Modelling the Impact of Reducing Ultra-Processed Foods Based on the NOVA Classification in Australian Women of Reproductive Age
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Population
2.2. Dietary Data
2.3. Dietary Scenarios
2.4. Dietary Modelling
3. Results
3.1. Population Baseline Intakes
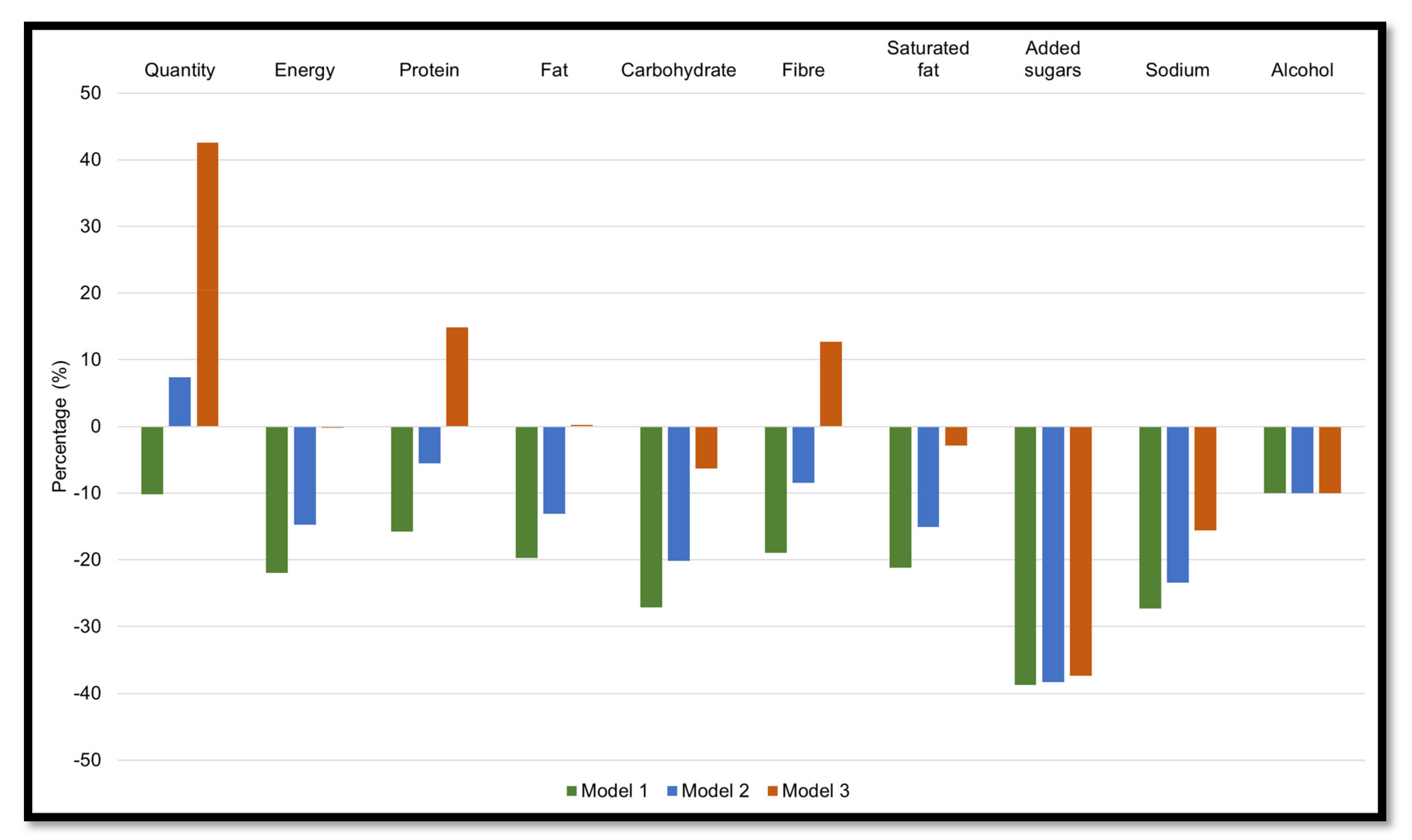
3.2. Strategy 1
3.2.1. Model 1: Reducing Ultra-Processed Foods by 50%
3.2.2. Models 2: Reducing Ultra-Processed Foods by 50% and Increasing Unprocessed or Minimally Processed Foods by 25%
3.2.3. Model 3: Reducing Ultra-Processed Foods by 50% and Increasing Unprocessed or Minimally Processed Foods by 75%
3.3. Strategy 2
3.3.1. Model 1: Reducing Processed Foods by 50%
3.3.2. Model 2: Reducing Processed Foods by 50% and Increasing Unprocessed or Minimally Processed Foods by 25%
3.3.3. Model 3: Reducing Processed Foods by 50% and Increasing Unprocessed or Minimally Processed Foods by 75%
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organisation (WHO). Reproductive Health Indicators. Reproductive Health and Research Guidelines for Their Generation, Interpretation and Analysis for Global Monitoring. 2006. Available online: http://apps.who.int/iris/bitstream/handle/10665/43185/924156315X_eng.pdf;jsessionid=13280E8CC5E65685D35F6AF1DA27B394?sequence=1 (accessed on 18 November 2021).
- Ng, M.; Fleming, T.; Robinson, M.; Thomson, B.; Graetz, N.; Margono, C.; Mullany, E.C.; Biryukov, S.; Abbafati, C.; Abera, S.F.; et al. Global, regional, and national prevalence of overweight and obesity in children and adults during 1980-2013: A systematic analysis for the Global Burden of Disease Study 2013. Lancet 2014, 384, 766–781. [Google Scholar] [CrossRef]
- Gomersall, S.R.; Dobson, A.J.; Brown, W.J. Weight Gain, Overweight, and Obesity: Determinants and Health Outcomes from the Australian Longitudinal Study on Women’s Health. Curr. Obes. Rep. 2014, 3, 46–53. [Google Scholar] [CrossRef] [PubMed]
- Grieger, J.A.; Hutchesson, M.J.; Cooray, S.D.; Bahri Khomami, M.; Zaman, S.; Segan, L.; Teede, H.; Moran, L.J. A review of maternal overweight and obesity and its impact on cardiometabolic outcomes during pregnancy and postpartum. Ther. Adv. Reprod. Health 2021, 15. [Google Scholar] [CrossRef] [PubMed]
- Patro Golab, B.; Santos, S.; Voerman, E.; Lawlor, D.A.; Jaddoe, V.W.V.; Gaillard, R.; Authors, M.S.G. Influence of maternal obesity on the association between common pregnancy complications and risk of childhood obesity: An individual participant data meta-analysis. Lancet Child Adolesc. Health 2018, 2, 812–821. [Google Scholar] [CrossRef]
- Jacob, C.M.; Baird, J.; Barker, M.; Cooper, C.; Hanson, M.; World Health Organization. The Importance of a Life Course Approach to Health: Chronic Disease Risk from Preconception through Adolescence and Adulthood. 2017. Available online: https://www.who.int/life-course/publications/life-course-approach-to-health.pdf (accessed on 18 November 2021).
- Rooney, B.L.; Schauberger, C.W.; Mathiason, M.A. Impact of perinatal weight change on long-term obesity and obesity-related illnesses. Obstet. Gynecol. 2005, 106, 1349–1356. [Google Scholar] [CrossRef] [PubMed]
- Linné, Y.; Dye, L.; Barkeling, B.; Rössner, S. Long-term weight development in women: A 15-year follow-up of the effects of pregnancy. Obes. Res. 2004, 12, 1166–1178. [Google Scholar] [CrossRef] [PubMed]
- Blumfield, M.L.; Hure, A.J.; Macdonald-Wicks, L.K.; Patterson, A.J.; Smith, R.; Collins, C.E. Disparities exist between National food group recommendations and the dietary intakes of women. BMC Womens Health 2011, 11, 37. [Google Scholar] [CrossRef] [PubMed]
- Martin, J.C.; Moran, L.J.; Teede, H.J.; Ranasinha, S.; Lombard, C.B.; Harrison, C.L. Exploring Diet Quality between Urban and Rural Dwelling Women of Reproductive Age. Nutrients 2017, 9, 586. [Google Scholar] [CrossRef]
- Mishra, G.D.; Schoenaker, D.A.; Mihrshahi, S.; Dobson, A.J. How do women’s diets compare with the new Australian dietary guidelines? Public Health Nutr. 2015, 18, 218–225. [Google Scholar] [CrossRef]
- Bhandari, S.; Sayami, J.T.; Thapa, P.; Sayami, M.; Kandel, B.P.; Banjara, M.R. Dietary intake patterns and nutritional status of women of reproductive age in Nepal: Findings from a health survey. Archives of Public Health 2016, 74, 2. [Google Scholar] [CrossRef]
- Devarshi, P.P.; Legette, L.L.; Grant, R.W.; Mitmesser, S.H. Total estimated usual nutrient intake and nutrient status biomarkers in women of childbearing age and women of menopausal age. Am. J. Clin. Nutr. 2021, 113, 1042–1052. [Google Scholar] [CrossRef]
- Padmadas, S.S.; Dias, J.G.; Willekens, F.J. Disentangling women’s responses on complex dietary intake patterns from an Indian cross-sectional survey: A latent class analysis. Public Health Nutr. 2006, 9, 204–211. [Google Scholar] [CrossRef][Green Version]
- Chen, X.; Zhang, Z.; Yang, H.; Qiu, P.; Wang, H.; Wang, F.; Zhao, Q.; Fang, J.; Nie, J. Consumption of ultra-processed foods and health outcomes: A systematic review of epidemiological studies. Nutr. J. 2020, 19, 86. [Google Scholar] [CrossRef]
- Monteiro, C.A.; Moubarac, J.C.; Cannon, G.; Ng, S.W.; Popkin, B. Ultra-processed products are becoming dominant in the global food system. Obes. Rev. 2013, 14 (Suppl. S2), 21–28. [Google Scholar] [CrossRef]
- Aguirre, A.; Borneo, M.T.; El Khori, S.; Borneo, R. Exploring the understanding of the term “ultra-processed foods” by young consumers. Food Res. Int. 2019, 115, 535–540. [Google Scholar] [CrossRef]
- Ares, G.; Vidal, L.; Allegue, G.; Gimenez, A.; Bandeira, E.; Moratorio, X.; Molina, V.; Curutchet, M.R. Consumers’ conceptualization of ultra-processed foods. Appetite 2016, 105, 611–617. [Google Scholar] [CrossRef]
- Adams, J.; White, M. Characterisation of UK diets according to degree of food processing and associations with socio-demographics and obesity: Cross-sectional analysis of UK National Diet and Nutrition Survey (2008–2012). Int. J. Behav. Nutr. Phys. Act. 2015, 12, 160. [Google Scholar] [CrossRef]
- Cediel, G.; Reyes, M.; da Costa Louzada, M.L.; Martinez Steele, E.; Monteiro, C.A.; Corvalan, C.; Uauy, R. Ultra-processed foods and added sugars in the Chilean diet (2010). Public Health Nutr 2018, 21, 125–133. [Google Scholar] [CrossRef]
- Nardocci, M.; Leclerc, B.S.; Louzada, M.L.; Monteiro, C.A.; Batal, M.; Moubarac, J.C. Consumption of ultra-processed foods and obesity in Canada. Can. J. Public Health 2019, 110, 4–14. [Google Scholar] [CrossRef]
- Machado, P.P.; Steele, E.M.; Levy, R.B.; da Costa Louzada, M.L.; Rangan, A.; Woods, J.; Gill, T.; Scrinis, G.; Monteiro, C.A. Ultra-processed food consumption and obesity in the Australian adult population. Nutr. Diabetes 2020, 10, 39. [Google Scholar] [CrossRef]
- Rauber, F.; Steele, E.M.; Louzada, M.; Millett, C.; Monteiro, C.A.; Levy, R.B. Ultra-processed food consumption and indicators of obesity in the United Kingdom population (2008–2016). PLoS ONE 2020, 15, e0232676. [Google Scholar] [CrossRef] [PubMed]
- Bielemann, R.M.; Motta, J.V.S.; Minten, G.C.; Horta, B.L.; Gigante, D.P. Consumption of ultra-processed foods and their impact on the diet of young adults. Rev. Saude Publica 2015, 49, 28. [Google Scholar] [CrossRef] [PubMed]
- Sung, H.; Park, J.M.; Oh, S.U.; Ha, K.; Joung, H. Consumption of Ultra-Processed Foods Increases the Likelihood of Having Obesity in Korean Women. Nutrients 2021, 13, 698. [Google Scholar] [CrossRef] [PubMed]
- Srour, B.; Fezeu, L.K.; Kesse-Guyot, E.; Alles, B.; Mejean, C.; Andrianasolo, R.M.; Chazelas, E.; Deschasaux, M.; Hercberg, S.; Galan, P.; et al. Ultra-processed food intake and risk of cardiovascular disease: Prospective cohort study (NutriNet-Sante). BMJ 2019, 365, l1451. [Google Scholar] [CrossRef]
- Fiolet, T.; Srour, B.; Sellem, L.; Kesse-Guyot, E.; Alles, B.; Mejean, C.; Deschasaux, M.; Fassier, P.; Latino-Martel, P.; Beslay, M.; et al. Consumption of ultra-processed foods and cancer risk: Results from NutriNet-Sante prospective cohort. BMJ 2018, 360, k322. [Google Scholar] [CrossRef]
- Machado, P.P.; Steele, E.M.; Louzada, M.; Levy, R.B.; Rangan, A.; Woods, J.; Gill, T.; Scrinis, G.; Monteiro, C.A. Ultra-processed food consumption drives excessive free sugar intake among all age groups in Australia. Eur. J. Nutr. 2020, 59, 2783–2792. [Google Scholar] [CrossRef]
- Weinstein, M.C.; O’Brien, B.; Hornberger, J.; Jackson, J.; Johannesson, M.; McCabe, C.; Luce, B.R. Principles of good practice for decision analytic modeling in health-care evaluation: Report of the ISPOR Task Force on Good Research Practices--Modeling Studies. Value Health 2003, 6, 9–17. [Google Scholar] [CrossRef]
- Australian Government. Department of Health and Aging, and the National Health and Medical Research Council. A Modelling System to Inform the Revision of the Australian Guide to Healthy Eating. 2011. Available online: https://www.eatforhealth.gov.au/sites/default/files/files/public_consultation/n55a_dietary_guidelines_food_modelling_111216.pdf (accessed on 16 June 2021).
- Heart Foundation. Rapid Review of the Evidence. Effectiveness of Food Reformulation as a Strategy to Improve Population Health. 2012. Available online: https://www.heartfoundation.org.au/getmedia/2bcb1637-1a86-48fc-bb6c-b243c4746272/RapidReview_FoodReformulation.pdf (accessed on 8 July 2021).
- Cobiac, L.J.; Tam, K.; Veerman, L.; Blakely, T. Taxes and Subsidies for Improving Diet and Population Health in Australia: A Cost-Effectiveness Modelling Study. PLoS Med. 2017, 14, e1002232. [Google Scholar] [CrossRef]
- Scarborough, P.; Nnoaham, K.E.; Clarke, D.; Capewell, S.; Rayner, M. Modelling the impact of a healthy diet on cardiovascular disease and cancer mortality. J. Epidemiol. Community Health 2012, 66, 420–426. [Google Scholar] [CrossRef]
- Hutchesson, M.J.; de Jonge Mulock Houwer, M.; Brown, H.M.; Lim, S.; Moran, L.J.; Vincze, L.; Rollo, M.E.; Hollis, J.L. Supporting women of childbearing age in the prevention and treatment of overweight and obesity: A scoping review of randomized control trials of behavioral interventions. BMC Womens Health 2020, 20, 14. [Google Scholar] [CrossRef]
- Australian Bureau of Statistics. ABS. Australian Health Survey: Users’ Guide 2011–2013 Catalogue No. 4363.0.55.001. 2015. Available online: http://www.abs.gov.au/ausstats/abs@.nsf/Lookup/4363.0.55.001Chapter1002011-13 (accessed on 16 June 2021).
- Food Standards Australia New Zealand. FSANZ. AUSNUT 2011–2013. Available online: http://www.foodstandards.gov.au/science/monitoringnutrients/ausnut/Pages/about.aspx (accessed on 8 July 2021).
- O’Halloran, S.A.; Lacy, K.E.; Grimes, C.A.; Woods, J.; Campbell, K.J.; Nowson, C.A. A novel processed food classification system applied to Australian food composition databases. J. Hum. Nutr. Diet. 2017, 30, 534–541. [Google Scholar] [CrossRef]
- Machado, P.P.; Steele, E.M.; Levy, R.B.; Sui, Z.; Rangan, A.; Woods, J.; Gill, T.; Scrinis, G.; Monteiro, C.A. Ultra-processed foods and recommended intake levels of nutrients linked to non-communicable diseases in Australia: Evidence from a nationally representative cross-sectional study. BMJ Open 2019, 9, e029544. [Google Scholar] [CrossRef]
- Monteiro, C.A.; Cannon, G.; Levy, R.B.; Moubarac, J.C.; Louzada, M.L.; Rauber, F.; Khandpur, N.; Cediel, G.; Neri, D.; Martinez-Steele, E.; et al. Ultra-processed foods: What they are and how to identify them. Public Health Nutr. 2019, 22, 936–941. [Google Scholar] [CrossRef]
- Moubarac, J.C.; Parra, D.C.; Cannon, G.; Monteiro, C.A. Food Classification Systems Based on Food Processing: Significance and Implications for Policies and Actions: A Systematic Literature Review and Assessment. Curr. Obes. Rep. 2014, 3, 256–272. [Google Scholar] [CrossRef]
- Australian Institute of Health and Welfare. AIHW. Poor Diet. 2019. Available online: https://www.aihw.gov.au/reports/food-nutrition/poor-diet/contents/poor-diet-in-adults (accessed on 8 July 2021).
- Habibi, N.; Livingstone, K.M.; Edwards, S.; Grieger, J.A. Do Older Women of Reproductive Age Have Better Diet Quality than Younger Women of Reproductive Age? Nutrients 2021, 13, 3830. [Google Scholar] [CrossRef]
- Food and Agriculture Organization of the United Nations. Plates, Pyramids, Planet. Developments in National Healthy and Sustainable Dietary Guidelines: A State of Play Assessment. FAO/University of Oxford. Rome. 2016. Available online: https://www.fao.org/documents/card/en/c/d8dfeaf1-f859-4191-954f-e8e1388cd0b7/ (accessed on 24 September 2021).
- Crimarco, A.; Landry, M.J.; Gardner, C.D. Ultra-processed Foods, Weight Gain, and Co-morbidity Risk. Curr. Obes. Rep. 2021. [Google Scholar] [CrossRef]
- Pulker, C.E.; Scott, J.A.; Pollard, C.M. Ultra-processed family foods in Australia: Nutrition claims, health claims and marketing techniques. Public Health Nutr. 2018, 21, 38–48. [Google Scholar] [CrossRef]
- Forde, C.G. From perception to ingestion; the role of sensory properties in energy selection, eating behaviour and food intake. Food Qual. Prefer. 2018, 66, 171–177. [Google Scholar] [CrossRef]
- Australian Government. National Health and Medical Research Council. Eat for Health. Discretionary Food and Drink Choices. 2017. Available online: https://www.eatforhealth.gov.au/food-essentials/discretionary-food-and-drink-choices (accessed on 16 June 2021).
- Ryan, D.; Heaner, M. Guidelines (2013) for managing overweight and obesity in adults. Preface to the full report. Obesity 2014, 22 (Suppl. S2), S1–S3. [Google Scholar] [CrossRef]
- Greenway, F.L. Physiological adaptations to weight loss and factors favouring weight regain. Int. J. Obes. 2015, 39, 1188–1196. [Google Scholar] [CrossRef]
- Gilbert, J.A.; Drapeau, V.; Astrup, A.; Tremblay, A. Relationship between diet-induced changes in body fat and appetite sensations in women. Appetite 2009, 52, 809–812. [Google Scholar] [CrossRef]
- Sumithran, P.; Prendergast, L.A.; Delbridge, E.; Purcell, K.; Shulkes, A.; Kriketos, A.; Proietto, J. Long-term persistence of hormonal adaptations to weight loss. N. Engl. J. Med. 2011, 365, 1597–1604. [Google Scholar] [CrossRef]
- Hill, A.J. The psychology of food craving. Proc. Nutr. Soc. 2007, 66, 277–285. [Google Scholar] [CrossRef]
- Hasan, H.; Nayfeh, T.; Alzuabi, M.; Wang, Z.; Kuchkuntla, A.R.; Prokop, L.J.; Newman, C.B.; Murad, M.H.; Rajjo, T.I. Weight Loss and Serum Lipids in Overweight and Obese Adults: A Systematic Review and Meta-Analysis. J. Clin. Endocrinol. Metab. 2020, 105, 3695–3703. [Google Scholar] [CrossRef]
- Xiang, L.; Wu, H.; Pan, A.; Patel, B.; Xiang, G.; Qi, L.; Kaplan, R.C.; Hu, F.; Wylie-Rosett, J.; Qi, Q. FTO genotype and weight loss in diet and lifestyle interventions: A systematic review and meta-analysis. Am. J. Clin. Nutr. 2016, 103, 1162–1170. [Google Scholar] [CrossRef]
- Melby, C.L.; Paris, H.L.; Foright, R.M.; Peth, J. Attenuating the Biologic Drive for Weight Regain Following Weight Loss: Must What Goes Down Always Go Back Up? Nutrients 2017, 9, 468. [Google Scholar] [CrossRef]
- Schwarz, N.A.; Rigby, B.R.; La Bounty, P.; Shelmadine, B.; Bowden, R.G. A review of weight control strategies and their effects on the regulation of hormonal balance. J. Nutr. Metab. 2011, 2011, 237932. [Google Scholar] [CrossRef]
- Grieger, J.A.; Johnson, B.J.; Wycherley, T.P.; Golley, R.K. Comparing the Nutritional Impact of Dietary Strategies to Reduce Discretionary Choice Intake in the Australian Adult Population: A Simulation Modelling Study. Nutrients 2017, 9, 442. [Google Scholar] [CrossRef]
- Australian Institute of Health and Welfare. AIHW. Australian Government. The Health of Australia’s Females. 2019. Available online: https://www.aihw.gov.au/reports/men-women/female-health/contents/lifestyle-risk-factors/tobacco-smoking-alcohol-and-illicit-drugs (accessed on 24 September 2021).
- Anwar, M.Y.; Marcus, M.; Taylor, K.C. The association between alcohol intake and fecundability during menstrual cycle phases. Hum. Reprod. 2021, 36, 2538–2548. [Google Scholar] [CrossRef]
- Lawrence, M.A.; Dickie, S.; Woods, J.L. Do Nutrient-Based Front-of-Pack Labelling Schemes Support or Undermine Food-Based Dietary Guideline Recommendations? Lessons from the Australian Health Star Rating System. Nutrients 2018, 10, 32. [Google Scholar] [CrossRef]
- Dickie, S.; Woods, J.L.; Lawrence, M. Analysing the use of the Australian Health Star Rating system by level of food processing. Int. J. Behav. Nutr. Phys. Act. 2018, 15, 128. [Google Scholar] [CrossRef] [PubMed]
- Page, B.; Sharp, A.; Lockshin, L.; Sorensen, H. Parents and children in supermarkets: Incidence and influence. J. Retail. Consum. Serv. 2018, 40, 31–39. [Google Scholar] [CrossRef]
- Marchese, L.; Livingstone, K.M.; Woods, J.L.; Wingrove, K.; Machado, P. Ultra-processed food consumption, socio-demographics and diet quality in Australian adults. Public Health Nutr. 2022, 25, 94–104. [Google Scholar] [CrossRef] [PubMed]
- Lee, A.J.; Kane, S.; Herron, L.M.; Matsuyama, M.; Lewis, M. A tale of two cities: The cost, price-differential and affordability of current and healthy diets in Sydney and Canberra, Australia. Int. J. Behav. Nutr. Phys. Act. 2020, 17, 80. [Google Scholar] [CrossRef]
- Lee, A.J.; Kane, S.; Ramsey, R.; Good, E.; Dick, M. Testing the price and affordability of healthy and current (unhealthy) diets and the potential impacts of policy change in Australia. BMC Public Health 2016, 16, 315. [Google Scholar] [CrossRef]
- Baraldi, L.G.; Martinez Steele, E.; Canella, D.S.; Monteiro, C.A. Consumption of ultra-processed foods and associated sociodemographic factors in the USA between 2007 and 2012: Evidence from a nationally representative cross-sectional study. BMJ Open 2018, 8, e020574. [Google Scholar] [CrossRef]
- Conde, W.L.; Monteiro, C.A. Nutrition transition and double burden of undernutrition and excess of weight in Brazil. Am. J. Clin. Nutr. 2014, 100, 1617S–1622S. [Google Scholar] [CrossRef]
- Monteiro, C.A.; Levy, R.B.; Claro, R.M.; de Castro, I.R.; Cannon, G. Increasing consumption of ultra-processed foods and likely impact on human health: Evidence from Brazil. Public Health Nutr. 2011, 14, 5–13. [Google Scholar] [CrossRef]

| Mean Baseline Intake | Intake from Ultra-Processed Foods (%) | Intake from Processed Foods (%) | Intake from Unprocessed or Minimally Processed Foods (%) | Intake from Processed Culinary Ingredients (%) | |
|---|---|---|---|---|---|
| Quantity (g) | 3112.6 | 548.9 (17.6) | 175.3 (5.6) | 2361.8 (75.9) | 26.6 (0.9) |
| Energy (kJ) * | 7388.2 | 3056.2 (41.4) | 1093.0 (14.8) | 2656.1 (36.0) | 582.9 (7.9) |
| Protein (g) | 74.6 | 20.8 (27.9) | 10.9 (14.6) | 42.7 (57.2) | 0.2 (0.3) |
| Fat (g) | 63.9 | 26.5 (41.5) | 8.7 (13.6) | 17.1 (26.8) | 11.6 (18.2) |
| Carbohydrate (g) | 198.7 | 97.1 (48.9) | 20.8 (10.5) | 71.5 (36.0) | 9.3 (4.7) |
| Fibre (g) | 19.8 | 6.3 (31.8) | 2.4 (12.1) | 11.1 (56.1) | 0.0 (0.0) |
| Saturated Fat (g) | 24.3 | 10.6 (43.6) | 4.0 (16.5) | 6.0 (24.7) | 3.7 (15.2) |
| Added sugar (g) | 46.2 | 36.8 (79.7) | 1.4 (3.0) | 0.2 (0.3) | 7.9 (17.1) |
| Sodium (mg) | 2142.3 | 1309.5 (61.1) | 463.4 (21.6) | 289.8 (13.5) | 79.6 (3.7) |
| Alcohol (g) | 9.1 | 1.8 (19.8) | 7.3 (80.2) | 0.0 (0.0) | 0 (0.0) |
| NOVA Food Groups | Energy (kJ) | Energy (kcal) | % of Total Energy Intake |
|---|---|---|---|
| Ultra-processed foods | 3056.2 | 730.4 | 41.4 |
| Mass-produced packaged breads | 333.5 | 79.7 | 4.5 |
| Pastries, buns, and cakes | 292.3 | 69.9 | 4.0 |
| Fast foods dishes a | 286.7 | 68.5 | 3.9 |
| Confectionery | 247.9 | 59.2 | 3.4 |
| Frozen and shelf stable ready meals b | 237.4 | 56.7 | 3.2 |
| Fruit drinks and iced teas | 206.2 | 49.3 | 2.8 |
| Breakfast cereals | 190.4 | 45.5 | 2.6 |
| Biscuits | 180.4 | 43.1 | 2.4 |
| Carbonated soft drinks | 171.7 | 41.0 | 2.3 |
| Milk-based drinks | 168.5 | 40.3 | 2.3 |
| Sausage and other reconstituted meat products | 163.5 | 39.1 | 2.2 |
| Sauces, dressing, and gravies | 157.7 | 37.7 | 2.1 |
| Salty snacks | 118.5 | 28.3 | 1.6 |
| Ice cream, ice pops, and frozen yoghurts | 101.7 | 24.3 | 1.4 |
| Margarine and other spreads | 91.3 | 21.8 | 1.2 |
| Alcoholic distilled drinks | 53.7 | 12.8 | 0.7 |
| Other c | 54.8 | 13.1 | 0.7 |
| Processed foods | 1093.0 | 261.2 | 14.8 |
| Processed breads | 427.0 | 102.1 | 5.8 |
| Beer and wine | 233.5 | 55.8 | 3.2 |
| Cheese | 220.2 | 52.6 | 3.0 |
| Bacon and other salted, smoked, or canned meat or fish | 84.0 | 20.1 | 1.1 |
| Vegetables and other plant foods preserved in brine | 36.2 | 8.7 | 0.5 |
| Other d | 92.1 | 22.0 | 1.2 |
| Unprocessed or minimally processed foods | 2656.1 | 634.8 | 36.0 |
| Red meat and poultry | 582.5 | 139.2 | 7.9 |
| Cereal grains and flours | 485.8 | 116.1 | 6.6 |
| Milk and plain yoghurt | 452.7 | 108.2 | 6.1 |
| Fruits e | 323.2 | 77.2 | 4.4 |
| Vegetables | 239.2 | 57.2 | 3.2 |
| Pasta | 204.8 | 48.9 | 2.8 |
| Nuts and seeds | 96.3 | 23.0 | 1.3 |
| Potatoes and other tubers and roots | 80.5 | 19.2 | 1.1 |
| Eggs | 71.7 | 17.1 | 1.0 |
| Fish | 62.1 | 14.8 | 0.8 |
| Legumes | 31.7 | 7.6 | 0.4 |
| Other f | 25.8 | 6.2 | 0.3 |
| Processed culinary ingredients | 582.9 | 139.3 | 7.9 |
| Plant oils | 269.6 | 64.4 | 3.6 |
| Animal fats | 164.3 | 39.3 | 2.2 |
| Table sugar | 125.6 | 30.0 | 1.7 |
| Other g | 23.4 | 5.6 | 0.3 |
| Total | 7388.2 | 1765.8 | 100.0 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Habibi, N.; Leemaqz, S.Y.-L.; Grieger, J.A. Modelling the Impact of Reducing Ultra-Processed Foods Based on the NOVA Classification in Australian Women of Reproductive Age. Nutrients 2022, 14, 1518. https://doi.org/10.3390/nu14071518
Habibi N, Leemaqz SY-L, Grieger JA. Modelling the Impact of Reducing Ultra-Processed Foods Based on the NOVA Classification in Australian Women of Reproductive Age. Nutrients. 2022; 14(7):1518. https://doi.org/10.3390/nu14071518
Chicago/Turabian StyleHabibi, Nahal, Shalem Yiner-Lee Leemaqz, and Jessica Anne Grieger. 2022. "Modelling the Impact of Reducing Ultra-Processed Foods Based on the NOVA Classification in Australian Women of Reproductive Age" Nutrients 14, no. 7: 1518. https://doi.org/10.3390/nu14071518
APA StyleHabibi, N., Leemaqz, S. Y.-L., & Grieger, J. A. (2022). Modelling the Impact of Reducing Ultra-Processed Foods Based on the NOVA Classification in Australian Women of Reproductive Age. Nutrients, 14(7), 1518. https://doi.org/10.3390/nu14071518