The Effect of a Multidisciplinary Lifestyle Intervention on Health Parameters in Children versus Adolescents with Severe Obesity
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design and Population
2.2. Intervention
2.3. Measurements
2.4. Anthropometric Data
2.5. Cardio Metabolic Health Parameters
2.6. Data Analysis
3. Results
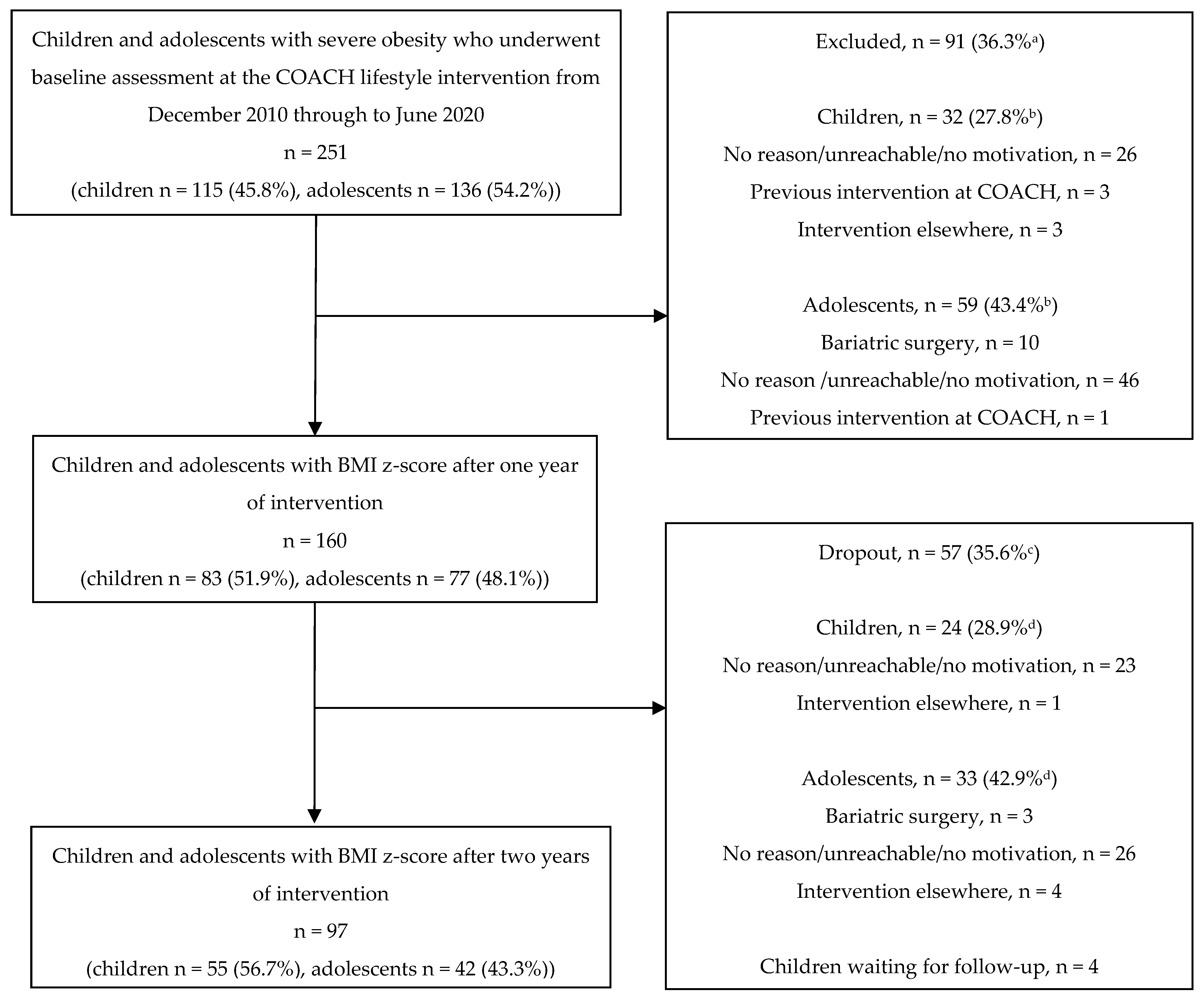
3.1. Program Retention
3.2. Baseline Characteristics
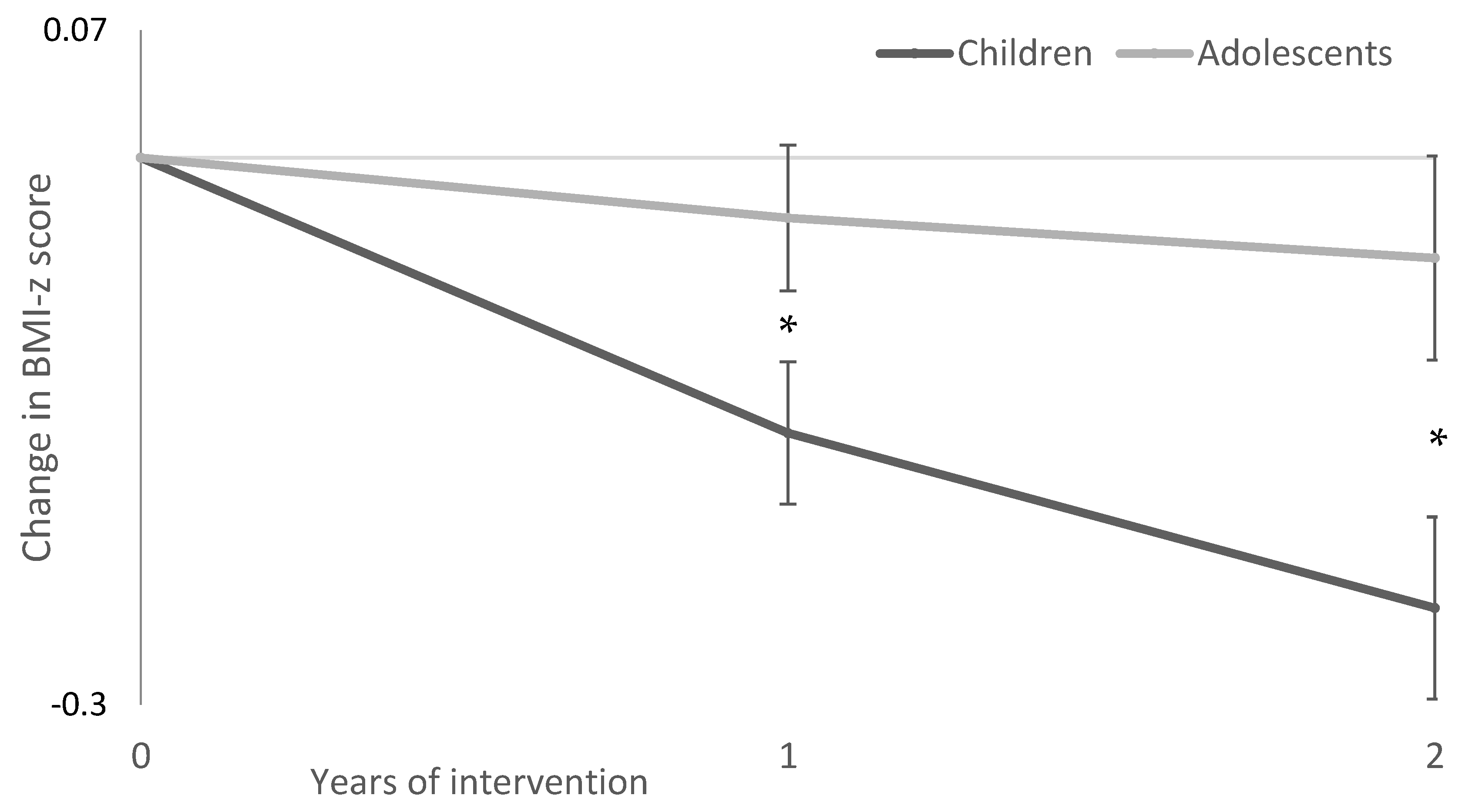
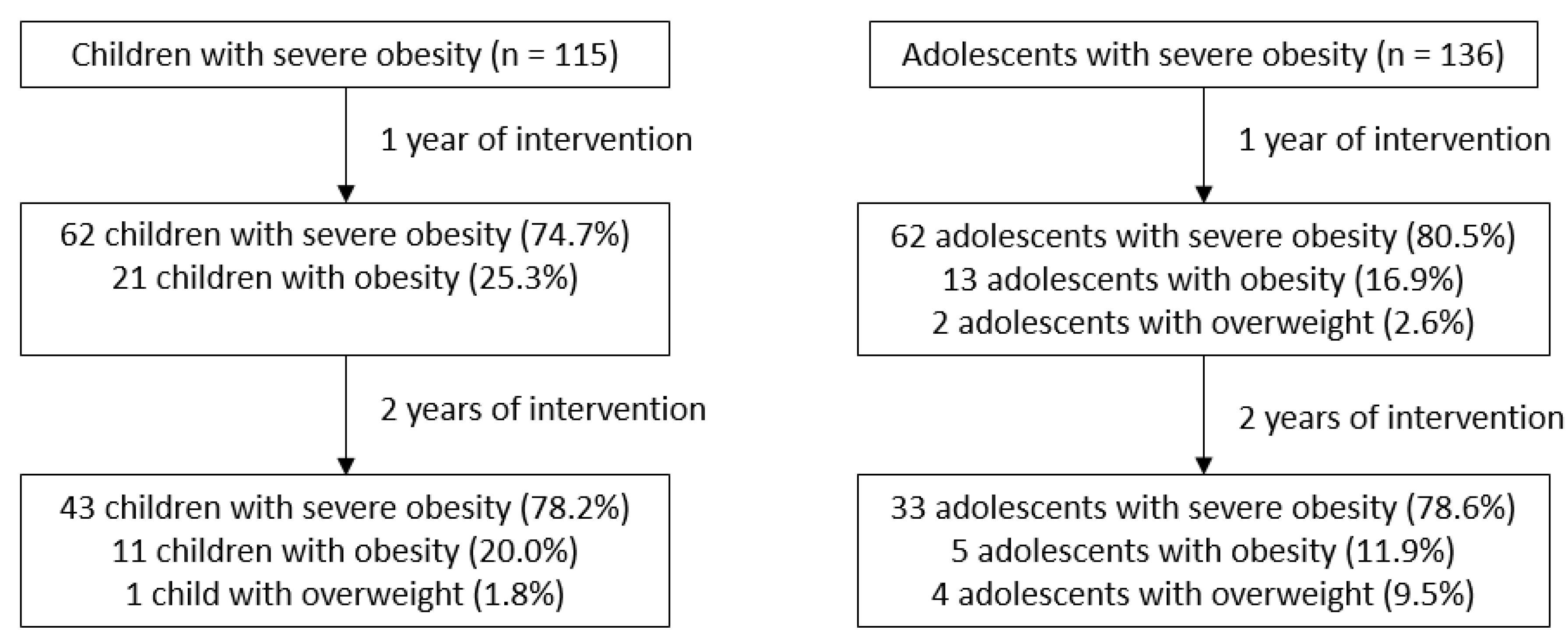
3.3. BMI z-Score
3.4. Cardio Metabolic Health Parameters
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organization. Final Report of the Commission on Ending Childhood Obesity. Available online: https://www.who.int/end-childhood-obesity/publications/echo-plan-executive-summary/en/ (accessed on 15 November 2021).
- NCD Risk Factor Collaboration. Worldwide trends in body-mass index, underweight, overweight, and obesity from 1975 to 2016: A pooled analysis of 2416 population-based measurement studies in 128·9 million children, adolescents, and adults. Lancet 2017, 390, 2627–2642. [Google Scholar] [CrossRef] [Green Version]
- Bass, R.; Eneli, I. Severe childhood obesity: An under-recognised and growing health problem. Postgrad. Med. J. 2015, 91, 639–645. [Google Scholar] [CrossRef]
- Wabitsch, M.; Moss, A.; Kromeyer-Hauschild, K. Unexpected plateauing of childhood obesity rates in developed countries. BMC Med. 2014, 12, 17. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Van Dommelen, P.; Schönbeck, Y.; van Buuren, S.; Hira Sing, R.A. Trends in a life threatening condition: Morbid obesity in dutch, Turkish and Moroccan children in The Netherlands. PLoS ONE 2014, 9, e94299. [Google Scholar] [CrossRef] [PubMed]
- Skelton, J.A.; Cook, S.R.; Auinger, P.; Klein, J.D.; Barlow, S.E. Prevalence and trends of severe obesity among US children and adolescents. Acad. Pediatr. 2009, 9, 322–329. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Van Emmerik, N.M.; Renders, C.M.; van de Veer, M.; van Buuren, S.; van der Baan-Slootweg, O.H.; Kist-van Holthe, J.E.; HiraSing, R.A. High cardiovascular risk in severely obese young children and adolescents. Arch. Dis. Child 2012, 97, 818–821. [Google Scholar] [CrossRef] [Green Version]
- Kelly, A.S.; Barlow, S.E.; Rao, G.; Inge, T.H.; Hayman, L.L.; Steinberger, J.; Urbina, E.M.; Ewing, L.J.; Daniels, S.R. Severe obesity in children and adolescents: Identification, associated health risks, and treatment approaches: A scientific statement from the American Heart Association. Circulation 2013, 128, 1689–1712. [Google Scholar] [CrossRef]
- Twig, G.; Yaniv, G.; Levine, H.; Leiba, A.; Goldberger, N.; Derazne, E.; Shor, D.B.-A.; Tzur, D.; Afek, A.; Shamiss, A.; et al. Body-Mass Index in 2.3 Million Adolescents and Cardiovascular Death in Adulthood. N. Engl. J. Med. 2016, 374, 2430–2440. [Google Scholar] [CrossRef]
- Rijks, J.M.; Plat, J.; Mensink, R.P.; Dorenbos, E.; Buurman, W.A.; Vreugdenhil, A.C. Children With Morbid Obesity Benefit Equally as Children With Overweight and Obesity From an Ongoing Care Program. J. Clin. Endocrinol. Metab. 2015, 100, 3572–3580. [Google Scholar] [CrossRef] [Green Version]
- Knop, C.; Singer, V.; Uysal, Y.; Schaefer, A.; Wolters, B.; Reinehr, T. Extremely obese children respond better than extremely obese adolescents to lifestyle interventions. Pediatr. Obes. 2015, 10, 7–14. [Google Scholar] [CrossRef]
- Danielsson, P.; Kowalski, J.; Ekblom, Ö.; Marcus, C. Response of severely obese children and adolescents to behavioral treatment. Arch. Pediatr. Adolesc. Med. 2012, 166, 1103–1108. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kalarchian, M.A.; Levine, M.D.; Arslanian, S.A.; Ewing, L.J.; Houck, P.R.; Cheng, Y.; Ringham, R.M.; Sheets, C.A.; Marcus, M.D. Family-based treatment of severe pediatric obesity: Randomized, controlled trial. Pediatrics 2009, 124, 1060–1068. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Van der Baan-Slootweg, O.; Benninga, M.A.; Beelen, A.; van der Palen, J.; Tamminga-Smeulders, C.; Tijssen, J.G.; van Aalderen, W.M. Inpatient treatment of children and adolescents with severe obesity in the Netherlands: A randomized clinical trial. JAMA Pediatr. 2014, 168, 807–814. [Google Scholar] [CrossRef] [Green Version]
- Makkes, S.; Renders, C.M.; Bosmans, J.E.; van der Baan-Slootweg, O.H.; Hoekstra, T.; Seidell, J.C. One-year effects of two intensive inpatient treatments for severely obese children and adolescents. BMC Pediatr. 2016, 16, 120. [Google Scholar] [CrossRef] [Green Version]
- Anderson, Y.C.; Wynter, L.E.; O’Sullivan, N.A.; Wild, C.E.; Grant, C.C.; Cave, T.L.; Derraik, J.G.; Hofman, P.L. Two-year outcomes of Whānau Pakari, a multi-disciplinary assessment and intervention for children and adolescents with weight issues: A randomized clinical trial. Pediatr. Obes. 2021, 16, e12693. [Google Scholar] [CrossRef] [PubMed]
- Skodvin, V.A.; Lekhal, S.; Kommedal, K.G.; Benestad, B.; Skjåkødegård, H.F.; Danielsen, Y.S.; Linde, S.R.F.; Roelants, M.; Hertel, J.K.; Hjelmesæth, J.; et al. Lifestyle intervention for children and adolescents with severe obesity—Results after one year. Tidsskr. Nor. Laegeforen. 2020, 140, 9. [Google Scholar] [CrossRef]
- De Goede, I.H.; Branje, S.J.; Meeus, W.H. Developmental changes in adolescents’ perceptions of relationships with their parents. J. Youth Adolesc. 2009, 38, 75–88. [Google Scholar] [CrossRef] [Green Version]
- Danielsson, P.; Svensson, V.; Kowalski, J.; Nyberg, G.; Ekblom, O.; Marcus, C. Importance of age for 3-year continuous behavioral obesity treatment success and dropout rate. Obes. Facts 2012, 5, 34–44. [Google Scholar] [CrossRef]
- Cole, T.J.; Lobstein, T. Extended international (IOTF) body mass index cut-offs for thinness, overweight and obesity. Pediatr. Obes. 2012, 7, 284–294. [Google Scholar] [CrossRef]
- Mead, E.; Brown, T.; Rees, K.; Azevedo, L.B.; Whittaker, V.; Jones, D.; Olajide, J.; Mainardi, G.M.; Corpeleijn, E.; O’Malley, C.; et al. Diet, physical activity and behavioural interventions for the treatment of overweight or obese children from the age of 6 to 11 years. Cochrane Database Syst. Rev. 2017, 6, CD012651. [Google Scholar] [CrossRef] [Green Version]
- Al-Khudairy, L.; Loveman, E.; Colquitt, J.L.; Mead, E.; Johnson, R.E.; Fraser, H.; Olajide, J.; Murphy, M.; Velho, R.M.; O’Malley, C.; et al. Diet, physical activity and behavioural interventions for the treatment of overweight or obese adolescents aged 12 to 17 years. Cochrane Database Syst. Rev. 2017, 6, CD012691. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jindal-Snape, D.; Hannah, E.F.; Cantali, D.; Barlow, W.; MacGillivray, S. Systematic literature review of primary-secondary transitions: International research. Rev. Educ. 2020, 8, 526–566. [Google Scholar] [CrossRef]
- Richtlijnen Goede Voeding 2015. Available online: https://www.gezondheidsraad.nl/documenten/adviezen/2015/11/04/richtlijnen-goede-voeding-2015 (accessed on 20 April 2022).
- Ford, A.L.; Hunt, L.P.; Cooper, A.; Shield, J.P. What reduction in BMI SDS is required in obese adolescents to improve body composition and cardiometabolic health? Arch. Dis. Child. 2010, 95, 256–261. [Google Scholar] [CrossRef] [PubMed]
- Matthews, D.R.; Hosker, J.P.; Rudenski, A.S.; Naylor, B.A.; Treacher, D.F.; Turner, R.C. Homeostasis model assessment: Insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia 1985, 28, 412–419. [Google Scholar] [CrossRef] [Green Version]
- Expert Panel on Integrated Guidelines for Cardiovascular Health and Risk Reduction in Children and Adolescents; National Heart, Lung, and Blood institute. Expert panel on integrated guidelines for cardiovascular health and risk reduction in children and adolescents: Summary report. Pediatrics 2011, 128 (Suppl. S5), S213–S256. [Google Scholar] [CrossRef] [Green Version]
- American Diabetes Association. 2. Classification and Diagnosis of Diabetes: Standards of Medical Care in Diabetes-2020. Diabetes Care 2020, 43 (Suppl. S1), S14–S31. [Google Scholar] [CrossRef] [Green Version]
- Vos, M.B.; Abrams, S.H.; Barlow, S.E.; Caprio, S.; Daniels, S.R.; Kohli, R.; Mouzaki, M.; Sathya, P.; Schwimmer, J.B.; Sundaram, S.S.; et al. NASPGHAN Clinical Practice Guideline for the Diagnosis and Treatment of Nonalcoholic Fatty Liver Disease in Children: Recommendations from the Expert Committee on NAFLD (ECON) and the North American Society of Pediatric Gastroenterology, Hepatology and Nutrition (NASPGHAN). J. Pediatr. Gastroenterol. Nutr. 2017, 64, 319–334. [Google Scholar]
- Persoon Met een WESTERSE Migratieachtergrond. Available online: https://www.cbs.nl/nl-nl/onze-diensten/methoden/begrippen/persoon-met-een-westerse-migratieachtergrond (accessed on 15 November 2021).
- Opleidingsniveau. Available online: https://www.cbs.nl/nl-nl/nieuws/2019/33/verschil-levensverwachting-hoog-en-laagopgeleid-groeit/opleidingsniveau (accessed on 15 November 2021).
- Dimitratos, S.M.; Swartz, J.R.; Laugero, K.D. Pathways of parental influence on adolescent diet and obesity: A psychological stress-focused perspective. Nutr. Rev. 2022, nuac004. [Google Scholar] [CrossRef]
- Ten Velde, G.; Plasqui, G.; Dorenbos, E.; Winkens, B.; Vreugdenhil, A. Objectively measured physical activity and sedentary time in children with overweight, obesity and morbid obesity: A cross-sectional analysis. BMC Public Health 2021, 21, 1558. [Google Scholar] [CrossRef]
| Children n = 83 | Adolescents n = 77 | p Value | |
|---|---|---|---|
| Age (years, ±SD) | 8.3 ± 2.4 | 15.2 ± 1.5 | <0.001 * |
| Gender, no. (%) | |||
| Female | 39 (47.0) | 47 (61.0) | 0.075 |
| Height (m, ±SD) | 1.4 ± 0.2 | 1.7 ± 0.1 | <0.001 * |
| Weight (kg, ±SD) | 56.1 ± 20.5 | 109.4 ± 18.8 | <0.001 * |
| BMI (kg/m2, ±SD) | 28.6 ± 4.6 | 38.9 ± 5.1 | <0.001 * |
| BMI z-score (±SD) | 4.07 ± 0.55 | 3.96 ± 0.40 | 0.139 |
| TC (mmol/L, ±SD) | 4.4 ± 0.8 | 4.4 ± 0.9 | 0.872 |
| HDL (mmol/L, ±SD) | 1.2 ± 0.2 | 1.1 ± 0.3 | 0.021 * |
| LDL (mmol/L, ±SD) | 2.6 ± 0.7 | 2.7 ± 0.7 | 0.546 |
| TG (mmol/L, Q1, Q3) | 1.1 [0.7–1.2] | 1.0 [0.7–1.3] | 0.729 |
| Fasting glucose (mmol/L, ±SD) | 4.3 ± 0.6 | 4.2 ± 0.6 | 0.605 |
| HbA1c (%, ±SD) | 5.3 ± 0.5 | 5.3 ± 0.4 | 0.527 |
| HOMA-IR [Q1, Q3] | 2.6 [1.4–3.7] | 4.0 [2.9–5.5] | <0.001 * |
| ALT (U/l, Q1, Q3) | 26.0 [21.0–32.0] | 22.0 [16.0–36.0] | 0.543 |
| Mother’s BMI (kg/m2, ±SD) | 31.6 ± 6.3 | 31.3 ± 7.0 | 0.843 |
| Father’s BMI (kg/m2, ±SD) | 29.0 ± 4.8 | 30.3 ± 5.1 | 0.158 |
| Ethnicity, no. (%) a | |||
| Dutch | 52 (62.7) | 59 (77.6) | 0.119 |
| Western | 8 (9.6) | 4 (5.3) | |
| Non-Western | 23 (27.7) | 13 (17.1) | |
| Parent’s education, no. (%) a | |||
| Low | 34 (42.5) | 28 (37.3) | 0.795 |
| Middle | 34 (42.5) | 34 (45.3) | |
| High | 12 (15.0) | 13 (17.3) |
| Children | Adolescents | |||
|---|---|---|---|---|
| Baseline—Year 1 Mean ± SD (n) | Baseline—Year 2 Mean ± SD (n) | Baseline—Year 1 Mean ± SD (n) | Baseline—Year 2 Mean ± SD (n) | |
| TC (mmol/L) | −0.1 ± 0.6 (29) | −0.6 ± 0.9 (21) * # | −0.1 ± 0.6 (34) | −0.1 ± 0.8 (15) |
| HDL (mmol/L) | 0.0 ± 0.2 (29) | −0.1 ± 0.3 (21) | 0.0 ± 0.2 (34) | 0.0 ± 0.3 (15) |
| LDL (mmol/L) | −0.1 ± 0.6 (29) | −0.5 ± 0.6 (21) * | −0.1 ± 0.7 (33) | −0.1 ± 0.8 (15) |
| TG (mmol/L) | 0.0 ± 0.4 (29) | −0.3 ± 0.6 (21) | 0.1 ± 0.7 (33) | 0.0 ± 0.6 (15) |
| Fasting glucose (mmol/L) | 0.2 ± 0.6 (27) | −0.1 ± 0.7 (20) | 0.2 ± 0.8 (34) | 0.1 ± 0.9 (15) |
| HbA1c (%) | −0.1 ± 0.4 (27) | −0.1 ± 0.2 (21) * | −0.2 ± 0.3 (34) * | −0.3 ± 0.3 (15) * |
| HOMA-IR | 0.5 ± 2.5 (23) | 0.0 ± 2.5 (15) | 0.5 ± 2.2 (29) | −0.3 ± 1.9 (11) |
| ALT (U/L) | −3.0 [−17.0–3.3] (28) | −6.5 [−27.8–0.8] (21) | 0.0 [−4.0–2.0] (34) | 5.0 [−13.0–22.0] (15) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
van de Pas, K.G.H.; Lubrecht, J.W.; Hesselink, M.L.; Winkens, B.; van Dielen, F.M.H.; Vreugdenhil, A.C.E. The Effect of a Multidisciplinary Lifestyle Intervention on Health Parameters in Children versus Adolescents with Severe Obesity. Nutrients 2022, 14, 1795. https://doi.org/10.3390/nu14091795
van de Pas KGH, Lubrecht JW, Hesselink ML, Winkens B, van Dielen FMH, Vreugdenhil ACE. The Effect of a Multidisciplinary Lifestyle Intervention on Health Parameters in Children versus Adolescents with Severe Obesity. Nutrients. 2022; 14(9):1795. https://doi.org/10.3390/nu14091795
Chicago/Turabian Stylevan de Pas, Kelly G. H., Judith W. Lubrecht, Marijn L. Hesselink, Bjorn Winkens, François M. H. van Dielen, and Anita C. E. Vreugdenhil. 2022. "The Effect of a Multidisciplinary Lifestyle Intervention on Health Parameters in Children versus Adolescents with Severe Obesity" Nutrients 14, no. 9: 1795. https://doi.org/10.3390/nu14091795
APA Stylevan de Pas, K. G. H., Lubrecht, J. W., Hesselink, M. L., Winkens, B., van Dielen, F. M. H., & Vreugdenhil, A. C. E. (2022). The Effect of a Multidisciplinary Lifestyle Intervention on Health Parameters in Children versus Adolescents with Severe Obesity. Nutrients, 14(9), 1795. https://doi.org/10.3390/nu14091795







