Acute Effects of Kawakawa (Piper excelsum) Intake on Postprandial Glycemic and Insulinaemic Response in a Healthy Population
Abstract
1. Introduction
2. Materials and Methods
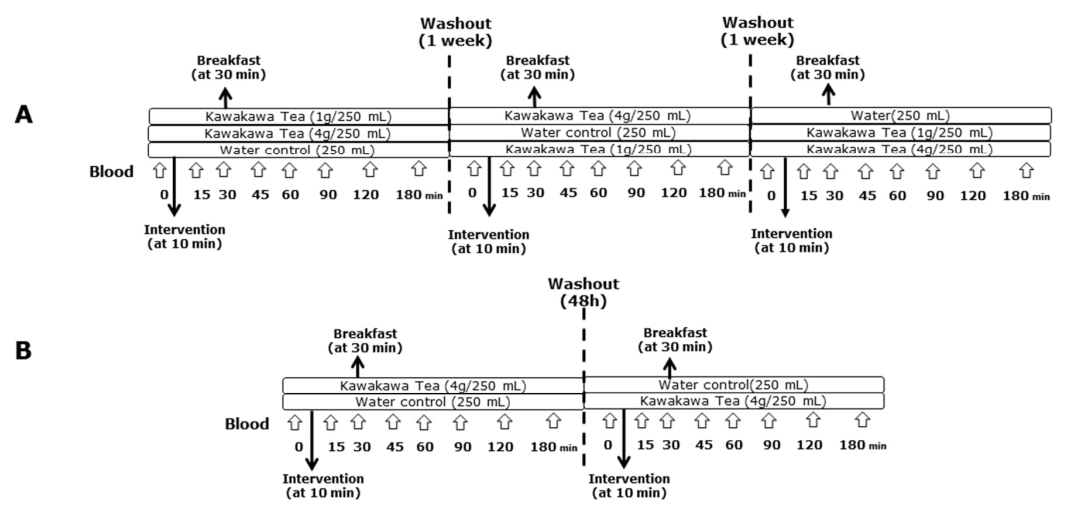
2.1. Study Design and Population
2.2. Intervention Dose and Breakfast
2.3. Sample Collection
2.4. Anthropometric and Biochemical Analysis
2.5. Insulin Sensitivity Assessment
2.6. Metabolomic Analysis
2.7. Statistical Analysis
3. Results
3.1. Participant Characteristics
3.2. Metabolomic Profiling of Kawakawa Tea
3.3. Postprandial Plasma Glucose Response in the BOKA-T and TOAST Studies
3.4. Postprandial Plasma Insulin Response in the BOKA-T and TOAST Studies
3.5. Postprandial Plasma Lipids Response in the BOKA-T and TOAST Studies
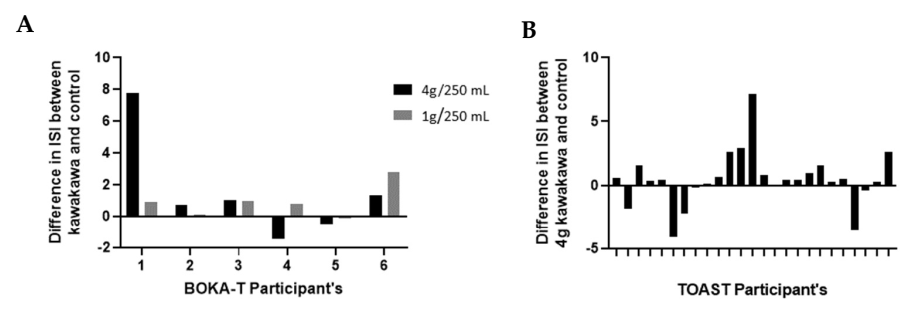
3.6. Insulin Sensitivity Index
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Hodge, S.; Keesing, V.; Wratten, S.D.; Lövei, G.L.; Palmer, J.; Çilgi, T. Herbivore Damage and Leaf Loss in the New Zealand Pepper Tree (“kawakawa”; Macropiper excelsum; Piperaceae). N. Z. J. Ecol. 1998, 22, 173–180. [Google Scholar]
- Briggs, L.H. The Essential Oil of Macropiper excelsum (Kawakawa). J. Soc. Chem. Ind. 1941, 60, 210–212. [Google Scholar] [CrossRef]
- Koia, J.H.; Shepherd, P. The Potential of Anti-Diabetic Rākau Rongoā (Māori Herbal Medicine) to Treat Type 2 Diabetes Mellitus (T2DM) Mate Huka: A Review. Front. Pharmacol. 2020, 11, 935. [Google Scholar] [CrossRef]
- Butts, C.A.; van Klink, J.W.; Joyce, N.I.; Paturi, G.; Hedderley, D.I.; Martell, S.; Harvey, D. Composition and Safety Evaluation of Tea from New Zealand Kawakawa (Piper Excelsum). J. Ethnopharmacol. 2019, 232, 110–118. [Google Scholar] [CrossRef] [PubMed]
- Obst, K.; Lieder, B.; Reichelt, K.V.; Backes, M.; Paetz, S.; Geißler, K.; Krammer, G.; Somoza, V.; Ley, J.P.; Engel, K.H. Sensory Active Piperine Analogues from Macropiper excelsum and Their Effects on Intestinal Nutrient Uptake in Caco-2 Cells. Phytochemistry 2017, 135, 181–190. [Google Scholar] [CrossRef] [PubMed]
- Russell, G.B.; Fenemore, P.G. New Lignans from Leaves of Macropiper excelsum. Phytochemistry 1973, 12, 1799–1803. [Google Scholar] [CrossRef]
- Lei, J.; Burgess, E.J.; Richardson, A.T.B.; Hawkins, B.C.; Baird, S.K.; Smallfield, B.M.; Van Klink, J.W.; Perry, N.B. Cytotoxic Amides from Fruits of Kawakawa, Macropiper excelsum. Planta Med. 2015, 81, 1163–1168. [Google Scholar] [CrossRef] [PubMed]
- Yang, J.P.; He, H.; Lu, Y.H. Four Flavonoid Compounds from Phyllostachys Edulis Leaf Extract Retard the Digestion of Starch and Its Working Mechanisms. J. Agric. Food Chem. 2014, 62, 7760–7770. [Google Scholar] [CrossRef]
- Farsi, E.; Ahmad, M.; Hor, S.Y.; Ahamed, M.B.K.; Yam, M.F.; Asmawi, M.Z. Standardized Extract of Ficus Deltoidea Stimulates Insulin Secretion and Blocks Hepatic Glucose Production by Regulating the Expression of Glucose-Metabolic Genes in Streptozitocin-Induced Diabetic Rats. BMC Complement. Altern. Med. 2014, 14, 220. [Google Scholar] [CrossRef]
- Kesavan, R.; Chandel, S.; Upadhyay, S.; Bendre, R.; Ganugula, R.; Potunuru, U.R.; Giri, H.; Sahu, G.; Kumar, P.U.; Reddy, G.B.; et al. Gentiana Lutea Exerts Anti-Atherosclerotic Effects by Preventing Endothelial Inflammation and Smooth Muscle Cell Migration. Nutr. Metab. Cardiovasc. Dis. 2016, 26, 293–301. [Google Scholar] [CrossRef]
- Martins, C.; Doran, C.; Silva, I.C.; Miranda, C.; Rueff, J.; Rodrigues, A.S. Myristicin from Nutmeg Induces Apoptosis via the Mitochondrial Pathway and down Regulates Genes of the DNA Damage Response Pathways in Human Leukaemia K562 Cells. Chem. Biol. Interact. 2014, 218, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.Y.; Park, W. Anti-Inflammatory Effect of Myristicin on RAW 264.7 Macrophages Stimulated with Polyinosinic-Polycytidylic Acid. Molecules 2011, 16, 7132–7142. [Google Scholar] [CrossRef] [PubMed]
- De León, E.J.; Olmedo, D.A.; Solís, P.N.; Gupta, M.P.; Terencio, M.C. Diayangambin Exerts Immunosuppressive and Anti-Inflammatory Effects in Vitro and in Vivo. Planta Med. 2002, 68, 1128–1131. [Google Scholar] [CrossRef] [PubMed]
- Rahman, N.A.A.; Fazilah, A.; Effarizah, M.E. Toxicity of Nutmeg (Myristicin): A Review. Int. J. Adv. Sci. Eng. Inf. Technol. 2015, 5, 212–215. [Google Scholar] [CrossRef]
- Yang, X.N.; Wang, Y.K.; Zhu, X.; Xiao, X.R.; Dai, M.Y.; Zhang, T.; Qu, Y.; Yang, X.W.; Qin, H.B.; Gonzalez, F.J.; et al. Metabolic Activation of Elemicin Leads to the Inhibition of Stearoyl-CoA Desaturase 1. Chem. Res. Toxicol. 2019, 32, 1965–1976. [Google Scholar] [CrossRef]
- Hui, D.; Zhukovsky, D.S.; Bruera, E. Which Treatment Is Better? Ascertaining Patient Preferences with Crossover Randomized Controlled Trials. J. Pain Symptom Manag. 2015, 49, 625–631. [Google Scholar] [CrossRef] [PubMed]
- University of Sydney Glycemic Index Research and GI News. Available online: https://glycemicindex.com/ (accessed on 8 February 2022).
- Augustin, L.S.A.; Kendall, C.W.C.; Jenkins, D.J.A.; Willett, W.C.; Astrup, A.; Barclay, A.W.; Björck, I.; Brand-Miller, J.C.; Brighenti, F.; Buyken, A.E.; et al. Glycemic Index, Glycemic Load and Glycemic Response: An International Scientific Consensus Summit from the International Carbohydrate Quality Consortium (ICQC). Nutr. Metab. Cardiovasc. Dis. 2015, 25, 795–815. [Google Scholar] [CrossRef]
- Matsuda, M.; DeFronzo, R.A. Insulin Sensitivity Indices Obtained from Oral Glucose Tolerance Testing: Comparison with the Euglycemic Insulin Clamp. Diabetes Care 1999, 22, 1462–1470. [Google Scholar] [CrossRef]
- Ich, C. ICH Topic E 9: Statistical Principles for Clinical Trials; 2006. Available online: https://www.ema.europa.eu/en/ich-e9-statistical-principles-clinical-trials (accessed on 30 March 2022).
- Kwak, S.K.; Kim, J.H. Statistical Data Preparation: Management of Missing Values and Outliers. Korean J. Anesthesiol. 2017, 70, 407–411. [Google Scholar] [CrossRef]
- Pre-Diabetes|Health Navigator NZ. Available online: https://www.healthnavigator.org.nz/health-a-z/d/diabetes-pre-diabetes/ (accessed on 16 February 2022).
- Gao, R.; Duff, W.; Chizen, D.; Zello, G.A.; Chilibeck, P.D. The Effect of a Low Glycemic Index Pulse-Based Diet on Insulin Sensitivity, Insulin Resistance, Bone Resorption and Cardiovascular Risk Factors during Bed Rest. Nutrients 2019, 11, 2012. [Google Scholar] [CrossRef]
- Kernan, W.N.; Inzucchi, S.E.; Viscoli, C.M.; Brass, L.M.; Bravata, D.M.; Shulman, G.I.; McVeety, J.C.; Horwitz, R.I. Pioglitazone Improves Insulin Sensitivity among Nondiabetic Patients with a Recent Transient Ischemic Attack or Ischemic Stroke. Stroke 2003, 34, 1431–1436. [Google Scholar] [CrossRef] [PubMed]
- Takahara, M.; Katakami, N.; Kaneto, H.; Noguchi, M.; Shimomura, I. Distribution of the Matsuda Index in Japanese Healthy Subjects. J. Diabetes Investig. 2013, 4, 369–371. [Google Scholar] [CrossRef] [PubMed]
- Paniagua, J.A. Nutrition, Insulin Resistance and Dysfunctional Adipose Tissue Determine the Different Components of Metabolic Syndrome. World J. Diabetes 2016, 7, 483–514. [Google Scholar] [CrossRef]
- Samuel, V.T.; Shulman, G.I. The Pathogenesis of Insulin Resistance: Integrating Signaling Pathways and Substrate Flux. J. Clin. Investig. 2016, 126, 12–22. [Google Scholar] [CrossRef] [PubMed]
- Folador, P.; Cazarolli, L.H.; Gazola, A.C.; Reginatto, F.H.; Schenkel, E.P.; Silva, F.R.M.B. Potential Insulin Secretagogue Effects of Isovitexin and Swertisin Isolated from Wilbrandia ebracteata Roots in Non-Diabetic Rats. Fitoterapia 2010, 81, 1180–1187. [Google Scholar] [CrossRef]
- Inamdar, S.; Joshi, A.; Malik, S.; Boppana, R.; Ghaskadbi, S. Vitexin Alleviates Non-Alcoholic Fatty Liver Disease by Activating AMPK in High Fat Diet Fed Mice. Biochem. Biophys. Res. Commun. 2019, 519, 106–112. [Google Scholar] [CrossRef] [PubMed]
- Ahrén, B.; Pacini, G. Importance of Quantifying Insulin Secretion in Relation to Insulin Sensitivity to Accurately Assess Beta Cell Function in Clinical Studies. Eur. J. Endocrinol. 2004, 150, 97–104. [Google Scholar] [CrossRef] [PubMed]
- Martin, B.J.; McGlory, C.; MacInnis, M.J.; Allison, M.K.; Phillips, S.M.; Gibala, M.J. Green Tea Extract Does Not Affect Exogenous Glucose Appearance but Reduces Insulinemia with Glucose Ingestion in Exercise Recovery. J. Appl. Physiol. 2016, 121, 1282–1289. [Google Scholar] [CrossRef][Green Version]
- Wang, J.G.; Anderson, R.A.; Graham, G.M.; Chu, M.C.; Sauer, M.V.; Guarnaccia, M.M.; Lobo, R.A. The Effect of Cinnamon Extract on Insulin Resistance Parameters in Polycystic Ovary Syndrome: A Pilot Study. Fertil. Steril. 2007, 88, 240–243. [Google Scholar] [CrossRef]
- Venables, M.C.; Hulston, C.J.; Cox, H.R.; Jeukendrup, A.E. Green Tea Extract Ingestion, Fat Oxidation, and Glucose Tolerance in Healthy Humans. Am. J. Clin. Nutr. 2008, 87, 778–784. [Google Scholar] [CrossRef]
- Roberts, J.D.; Willmott, A.G.B.; Beasley, L.; Boal, M.; Davies, R.; Martin, L.; Chichger, H.; Gautam, L.; Del Coso, J. The Impact of Decaffeinated Green Tea Extract on Fat Oxidation, Body Composition and Cardio-Metabolic Health in Overweight, Recreationally Active Individuals. Nutrients 2021, 13, 764. [Google Scholar] [CrossRef] [PubMed]
- Vergès, B. Pathophysiology of Diabetic Dyslipidaemia: Where Are We? Diabetologia 2015, 58, 886–899. [Google Scholar] [CrossRef] [PubMed]
- Hiyoshi, T.; Fujiwara, M.; Yao, Z. Postprandial Hyperglycemia and Postprandial Hypertriglyceridemia in Type 2 Diabetes. J. Biomed. Res. 2019, 33, 1–16. [Google Scholar]
- Lieder, B.; Zaunschirm, M.; Holik, A.K.; Ley, J.P.; Hans, J.; Krammer, G.E.; Somoza, V. The Alkamide Trans-Pellitorine Targets PPARγ via TRPV1 and TRPA1 to Reduce Lipid Accumulation in Developing 3T3-L1 Adipocytes. Front. Pharmacol. 2017, 8, 316. [Google Scholar] [CrossRef]



| Variables | BOKA-T | TOAST | ||
|---|---|---|---|---|
| Male | Female | Male | All | |
| Total number (n) | 6 | 15 | 14 | 29 |
| Age (year) | 31.2 ± 2.7 | 30.9 ± 1.3 | 32.0 ± 1.6 | 32.0 ± 1.7 |
| Body weight (kg) | 72.0 ± 2.7 | 58.8 ± 1.8 | 68.0 ± 1.8 | 68.2 ± 1.7 |
| BMI (kg/m2) | 23.8 ± 0.8 | 22.3 ± 0.3 | 22.3 ± 0.4 | 22.4 ± 0.3 |
| Systolic BP (mmHg) | 120 ± 4.5 | 109 ± 2.1 | 117 ± 3.1 | 114 ± 2.9 |
| Diastolic BP (mmHg) | 77 ± 4.2 | 73 ± 1.9 | 75 ± 2.0 | 75 ± 2.1 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ramzan, F.; Jayaprakash, R.; Pook, C.; Foster, M.; Miles-Chan, J.L.; Mithen, R. Acute Effects of Kawakawa (Piper excelsum) Intake on Postprandial Glycemic and Insulinaemic Response in a Healthy Population. Nutrients 2022, 14, 1638. https://doi.org/10.3390/nu14081638
Ramzan F, Jayaprakash R, Pook C, Foster M, Miles-Chan JL, Mithen R. Acute Effects of Kawakawa (Piper excelsum) Intake on Postprandial Glycemic and Insulinaemic Response in a Healthy Population. Nutrients. 2022; 14(8):1638. https://doi.org/10.3390/nu14081638
Chicago/Turabian StyleRamzan, Farha, Ramya Jayaprakash, Chris Pook, Meika Foster, Jennifer L. Miles-Chan, and Richard Mithen. 2022. "Acute Effects of Kawakawa (Piper excelsum) Intake on Postprandial Glycemic and Insulinaemic Response in a Healthy Population" Nutrients 14, no. 8: 1638. https://doi.org/10.3390/nu14081638
APA StyleRamzan, F., Jayaprakash, R., Pook, C., Foster, M., Miles-Chan, J. L., & Mithen, R. (2022). Acute Effects of Kawakawa (Piper excelsum) Intake on Postprandial Glycemic and Insulinaemic Response in a Healthy Population. Nutrients, 14(8), 1638. https://doi.org/10.3390/nu14081638






