A High-Protein and Low-Glycemic Formula Diet Improves Blood Pressure and Other Hemodynamic Parameters in High-Risk Individuals
Abstract
1. Introduction
2. Materials and Methods
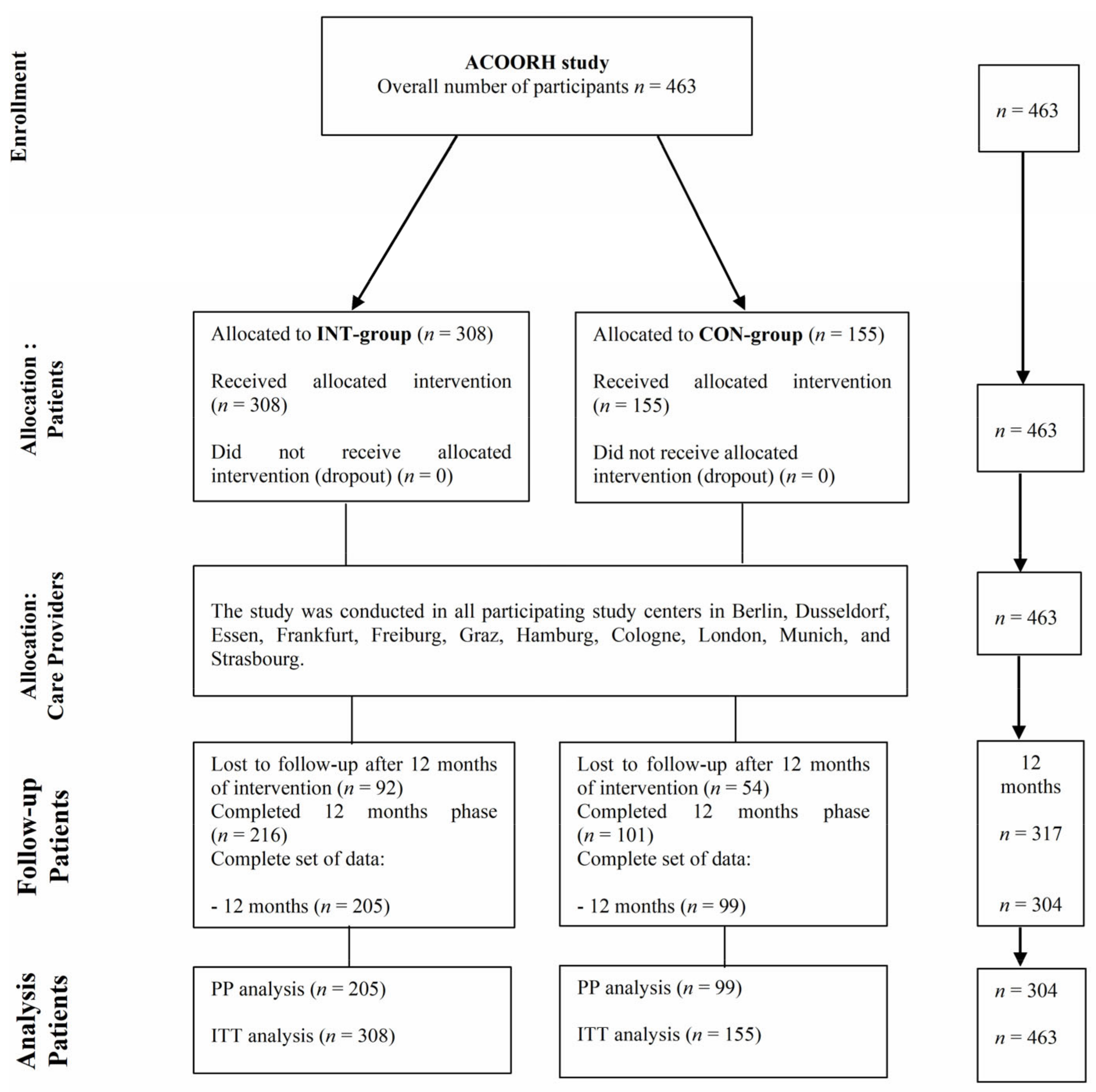
2.1. Study Design and Population
2.2. Intervention and Meal Replacement Regimen
2.3. Measurements
2.4. Statistics
3. Results
3.1. Intra and Intergroup Differences in Hemodynamic Parameters after 6 and 12 Months Focusing on Risk Groups
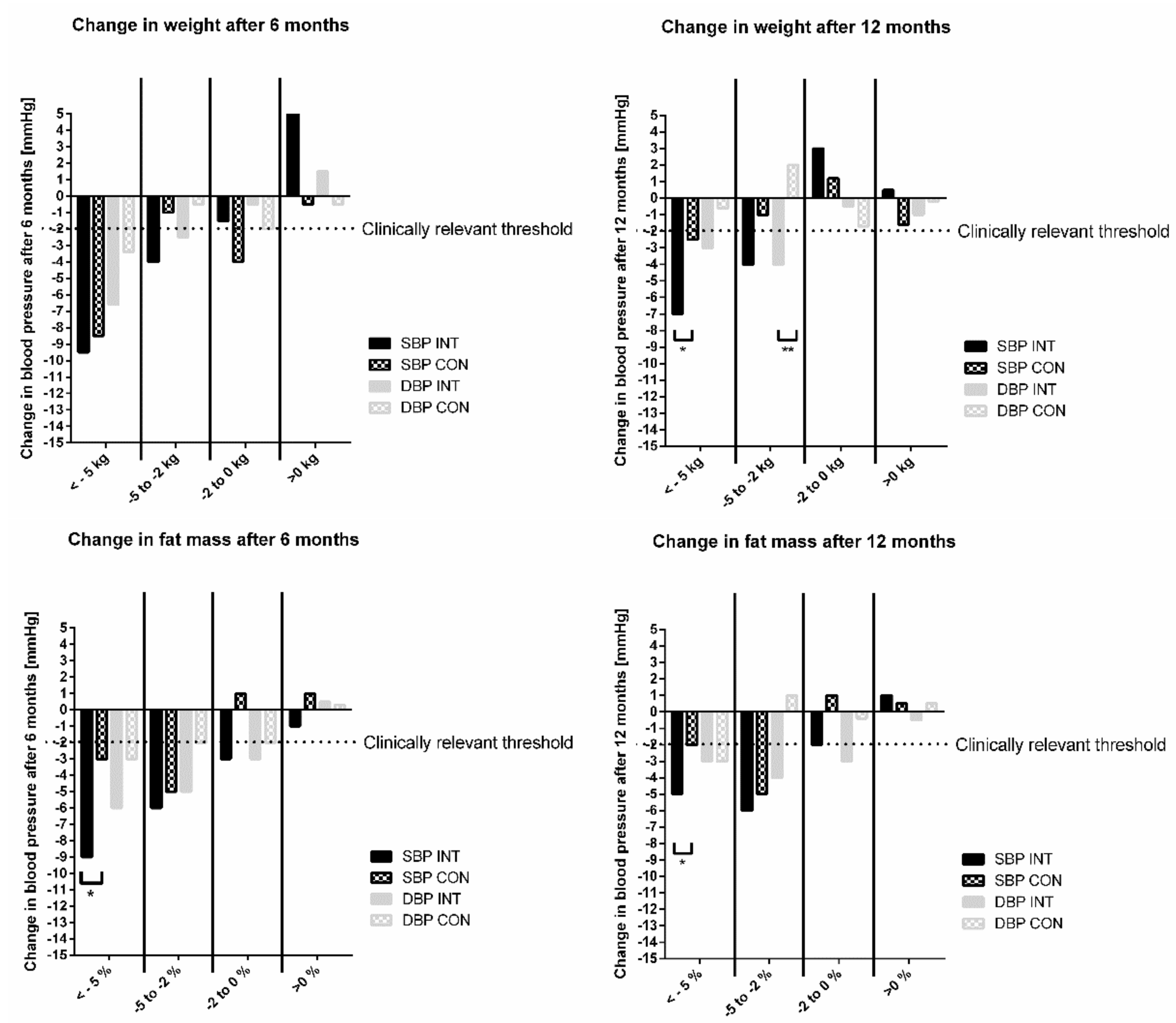
3.2. Association of Changes in Hemodynamic Parameters with Clinical Parameters
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Emdin, C.A.; Rahimi, K.; Neal, B.; Callender, T.; Perkovic, V.; Patel, A. Blood pressure lowering in type 2 diabetes: A systematic review and meta-analysis. JAMA 2015, 313, 603–615. [Google Scholar] [CrossRef] [PubMed]
- Jiang, X.; Liu, X.; Wu, S.; Zhang, G.Q.; Peng, M.; Wu, Y.; Zheng, X.; Ruan, C.; Zhang, W. Metabolic syndrome is associated with and predicted by resting heart rate: A cross-sectional and longitudinal study. Heart 2015, 101, 44–49. [Google Scholar] [CrossRef] [PubMed]
- Safar, M.E. Arterial stiffness as a risk factor for clinical hypertension. Nat. Rev. Cardiol. 2018, 15, 97–105. [Google Scholar] [CrossRef] [PubMed]
- Gaede, P.; Vedel, P.; Larsen, N.; Jensen, G.V.; Parving, H.H.; Pedersen, O. Multifactorial intervention and cardiovascular disease in patients with type 2 diabetes. N. Engl. J. Med. 2003, 348, 383–393. [Google Scholar] [CrossRef] [PubMed]
- Liu, X.; Wu, S.; Song, Q.; Wang, X. Reversion from Pre-Diabetes Mellitus to Normoglycemia and Risk of Cardiovascular Disease and All-Cause Mortality in a Chinese Population: A Prospective Cohort Study. J. Am. Heart Assoc. 2021, 10, e019045. [Google Scholar] [CrossRef] [PubMed]
- Kolb, H.; Martin, S. Environmental/lifestyle factors in the pathogenesis and prevention of type 2 diabetes. BMC Med. 2017, 15, 131. [Google Scholar] [CrossRef]
- Kolb, H.; Stumvoll, M.; Kramer, W.; Kempf, K.; Martin, S. Insulin translates unfavourable lifestyle into obesity. BMC Med. 2018, 16, 232. [Google Scholar] [CrossRef]
- Kolb, H.; Kempf, K.; Röhling, M.; Martin, S. Insulin: Too much of a good thing is bad. BMC Med. 2020, 18, 224. [Google Scholar] [CrossRef]
- Ge, L.; Sadeghirad, B.; Ball, G.D.C.; da Costa, B.R.; Hitchcock, C.L.; Svendrovski, A.; Kiflen, R.; Quadri, K.; Kwon, H.; Karamouzian, M.; et al. Comparison of dietary macronutrient patterns of 14 popular named dietary programmes for weight and cardiovascular risk factor reduction in adults: Systematic review and network meta-analysis of randomised trials. BMJ 2020, 369, m696. [Google Scholar] [CrossRef]
- Schwingshackl, L.; Zähringer, J.; Nitschke, K.; Torbahn, G.; Lohner, S.; Kühn, T.; Fontana, L.; Veronese, N.; Schmucker, C.; Meerpohl, J.J. Impact of intermittent energy restriction on anthropometric outcomes and intermediate disease markers in patients with overweight and obesity: Systematic review and meta-analyses. Crit. Rev. Food Sci. Nutr. 2021, 61, 1293–1304. [Google Scholar] [CrossRef]
- Leslie, W.S.; Ali, E.; Harris, L.; Messow, C.M. Antihypertensive medication needs and blood pressure control with weight loss in the Diabetes Remission Clinical Trial (DiRECT). Diabetologia 2021, 64, 1927–1938. [Google Scholar] [CrossRef] [PubMed]
- Röhling, M.; Kempf, K.; Banzer, W.; Berg, A.; Braumann, K.M.; Tan, S.; Halle, M.; McCarthy, D.; Pinget, M.; Predel, H.-G.; et al. Prediabetes Conversion to Normoglycemia Is Superior Adding a Low-Carbohydrate and Energy Deficit Formula Diet to Lifestyle Intervention-A 12-Month Subanalysis of the ACOORH Trial. Nutrients 2020, 12, 2022. [Google Scholar] [CrossRef] [PubMed]
- Halle, M.; Röhling, M.; Banzer, W.; Braumann, K.M.; Kempf, K.; McCarthy, D.; Schaller, N.; Predel, H.-G.; Scholze, J.; Führer-Sakel, D.; et al. Meal replacement by formula diet reduces weight more than a lifestyle intervention alone in patients with overweight or obesity and accompanied cardiovascular risk factors-the ACOORH trial. Eur. J. Clin. Nutr. 2021, 75, 661–669. [Google Scholar] [CrossRef] [PubMed]
- Röhling, M.; Stensitzky, A.; Oliveira, C.L.P.; Beck, A.; Braumann, K.M.; Halle, M.; Führer-Sakel, D.; Kempf, K.; McCarthy, D.; Predel, H.-G.; et al. Effects of a Protein-Rich, Low-Glycaemic Meal Replacement on Changes in Dietary Intake and Body Weight Following a Weight-Management Intervention—The ACOORH Trial. Nutrients 2021, 13, 376. [Google Scholar] [CrossRef] [PubMed]
- Kempf, K.; Röhling, M.; Banzer, W.; Braumann, K.M.; Halle, M.; McCarthy, D.; Predel, H.-G.; Schenkenberger, I.; Tan, S.; Toplak, H.; et al. High-Protein, Low-Glycaemic Meal Replacement Decreases Fasting Insulin and Inflammation Markers—A 12-Month Subanalysis of the ACOORH Trial. Nutrients 2021, 13, 1433. [Google Scholar] [CrossRef]
- Koohkan, S.; McCarthy, D.; Berg, A. The effect of a soy-yoghurt-honey product on excess weight and related Page health risk factors—A review. J. Nutr. Health Food Sci. 2017, 5, 1–10. [Google Scholar]
- Bosy-Westphal, A.; Schautz, B.; Later, W.; Kehayias, J.J.; Gallagher, D.; Müller, M.J. What makes a BIA equation unique? Validity of eight-electrode multifrequency BIA to estimate body composition in a healthy adult population. Eur. J. Clin. Nutr. 2013, 67, S14–S21. [Google Scholar] [CrossRef]
- Hametner, B.; Wassertheurer, S.; Kropf, J.; Mayer, C.; Eber, B.; Weber, T. Oscillometric estimation of aortic pulse wave velocity: Comparison with intra-aortic catheter measurements. Blood Press. Monit. 2013, 18, 173–176. [Google Scholar] [CrossRef]
- U.S. Food and Drug Administration. Investigational New Drug Application (IND); Sec. 312.32 IND Safety Reporting; U.S. Food and Drug Administration: Silver Spring, MD, USA, 2018.
- Makai, P.; IntHout, J.; Deinum, J.; Jenniskens, K.; Wilt, G.J.V. A Network Meta-Analysis of Clinical Management Strategies for Treatment-Resistant Hypertension: Making Optimal Use of the Evidence. J. Gen. Intern. Med. 2017, 32, 921–930. [Google Scholar] [CrossRef]
- Whelton, P.K.; He, J.; Appel, L.J.; Cutler, J.A.; Havas, S.; Kotchen, T.A.; Roccella, E.J.; Stout, R.; Vallbona, C.; Winston, M.C.; et al. Primary prevention of hypertension: Clinical and public health advisory from The National High Blood Pressure Education Program. JAMA 2002, 288, 1882–1888. [Google Scholar] [CrossRef]
- Di Daniele, N.; Marrone, G. Effects of Caloric Restriction Diet on Arterial Hypertension and Endothelial Dysfunction. Nutrients 2021, 13, 274. [Google Scholar] [CrossRef] [PubMed]
- Gabel, K.; Cienfuegos, S.; Kalam, F.; Ezpeleta, M.; Varady, K.A. Time-Restricted Eating to Improve Cardiovascular Health. Curr. Atheroscler. Rep. 2021, 23, 22. [Google Scholar] [CrossRef] [PubMed]
- Brinkley, T.E.; Leng, I.; Bailey, M.J.; Houston, D.K.; Hugenschmidt, C.E.; Nicklas, B.J.; Hundley, W.G. Effects of Exercise and Weight Loss on Proximal Aortic Stiffness in Older Adults with Obesity. Circulation 2021, 144, 684–693. [Google Scholar] [CrossRef] [PubMed]
- Vogtschmidt, Y.D.; Raben, A.; Faber, I.; de Wilde, C.; Lovegrove, J.A.; Givens, D.I.; Pfeiffer, A.F.; Soedamah-Muthu, S.S. Is protein the forgotten ingredient: Effects of higher compared to lower protein diets on cardiometabolic risk factors. A systematic review and meta-analysis of randomised controlled trials. Atherosclerosis 2021, 328, 124–135. [Google Scholar] [CrossRef] [PubMed]
- Fekete, Á.A.; Giromini, C. Whey protein lowers blood pressure and improves endothelial function and lipid biomarkers in adults with prehypertension and mild hypertension: Results from the chronic Whey2Go randomized controlled trial. Am. J. Clin. Nutr. 2016, 104, 1534–1544. [Google Scholar] [CrossRef]
- Fu, Q. Sex differences in sympathetic activity in obesity and its related hypertension. Ann. N. Y. Acad. Sci. 2019, 1454, 31–41. [Google Scholar] [CrossRef]
- Farkhondeh, T.; Llorens, S. An Overview of the Role of Adipokines in Cardiometabolic Diseases. Molecules 2020, 25, 5218. [Google Scholar] [CrossRef]
- Tanaka, M. Improving obesity and blood pressure. Hypertens. Res. 2020, 43, 79–89. [Google Scholar] [CrossRef]
- Rabe, K.; Lehrke, M.; Parhofer, K.G.; Broedl, U.C. Adipokines and insulin resistance. Mol. Med. 2008, 14, 741–751. [Google Scholar] [CrossRef]
- Festa, A.; D’Agostino, R., Jr.; Hales, C.N.; Mykkänen, L.; Haffner, S.M. Heart rate in relation to insulin sensitivity and insulin secretion in nondiabetic subjects. Diabetes Care 2000, 23, 624–628. [Google Scholar] [CrossRef][Green Version]
- Manzella, D.; Paolisso, G. Cardiac autonomic activity and Type II diabetes mellitus. Clin. Sci. 2005, 108, 93–99. [Google Scholar] [CrossRef] [PubMed]
- Hansen, C.S.; Færch, K. Heart Rate, Autonomic Function, and Future Changes in Glucose Metabolism in Individuals without Diabetes: The Whitehall II Cohort Study. Diabetes Care 2019, 42, 867–874. [Google Scholar] [CrossRef] [PubMed]
- Taheri, S.; Zaghloul, H.; Chagoury, O.; Elhadad, S.; Ahmed, S.H.; El Khatib, N.; Amona, R.A.; El Nahas, K.; Suleiman, N.; Alnaama, A.; et al. Effect of intensive lifestyle intervention on bodyweight and glycaemia in early type 2 diabetes (DIADEM-I): An open-label, parallel-group, randomised controlled trial. Lancet Diabetes Endocrinol. 2020, 8, 477–489. [Google Scholar] [CrossRef]
- Leslie, W.S.; Taylor, R.; Harris, L.; Lean, M.E. Weight losses with low-energy formula diets in obese patients with and without type 2 diabetes: Systematic review and meta-analysis. Int. J. Obes. 2017, 41, 96–101. [Google Scholar] [CrossRef]
- Stefan, N.; Haring, H.U.; Schulze, M.B. Metabolically healthy obesity: The low-hanging fruit in obesity treatment? Lancet Diabetes Endocrinol. 2018, 6, 249–258. [Google Scholar] [CrossRef]
- Huang, L.; Trieu, K.; Yoshimura, S.; Neal, B.; Woodward, M.; Campbell, N.R.C.; Li, Q.; Lackland, D.T.; Leung, A.A.; Anderson, C.A.M.; et al. Effect of dose and duration of reduction in dietary sodium on blood pressure levels: Systematic review and meta-analysis of randomised trials. BMJ 2020, 368, m315. [Google Scholar] [CrossRef]
- Röhling, M.; Strom, A.; Bonhof, G.; Puttgen, S.; Bodis, K.; Mussig, K.; Szendrödi, J.; Markgraf, D.; Lehr, S.; Roden, M.; et al. Differential Patterns of Impaired Cardiorespiratory Fitness and Cardiac Autonomic Dysfunction in Recently Diagnosed Type 1 and Type 2 Diabetes. Diabetes Care 2017, 40, 246–252. [Google Scholar] [CrossRef]
- Röhling, M.; Strom, A.; Bönhof, G.J.; Roden, M.; Ziegler, D. Cardiorespiratory Fitness and Cardiac Autonomic Function in Diabetes. Curr. Diabetes Rep. 2017, 17, 125. [Google Scholar] [CrossRef]
- Bhanpuri, N.H.; Hallberg, S.J.; Williams, P.T.; McKenzie, A.L.; Ballard, K.D.; Campbell, W.W.; McCarter, J.P.; Phinney, S.D.; Volek, J.S. Cardiovascular disease risk factor responses to a type 2 diabetes care model including nutritional ketosis induced by sustained carbohydrate restriction at 1 year: An open label, non-randomized, controlled study. Cardiovasc. Diabetol. 2018, 17, 56. [Google Scholar] [CrossRef]

| INT-Group (n = 205) | CON-Group (n = 99) | |
|---|---|---|
| Clinical parameters | ||
| Sex (% male) | 35.2 | 40.6 |
| Age (years) | 51 ± 10 | 50 ± 9 |
| Weight (kg) | 92 ± 14 | 94 ± 12 |
| BMI (kg/m2) | 31.5 ± 2.3 | 31.5 ± 2.4 |
| Fat mass (kg) | 36.6 ± 6.6 | 37.2 ± 6.5 |
| Fat-free mass (kg) | 54.9 ± 11.7 | 56.4 ± 11.5 |
| Fasting insulin (µU/mL) | 15.9 ± 10.3 | 15.1 ± 8.7 |
| Fasting glucose (mg/dL) | 94 ± 12 | 93 ± 11 |
| HbA1c (%) | 5.50 ± 0.34 | 5.47 ± 0.38 |
| Hemodynamic parameters | ||
| SBP (mmHg) | ||
| Normotension (≤120 mmHg) | 113 ± 6 (n = 86) | 112 ± 6 (n = 44) |
| Prehypertension (121–139 mm Hg) | 129 ± 6 (n = 91) | 128 ± 5 (n = 40) |
| Hypertension (≥140 mmHg) | 152 ± 11 (n = 28) | 156 ± 11 (n = 15) |
| DBP (mmHg) | ||
| Normotension (≤80 mmHg) | 64 ± 15 (n = 59) | 64 ± 18 (n = 26) |
| Prehypertension (81–89 mm Hg) | 85 ± 2 (n = 53) | 85 ± 2 (n = 31) |
| Hypertension (≥90 mmHg) | 99 ± 8 (n = 93) | 97 ± 5 (n = 42) |
| Resting HR (bpm) | ||
| 1st tertile | 60 ± 6 (n = 68) | 60 ± 5 (n = 39) |
| 2nd tertile | 71 ± 3 (n = 70) | 71 ± 2 (n = 24) |
| 3rd tertile | 84 ± 7 (n = 67) | 83 ± 7 (n = 36) |
| PWV (m/s) | ||
| 1st tertile | 6.4 ± 0.7 (n = 68) | 6.3 ± 0.6 (n = 34) |
| 2nd tertile | 7.7 ± 0.3 (n = 67) | 7.7 ± 0.3 (n = 35) |
| 3rd tertile | 8.9 ± 0.6 (n = 70) | 8.9 ± 0.7 (n = 30) |
| Baseline | 6 Months | 12 Months | ||||||
|---|---|---|---|---|---|---|---|---|
| INT | CON | INT | CON | P (INT vs. CON) | INT | CON | P (INT vs. CON) | |
| SBP (mmHg) ‡ | ||||||||
| ITT (n = 180 vs. 89) | 134 ± 11 | 133 ± 10 | −8.6 [−11.1; −7.3] *** | −7.9 [−10.9; −5.4] *** | 0.652 | −7.3 [−9.2; −5.3] *** | −3.3 [−5.9; −0.8] * | 0.049 |
| PP (n = 119 vs. 55) | 134 ± 12 | 133 ± 11 | −10.6 [−11.4; −9.6] *** | −9.9 [−13.7; −6.3] *** | 0.534 | −8.8 [−11.4; −6.1] *** | −4.0 [−7.9; −0.1] * | 0.031 |
| DBP (mmHg) † | ||||||||
| ITT (n = 225 vs. 117) | 94 ± 10 | 92 ± 8 | −4.6 [−5.7; −3.2] *** | −1.6 [−3.3; −0.1] * | 0.009 | −3.7 [−4.9; −2.5] *** | −1.4 [−3.1; 0.2] | 0.028 |
| PP (n = 146 vs. 73) | 94 ± 9 | 92 ± 7 | −5.8 [−7.0; −4.1] *** | −2.1 [−4.1; −0.2] * | 0.003 | −4.4 [−5.8; −3.0] *** | −1.5 [−3.4; 0.5] | 0.019 |
| Resting HR (bpm) $ | ||||||||
| ITT (n = 208 vs. 94) | 78 ± 8 | 77 ± 8 | −4.0 [−5.3; −2.7] *** | −1.6 [−3.5; 0.4] | 0.045 | −2.7 [−4.0; −1.4] *** | −2.4 [−4.3; −0.4] * | 0.783 |
| PP (n = 137 vs. 60) | 77 ± 8 | 78 ± 8 | −5.0 [−6.6; −3.4] *** | −3.6 [−6.3; −1.2] ** | 0.353 | −3.4 [−4.9; −1.6] *** | −4.5 [−6.9; −2.3] *** | 0.240 |
| PWV (m/s) $ | ||||||||
| ITT (n = 194 vs. 98) | 8.4 ± 0.7 | 8.2 ± 0.7 | −0.18 [−0.28; −0.08] *** | −0.07 [−0.20; 0.13] | 0.043 | −0.10 [−0.18; −0.03] * | −0.01 [−0.11; 0.10] | 0.110 |
| PP (n = 137 vs. 65) | 8.3 ± 0.7 | 8.3 ± 0.8 | −0.25 [−0.36; −0.16] *** | −0.11 [−0.27; 0.15] | 0.049 | −0.09 [−0.18; 0.01] | 0.02 [−0.12; 0.16] | 0.200 |
| Hemodynamic Parameters Clinical Parameters | Systolic Blood Pressure | Diastolic Blood Pressure | Resting Heart Rate | Pulse Wave Velocity | |||||
|---|---|---|---|---|---|---|---|---|---|
| Δ 6 Months | Δ 12 Months | Δ 6 Months | Δ 12 Months | Δ 6 Months | Δ 12 Months | Δ 6 Months | Δ 12 Months | ||
| Δ Weight | r | +0.336 | +0.206 | +0.260 | +0.132 | +0.186 | +0.144 | +0.255 | +0.198 |
| [kg] | p | <0.001 | <0.001 | <0.001 | 0.025 | 0.002 | 0.015 | <0.001 | <0.001 |
| Δ Fat mass | r | +0.290 | +0.207 | +0.253 | +0.155 | +0.172 | +0.163 | +0.213 | +0.155 |
| [kg] | p | <0.001 | <0.001 | <0.001 | 0.008 | 0.003 | 0.006 | <0.001 | 0.008 |
| Δ Fat-free mass | r | +0.179 | +0.170 | +0.117 | +0.030 | +0.019 | +0.021 | +0.092 | +0.180 |
| [kg] | p | 0.003 | 0.004 | 0.049 | 0.611 | 0.748 | 0.723 | 0.190 | 0.002 |
| Δ Fasting insulin | r | +0.128 | +0.110 | +0.036 | +0.002 | +0.229 | +0.220 | +0.111 | +0.132 |
| [µU/mL] | p | 0.030 | 0.062 | 0.541 | 0.878 | <0.001 | <0.001 | 0.062 | 0.025 |
| Δ Glukose | r | +0.123 | +0.069 | +0.123 | +0.046 | +0.057 | +0.014 | +0.119 | +0.066 |
| [mg/dL] | p | 0.030 | 0.248 | 0.039 | 0.440 | 0.335 | 0.809 | 0.045 | 0.264 |
| Δ HbA1c | r | +0.067 | +0.121 | +0.052 | +0.098 | +0.128 | +0.134 | +0.030 | +0.047 |
| [%] | p | 0.259 | 0.175 | 0.380 | 0.098 | 0.031 | 0.003 | 0.616 | 0.426 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Röhling, M.; Kempf, K.; Banzer, W.; Braumann, K.M.; Führer-Sakel, D.; Halle, M.; McCarthy, D.; Martin, S.; Scholze, J.; Toplak, H.; et al. A High-Protein and Low-Glycemic Formula Diet Improves Blood Pressure and Other Hemodynamic Parameters in High-Risk Individuals. Nutrients 2022, 14, 1443. https://doi.org/10.3390/nu14071443
Röhling M, Kempf K, Banzer W, Braumann KM, Führer-Sakel D, Halle M, McCarthy D, Martin S, Scholze J, Toplak H, et al. A High-Protein and Low-Glycemic Formula Diet Improves Blood Pressure and Other Hemodynamic Parameters in High-Risk Individuals. Nutrients. 2022; 14(7):1443. https://doi.org/10.3390/nu14071443
Chicago/Turabian StyleRöhling, Martin, Kerstin Kempf, Winfried Banzer, Klaus Michael Braumann, Dagmar Führer-Sakel, Martin Halle, David McCarthy, Stephan Martin, Jürgen Scholze, Hermann Toplak, and et al. 2022. "A High-Protein and Low-Glycemic Formula Diet Improves Blood Pressure and Other Hemodynamic Parameters in High-Risk Individuals" Nutrients 14, no. 7: 1443. https://doi.org/10.3390/nu14071443
APA StyleRöhling, M., Kempf, K., Banzer, W., Braumann, K. M., Führer-Sakel, D., Halle, M., McCarthy, D., Martin, S., Scholze, J., Toplak, H., Berg, A., Predel, H.-G., & ACOORH Study Group. (2022). A High-Protein and Low-Glycemic Formula Diet Improves Blood Pressure and Other Hemodynamic Parameters in High-Risk Individuals. Nutrients, 14(7), 1443. https://doi.org/10.3390/nu14071443








