The Influence of Diet on Ovulation Disorders in Women—A Narrative Review
Abstract
1. Introduction
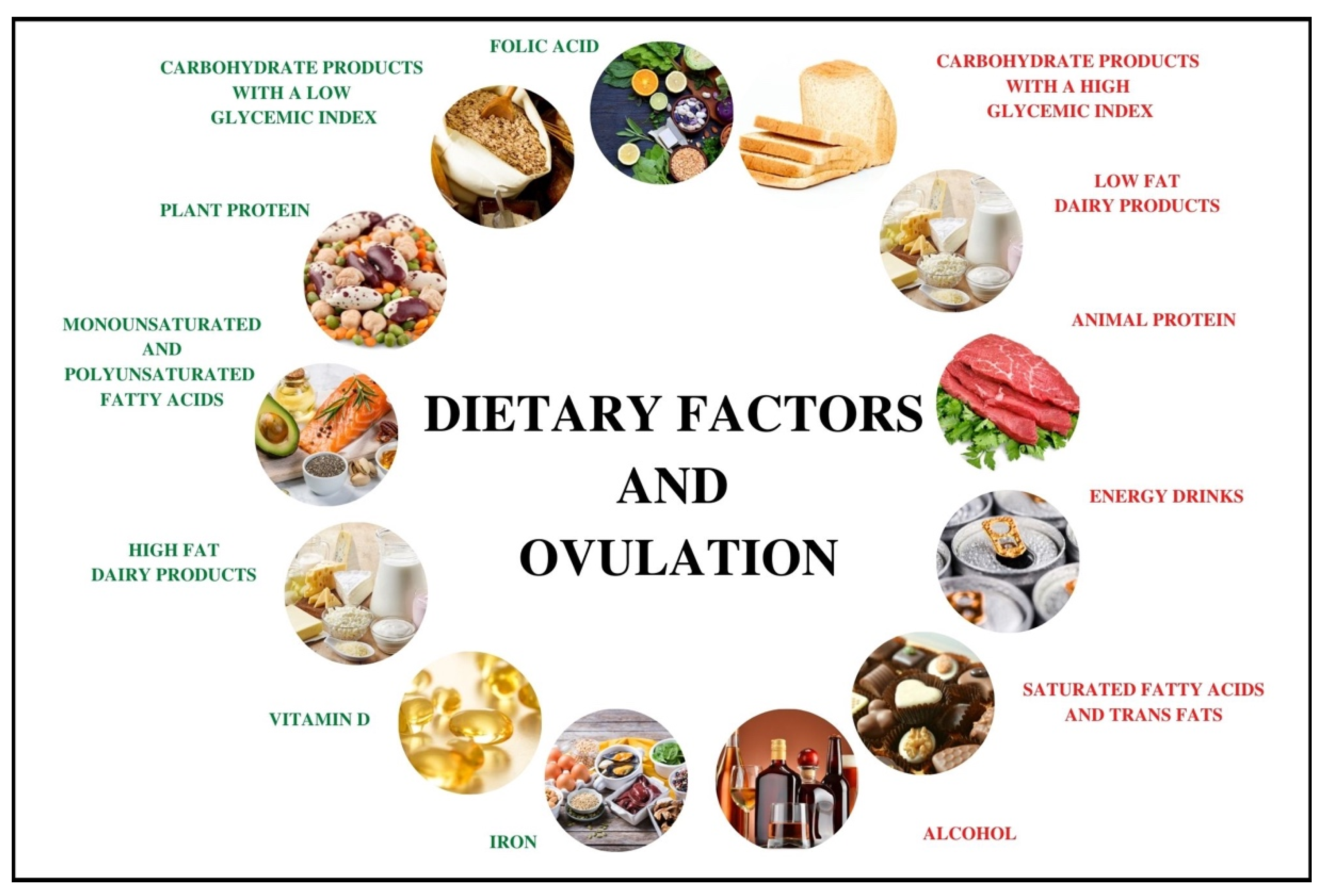
2. Dietary Patterns
3. Carbohydrates and Low Glycemic Index Diet
4. Plant and Animal Protein
5. Unsaturated and Saturated Fatty Acids
6. Alcohol and Caffeine
7. Vitamins and Minerals
8. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Word Health Organization. Infertility. Available online: https://www.who.int/health-topics/infertility#tab=tab_1 (accessed on 20 December 2021).
- Sun, C.; Rong, X.; Cai, Y.; Qiu, S.; Farzaneh, M. Mini review: The FDA-approved prescription drugs that induce ovulation in women with ovulatory problems. Drug Dev. Res. 2020, 81, 815–822. [Google Scholar] [CrossRef] [PubMed]
- Hakimi, O.; Cameron, L.C. Effect of Exercise on Ovulation: A Systematic Review. Sports Med. 2017, 47, 1555–1567. [Google Scholar] [CrossRef] [PubMed]
- Shang, Y.; Zhou, H.; He, R.; Lu, W. Dietary Modification for Reproductive Health in Women with Polycystic Ovary Syndrome: A Systematic Review and Meta-Analysis. Front. Endocrinol. 2021, 12, 735954. [Google Scholar] [CrossRef] [PubMed]
- Franks, S.; Hardy, K. What causes anovulation in polycystic ovary syndrome? Curr. Opin. Endocr. Metab. Res. 2020, 12, 59–65. [Google Scholar] [CrossRef]
- Franks, S.; Stark, J.; Hardy, K. Follicle dynamics and anovulation in polycystic ovary syndrome. Hum. Reprod. Update 2008, 14, 367–378. [Google Scholar] [CrossRef]
- Teede, H.; Misso, M.; Tassone, E.C.; Dewailly, D.; Ng, E.H.; Azziz, R.; Norman, R.J.; Andersen, M.; Franks, S.; Hoeger, K.; et al. Anti-mullerian hormone in PCOS: A review informing international guidelines. Trends Endocrinol. Metabol. 2019, 30, 467–478. [Google Scholar] [CrossRef]
- Chavarro, J.E.; Rich-Edwards, J.W.; Rosner, B.A.; Willett, W.C. Diet and lifestyle in the prevention of ovulatory disorder infertility. Obstet. Gynecol. 2007, 110, 1050–1058. [Google Scholar] [CrossRef]
- Rich-Edwards, J.W.; Spiegelman, D.; Garland, M.; Hertzmark, E.; Hunter, D.J.; Colditz, G.A.; Willett, W.C.; Wand, H.; Manson, J.E. Physical activity, body mass index, and ovulatory disorder infertility. Epidemiology 2002, 13, 184–190. [Google Scholar] [CrossRef]
- Obirikorang, C.; Owiredu, W.K.B.A.; Adu-Afram, S.; Acheampong, E.; Asamoah, E.A.; Antwi-Boasiakoh, E.K.; Owiredu, E.W. Assessing the variability and predictability of adipokines (adiponectin, leptin, resistin and their ratios) in non-obese and obese women with anovulatory polycystic ovary syndrome. BMC Res. Notes 2019, 12, 513–521. [Google Scholar] [CrossRef]
- Sylvia, K.E.; Lorenz, T.K.; Heiman, J.R.; Demas, G.E. Physiological predictors of leptin vary during menses and ovulation in healthy women. Reprod. Biol. 2018, 18, 132–136. [Google Scholar] [CrossRef]
- Ahrens, K.; Mumford, S.L.; Schliep, K.C.; Kissell, K.A.; Perkins, N.J.; Wactawski-Wende, J.; Schisterman, E.F. Serum leptin levels and reproductive function during the menstrual cycle. Am. J. Obstet. Gynecol. 2014, 210, 248-e1. [Google Scholar] [CrossRef] [PubMed]
- Boyd, M.; Ziegler, J. Polycystic Ovary Syndrome, Fertility, Diet, and Lifestyle Modifications: A Review of the Current Evidence. Top. Clin. Nutr. 2019, 34, 14–30. [Google Scholar] [CrossRef]
- McGrice, M.; Porter, J. The Effect of Low Carbohydrate Diets on Fertility Hormones and Outcomes in Overweight and Obese Women: A Systematic Review. Nutrients 2017, 9, 204. [Google Scholar] [CrossRef] [PubMed]
- Azziz, R.; Carmina, E.; Chen, Z.; Dunaif, A.; Laven, J.S.; Legro, R.S.; Lizneva, D.; Natterson-Horowtiz, B.; Teede, H.J.; Yildiz, B.O. Polycystic ovary syndrome. Nat. Rev. Dis. Prim. 2016, 2, 16057. [Google Scholar] [CrossRef] [PubMed]
- Barbe, A.; Bongrani, A.; Mellouk, N.; Estienne, A.; Kurowska, P.; Grandhaye, J.; Elfassy, Y.; Levy, R.; Rak, A.; Froment, P.; et al. Mechanisms of Adiponectin Action in Fertility: An Overview from Gametogenesis to Gestation in Humans and Animal Models in Normal and Pathological Conditions. Int. J. Mol. Sci. 2019, 20, 1526. [Google Scholar] [CrossRef]
- Skoracka, K.; Ratajczak, A.E.; Rychter, A.M.; Dobrowolska, A.; Krela-Kaźmierczak, I. Female Fertility and the Nutritional Approach: The Most Essential Aspects. Adv. Nutr. 2021, 12, 2372–2386. [Google Scholar] [CrossRef]
- Fontana, R.; Della Torre, S. The Deep Correlation between Energy Metabolism and Reproduction: A View on the Effects of Nutrition for Women Fertility. Nutrients 2016, 8, 87. [Google Scholar] [CrossRef]
- Sandhu, J.K.; Waqar, A.; Jain, A.; Joseph, C.; Srivastava, K.; Ochuba, O.; Alkayyali, T.; Ruo, S.W.; Poudel, S. Oxidative Stress in Polycystic Ovarian Syndrome and the Effect of Antioxidant N-Acetylcysteine on Ovulation and Pregnancy Rate. Cureus 2021, 13, e17887. [Google Scholar] [CrossRef]
- Lorenz, T.K.; Worthman, C.M.; Vitzthum, V.J. Links among inflammation, sexual activity and ovulation: Evolutionary trade-offs and clinical implications. Evol. Med. Public Health 2015, 1, 304–324. [Google Scholar] [CrossRef]
- Noormohammadi, M.; Eslamian, G.; Malek, S.; Shoaibinobarian, N.; Mirmohammadali, S.N. The association between fertility diet score and polycystic ovary syndrome: A Case-Control study. Health Care Women Int. 2022, 43, 70–84. [Google Scholar] [CrossRef]
- Barger, M.K. Maternal nutrition and perinatal outcomes. J. Midwifery Womens Health 2010, 55, 502–511. [Google Scholar] [CrossRef] [PubMed]
- Toledo, E.; Lopez-del Burgo, C.; Ruiz-Zambrana, A.; Donazar, M.; Navarro-Blasco, I.; Martínez-González, M.A.; de Irala, J. Dietary patterns and difficulty conceiving: A nested case-control study. Fertil. Steril. 2011, 96, 1149–1153. [Google Scholar] [CrossRef] [PubMed]
- Fatima, Q.; Amin, S.; Kawa, I.A.; Jeelani, H.; Manzoor, S.; Rizvi, S.M.; Rashid, F. Evaluation of antioxidant defense markers in relation to hormonal and insulin parameters in women with polycystic ovary syndrome (PCOS): A case-control study. Diabetes Metab. Syndr. 2019, 13, 1957–1961. [Google Scholar] [CrossRef] [PubMed]
- Velez, L.M.; Seldin, M.; Motta, A.B. Inflammation and reproductive function in women with polycystic ovary syndrome. Biol. Reprod. 2021, 104, 1205–1217. [Google Scholar] [CrossRef] [PubMed]
- Zabaleta, M.E. Mediterranean Diet: Woman Fertility and Pregnancy. Med. J. Nutr. Metab. 2020, 13, 101–111. [Google Scholar] [CrossRef]
- Carlos, S.; De La Fuente-Arrillaga, C.; Bes-Rastrollo, M.; Razquin, C.; Rico-Campà, A.; Martínez-González, M.A.; Ruiz-Canela, M. Mediterranean Diet and Health Outcomes in the SUN Cohort. Nutrients 2018, 10, 439. [Google Scholar] [CrossRef]
- Hajishafiee, M.; Ghiasvand, R.; Feizi, A.; Askari, G. Dietary patterns and Ovulatory infertility: A case-control study. J. Nutr. Sci. Diet. 2017, 3, 1–10. [Google Scholar]
- Silvestris, E.; Lovero, D.; Palmirotta, R. Nutrition and Female Fertility: An Interdependent Correlation. Front. Endocrinol. 2019, 10, 346. [Google Scholar] [CrossRef]
- Noli, S.A.; Ricci, E.; Cipriani, S.; Ferrari, S.; Castiglioni, M.; La Vecchia, I.; Somigliana, E.; Parazzini, F. Dietary Carbohydrate Intake, Dietary Glycemic Load and Outcomes of In Vitro Fertilization: Findings from an Observational Italian Cohort Study. Nutrients 2020, 12, 1568. [Google Scholar] [CrossRef]
- Barrea, L.; Marzullo, P.; Muscogiuri, G.; Di Somma, C.; Scacchi, M.; Orio, F.; Aimaretti, G.; Colao, A.; Savastano, S. Source and amount of carbohydrate in the diet and inflammation in women with polycystic ovary syndrome. Nutr. Res. Rev. 2018, 31, 291–301. [Google Scholar] [CrossRef]
- Chavarro, J.E.; Rich-Edwards, J.W.; Rosner, B.A.; Willett, W.C. A prospective study of dietary carbohydrate quantity and quality in relation to risk of ovulatory infertility. Eur. J. Clin. Nutr. 2009, 63, 78–86. [Google Scholar] [CrossRef] [PubMed]
- Palomba, S.; Falbo, A.; Giallauria, F.; Russo, T.; Rocca, M.; Tolino, A.; Zullo, F.; Orio, F. Six weeks of structured exercise training and hypocaloric diet increases the probability of ovulation after clomiphene citrate in overweight and obese patients with polycystic ovary syndrome: A randomized controlled trial. Hum. Reprod. 2010, 11, 2783–2791. [Google Scholar] [CrossRef] [PubMed]
- Caprio, M.; Infante, M.; Moriconi, E.; Armani, A.; Fabbri, A.; Mantovani, G.; Mariani, S.; Lubrano, C.; Poggiogalle, E.; Migliaccio, S.; et al. Cardiovascular Endocrinology Club of the Italian Society of Endocrinology. Very-low-calorie ketogenic diet (VLCKD) in the management of metabolic diseases: Systematic review and consensus statement from the Italian Society of Endocrinology (SIE). J. Endocrinol. Investig. 2019, 42, 1365–1386. [Google Scholar] [CrossRef] [PubMed]
- Mavropoulos, J.C.; Yancy, W.S.; Hepburn, J.; Westman, E.C. The effects of a low-carbohydrate, ketogenic diet on the polycystic ovary syndrome: A pilot study. Nutr. Metab. 2005, 16, 35–40. [Google Scholar] [CrossRef]
- Gaskins, A.J.; Mumford, S.L.; Zhang, C.; Wactawski-Wende, J.; Hovey, K.M.; Whitcomb, B.W.; Howards, P.P.; Perkins, N.J.; Yeung, E.; Schisterman, E.F. Effect of daily fiber intake on reproductive function: The BioCycle Study. Am. J. Clin. Nutr. 2009, 90, 1061–1069. [Google Scholar]
- Chiu, Y.H.; Chavarro, J.E.; Souter, I. Diet and female fertility: Doctor, what should I eat? Fertil. Steril. 2018, 110, 560–569. [Google Scholar] [CrossRef]
- He, F.F.; Li, Y.M. Role of gut microbiota in the development of insulin resistance and the mechanism underlying polycystic ovary syndrome: A review. J. Ovarian Res. 2020, 13, 73–86. [Google Scholar] [CrossRef]
- Kazemi, M.; Hadi, A.; Pierson, R.A.; Lujan, M.E.; Zello, G.A.; Chilibeck, P.D. Effects of Dietary Glycemic Index and Glycemic Load on Cardiometabolic and Reproductive Profiles in Women with Polycystic Ovary Syndrome: A Systematic Review and Meta-analysis of Randomized Controlled Trials. Adv. Nutr. 2021, 12, 161–178. [Google Scholar] [CrossRef]
- Sordia-Hernández, L.H.; Ancer Rodríguez, P.; Saldivar Rodriguez, D.; Trejo Guzman, S.; Servín Zenteno, E.S.; Guerrero González, G.; Ibarra Patiño, R. Effect of a low glycemic diet in patients with polycystic ovary syndrome and anovulation—A randomized controlled trial. Clin. Exp. Obstet. Gynecol. 2016, 43, 555–559. [Google Scholar] [CrossRef]
- Kandaraki, E.A.; Chatzigeorgiou, A.; Papageorgiou, E.; Piperi, C.; Adamopoulos, C.; Papavassiliou, A.G.; Koutsilieris, M.; Diamanti-Kandarakis, E. Advanced glycation end products interfere in luteinizing hormone and follicle stimulating hormone signaling in human granulosa KGN cells. Exp. Biol. Med. 2018, 243, 29–33. [Google Scholar] [CrossRef]
- Mouanness, M.; Merhi, Z. Impact of Dietary Advanced Glycation End Products on Female Reproduction: Review of Potential Mechanistic Pathways. Nutrients 2022, 14, 966. [Google Scholar] [CrossRef] [PubMed]
- Górna, I.; Więckowska, B.; Przysławski, J.; Szymanowski, K. Effect of increased protein intake on the risk of female infertility. Pol. Arch. Med. Wewn. 2016, 126, 198–200. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Chavarro, J.E.; Rich-Edwards, J.W.; Rosner, B.A.; Willett, W.C. Protein intake and ovulatory infertility. Am. J. Obstet. Gynecol. 2008, 198, 210–222. [Google Scholar] [CrossRef] [PubMed]
- Zhang, B.; Zhou, W.; Shi, Y.; Zhang, J.; Cui, L.; Chen, Z.-J. Lifestyle and environmental contributions to ovulatory dysfunction in women of polycystic ovary syndrome. BMC Endocr. Disord. 2020, 20, 19–26. [Google Scholar] [CrossRef]
- Libera, J.; Iłowiecka, K.; Stasiak, D. Consumption of processed red meat and its impact on human health: A review. Int. J. Food Sci. 2021, 56, 6115–6123. [Google Scholar] [CrossRef]
- Holmes, M.; Pollak, M.N.; Willett, W.C.; Hankinson, S.E. Dietary correlates of plasma insulin-like growth factor I and insulin-like growth factor binding protein 3 concentrations. Cancer Epidemiol. Biomark. Prev. 2002, 9, 852–861. [Google Scholar]
- Gaskins, A.J.; Chavarro, J.E. Diet and fertility: A review. Am. J. Obstet. Gynecol. 2018, 218, 379–389. [Google Scholar] [CrossRef]
- Kim, K.; Wactawski-Wende, J.; Michels, K.A.; Plowden, T.C.; Chaljub, E.N.; Sjaarda, L.A.; Mumford, S.L. Dairy Food Intake Is Associated with Reproductive Hormones and Sporadic Anovulation among Healthy Premenopausal Women. J. Nutr. 2017, 147, 218–226. [Google Scholar] [CrossRef]
- Greenlee, A.R.; Arbuckle, T.E.; Chyou, P.H. Risk factors for female infertility in an agricultural region. Epidemiology 2003, 14, 429–436. [Google Scholar] [CrossRef]
- Wise, L.A.; Wesselink, A.K.; Mikkelsen, E.M.; Cueto, H.; Hahn, K.A.; Rothman, K.J.; Tucker, K.L.; Sorensen, H.T.; Hatch, E.E. Dietary fat intake and fecundability in 2 preconception cohort studies. Am. J. Epidemiol. 2017, 105, 100–110. [Google Scholar] [CrossRef]
- Chavarro, J.E.; Rich-Edwards, J.W.; Rosner, B.; Willett, W.C. A prospective study of dairy foods intake and anovulatory infertility. Hum. Reprod. 2007, 22, 1340–1347. [Google Scholar] [CrossRef] [PubMed]
- Chavarro, J.E.; Rich-Edwards, J.W.; Rosner, B.A.; Willett, W.C. Dietary fatty acid intakes and the risk of ovulatory infertility. Am. J. Clin. Nutr. 2007, 85, 231–237. [Google Scholar] [CrossRef] [PubMed]
- Mumford, S.L.; Chavarro, J.E.; Zhang, C.; Perkins, N.J.; Sjaarda, L.A.; Pollack, A.Z.; Schliep, K.C.; Michels, K.A.; Zarek, S.M.; Plowden, T.C.; et al. Dietary fat intake and reproductive hormone concentrations and ovulation in regularly menstruating women. Am. J. Clin. Nutr. 2016, 103, 868–877. [Google Scholar] [CrossRef]
- Hohos, N.M.; Skaznik-Wikiel, M.E. High-Fat Diet and Female Fertility. Endocrinology 2017, 158, 2407–2419. [Google Scholar] [CrossRef]
- Bauer, J.L.; Kuhn, K.; Bradford, A.P.; Al-Safi, Z.A.; Harris, M.A.; Eckel, R.H.; Robledo, C.Y.; Malkhasyan, A.; Johnson, J.; Gee, N.R.; et al. Reduction in FSH Throughout the Menstrual Cycle After Omega-3 Fatty Acid Supplementation in Young Normal Weight but not Obese Women. Reprod. Sci. 2019, 26, 1025–1033. [Google Scholar] [CrossRef] [PubMed]
- Zarezadeh, R.; Mehdizadeh, A.; Leroy, J.L.M.R.; Nouri, M.; Fayezi, S.; Darabi, M. Action mechanisms of n-3 polyunsaturated fatty acids on the oocyte maturation and developmental competence: Potential advantages and disadvantages. J. Cell Physiol. 2019, 234, 1016–1029. [Google Scholar] [CrossRef]
- Mumford, S.L.; Browne, R.W.; Kim, K.; Nichols, C.; Wilcox, B.; Silver, R.M.; Connell, M.T.; Holland, T.L.; Kuhr, D.L.; Omosigho, U.R.; et al. Preconception Plasma Phospholipid Fatty Acids and Fecundability. J. Clin. Endocrinol. Metab. 2018, 103, 4501–4510. [Google Scholar] [CrossRef]
- Çekici, H.; Akdevelioğlu, Y. The association between trans fatty acids, infertility and fetal life: A review. Hum. Fertil. 2019, 22, 154–163. [Google Scholar] [CrossRef]
- Ghaffarzad, A.; Amani, R.; Darabi, M.; Ghaffarzad, A.; Sadaghiani, M.M.; Cheraghian, B. Correlation of Erythrocyte Trans Fatty Acids with Ovulatory Disorder Infertility in Polycystic Ovarian Syndrome. ABCmed 2014, 2, 8–19. [Google Scholar]
- Chavarro, J.E.; Rich-Edwards, J.W.; Rosner, B.A.; Willett, W.C. Caffeinated and alcoholic beverage intake in relation to ovulatory disorder infertility. Epidemiology 2009, 20, 374–381. [Google Scholar] [CrossRef]
- Lyngsø, J.; Ramlau-Hansen, C.H.; Bay, B.; Ingerslev, H.J.; Hulman, A.; Kesmodel, U.S. Association between coffee or caffeine consumption and fecundity and fertility: A systematic review and dose-response meta-analysis. Clin. Epidemiol. 2017, 9, 699–719. [Google Scholar] [CrossRef] [PubMed]
- Soylu, L.I.; Jensen, A.; Juul, K.E.; Kesmodel, U.S.; Frederiksen, K.; Kjaer, S.K.; Hargreave, M. Coffee, tea and caffeine consumption and risk of primary infertility in women: A Danish cohort study. Acta Obstet. Gynecol. Scand. 2018, 97, 570–576. [Google Scholar] [CrossRef] [PubMed]
- Bu, F.L.; Feng, X.; Yang, X.Y.; Ren, J.; Cao, H.J. Relationship between caffeine intake and infertility: A systematic review of controlled clinical studies. BMC Womens Health 2020, 20, 125–134. [Google Scholar] [CrossRef] [PubMed]
- Rossi, B.V.; Abusief, M.; Missmer, S.A. Modifiable Risk Factors and Infertility: What are the Connections? Am. J. Lifestyle Med. 2014, 10, 220–231. [Google Scholar] [CrossRef]
- Collins, G.G.; Rossi, B.V. The impact of lifestyle modifications, diet, and vitamin supplementation on natural fertility. Fertil. Res. Pract. 2015, 1, 11–21. [Google Scholar] [CrossRef] [PubMed]
- Van Heertum, K.; Rossi, B. Alcohol and fertility: How much is too much? Fertil. Res. Pract. 2017, 3, 10–18. [Google Scholar] [CrossRef]
- Schliep, K.C.; Zarek, S.M.; Schisterman, E.F.; Wactawski-Wende, J.; Trevisan, M.; Sjaarda, L.A.; Perkins, N.J.; Mumford, S.L. Alcohol intake, reproductive hormones, and menstrual cycle function: A prospective cohort study. Am. J. Clin. Nutr. 2015, 102, 933–942. [Google Scholar] [CrossRef]
- Fan, D.; Liu, L.; Xia, Q.; Wang, W.; Wu, S.; Tian, G.; Liu, Y.; Ni, J.; Wu, S.; Guo, X.; et al. Female alcohol consumption and fecundability: A systematic review and dose-response meta-analysis. Sci. Rep. 2017, 7, 13815. [Google Scholar] [CrossRef]
- Chavarro, J.E.; Rich-Edwards, J.W.; Rosner, B.A.; Willett, W.C. Use of multivitamins, intake of B vitamins, and risk of ovulatory infertility. Fertil. Steril. 2008, 89, 668–676. [Google Scholar] [CrossRef]
- Gaskins, A.J.; Mumford, S.L.; Chavarro, J.E.; Zhang, C.; Pollack, A.Z.; Wactawski-Wende, J.; Perkins, N.J.; Schisterman, E.F. The impact of dietary folate intake on reproductive function in premenopausal women: A prospective cohort study. PLoS ONE 2012, 7, e46276. [Google Scholar] [CrossRef][Green Version]
- Michels, K.A.; Wactawski-Wende, J.; Mills, J.L.; Schliep, K.C.; Gaskins, A.J.; Yeung, E.H.; Kim, K.; Plowden, T.C.; Sjaarda, L.A.; Chaljub, E.N.; et al. Folate, homocysteine and the ovarian cycle among healthy regularly menstruating women. Hum. Reprod. 2017, 32, 1743–1750. [Google Scholar] [CrossRef] [PubMed]
- Smits, R.M.; Mackenzie-Proctor, R.; Fleischer, K.; Showell, M.G. Antioxidants in fertility: Impact on male and female reproductive outcomes. Fertil. Steril. 2018, 110, 578–580. [Google Scholar] [CrossRef] [PubMed]
- Rasheedy, R.; Sammour, H.; Elkholy, A.; Salim, Y. The efficacy of vitamin D combined with clomiphene citrate in ovulation induction in overweight women with polycystic ovary syndrome: A double blind, randomized clinical trial. Endocrine 2020, 69, 393–401. [Google Scholar] [CrossRef] [PubMed]
- Yahya, A.A.; Abdulridha, M.K.; Al-Rubuyae, B.J.; Al-Atar, H.A. The Effect of Vitamin D and Co-enzyme Q10 Replacement Therapy on Hormonal Profile and Ovulation Statusin Women with Clomiphene Citrate Resistant Polycystic Ovary Syndrome. Pharm. Sci. Res. 2019, 11, 208–215. [Google Scholar]
- Chavarro, J.E.; Rich-Edwards, J.W.; Rosner, B.A.; Willett, W.C. Iron intake and risk of ovulatory infertility. Obstet. Gynecol. 2006, 108, 1145–1152. [Google Scholar] [CrossRef] [PubMed]
- Kim, K.; Wactawski-Wende, J.; Michels, K.A.; Schliep, K.C.; Plowden, T.C.; Chaljub, E.N.; Mumford, S.L. Dietary minerals, reproductive hormone levels and sporadic anovulation: Associations in healthy women with regular menstrual cycles. Br. J. Nutr. 2018, 120, 81–89. [Google Scholar] [CrossRef]
| First Author/Reference Number | Year | Study Design | Sample | Result |
|---|---|---|---|---|
| Dietary pattern | ||||
| Chavarro et al. [8] | 2007 | A prospective cohort study (NHS II) | 17,544 women, aged 25–42 years | Higher adherence to the FD was associated with a lower risk of anovulatory infertility compared to the lowest adherence (RR 0.34 (95% CI 0.23–0.48) vs. RR 0.68 (95% CI 0.52–0.89); p < 0.001). |
| Carbohydrates and low glycemic index diet | ||||
| Chavarro et al. [32] | 2009 | A prospective cohort study (NHS II) | 18,555 women, 25–42 years | An increase in cereal fiber intake by 10 g/day was associated with a 44% lower risk of anovulatory infertility among women older than 32 (RR 0.56 (95% CI 0.34–0.93); p = 0.02). The risk of anovulatory infertility was 78% higher in women from the highest quintile of total carbohydrate intake (60% of calories) compared to women from the lowest quintile (42% of calories) (RR 1.78 (95% CI 1.14–2.78); p = 0.005). A linear trend towards a higher risk of anovulatory infertility with increasing carbohydrate intake (p trend = 0.005). The risk of anovulatory infertility was 92% higher in women from the highest quintile of glycemic load compared to women from the lowest quintile (RR 1.92 (95% CI 1.26–2.92); p = 0.01). The risk of anovulatory infertility was 55% higher in nulliparous women from the highest quintile of glycemic index compared to women from the lowest quintile (RR 1.55 (95% CI 1.02–2.37); p = 0.05). Dietary glycemic index was positively associated with the risk of anovulatory infertility among nulliparous women (p interaction = 0.02). |
| Gaskin et al. [36] | 2009 | A prospective cohort study (The BioCycle Study) | 250 women, aged 18–44 years | Each 5 g/day increase in total fiber intake was associated with a 78% increased risk of an anovulatory cycle (RR 1.78 (95% CI 1.11–2.84); p < 0.05). Soluble fiber had a stronger, positive association with an increased risk of anovulation (OR 6.73 (95% CI 1.18–38.26) than insoluble fiber (OR 2.15 (95% CI 1.22–3.77) and fruit fiber (OR 3.05 (95% CI 1.07–8.71); p < 0.05). Dietary fiber consumption was positively associated with incidents of anovulation (p = 0.004), with an OR of 10.98 (95% CI: 1.5, 80.5) for women at or above the DRI (≥22 g/day) compared to the lowest DRI (≤10 g/day). |
| McGrice et al. [14] | 2017 | A Systematic Review of 7 intervention studies | Infertile women with obesity, aged > 18 years | The use of low-carbohydrate diet (less than 45% of total energy obtained from carbohydrates) was associated with a higher ovulation rate (p < 0.05) compared to the usual diet. |
| Palomba et al. [33] | 2010 | A randomized controlled trial | 96 PCOS women with obesity, aged 18–35 years with anovulatory infertility and known CC resistance | The intervention (structured exercise + 35% protein, 45% carbohydrate, 20% fat diet with calorie deficit + CC) was effective in increasing probability of ovulation under CC treatment. |
| Sordia-Hernández et al. [40] | 2015 | A randomized controlled clinical trial | 40 patients with the diagnosis of PCOS, infertility, and anovulation, mean age 26 years | 24.6% (14/57) of the cycles were ovulatory in women who consumed a low glycemic index diet. In those who consumed a normal glycemic index diet, only 7.4% (4/54) of the cycles were ovulatory (p = 0.014). |
| Plant and animal protein products | ||||
| Chavarro et al. [52] | 2007 | A prospective cohort study (NHS II) | 18,555 women, 25–42 years | The risk of anovulatory infertility was 27% lower in women from the highest quintile of intake of high-fat dairy products (≥1 servings/day) compared to women from the lowest quintile (≤1 servings/week) (RR 0.73 (95% CI 0.52–1.01); p < 0.05). Adding one daily serving of full-fat milk without increasing energy intake was associated with a reduction in the risk of anovulatory infertility by 63% (RR 0.37 (95% CI 0.19–0.70), p = 0.002). An inverse association between dairy fat intake and anovulatory infertility (p trend = 0.05). The risk of anovulatory infertility higher by 71% in women from the highest quintile of intake of low-fat dairy products (especially yoghurt and sherbet/frozen yoghurt) (one serving a day) compared to women from the lowest quintile (≤1 servings/week) (RR 1.71 (95% CI 1.24–2.77); p = 0.002). |
| Chavarro et al. [44] | 2008 | A prospective cohort study (NHS II) | 18,555 women, 25–42 years | Consuming 5% of energy from plant protein rather than from carbohydrates was associated with a 43% lower risk of anovulatory infertility (RR 0.57 (95% CI 0.32–1.00); p = 0.05). Consuming 5% of energy from vegetable protein rather than from animal protein was associated with a 52% lower risk of anovulatory infertility (RR 0.48 (95% CI 0.28–0.81); p = 0.007). The risk of anovulatory infertility was 41% higher in women from the highest quintile of total protein intake (23.1% of calories) compared to women from the lowest quintile (15.4% of calories) (RR 1.41 (95% CI 1.04–1.91); p = 0.02). The risk of anovulatory infertility was 39% higher in women from the highest quintile of animal protein intake (18.5% of calories) compared to women from the lowest quintile (10.2% of calories) (RR 1.39 (95% Cl 1.01–1.90); p = 0.03). Adding one serving of meat per day was associated with a 32% higher risk of anovulatory infertility (RR 1.32 (95% CI 1.08–1.62); p = 0.01). Adding one serving of chicken or turkey per day was associated with a 53% greater risk of anovulatory infertility (RR 1.53 (95% CI 1.12–2.09); p = 0.01). Consuming 5% of total energy intake as animal protein instead of from carbohydrates was associated with 19% greater risk of anovulatory infertility (RR 1.19 (95% CI 1.03–1.38); p = 0.02). |
| Kim et al. [49] | 2017 | A prospective cohort study (The BioCycle Study) | 259 healthy, regularly menstruating women, aged 18–35 years | Associations between intakes of >0 servings of yoghurt (RR 2.1 (95% CI 1.2–3.7) and cream (RR 1.8 (95% CI 1.0–3.2) and a higher risk of sporadic anovulation compared to no intake. |
| Zhang et al. [44] | 2020 | A prospective cohort study | 2217 infertile women with PCOS (with ovulation and without), aged > 18 years | PCOS women with anovulation had a higher rate of meat favorable diet than PCOS women with ovulation (54.60% vs. 41.30%, RR 1.69 (95%CI 1.28–2.23), p < 0.01). |
| Unsaturated and saturated fatty acids | ||||
| Chavarro et al. [53] | 2007 | A prospective cohort study (NHS II) | 18,555 women, 25–42 years | Each 2% increase in the intake of energy from trans unsaturated fats, rather than from carbohydrates was associated with a 73% higher risk of anovulatory infertility (RR 1.73 (95% CI 1.09–2.73); p = 0.02). Obtaining 2% of energy intake from trans fats rather than from n-6 polyunsaturated fats was associated with a 79% higher risk of anovulatory infertility (RR 1.79 (95% CI 1.11–2.89); p = 0.02). Obtaining 2% of energy from trans fats rather than from monounsaturated fats was associated with a more than doubled risk of anovulatory infertility (RR 2.31; (95% CI 1.09–4.87), p < 0.05). |
| Ghaffarzad et al. [60] | 2014 | A case-control study | 29 women with PCOS, aged 19–35 years | Higher concentrations of trans fatty acids (trans linoleate) in erythrocytes were associated with an increased incidence of ovulation disorders in this group of women (OR 1.218 (95% CI 1.016–1.46); p = 0.033). |
| Mumford et al. [54] | 2016 | A prospective cohort study (The BioCycle Study) | 259 regularly menstruating, healthy women, aged 18–44 years | The intake of PUFA docosapentaenoic acid (22:5 n–3) was associated with a reduced risk of anovulation (highest tertile compared with the lowest tertile: (RR: 0.42 (95% CI 0.18–0.95); p < 0.05). |
| Alcohol and caffeine | ||||
| Chavarro et al. [61] | 2009 | A prospective cohort study (NHS II) | 18,555 women, 25–42 years | Women consuming 2 or more caffeinated soft drinks per day were at a 47% greater risk of anovulatory infertility than women who consumed less than 1 caffeinated soft drink per week (RR 1.47 (95% CI 1.09–1.98); p = 0.01). Women consuming 10 g or more of alcohol per day (approximately > 1 drink/day) were at a 47% greater risk of anovulatory infertility than women who did not drink any alcohol (RR 1.47 (95% CI 1.02–2.10), p = 0.03). |
| Vitamins and minerals | ||||
| Chavarro et al. [76] | 2006 | A prospective cohort study (NHS II) | 17,544 women, aged 25–42 years | Women who consumed iron supplements were at a significantly lower risk of anovulatory infertility than women who did not use iron supplements (RR 0.60 (95% CI 0.39–0.92); p = 0.003). The risk of anovulatory infertility was 47% lower in women from the highest quintile of iron intake (77 mg/day) compared to women from the lowest quintile (11 mg/day) (RR 0.53 (95% CI 0.35–0.82); p = 0.003). The risk of anovulatory infertility was 40% lower in women from the highest quintile of nonheme iron intake (76 mg/d) compared to women from the lowest quintile (9.7 mg/d) (RR 0.60 (95% CI (0.39–0.92); p = 0.005). |
| Chavarro et al. [70] | 2008 | A prospective cohort study (NHS II) | 18,555 women, 25–42 years | The risk of anovulatory infertility was 41% lower in women who used multivitamins ≥ 6 times per week compared to women who did not use multivitamins (RR 0.59 (95% CI 0.46, 0.75); p < 0.001). The risk of anovulatory infertility was 39% lower in women from the highest quintile of intake of folic acid (1138 μg/day) compared to women from the lowest quintile (243 μg/day) (RR 0.61 (95% CI 0.37, 1.00); p = 0.04). |
| Gaskin et al. [71] | 2012 | A prospective cohort study (The BioCycle Study) | 259 women, aged 18–44 years | Women in the highest tertile of folate consumption (270.6 g/d) had a 64% lower chance of anovulation compared to women in the lowest tertile of folate consumption (100.9 g/d) (OR 0.36 (95% CI 0.14, 0.92); p = 0.03). |
| Kim et al. [77] | 1217 | A prospective cohort study (The BioCycle Study) | 259 regularly menstruating women, aged 18–44 years | Sodium intake < 1500 mg (RR 2.70 (95 % CI 1.00–7.31) and manganese intake < 1.8 mg (RR 2.00 (95% CI 1.02–3.94) were associated with an increased risk of anovulation, compared to higher intakes, p < 0.05. |
| Yahya et al. [75] | 2019 | A randomized- controlled, open-label study | 45 PCOS women, aged 18–40 years | Both dietary supplements (vitamin D3 or CO-enzyme Q10) in combination with CC, significantly improved ovulation rates in clomiphene citrate-resistant women with PCOS. |
| Rasheedy et al. [74] | 2019 | A double blind, randomized clinical trial | 186 women undergoing the induction of ovulation with CC, aged 25–35 years | Women with PCOS undergoing the induction of ovulation: vitamin D supplementation significantly improved the ovulation rate. More than 90% (92.5%) of women in the treatment group took CC (50 mg) twice daily and vitamin D3 (10,000 IU), and 78.5% in the control group (placebo) had successful ovulation (p = 0.007). |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jurczewska, J.; Szostak-Węgierek, D. The Influence of Diet on Ovulation Disorders in Women—A Narrative Review. Nutrients 2022, 14, 1556. https://doi.org/10.3390/nu14081556
Jurczewska J, Szostak-Węgierek D. The Influence of Diet on Ovulation Disorders in Women—A Narrative Review. Nutrients. 2022; 14(8):1556. https://doi.org/10.3390/nu14081556
Chicago/Turabian StyleJurczewska, Justyna, and Dorota Szostak-Węgierek. 2022. "The Influence of Diet on Ovulation Disorders in Women—A Narrative Review" Nutrients 14, no. 8: 1556. https://doi.org/10.3390/nu14081556
APA StyleJurczewska, J., & Szostak-Węgierek, D. (2022). The Influence of Diet on Ovulation Disorders in Women—A Narrative Review. Nutrients, 14(8), 1556. https://doi.org/10.3390/nu14081556







