Current Practice of Assessing and Monitoring Muscle Strength, Muscle Mass and Muscle Function during Nutritional Care by Dietitians in Switzerland—An Online Survey
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design
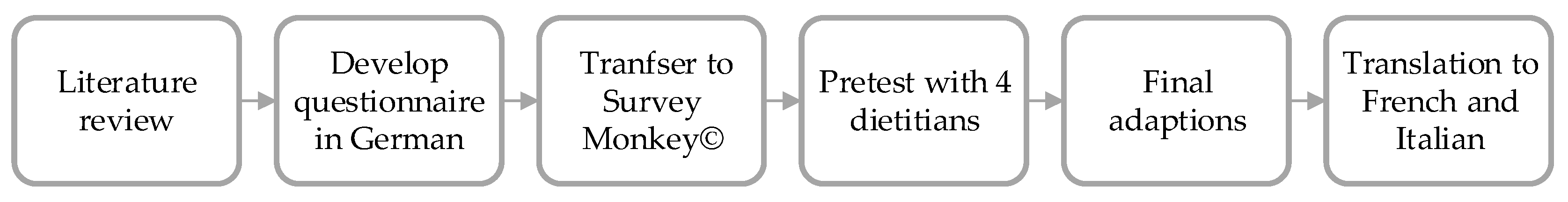
2.2. Development of an Online Questionnaire
2.3. Distribution of the Questionnaire
2.4. Data Analysis
3. Results
3.1. Demographic Data of the Respondents
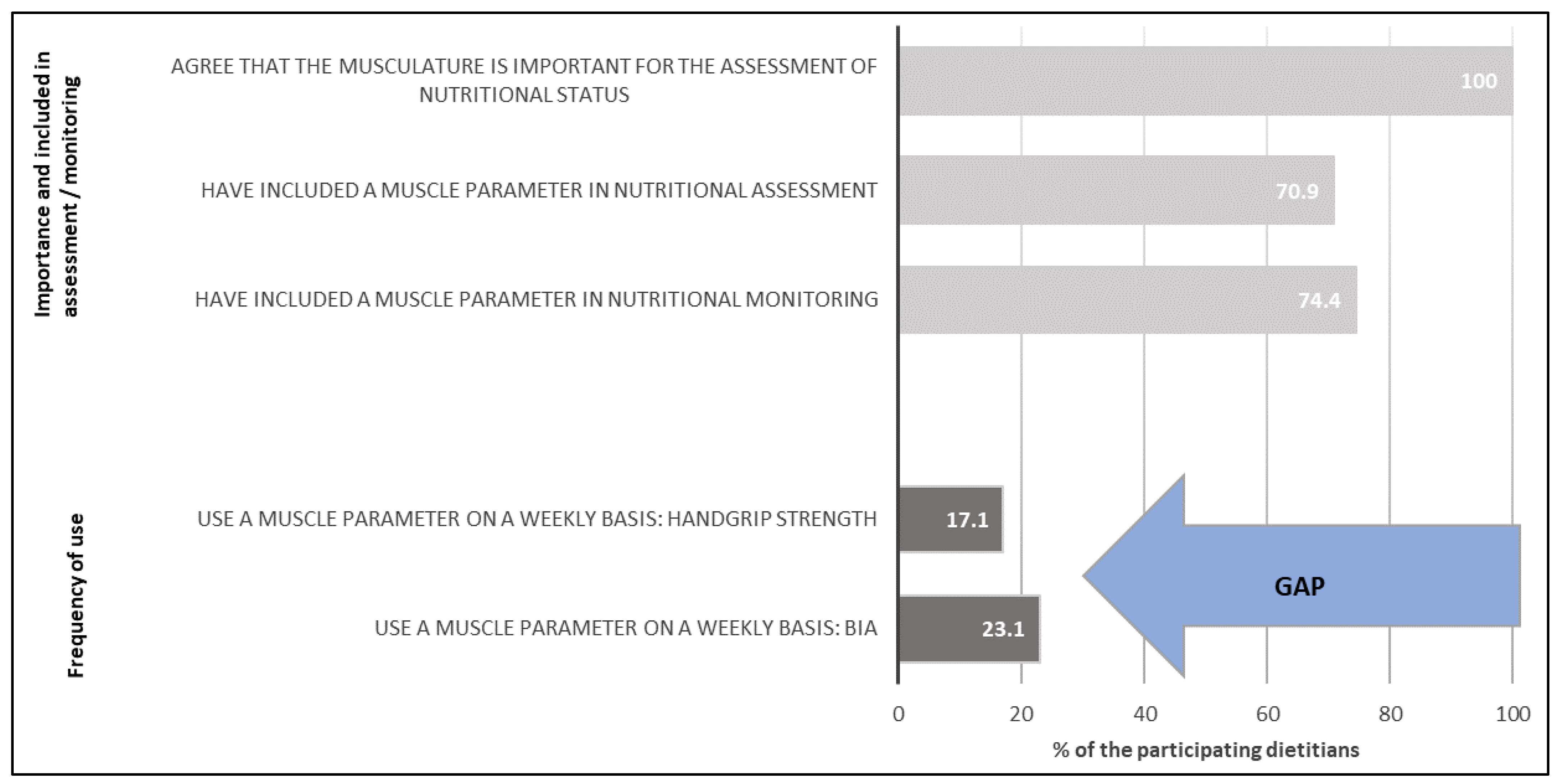
3.2. Perception and Attitudes towards Muscle Parameters
3.3. Application of Muscle Parameters
3.4. Self-Estimation Regarding Knowledge
3.5. Relationships between Demographic Data and the Application of Muscle Parameters
4. Discussion
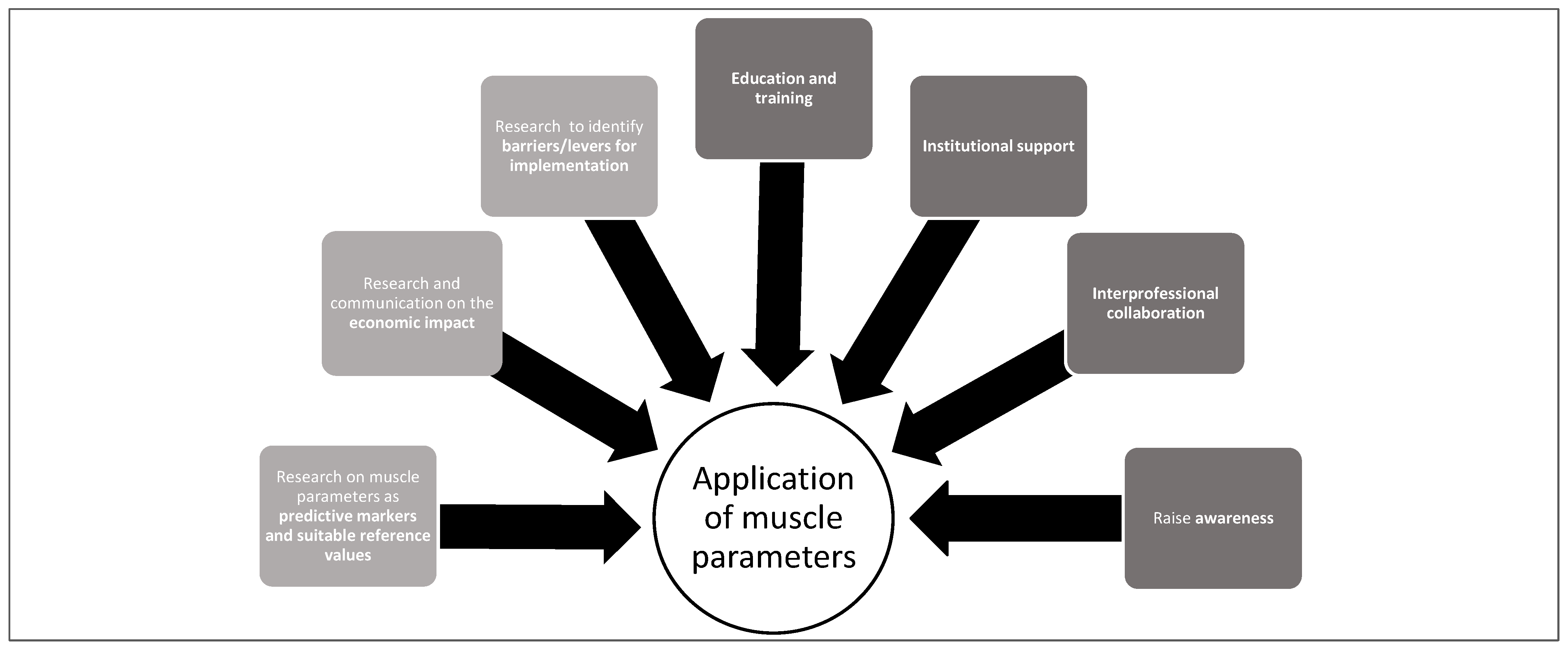
- Raise awareness among healthcare professionals concerning the application of muscle parameters (muscle mass, strength and function) to assess and monitor malnutrition and sarcopenia and initiating appropriate nutritional care to improve patient outcomes;
- Develop and encourage attendance in training on methods and tools for assessing muscle mass, strength and function;
- Strengthen interprofessional collaboration for patient screening, assessment and management among health professionals;
- Institutional support to provide the necessary conditions to promote the application of muscle parameters in daily practice;
- Research and communication on the economic impact of the inclusion of muscle parameters in the scope of practice;
- Research to identify barriers for implementation and steps to overcome these barriers, as well as specific research on muscle parameters as predictive markers and suitable reference values.
Strengths and Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Kaiser, M.J.; Bauer, J.M.; Rämsch, C.; Uter, W.; Guigoz, Y.; Cederholm, T.; Thomas, D.R.; Anthony, P.S.; Charlton, K.E.; Maggio, M.; et al. Frequency of malnutrition in older adults: A multinational perspective using the mini nutritional assessment. J. Am. Ger. Soc. 2010, 58, 1734–1738. [Google Scholar] [CrossRef] [PubMed]
- Felder, S.; Lechtenboehmer, C.; Bally, M.; Fehr, R.; Deiss, M.; Faessler, L.; Kutz, A.; Steiner, D.; Rast, A.C.; Laukemann, S.; et al. Association of nutritional risk and adverse medical outcomes across different medical inpatient populations. Nutrition 2015, 31, 1385–1393. [Google Scholar] [CrossRef] [PubMed]
- Marshall, S.; Bauer, J.; Isenring, E. The consequences of malnutrition following discharge from rehabilitation to the community: A systematic review of current evidence in older adults. J. Hum. Nutr. Diet. 2014, 27, 133–141. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Souza, T.T.; Sturion, C.J.; Faintuch, J. Is the skeleton still in the hospital closet? A review of hospital malnutrition emphasizing health economic aspects. Clin. Nutr. 2015, 34, 1088–1092. [Google Scholar] [CrossRef] [PubMed]
- Gomes, F.; Baumgartner, A.; Bounoure, L.; Bally, M.; Deutz, N.E.; Greenwald, J.L.; Stanga, Z.; Mueller, B.; Schuetz, P. Association of Nutritional Support With Clinical Outcomes Among Medical Inpatients Who Are Malnourished or at Nutritional Risk: An Updated Systematic Review and Meta-analysis. JAMA Netw. Open 2019, 2, e1915138. [Google Scholar] [CrossRef] [Green Version]
- Cederholm, T.; Barazzoni, R.; Austin, P.; Ballmer, P.; Biolo, G.; Bischoff, S.C.; Compher, C.; Correia, I.; Higashiguchi, T.; Holst, M.; et al. ESPEN guidelines on definitions and terminology of clinical nutrition. Clin. Nutr. 2017, 36, 49–64. [Google Scholar] [CrossRef]
- Gümüşsoy, M.; Atmış, V.; Yalçın, A.; Bahşi, R.; Yiğit, S.; Arı, S.; Dokuyan, H.C.; Gözükara, M.G.; Silay, K. Malnutrition-sarcopenia syndrome and all-cause mortality in hospitalized older people. Clin. Nutr. 2021, 40, 5475–5481. [Google Scholar] [CrossRef]
- Xu, J.; Wan, C.S.; Ktoris, K.; Reijnierse, E.M.; Maier, A.B. Sarcopenia Is Associated with Mortality in Adults: A Systematic Review and Meta-Analysis. Gerontology 2022, 68, 361–376. [Google Scholar] [CrossRef]
- Kaluzniak-Szymanowska, A.; Krzyminska-Siemaszko, R.; Deskur-Smielecka, E.; Lewandowicz, M.; Kaczmarek, B.; Wieczorowska-Tobis, K. Malnutrition, sarcopenia, and malnutrition-sarcopenia syndrome in older adults with COPD. Nutrients 2022, 14, 44. [Google Scholar] [CrossRef]
- Argilés, J.M.; Campos, N.; Lopez-Pedrosa, J.M.; Rueda, R.; Rodriguez-Mañas, L. Skeletal Muscle Regulates Metabolism via Interorgan Crosstalk: Roles in Health and Disease. J. Am. Med. Dir. Assoc. 2016, 17, 789–796. [Google Scholar] [CrossRef] [Green Version]
- Drescher, C.; Konishi, M.; Ebner, N.; Springer, J. Loss of muscle mass: Current developments in cachexia and sarcopenia focused on biomarkers and treatment. J. Cachexia Sarcop. Musc. 2015, 6, 303–311. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Puthucheary, Z.A.; Rawal, J.; McPhail, M.; Connolly, B.; Ratnayake, G.; Chan, P.; Hopkinson, N.S.; Phadke, R.; Padhke, R.; Dew, T.; et al. Acute skeletal muscle wasting in critical illness. JAMA 2013, 310, 1591–1600. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wolfe, R.R. The underappreciated role of muscle in health and disease. Am. J. Clin. Nutr. 2006, 84, 475–482. [Google Scholar] [CrossRef] [PubMed]
- Sartori, R.; Romanello, V.; Sandri, M. Mechanisms of muscle atrophy and hypertrophy: Implications in health and disease. Nat. Commun. 2021, 12, 1–12. [Google Scholar] [CrossRef]
- Lengelé, L.; Bruyère, O.; Beaudart, C.; Reginster, J.-Y.; Locquet, M. Impact of Malnutrition Status on Muscle Parameter Changes over a 5-Year Follow-Up of Community-Dwelling Older Adults from the SarcoPhAge Cohort. Nutrients 2021, 13, 407. [Google Scholar] [CrossRef]
- Cruz-Jentoft, A.J.; Bahat, G.; Bauer, J.; Boirie, Y.; Bruyère, O.; Cederholm, T.; Cooper, C.; Landi, F.; Rolland, Y.; Sayer, A.A.; et al. Sarcopenia: Revised European consensus on definition and diagnosis. Age Ageing 2019, 48, 16–31. [Google Scholar] [CrossRef] [Green Version]
- Cederholm, T.; Jensen, G.L.; Correia, M.I.T.D.; Gonzalez, M.C.; Fukushima, R.; Higashiguchi, T.; Baptista, G.; Barazzoni, R.; Blaauw, R.; Coats, A.; et al. GLIM criteria for the diagnosis of malnutrition-A consensus report from the global clinical nutrition community. Clin. Nutr. 2019, 38, 1–9. [Google Scholar] [CrossRef] [Green Version]
- Leong, D.P.; Teo, K.K.; Rangarajan, S.; Lopez-Jaramillo, P.; Avezum, A.; Orlandini, A.; Seron, P.; Ahmed, S.H.; Rosengren, A.; Kelishadi, R.; et al. Prognostic value of grip strength: Findings from the Prospective Urban Rural Epidemiology (PURE) study. Lancet 2015, 386, 266–273. [Google Scholar] [CrossRef]
- McNicholl, T.; Curtis, L.; Dubin, J.A.; Mourtzakis, M.; Nasser, R.; Laporte, M.; Keller, H. Handgrip strength predicts length of stay and quality of life in and out of hospital. Clin. Nutr. 2020, 39, 2501–2509. [Google Scholar] [CrossRef]
- Van Abellan Kan, G.; Rolland, Y.; Andrieu, S.; Bauer, J.; Beauchet, O.; Bonnefoy, M.; Cesari, M.; Donini, L.M.; Gillette Guyonnet, S.; Inzitari, M.; et al. Gait speed at usual pace as a predictor of adverse outcomes in community-dwelling older people an International Academy on Nutrition and Aging (IANA) Task Force. J. Nutr. Health Aging 2009, 13, 881–889. [Google Scholar] [CrossRef]
- Kaegi-Braun, N.; Tribolet, P.; Baumgartner, A.; Fehr, R.; Baechli, V.; Geiser, M.; Deiss, M.; Gomes, F.; Kutz, A.; Hoess, C.; et al. Value of handgrip strength to predict clinical outcomes and therapeutic response in malnourished medical inpatients: Secondary analysis of a randomized controlled trial. Am. J. Clin. Nutr. 2021, 114, 731–740. [Google Scholar] [CrossRef] [PubMed]
- Bohannon, R.W. Muscle strength: Clinical and prognostic value of hand-grip dynamometry. Curr. Opin. Clin. Nutr. Metab. Care 2015, 18, 465–470. [Google Scholar] [CrossRef] [PubMed]
- Norman, K.; Stobäus, N.; Gonzalez, C.M.; Schulzke, J.; Pirlich, M. Hand grip strength: Outcome predictor and marker of nutritional status. Clin. Nutr. 2011, 30, 135–142. [Google Scholar] [CrossRef]
- Matheson, E.M.; Nelson, J.L.; Baggs, G.E.; Luo, M.; Deutz, N.E. Specialized oral nutritional supplement (ONS) improves handgrip strength in hospitalized, malnourished older patients with cardiovascular and pulmonary disease: A randomized clinical trial. Clin. Nutr. 2021, 40, 844–849. [Google Scholar] [CrossRef] [PubMed]
- Swan, W.I.; Vivanti, A.; Hakel-Smith, N.A.; Hotson, B.; Orrevall, Y.; Trostler, N.; Beck Howarter, K.; Papoutsakis, C. Nutrition Care Process and Model Update: Toward Realizing People-Centered Care and Outcomes Management. J. Acad. Nutr. Diet. 2017, 117, 2003–2014. [Google Scholar] [CrossRef]
- Swan, W.I.; Pertel, D.G.; Hotson, B.; Lloyd, L.; Orrevall, Y.; Trostler, N.; Vivanti, A.; Howarter, K.B.; Papoutsakis, C. Nutrition Care Process (NCP) Update Part 2: Developing and Using the NCP Terminology to Demonstrate Efficacy of Nutrition Care and Related Outcomes. J. Acad. Nutr. Diet. 2019, 119, 840–855. [Google Scholar] [CrossRef] [Green Version]
- Almeida, J.; Bascuñana Ambrós, H.; Terrados, N.; Sanz, R. The role of muscle in disease-related malnutrition. Decalogue of Good Practices. Prog. Nutr. 2018, 20, 447–454. [Google Scholar] [CrossRef]
- Dennett, C. Physical exams. Today Diet. 2016, 18, 37–39. [Google Scholar]
- Mareschal, J.; Achamrah, N.; Norman, K.; Genton, L. Clinical Value of Muscle Mass Assessment in Clinical Conditions Associated with Malnutrition. J. Clin. Med. 2019, 8, 1040. [Google Scholar] [CrossRef] [Green Version]
- Esper, D.H. Utilization of nutrition-focused physical assessment in identifying micronutrient deficiencies. Nutr. Clin. Pract. 2015, 30, 194–202. [Google Scholar] [CrossRef]
- Galli, L.; Steiner, N.; Uhlmann, K.; Kurmann, S. Faustschlusskraft: Nützliches Tool–selten angewandt. Schweiz. Z. Ernährungsmedizin 2020, 2020, 24–25. [Google Scholar]
- Stankorb, S.; Rigassio-Radler, D.; Hafiz, K.; Touger-Decker, R. The Professional Practices of Nutrition Focused Physical Examination among Registered Dietitians. J. Am. Diet. Assoc. 2009, 9, A9. [Google Scholar] [CrossRef]
- Mordarski, B.; Hand, R. Patterns in Adult Malnutrition Assessment and Diagnosis by Registered Dietitian Nutritionists: 2014-2017. J. Acad. Nutr. Diet. 2019, 119, 310–322. [Google Scholar] [CrossRef] [PubMed]
- Demeny, D.; Jukic, K.; Dawson, B.; O’Leary, F. Current practices of dietitians in the assessment and management of malnutrition in elderly patients. Nutr. Diet. 2015, 72, 254–260. [Google Scholar] [CrossRef]
- Montero, I.; Léon, O.G. A guide for naming research studies in psychology. Int. J. Clin. Health Psychol. 2007, 7, 847–862. [Google Scholar]
- Mackle, T.J.; Touger-Decker, R.; O’Sullivan Maillet, J.; Holland, B.K. Registered dietitians’ use of physical assessment parameters in professional practice. J. Am. Diet. Assoc. 2003, 103, 1632–1638. [Google Scholar] [CrossRef] [PubMed]
- Mordarski, B. Nutrition-Focused Physical Exam Hands-On Training Workshop. J. Acad. Nutr. Diet. 2016, 116, 868–869. [Google Scholar] [CrossRef]
- Reijnierse, E.M.; de van der Schueren, M.A.E.; Trappenburg, M.C.; Doves, M.; Meskers, C.G.M.; Maier, A.B. Lack of knowledge and availability of diagnostic equipment could hinder the diagnosis of sarcopenia and its management. PLoS ONE 2017, 12, e0185837. [Google Scholar] [CrossRef] [Green Version]
- Abe Bieri, F. Faustschlusskraft als Ernährungstherapeutischer Indikator bei der Behandlung der Mangelernährung: Eine Qualitative Forschungsarbeit. Bachelor’s Thesis, Bern University of Applied Science, Health Division, Bern, Switzerland, 2017, unpublished. [Google Scholar]
- Meyer, F.; Valentini, L. Disease-Related Malnutrition and Sarcopenia as Determinants of Clinical Outcome. Visc. Med. 2019, 35, 282–291. [Google Scholar] [CrossRef]
- Girsemihl, C.; Blumenschein, B.; Rubin, D. Online-Befragung von Ernährungsfachkräften mit klinischem Arbeitsfeld in Deutschland zum Thema Variablen des Ernährungsassessments. Aktuelle Ernährungsmedizin 2021, 46, 160–167. [Google Scholar] [CrossRef]
- Kondrup, J.; Allison, P.; Elia, M.; Vellas, B.; Plauth, M. ESPEN Guidelines for Nutrition Screening 2002. Clin. Nutr. 2003, 22, 415–421. [Google Scholar] [CrossRef]
- Patrick, K.; Goodroe, A.C.; Brech, D. Assessment of Nutrition Status of Adults Using the Nutrition Focused Physical Examination; Ouachita Baptist University: Ouachita, AR, USA, 2018. [Google Scholar]
- Desjardins, S.; Brody, R.; Marcus, A.; Touger-Decker, R. Nutrition Focused Physical Examination Practices of Registered Dietitian Nutritionists That Have Completed an In-Person Nutrition Focused Physical Examination Course. J. Acad. Nutr. Diet. 2016, 116, A87. [Google Scholar] [CrossRef]
- Deutz, N.E.P.; Ashurst, I.; Ballesteros, M.D.; Bear, D.E.; Cruz-Jentoft, A.J.; Genton, L.; Landi, F.; Laviano, A.; Norman, K.; Prado, C.M. The Underappreciated Role of Low Muscle Mass in the Management of Malnutrition. J. Am. Med. Dir. Assoc. 2019, 20, 22–27. [Google Scholar] [CrossRef] [PubMed] [Green Version]
| Demographic Data of Respondents | n | % |
|---|---|---|
| Highest education | ||
| Student (in education) | 2 | 1.7 |
| College of higher education | 12 | 10.3 |
| Bachelor of Science | 88 | 75.2 |
| Master of Science | 14 | 12.0 |
| PhD | 1 | 0.9 |
| Professional environment | ||
| Private practice/freelance | 25 | 21.4 |
| Hospital (mainly inpatient) | 52 | 44.4 |
| Hospital (mainly outpatient) | 16 | 13.7 |
| Rehabilitation clinic | 16 | 13.7 |
| Nursing home | 3 | 2.6 |
| Other | 5 | 4.3 |
| Professional focus 1 | ||
| Malnutrition | 98 | 83.8 |
| Adiposity | 74 | 63.2 |
| Metabolic diseases | 62 | 53.0 |
| Cardiovascular disease | 43 | 36.8 |
| Diseases of the digestive system | 58 | 49.6 |
| Kidney diseases | 23 | 19.7 |
| Allergies/intolerances | 24 | 20.5 |
| Other | 15 | 12.8 |
| Parameter | Response Frequency % | |||||||
|---|---|---|---|---|---|---|---|---|
| Dietitians | Doctors | Nurses | Physio-Therapists | Other Therapists | Nobody | Not Important | No Answer | |
| Body weight | 59.0 | 30.8 | 78.6 | 7.7 | 3.4 | 0.0 | 0.9 | 0.0 |
| BMI | 76.1 | 36.8 | 52.1 | 6.0 | 3.4 | 0.0 | 5.1 | 0.0 |
| Upper arm/calf circumference | 58.1 | 20.5 | 29.1 | 37.6 | 2.6 | 0.9 | 1.7 | 6.8 |
| BIA | 94.0 | 10.3 | 6.8 | 11.1 | 6.0 | 0.0 | 0.9 | 1.7 |
| DXA, MRI, CT | 11.1 | 76.9 | 10.3 | 3.4 | 9.4 | 1.7 | 2.6 | 7.7 |
| Handgrip strength | 71.8 | 15.4 | 18.8 | 70.1 | 19.7 | 0.0 | 0.9 | 0.9 |
| TUG, Chair Stand Test or SPPB | 17.1 | 8.5 | 14.5 | 92.3 | 6.0 | 0.0 | 0.0 | 4.3 |
| Walking test | 11.1 | 8.5 | 12.0 | 95.7 | 6.8 | 0.0 | 0.0 | 1.7 |
| Parameter | Response Frequency % | |||||||
|---|---|---|---|---|---|---|---|---|
| Dietitians | Doctors | Nurses | Physio-Therapists | Other Therapists | Nobody | Not Important | No Answer | |
| Body weight | 98.3 | 72.6 | 37.6 | 13.7 | 2.6 | 0.0 | 0.0 | 0.0 |
| BMI | 97.4 | 65.8 | 27.4 | 11.1 | 2.6 | 0.0 | 0.9 | 0.0 |
| Upper arm/calf circumference | 71.8 | 44.4 | 11.1 | 46.2 | 0.9 | 0.0 | 1.7 | 6.8 |
| BIA | 97.4 | 47.0 | 3.4 | 17.9 | 0.9 | 0.0 | 0.0 | 0.9 |
| DXA, MRI, CT | 32.5 | 87.2 | 6.0 | 7.7 | 3.4 | 0.0 | 0.9 | 7.7 |
| Handgrip strength | 84.6 | 43.6 | 14.5 | 72.6 | 19.7 | 0.0 | 0.0 | 0.9 |
| TUG, Chair Stand Test or SPPB | 39.3 | 45.3 | 15.4 | 91.5 | 9.4 | 0.0 | 0.0 | 4.3 |
| Walking test | 32.5 | 46.2 | 14.5 | 94.9 | 9.4 | 0.0 | 0.0 | 2.6 |
| Parameter | Response Frequency % | |||||
|---|---|---|---|---|---|---|
| Never (<1 x/Year) | Rare (<5 x/Year) | Occasionally (<10 x/Year) | Frequently (>1 x/Month) | Very Often (>1 x/Week) | No Answer | |
| Body weight | 0.0 | 0.0 | 0.0 | 6.8 | 93.2 | 0.0 |
| BMI | 0.0 | 0.9 | 3.4 | 9.4 | 86.3 | 0.0 |
| Upper arm/calf circumference | 59.8 | 19.7 | 9.4 | 6.0 | 3.4 | 1.7 |
| BIA | 17.9 | 13.7 | 17.1 | 28.2 | 23.1 | 0.0 |
| DXA, MRI, CT | 80.3 | 10.3 | 3.4 | 0.9 | 0.0 | 5.1 |
| Handgrip strength | 41.9 | 16.2 | 8.5 | 16.2 | 17.1 | 0.0 |
| TUG, Chair Stand Test or SPPB | 68.4 | 10.3 | 8.5 | 6.8 | 2.6 | 3.4 |
| Walking test | 65.0 | 11.1 | 7.7 | 9.4 | 3.4 | 3.4 |
| Parameter | Response Frequency % | |||||||
|---|---|---|---|---|---|---|---|---|
| Dietitians | Doctor | Nurse | Physio-Therapists | Other Therapists | Nobody | Not Important | No Answer | |
| Body weight | 51.3 | 24.8 | 74.4 | 0.9 | 2.6 | 1.7 | 0.9 | 0.9 |
| BMI | 76.9 | 33.3 | 37.6 | 0.9 | 1.7 | 2.6 | 1.7 | 1.7 |
| Upper arm/calf circumference | 17.9 | 3.4 | 4.3 | 5.1 | 0.0 | 65.8 | 0.9 | 9.4 |
| BIA | 71.8 | 6.0 | 4.3 | 2.6 | 5.1 | 16.2 | 1.7 | 4.3 |
| DXA, MRI, CT | 0.9 | 34.2 | 3.4 | 0.9 | 3.4 | 46.2 | 1.7 | 14.5 |
| Handgrip strength | 35.0 | 2.6 | 1.7 | 22.2 | 21.4 | 32.5 | 1.7 | 7.7 |
| TUG, Chair Stand Test or SPPB | 4.3 | 0.9 | 2.6 | 58.1 | 0.0 | 25.6 | 0.9 | 11.1 |
| Walking test | 2.6 | 0.9 | 1.7 | 60.7 | 0.9 | 26.5 | 0.9 | 8.5 |
| Parameter | Response Frequency % | |||||
|---|---|---|---|---|---|---|
| Very Good Knowledge | Rather Good Knowledge | Neither Good/Nor Bad Knowledge | Rather Poor Knowledge | Poor Knowledge | No Answer | |
| Body weight | 76.9 | 21.4 | 1.7 | 0.0 | 0.0 | 0.0 |
| BMI | 77.8 | 21.4 | 0.9 | 0.0 | 0.0 | 0.0 |
| Upper arm/calf circumference | 6.0 | 21.4 | 28.2 | 33.3 | 10.3 | 0.9 |
| BIA | 29.1 | 45.3 | 13.7 | 8.5 | 2.6 | 0.9 |
| DXA, MRI, CT | 0.0 | 9.4 | 21.4 | 26.5 | 39.3 | 3.4 |
| Handgrip strength | 13.7 | 42.7 | 15.4 | 20.5 | 7.7 | 0.0 |
| TUG, Chair Stand Test or SPPB | 3.4 | 21.4 | 20.5 | 24.8 | 28.2 | 1.7 |
| Walking test | 3.4 | 23.9 | 21.4 | 22.2 | 27.4 | 1.7 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Uhlmann, K.; Schaller, F.; Lehmann, U. Current Practice of Assessing and Monitoring Muscle Strength, Muscle Mass and Muscle Function during Nutritional Care by Dietitians in Switzerland—An Online Survey. Nutrients 2022, 14, 1741. https://doi.org/10.3390/nu14091741
Uhlmann K, Schaller F, Lehmann U. Current Practice of Assessing and Monitoring Muscle Strength, Muscle Mass and Muscle Function during Nutritional Care by Dietitians in Switzerland—An Online Survey. Nutrients. 2022; 14(9):1741. https://doi.org/10.3390/nu14091741
Chicago/Turabian StyleUhlmann, Katja, Fabienne Schaller, and Undine Lehmann. 2022. "Current Practice of Assessing and Monitoring Muscle Strength, Muscle Mass and Muscle Function during Nutritional Care by Dietitians in Switzerland—An Online Survey" Nutrients 14, no. 9: 1741. https://doi.org/10.3390/nu14091741
APA StyleUhlmann, K., Schaller, F., & Lehmann, U. (2022). Current Practice of Assessing and Monitoring Muscle Strength, Muscle Mass and Muscle Function during Nutritional Care by Dietitians in Switzerland—An Online Survey. Nutrients, 14(9), 1741. https://doi.org/10.3390/nu14091741








