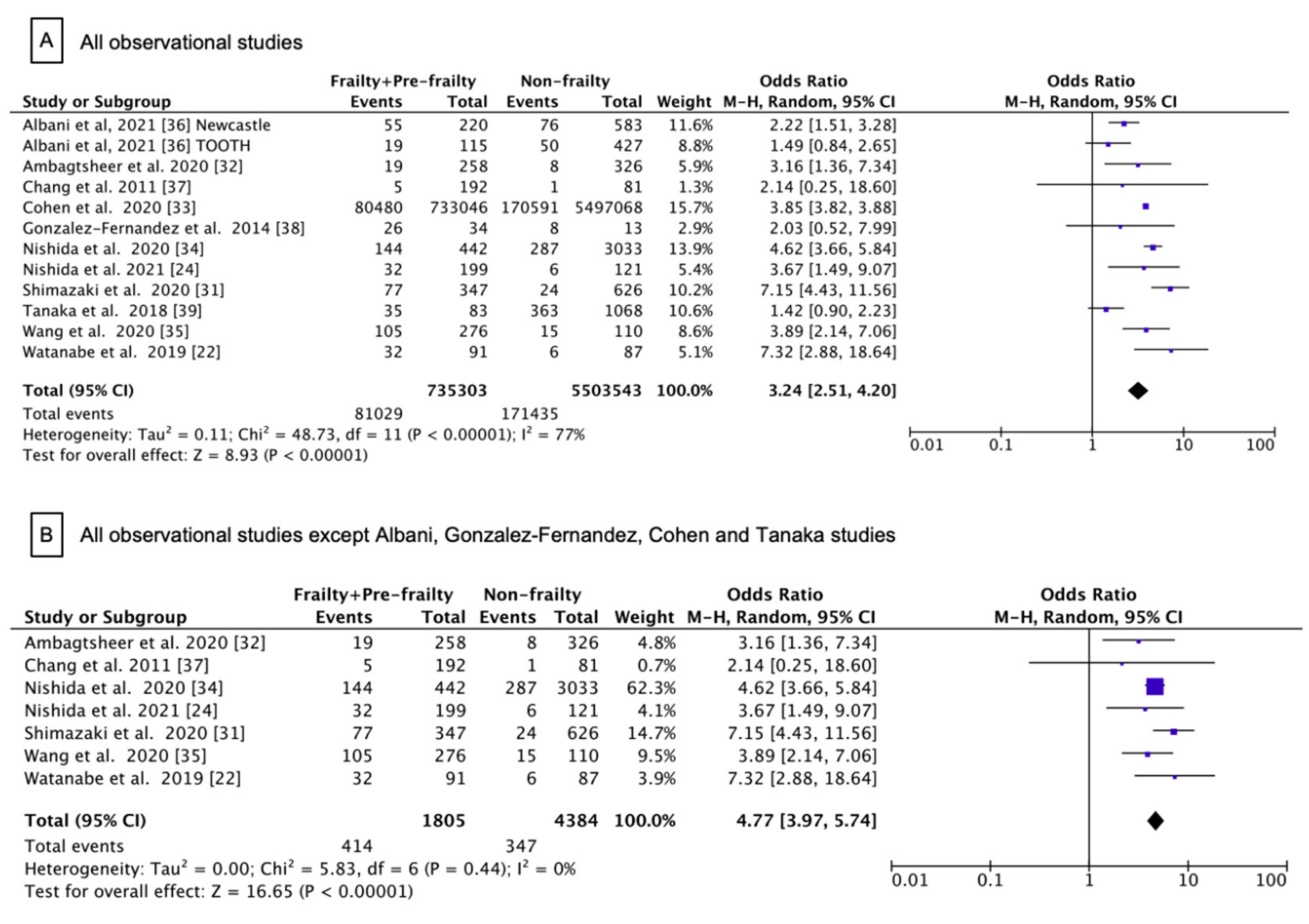
3.5. Subgroup Meta-Analysis
3.6. Assessment of Methodological Quality and Publication Bias
4. Discussion
Strengths and Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Martin-Harris, B. Clinical implications of respiratory-swallowing interactions. Curr. Opin. Otolaryngol. Head Neck Surg. 2008, 16, 194–199. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Valenzano, T.J.; Guida, B.T.; Peladeau-Pigeon, M.; Steele, C.M. Respiratory-Swallow Coordination in Healthy Adults During Drinking of Thin to Extremely Thick Liquids: A Research Note. J. Speech Lang. Hear. Res. 2020, 63, 702–709. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Humbert, I.A.; Fitzgerald, M.E.; McLaren, D.G.; Johnson, S.; Porcaro, E.; Kosmatka, K.; Hind, J.; Robbins, J. Neurophysiology of swallowing: Effects of age and bolus type. Neuroimage 2009, 44, 982–991. [Google Scholar] [CrossRef] [Green Version]
- Teismann, I.K.; Steinstraeter, O.; Schwindt, W.; Ringelstein, E.B.; Pantev, C.; Dziewas, R. Age-related changes in cortical swallowing processing. Neurobiol. Aging 2010, 31, 1044–1050. [Google Scholar] [CrossRef] [PubMed]
- Bahat, G.; Yilmaz, O.; Durmazoglu, S.; Kilic, C.; Tascioglu, C.; Karan, M.A. Association between Dysphagia and Frailty in Community Dwelling Older Adults. J. Nutr. Health Aging 2019, 23, 571–577. [Google Scholar] [CrossRef]
- Muhle, P.; Wirth, R.; Glahn, J.; Dziewas, R. Age-related changes in swallowing. Physiology and pathophysiology. Nervenarzt 2015, 86, 440–451. [Google Scholar] [CrossRef] [PubMed]
- Robbins, J.; Hamilton, J.W.; Lof, G.L.; Kempster, G.B. Oropharyngeal swallowing in normal adults of different ages. Gastroenterology 1992, 103, 823–829. [Google Scholar] [CrossRef]
- Ney, D.M.; Weiss, J.M.; Kind, A.J.; Robbins, J. Senescent swallowing: Impact, strategies, and interventions. Nutr. Clin. Pract. 2009, 24, 395–413. [Google Scholar] [CrossRef] [Green Version]
- Wang, C.M.; Chen, J.Y.; Chuang, C.C.; Tseng, W.C.; Wong, A.M.; Pei, Y.C. Aging-related changes in swallowing, and in the coordination of swallowing and respiration determined by novel non-invasive measurement techniques. Geriatr. Gerontol. Int. 2015, 15, 736–744. [Google Scholar] [CrossRef] [PubMed]
- Sadakane-Sakuramoto, A.; Hasegawa, Y.; Sugahara, K.; Horii, N.; Saito, S.; Nakao, Y.; Nanto, T.; Ono, T.; Domen, K.; Kishimoto, H. Change in Nutritional Status and Dysphagia after Resection of Head and Neck Cancer. Nutrients 2021, 13, 2438. [Google Scholar] [CrossRef] [PubMed]
- Ortega, O.; Martin, A.; Clave, P. Diagnosis and Management of Oropharyngeal Dysphagia Among Older Persons, State of the Art. J. Am. Med. Dir. Assoc. 2017, 18, 576–582. [Google Scholar] [CrossRef] [PubMed]
- Baijens, L.W.; Clave, P.; Cras, P.; Ekberg, O.; Forster, A.; Kolb, G.F.; Leners, J.C.; Masiero, S.; Mateos-Nozal, J.; Ortega, O.; et al. European Society for Swallowing Disorders–European Union Geriatric Medicine Society white paper: Oropharyngeal dysphagia as a geriatric syndrome. Clin. Interv. Aging 2016, 11, 1403–1428. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Clegg, A.; Young, J.; Iliffe, S.; Rikkert, M.O.; Rockwood, K. Frailty in elderly people. Lancet 2013, 381, 752–762. [Google Scholar] [CrossRef] [Green Version]
- Fried, L.P.; Tangen, C.M.; Walston, J.; Newman, A.B.; Hirsch, C.; Gottdiener, J.; Seeman, T.; Tracy, R.; Kop, W.J.; Burke, G.; et al. Frailty in older adults: Evidence for a phenotype. J. Gerontol. A Biol. Sci. Med. Sci. 2001, 56, M146–M156. [Google Scholar] [CrossRef] [PubMed]
- Achem, S.R.; Devault, K.R. Dysphagia in aging. J. Clin. Gastroenterol. 2005, 39, 357–371. [Google Scholar] [CrossRef] [PubMed]
- Ofori-Asenso, R.; Chin, K.L.; Mazidi, M.; Zomer, E.; Ilomaki, J.; Zullo, A.R.; Gasevic, D.; Ademi, Z.; Korhonen, M.J.; LoGiudice, D.; et al. Global Incidence of Frailty and Prefrailty Among Community-Dwelling Older Adults: A Systematic Review and Meta-analysis. JAMA Netw. Open 2019, 2, e198398. [Google Scholar] [CrossRef] [Green Version]
- Nagano, A.; Maeda, K.; Shimizu, A.; Nagami, S.; Takigawa, N.; Ueshima, J.; Suenaga, M. Association of Sarcopenic Dysphagia with Underlying Sarcopenia Following Hip Fracture Surgery in Older Women. Nutrients 2020, 12, 1365. [Google Scholar] [CrossRef]
- Hatcher, V.H.; Galet, C.; Lilienthal, M.; Skeete, D.A.; Romanowski, K.S. Association of Clinical Frailty Scores With Hospital Readmission for Falls After Index Admission for Trauma-Related Injury. JAMA Netw. Open 2019, 2, e1912409. [Google Scholar] [CrossRef] [Green Version]
- Gill, T.M.; Allore, H.G.; Gahbauer, E.A.; Murphy, T.E. Change in disability after hospitalization or restricted activity in older persons. JAMA 2010, 304, 1919–1928. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gill, T.M.; Allore, H.G.; Holford, T.R.; Guo, Z. Hospitalization, restricted activity, and the development of disability among older persons. JAMA 2004, 292, 2115–2124. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Maeda, K.; Ishida, Y.; Nonogaki, T.; Shimizu, A.; Yamanaka, Y.; Matsuyama, R.; Kato, R.; Mori, N. Development and Predictors of Sarcopenic Dysphagia during Hospitalization of Older Adults. Nutrients 2019, 12, 70. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Watanabe, K.; Umegaki, H.; Huang, C.H.; Arakawa Martins, B.; Asai, A.; Kanda, S.; Nomura, H.; Kuzuya, M. Association between dysphagia risk and unplanned hospitalization in older patients receiving home medical care. Geriatr. Gerontol. Int. 2019, 19, 977–981. [Google Scholar] [CrossRef] [PubMed]
- Chang, K.V.; Wu, W.T.; Chen, L.R.; Wang, H.I.; Wang, T.G.; Han, D.S. Suboptimal Tongue Pressure Is Associated with Risk of Malnutrition in Community-Dwelling Older Individuals. Nutrients 2021, 13, 1821. [Google Scholar] [CrossRef] [PubMed]
- Nishida, T.; Yamabe, K.; Honda, S. The Influence of Dysphagia on Nutritional and Frailty Status among Community-Dwelling Older Adults. Nutrients 2021, 13, 512. [Google Scholar] [CrossRef] [PubMed]
- Shimizu, A.; Fujishima, I.; Maeda, K.; Wakabayashi, H.; Nishioka, S.; Ohno, T.; Nomoto, A.; Kayashita, J.; Mori, N.; The Japanese Working Group On Sarcopenic Dysphagia. Nutritional Management Enhances the Recovery of Swallowing Ability in Older Patients with Sarcopenic Dysphagia. Nutrients 2021, 13, 596. [Google Scholar] [CrossRef] [PubMed]
- Coelho-Junior, H.J.; Calvani, R.; Picca, A.; Goncalves, I.O.; Landi, F.; Bernabei, R.; Cesari, M.; Uchida, M.C.; Marzetti, E. Protein-Related Dietary Parameters and Frailty Status in Older Community-Dwellers across Different Frailty Instruments. Nutrients 2020, 12, 508. [Google Scholar] [CrossRef] [Green Version]
- de Sire, A.; Giachero, A.; De Santi, S.; Inglese, K.; Solaro, C. Screening dysphagia risk in 534 older patients undergoing rehabilitation after total joint replacement: A cross-sectional study. Eur. J. Phys. Rehabil. Med. 2021, 57, 131–136. [Google Scholar] [CrossRef]
- de Sire, A.; Ferrillo, M.; Lippi, L.; Agostini, F.; de Sire, R.; Ferrara, P.E.; Raguso, G.; Riso, S.; Roccuzzo, A.; Ronconi, G.; et al. Sarcopenic Dysphagia, Malnutrition, and Oral Frailty in Elderly: A Comprehensive Review. Nutrients 2022, 14, 982. [Google Scholar] [CrossRef]
- Kagaya, H.; Inamoto, Y. Possible Rehabilitation Procedures to Treat Sarcopenic Dysphagia. Nutrients 2022, 14, 778. [Google Scholar] [CrossRef]
- Mateos-Nozal, J.; Sanchez Garcia, E.; Montero-Errasquin, B.; Romero Rodriguez, E.; Cruz-Jentoft, A.J. Short-Term Therapeutic Adherence of Hospitalized Older Patients with Oropharyngeal Dysphagia after an Education Intervention: Analysis of Compliance Rates, Risk Factors and Associated Complications. Nutrients 2022, 14, 413. [Google Scholar] [CrossRef]
- Shimazaki, Y.; Nonoyama, T.; Tsushita, K.; Arai, H.; Matsushita, K.; Uchibori, N. Oral hypofunction and its association with frailty in community-dwelling older people. Geriatr Gerontol Int 2020, 20, 917–926. [Google Scholar] [CrossRef] [PubMed]
- Ambagtsheer, R.C.; Beilby, J.; Seiboth, C.; Dent, E. Prevalence and associations of frailty in residents of Australian aged care facilities: Findings from a retrospective cohort study. Aging Clin Exp Res 2020, 32, 1849–1856. [Google Scholar] [CrossRef] [PubMed]
- Cohen, S.M.; Lekan, D.; Risoli, T., Jr.; Lee, H.J.; Misono, S.; Whitson, H.E.; Raman, S. Association Between Dysphagia and Inpatient Outcomes Across Frailty Level Among Patients >/= 50 Years of Age. Dysphagia 2020, 35, 787–797. [Google Scholar] [CrossRef]
- Nishida, T.; Yamabe, K.; Honda, S. Dysphagia is associated with oral, physical, cognitive and psychological frailty in Japanese community-dwelling elderly persons. Gerodontology 2020, 37, 185–190. [Google Scholar] [CrossRef]
- Wang, T.; Zhao, Y.; Guo, A. Association of swallowing problems with frailty in Chinese hospitalized older patients. Int. J. Nurs. Sci. 2020, 7, 408–412. [Google Scholar] [CrossRef]
- Albani, V.; Nishio, K.; Ito, T.; Kotronia, E.; Moynihan, P.; Robinson, L.; Hanratty, B.; Kingston, A.; Abe, Y.; Takayama, M.; et al. Associations of poor oral health with frailty and physical functioning in the oldest old: Results from two studies in England and Japan. BMC Geriatr. 2021, 21, 187. [Google Scholar] [CrossRef]
- Chang, C.I.; Chan, D.C.; Kuo, K.N.; Hsiung, C.A.; Chen, C.Y. Prevalence and correlates of geriatric frailty in a northern Taiwan community. J. Formos. Med. Assoc. 2011, 110, 247–257. [Google Scholar] [CrossRef] [Green Version]
- Gonzalez-Fernandez, M.; Humbert, I.; Winegrad, H.; Cappola, A.R.; Fried, L.P. Dysphagia in old-old women: Prevalence as determined according to self-report and the 3-ounce water swallowing test. J. Am. Geriatr. Soc. 2014, 62, 716–720. [Google Scholar] [CrossRef] [Green Version]
- Tanaka, T.; Takahashi, K.; Hirano, H.; Kikutani, T.; Watanabe, Y.; Ohara, Y.; Furuya, H.; Tetsuo, T.; Akishita, M.; Iijima, K. Oral Frailty as a Risk Factor for Physical Frailty and Mortality in Community-Dwelling Elderly. J. Gerontol. A Biol. Sci. Med. Sci. 2018, 73, 1661–1667. [Google Scholar] [CrossRef]
- Stroup, D.F.; Berlin, J.A.; Morton, S.C.; Olkin, I.; Williamson, G.D.; Rennie, D.; Moher, D.; Becker, B.J.; Sipe, T.A.; Thacker, S.B. Meta-analysis of observational studies in epidemiology: A proposal for reporting. Meta-analysis Of Observational Studies in Epidemiology (MOOSE) group. JAMA 2000, 283, 2008–2012. [Google Scholar] [CrossRef]
- Clegg, A.; Bates, C.; Young, J.; Ryan, R.; Nichols, L.; Ann Teale, E.; Mohammed, M.A.; Parry, J.; Marshall, T. Development and validation of an electronic frailty index using routine primary care electronic health record data. Age Ageing 2016, 45, 353–360. [Google Scholar] [CrossRef] [Green Version]
- Lekan, D.A.; Wallace, D.C.; McCoy, T.P.; Hu, J.; Silva, S.G.; Whitson, H.E. Frailty Assessment in Hospitalized Older Adults Using the Electronic Health Record. Biol. Res. Nurs. 2017, 19, 213–228. [Google Scholar] [CrossRef]
- Rockwood, K.; Song, X.; MacKnight, C.; Bergman, H.; Hogan, D.B.; McDowell, I.; Mitnitski, A. A global clinical measure of fitness and frailty in elderly people. CMAJ 2005, 173, 489–495. [Google Scholar] [CrossRef] [Green Version]
- Sewo Sampaio, P.Y.; Sampaio, R.A.; Yamada, M.; Arai, H. Systematic review of the Kihon Checklist: Is it a reliable assessment of frailty? Geriatr. Gerontol. Int. 2016, 16, 893–902. [Google Scholar] [CrossRef]
- Wells, G.A.; Shea, B.; O’Connell, D.; Peterson, J.; Welch, V.; Losos, M.; Tugwell, P. The Newcastle-Ottawa Scale (NOS) for Assessing the Quality of Nonrandomised Studies in Meta-Analyses. 2021. Available online: http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp (accessed on 23 April 2022).
- Higgins, J.P.T.; Thomas, J.; Chandler, J.; Cumpston, M.; Li, T.; Page, M.J.; Welch, V.A. Cochrane Handbook for Systematic Reviews of Interventions. In Cochrane Handbook for Systematic Reviews of Interventions, 2nd ed.; Welch, V.A., Ed.; John Wiley & Sons: Chichester, UK, 2019. [Google Scholar]
- Herzog, R.; Alvarez-Pasquin, M.J.; Diaz, C.; Del Barrio, J.L.; Estrada, J.M.; Gil, A. Are healthcare workers’ intentions to vaccinate related to their knowledge, beliefs and attitudes? A systematic review. BMC Public Health 2013, 13, 154. [Google Scholar] [CrossRef] [Green Version]
- Kojima, G.; Avgerinou, C.; Iliffe, S.; Walters, K. Adherence to Mediterranean Diet Reduces Incident Frailty Risk: Systematic Review and Meta-Analysis. J. Am. Geriatr. Soc. 2018, 66, 783–788. [Google Scholar] [CrossRef]
- World Health Organization. Ageing: Overview. 2021. Available online: https://www.who.int/health-topics/ageing#tab=tab_1 (accessed on 23 April 2022).
- United States Census Bureau. Demographic Trends of Global Aging. An Aging World: 2020. Available online: https://mtgis-portal.geo.census.gov/arcgis/apps/MapSeries/index.html?appid=3d832796999042daae7982ff36835e2e (accessed on 23 April 2022).
- World Health Organization. Decade of Healthy Ageing: Baseline Report. 2021. Available online: https://www.who.int/publications/i/item/9789240017900 (accessed on 23 April 2022).
- Centers for Disease Control. International Classification of Diseases, Tenth Revision, Clinical Modification (ICD-10-CM). 2022. Available online: https://www.cdc.gov/nchs/icd/icd10cm.htm (accessed on 23 April 2022).
- World Health Organization. International Classification of Diseases 11th Revision: The global standard for diagnostic health information. 2022. Available online: https://icd.who.int/en (accessed on 23 April 2022).
- Kaiser, M.; Bandinelli, S.; Lunenfeld, B. Frailty and the role of nutrition in older people. A review of the current literature. Acta Biomed. 2010, 81 (Suppl. S1), 37–45. [Google Scholar]
- Xue, Q.L.; Bandeen-Roche, K.; Varadhan, R.; Zhou, J.; Fried, L.P. Initial manifestations of frailty criteria and the development of frailty phenotype in the Women’s Health and Aging Study II. J. Gerontol. A Biol. Sci. Med. Sci. 2008, 63, 984–990. [Google Scholar] [CrossRef] [Green Version]
- de Sire, A.; Invernizzi, M.; Lippi, L.; Curci, C.; Cisari, C.; Iolascon, G. Nutritional supplementation in hip fracture sarcopenic patients: A narrative review. Clin. Cases Miner. Bone Metab. 2019, 16, 27–30. [Google Scholar]
- Saka, B.; Kaya, O.; Ozturk, G.B.; Erten, N.; Karan, M.A. Malnutrition in the elderly and its relationship with other geriatric syndromes. Clin. Nutr. 2010, 29, 745–748. [Google Scholar] [CrossRef]
- He, B.; Ma, Y.; Wang, C.; Jiang, M.; Geng, C.; Chang, X.; Ma, B.; Han, L. Prevalence and Risk Factors for Frailty among Community-Dwelling Older People in China: A Systematic Review and Meta-Analysis. J. Nutr. Health Aging 2019, 23, 442–450. [Google Scholar] [CrossRef] [PubMed]
- Takeuchi, K.; Aida, J.; Ito, K.; Furuta, M.; Yamashita, Y.; Osaka, K. Nutritional status and dysphagia risk among community-dwelling frail older adults. J. Nutr. Health Aging 2014, 18, 352–357. [Google Scholar] [CrossRef]
- Tagliaferri, S.; Lauretani, F.; Pela, G.; Meschi, T.; Maggio, M. The risk of dysphagia is associated with malnutrition and poor functional outcomes in a large population of outpatient older individuals. Clin. Nutr. 2019, 38, 2684–2689. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mareschal, J.; Genton, L.; Collet, T.H.; Graf, C. Nutritional Intervention to Prevent the Functional Decline in Community-Dwelling Older Adults: A Systematic Review. Nutrients 2020, 12, 2820. [Google Scholar] [CrossRef] [PubMed]
- de Sire, A.; Invernizzi, M.; Baricich, A.; Lippi, L.; Ammendolia, A.; Grassi, F.A.; Leigheb, M. Optimization of transdisciplinary management of elderly with femur proximal extremity fracture: A patient-tailored plan from orthopaedics to rehabilitation. World J. Orthop. 2021, 12, 456–466. [Google Scholar] [CrossRef]
- Park, Y.H.; Han, H.R.; Oh, B.M.; Lee, J.; Park, J.A.; Yu, S.J.; Chang, H. Prevalence and associated factors of dysphagia in nursing home residents. Geriatr. Nurs. 2013, 34, 212–217. [Google Scholar] [CrossRef] [PubMed]
- Almirall, J.; Rofes, L.; Serra-Prat, M.; Icart, R.; Palomera, E.; Arreola, V.; Clave, P. Oropharyngeal dysphagia is a risk factor for community-acquired pneumonia in the elderly. Eur. Respir. J. 2013, 41, 923–928. [Google Scholar] [CrossRef] [Green Version]
- Marik, P.E.; Kaplan, D. Aspiration pneumonia and dysphagia in the elderly. Chest 2003, 124, 328–336. [Google Scholar] [CrossRef] [Green Version]
- Croghan, J.E.; Burke, E.M.; Caplan, S.; Denman, S. Pilot study of 12-month outcomes of nursing home patients with aspiration on videofluoroscopy. Dysphagia 1994, 9, 141–146. [Google Scholar] [CrossRef]
- Albert, R.H. Response to a Patient’s Failed Swallowing Study: Decisions Regarding Feeding Tubes and Dysphagia. JAMA Intern. Med. 2016, 176, 1431–1432. [Google Scholar] [CrossRef] [PubMed]
- Finucane, T.E. Questioning Feeding Tubes to Treat Dysphagia. JAMA Intern. Med. 2017, 177, 443. [Google Scholar] [CrossRef] [PubMed]
- Wei, K.; Nyunt, M.S.; Gao, Q.; Wee, S.L.; Yap, K.B.; Ng, T.P. Association of Frailty and Malnutrition With Long-term Functional and Mortality Outcomes Among Community-Dwelling Older Adults: Results From the Singapore Longitudinal Aging Study 1. JAMA Netw. Open. 2018, 1, e180650. [Google Scholar] [CrossRef] [PubMed] [Green Version]

| Source | Country | Participants No. and Dwelling | Study Design | Age, Mean Range, y | Female, N (%) | Dysphagia Ascertainment | Frailty Ascertainment | Baseline Prevalence of Frailty and Pre-Frailty N (%) | Adjustment for Original Investigation |
|---|---|---|---|---|---|---|---|---|---|
| Chang et al. [37], 2011 | Taiwan | 275 Community-Dwelling | Cross-sectional | 71.1 65–79 | 148 (53.8) | Self-reported | FFI | Pre-frailty 161 (58.5) Frailty 31 (11.3) | Age, education status, history of falls in 1 year, pain history, depression, polypharmacy, timed up and go, number of comorbidities, MMSE score, and Barthel Index score |
| Gonzalez-Fernandez et al. [38], 2014 | United States | 47 Community-Dwelling | Cross-sectional | 86.3 85–94 | 47 (100) | Self-reported and 3-Ounce water swallowing test | FFI | Pre-frailty 28 (59.6) Frailty 6 (12.7) | NA |
| Tanaka et al. [39], 2018 (Kashiwa Study) | Japan | 2011 Community-Dwelling | Longitudinal | 73.0 ≥65 | 1017 (50.6) | Self-reported | FFI | Frailty 1151 (57.2) | Age, sex, BMI, chronic conditions, cognitive function, depressive symptoms, living arrangements, yearly income, and current smoking status |
| Bahat et al. [5], 2019 | Turkey | 1138 Community-Dwelling | Cross-sectional | 74.1 ≥60 | 790 (69.4) | EAT-10 | FRAIL scale | Pre-frailty 514 (45.3) Frailty 325 (28.6) | Age, sex, presence of neurodegenerative diseases, number of chronic diseases and drugs, HGS (handgrip strength), UGS (usual gait speed), and nutritional status |
| Watanabe et al. [22], 2019 (ONEHOME) | Japan | 178 Community-Dwelling | Cross-sectional | 80.2 66–90 | 76 (42.7) | DSS | Frailty Index | Frailty 91 (51.1) | Age and sex |
| Ambagtsheer et al. [32], 2020 | Australia | 592 Facility-Dwelling | Cross-sectional | 88.0 (median) ≥75 | 394 (66.6) | Self-reported | Modified 36-Item eFI | Pre-frailty 274 (46.3) Frailty 258 (43.6) | Model 1: age, sex, and facility characteristics (size, rurality) Model 2: Model 1 + 12 ACFI domains Model 3: Model 2 + five most prevalent conditions (arthritis, diabetes, hypertension, osteoporosis, and vision problems) |
| Cohen et al. [33], 2020 (NIS-HCUP-AHRQ) | United States | 6,230,114 Hospitalized | Cross-sectional | 70.1 ≥50 | 3,264,580 (52.4) | ICD-9-CM codes | ACG and FRS | Pre-frailty 1,295,864 (20.8) Frailty 43,611 (0.7) | Age, sex, race, hospital characteristics, geographic region, insurance, smoking status, household income, and admission type |
| Nishida et al. [34], 2020 | Japan | 3475 Community-Dwelling | Cross-sectional | 75.8 ≥65 | 1920 (55.3) | Self-reported | 25-Item Kihon Checklist | Frailty 419 (12.1) | Age, sex, domains of oral function, nutrition, physical function, homebound status, cognitive function, and depressive mood |
| Shimazaki et al. [31], 2020 | Japan | 978 Community-Dwelling | Cross-sectional | M: 73.2 F: 72.9 (median) 65–85 | 510 (52.1) | EAT-10 | 25-Item Kihon Checklist | Pre-frailty 295 (30.3) Frailty 81 (8.3) | Age, sex, BMI, hypertension, and stroke |
| Wang et al. [35], 2020 | China | 386 Hospitalized | Cross-sectional | 74.8 65–93 | 190 (49.2) | 30-mL water swallow test | FFI | Pre-frailty 182 (47.2) Frailty 94 (24.4) | Sex, number of chronic diseases, and history of choking/coughing while drinking |
| Nishida et al. [24], 2021 | Japan | 320 Community-Dwelling | Cross-sectional | 77.3 ≥65 | 268 (83.8) | EAT-10 | FFI | Pre-frailty 154 (48.1) Frailty 45 (14.1) | Age, sex, family structure, and self-rated health |
| Albani et al. [36], 2021 (Newcastle 85+ Study) | England | 853 Community-Dwelling | Cross-sectional | 85.0 >85 | 530 (62.1) | Self-reported | FFI | Pre-frailty 433 (53.9) Frailty 226 (28.1) | Age, sex, BMI, alcohol intake, smoking status, social class, cardiovascular disease, diabetes, hypertension, neuropsychiatric disease, and other health conditions |
| Albani et al. [36], 2021 (TOOTH Study) | Japan | 542 Community-Dwelling | Cross-sectional | 87.0 >85 | 306 (56.5) | Self-reported | FFI | Pre-frailty 339 (62.5) Frailty 120 (22.1) | Age, sex, BMI, alcohol intake, smoking status, social class, cardiovascular disease, diabetes, hypertension, neuropsychiatric disease, and other health conditions |
| Characteristic | Odds of Frailty | Odds of Frailty and Pre-Frailty | ||||
|---|---|---|---|---|---|---|
| Studies, No. | Pooled Odds Ratio [95% CI] | I 2, % | p Value for Subgroup Differences | Studies, No. | Pooled Odds Ratio [95% CI] | |
| Main estimate | 7 | 5.22 [3.96, 6.89] | 22% | 7 | 4.77 [3.97, 5.74] | |
| Study population | 0.44 | |||||
| Community-dwelling | 5 | 5.79 [3.91, 8.58] | 38% | 5 | 5.08 [4.04, 6.39] | |
| Hospitalized | 1 | 5.11 [2.58, 10.13] | - | 1 | 3.89 [2.14, 7.06] | |
| Facility-dwelling | 1 | 3.16 [1.36, 7.34] | - | 1 | 3.16 [1.36, 7.34] | |
| Geographic location | 0.22 | |||||
| US/Australia | 1 | 3.16 [1.36, 7.34] | - | 1 | 3.16 [1.36, 7.34] | |
| Asia | 6 | 5.50 [4.10, 7.38] | 23% | 6 | 4.87 [4.04, 5.89] | |
| Sample size | 0.94 | |||||
| N < 500 | 4 | 5.22 [3.29, 8.29] | 0% | 4 | 4.29 [2.79, 6.59] | |
| N ≥ 500 | 3 | 5.36 [3.07, 9.38] | 69% | 3 | 5.01 [3.50, 7.18] | |
| Mean age | 0.75 | |||||
| 70 ≤ age < 80 | 5 | 4.69 [2.06, 10.69] | 32% | 5 | 4.80 [3.92, 5.87] | |
| Age ≥ 80 | 2 | 5.22 [3.96, 6.89] | 42% | 2 | 4.69 [2.06, 10.69] | |
| Assessment tools for frailty in all study populations | 0.61 | |||||
| FFI | 3 | 5.63 [3.56, 8.89] | 0% | 3 | 3.71 [2.29, 6.03] | |
| Non-FFI | 4 | 5.22 [3.96, 6.89] | 57% | 4 | 5.20 [3.82, 7.07] | |
| Assessment tools for dysphagia in all study populations | 0.44 | |||||
| Self-reported | 3 | 4.53 [3.62, 5.66] | 0% | 3 | 4.46 [3.57, 5.58] | |
| EAT-10 or DSS | 3 | 6.86 [3.74, 12.60] | 41% | 3 | 6.36 [4.32, 9.36] | |
| Water swallow test | 1 | 5.11 [2.58, 10.13] | - | 1 | 3.89 [2.14, 7.06] | |
| Community-dwelling study populations | 5 | 5.79 [3.91, 8.58] | 38% | 5 | 5.08 [4.04, 6.39] | |
| Sample size | ||||||
| N < 500 | 3 | 5.32 [2.85, 9.94] | 0% | 0.70 | 3 | 4.77 [2.56, 8.88] |
| N ≥ 500 | 2 | 6.42 [3.05, 13.51] | 81% | 2 | 5.46 [3.59, 8.32] | |
| Mean age | ||||||
| 70 ≤ age < 80 | 4 | 5.66 [3.51, 9.12] | 49% | 0.63 | 4 | 5.01 [3.80, 6.59] |
| Age ≥ 80 | 1 | 7.32 [2.88, 18.64] | - | 1 | 7.32 [2.88, 18.64] | |
| Assessment tools for frailty in Community-dwelling study populations | 0.37 | |||||
| FFI | 2 | 4.11 [1.77, 9.52] | 0% | 2 | 3.39 [1.47, 7.80] | |
| Non-FFI | 3 | 6.47 [3.74, 11.19] | 65% | 3 | 5.57 [3.97, 7.81] | |
| Assessment tools for dysphagia in Community-dwelling study populations | 0.21 | |||||
| Self-reported | 2 | 4.53 [3.62, 5.66] | 0% | 2 | 4.58 [3.63, 5.78] | |
| EAT-10 or DSS | 3 | 6.86 [3.74, 12.60] | 41% | 3 | 6.36 [4.32, 9.36] | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yang, R.-Y.; Yang, A.-Y.; Chen, Y.-C.; Lee, S.-D.; Lee, S.-H.; Chen, J.-W. Association between Dysphagia and Frailty in Older Adults: A Systematic Review and Meta-Analysis. Nutrients 2022, 14, 1812. https://doi.org/10.3390/nu14091812
Yang R-Y, Yang A-Y, Chen Y-C, Lee S-D, Lee S-H, Chen J-W. Association between Dysphagia and Frailty in Older Adults: A Systematic Review and Meta-Analysis. Nutrients. 2022; 14(9):1812. https://doi.org/10.3390/nu14091812
Chicago/Turabian StyleYang, Ru-Yung, An-Yun Yang, Yong-Chen Chen, Shyh-Dye Lee, Shao-Huai Lee, and Jeng-Wen Chen. 2022. "Association between Dysphagia and Frailty in Older Adults: A Systematic Review and Meta-Analysis" Nutrients 14, no. 9: 1812. https://doi.org/10.3390/nu14091812
APA StyleYang, R.-Y., Yang, A.-Y., Chen, Y.-C., Lee, S.-D., Lee, S.-H., & Chen, J.-W. (2022). Association between Dysphagia and Frailty in Older Adults: A Systematic Review and Meta-Analysis. Nutrients, 14(9), 1812. https://doi.org/10.3390/nu14091812







