Food Security Impacts of the COVID-19 Pandemic: Longitudinal Evidence from a Cohort of Adults in Vermont during the First Year
Abstract
1. Introduction
- What was the trajectory of food insecurity during the first year of the COVID-19 pandemic among a cohort of respondents?
- What socio-demographic factors and life experiences were associated with increased odds of experiencing food insecurity during the first year of the COVID-19 pandemic?
- What factors, if any, contributed to the recovery from food insecurity during the first year of the COVID-19 pandemic?
2. Materials and Methods
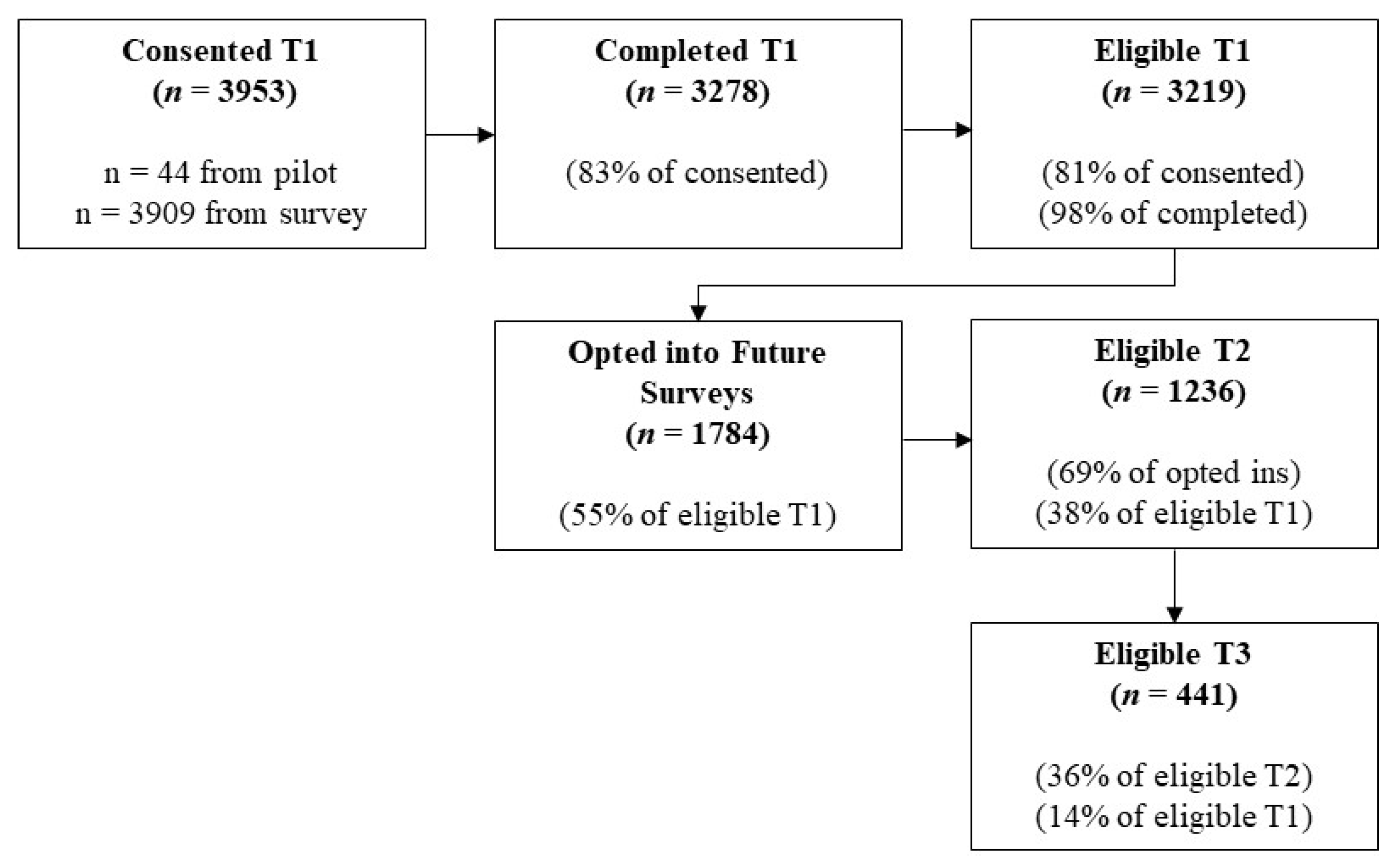
2.1. Survey Development and Recruitment
2.2. Statistical Analysis
3. Results
3.1. Demographic Characteristics of Respondents
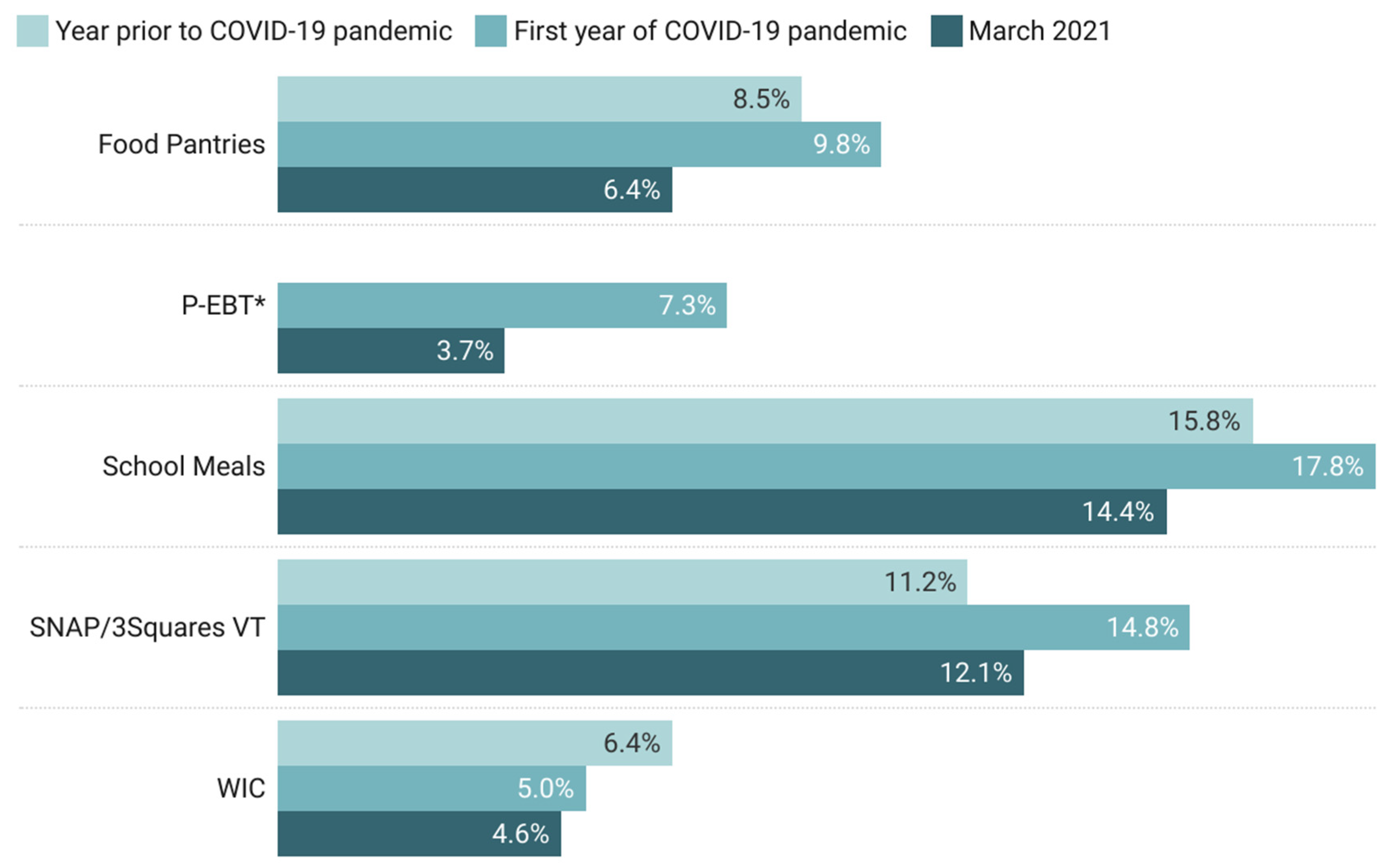
3.2. Food Insecurity, Job Disruptions, and Food Assistance Program Use
3.3. Factors Correlated with Food Insecurity
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
| Variable | Question | Scale |
|---|---|---|
| Food-secure | Determined based on the responses to the U.S Household Food Security Survey Module: Six-Item Short Form. These households were not classified as food-insecure at any time during COVID-19. | Binary (1 = Food-secure, 0 = Food-insecure) |
| Food-insecure | Determined based on the responses to the U.S Household Food Security Survey Module: Six-Item Short Form. These households were food-insecure at any time during COVID-19, including newly food-insecure and consistently food-insecure households. | Binary (1 = Food-insecure, 0 = Food-secure) |
| Newly food-insecure | Determined based on the responses to the U.S Household Food Security Survey Module: Six-Item Short Form. These households were classified as not food-insecure during the year prior to COVID-19, but were classified as food-insecure at some point during the first year of the COVID-19 pandemic. | Binary (1 = Newly food-insecure, 0 = Consistently food-insecure) |
| Consistently food-insecure | Determined based on the responses to the U.S Household Food Security Survey Module: Six-Item Short Form. These households were classified as food-insecure both in the year prior to COVID-19 and at anytime during the first year of the COVID-19 pandemic. | Binary (1 = Consistently food-insecure, 0 = Newly food-insecure) |
| Recovered in March 2021 | Determined based on the responses to the U.S Household Food Security Survey Module: Six-Item Short Form. These households were food-insecure at any point since the start of the pandemic, but were food-secure in March 2021. | Binary (1 = Recovered, 0 = Still food-insecure) |
| Still food-insecure in March 2021 | Determined based on the responses to the U.S Household Food Security Survey Module: Six-Item Short Form. These households were food-insecure at any point since the start of the COVID-19 pandemic and were still food-insecure in March 2021 | Binary (1 = Still food-insecure, 0 = Recovered) |
| Age | In what year were you born? (age determined by subtracting birth year from 2020) | Continuous |
| Age (binary) | Determined based on the responses to age question | Binary (1 = 63 and over, 0 = 18–62) |
| Household size | How many people in the following age groups currently live in your household (household defined as those currently living within your household, including family and non-family members)? | Number of people in each category (under 5, 5–17, 18–65, over 65) |
| Households with children | Whether respondent indicated any children in response to household size question | Binary (1 = Yes, 0 = No) |
| Gender | Which of the following best describes your gender identity? | 1 = Male, 2 = Female, 3 = Transgender, 4 = Non-binary, 5 = Self describe |
| Gender (binary) | Determined based on the responses to gender question | Binary (1 = Female, 0 = Not female) |
| Race (binary) | Determined based on the responses to the questions "What is your race? Check all that apply" | Binary (1 = White, 0 = Non-white) |
| Ethnicity (binary) | Are you of Hispanic, Latino, or Spanish origin? | Binary (1 = Hispanic, 0 = Not Hispanic) |
| Race and ethnicity (binary) | Determined based on the responses to the race and ethnicity questions | Binary (1 = BIPOC and/or Hispanic, 0 = Non-Hispanic white) |
| Education | What is the highest level of formal education that you have? | Categorical (1 = Some high school, 2 = High school graduate/GED, 3 = Some college, 4 = Associates degree/technical school/apprenticeship, 5 = Bachelor’s degree, 6 = Postgraduate/professional degree |
| Education (binary) | Indication of associates degree/technical school/apprenticeship, bachelor’s degree, or postgraduate/professional degree in education question | Binary (1 = College degree, 0 = No college degree) |
| Household income | Which of the following best describes your household income range in 2020 before taxes? | 1 = Less than USD 10,000, 2 = USD 10,000 to 14,999, 3 = USD 15,000 to 24,999, 4 = USD 25,000 to 34,999, 5 = USD 35,000 to 49,999, 6 = USD 50,000 to 74,999, 7 = USD 75,000 to 99,999, 8 = USD 100,000 to 149,999, 9 = USD 150,000 to 199,999, 10 = USD 200,000 or more |
| Household income (binary) | Determined based on the responses to household income question | Binary (1 = USD 50,000 or more, 0 = Less than USD 50,000) |
| Rural/urban classification | Determined based on the responses to the question "What is your ZIP code?" ZIP codes were categorized using the Rural-Urban Commuting Area codes and the four-category classification scheme. | Categorical (1 = Urban, 2 = Large rural, 3 = Small rural, 4 = Isolated) |
| Rural/urban classification (binary) | Determined based on rural/urban classification variable. Rural = large rural, small rural, and isolated. | Binary (1 = Urban, 0 = Rural) |
| SNAP participation | Determined based on the responses to question "Which of the following food assistance programs did your household use? Check all that apply." In each survey, the question was asked for the following reference periods: T1: in the year prior to COVID-19; since the coronavirus outbreak (March 11th) T2: in the last 30 days T3: since the coronavirus outbreak (March 2020); in the last 30 days | Binary (1 = Yes, 0 = No) |
| WIC participation | Binary (1 = Yes, 0 = No) | |
| P-EBT participation | Binary (1 = Yes, 0 = No) | |
| School meals participation | Binary (1 = Yes, 0 = No) | |
| Food pantry participation | Binary (1 = Yes, 0 = No) | |
| Any food assistance program participation (binary) | Determined based on the responses to the questions about individual program use | Binary (1 = Yes, 0 = No) |
| Job disruption during COVID-19 pandemic | Determined based on the responses to the questions: "Have you or anyone in your household experienced a loss of income, reduction in hours, furlough, or job loss since the COVID-19 outbreak? Check all that apply" and "In which month(s) did this job disruption occur?" | Binary (1 = Yes, 0 = No) |
| Job disruption in March 2021 | Binary (1 = Yes, 0 = No) | |
| Type of job disruption | Categorical (1 = Job loss, 2 = Loss of income/hours, 3 = Furlough, 4 = Other) | |
| Length of job disruption | Continuous | |
| Received unemployment | Have you received any money from these sources since the COVID-19 outbreak? Check all that apply. | Binary (1 = Yes, 0 = No) |
| Food Security Category | |||||||
|---|---|---|---|---|---|---|---|
| Characteristic | Respondents (n = 441) | Vermont Population 1 | Food-Secure (n = 307) | Food-Insecure (n = 134) | Consistently Food-Insecure (n = 61) | Newly Food-Insecure (n = 69) | |
| no. (%) | (%) | no. (%) | |||||
| Age | 18–34 | 49 (11.1) | 27.6 | 29 (9.4) | 20 (14.9) | 11 (18.0) | 9 (13.0) |
| 35–62 | 225 (51.0) | 45.6 | 138 (45.0) | 87 (64.9) | 40 (65.6) | 47 (68.2) | |
| 63+ | 167 (37.9) | 26.8 | 140 (45.6) | 27 (20.1) | 10 (16.4) | 13 (18.8) | |
| Household size | 1–2 | 268 (62.8) | 69.3 | 208 (69.1) | 60 (47.6) | 23 (39.7) | 36 (53.7) |
| 2–4 | 126 (29.5) | 25.0 | 82 (27.2) | 44 (34.9) | 18 (31.0) | 26 (38.8) | |
| 5 or more | 33 (7.7) | 5.6 | 11 (3.7) | 22 (17.5) | 17 (29.3) | 5 (7.5) | |
| Gender | Female | 347 (79.8) | 50.7 | 231 (76.0) | 116 (88.5) | 52 (85.2) | 63 (91.3) |
| Male | 86 (19.8) | 49.3 | 71 (23.4) | 15 (11.5) | 9 (14.8) | 6 (8.7) | |
| Non-binary | 2 (0.5) | -- | 2 (0.7) | 0 (0.0) | 0 (0.0) | 0 (0.0) | |
| Transgender | 0 (0.0) | -- | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | |
| Other (self-describe) | 0 (0.0) | -- | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | |
| Race | White | 412 (97.4) | 94.2 | 292 (98.3) | 120 (95.2) | 58 (96.7) | 62 (95.4) |
| Two or more races | 4 (0.9) | 2.0 | 0 (0.0) | 4 (3.2) | 1 (1.7) | 2 (3.1) | |
| American Indian or Alaska Native | 5 (1.2) | 0.3 | 4 (1.3) | 1 (0.8) | 1 (1.7) | 0 (0.0) | |
| Asian or Pacific Islander | 0 (0.0) | 1.7 | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | |
| Black | 2 (0.5) | 1.4 | 1 (0.3) | 1 (0.8) | 0 (0.0) | 1 (1.5) | |
| Ethnicity | Not Hispanic or Latino | 423 (98.4) | 98.1 | 298 (98.7) | 125 (97.7) | 58 (96.7) | 66 (98.5) |
| Hispanic or Latino | 7 (1.6) | 1.9 | 4 (1.3) | 3 (2.3) | 2 (3.3) | 1 (1.5) | |
| Education level | Some high school (no diploma) | 1 (0.2) | 5.2 | 0 (0.0) | 1 (0.8) | 1 (1.7) | 0 (0.0) |
| High school graduate (incl. GED) | 32 (7.4) | 29.5 | 13 (4.3) | 19 (14.6) | 12 (20.0) | 7 (10.1) | |
| Some college (no degree) | 62 (14.3) | 17.5 | 28 (9.2) | 34 (26.2) | 18 (30.0) | 15 (21.7) | |
| Associate degree/technical school/apprenticeship | 33 (7.6) | 8.9 | 19 (6.3) | 15 (11.5) | 7 (11.7) | 7 (10.1 | |
| Bachelor’s degree | 149 (34.3) | 23.0 | 114 (37.5) | 35 (26.9) | 12 (20.0) | 23 (33.3) | |
| Postgraduate/professional degree | 157 (36.2) | 15.9 | 130 (42.8) | 27 (20.8) | 10 (16.7) | 17 (24.6) | |
| Household income (2020) | Less than USD 10,000 | 13 (3.1) | 4.8 | 1 (0.3) | 12 (9.6) | 8 (13.3) | 4 (6.6) |
| USD 10,000–14,999 | 25 (6.0) | 5.0 | 9 (3.1) | 16 (12.8) | 8 (13.3) | 7 (11.5) | |
| USD 15,000–24,999 | 39 (9.4) | 9.1 | 13 (4.5) | 26 (20.8) | 14 (23.3) | 11 (18.0) | |
| USD 25,000–34,999 | 40 (9.6) | 9.1 | 21 (7.2) | 19 (15.2) | 9 (15.0) | 10 (16.4) | |
| USD 35,000–49,999 | 58 (13.9) | 12.2 | 38 (13.1) | 20 (16.0) | 10 (16.7) | 9 (14.8) | |
| USD 50,000–74,999 | 71 (17.1) | 18.7 | 53 (18.2) | 18 (14.4) | 6 (10.0) | 11 (18.0) | |
| USD 75,000–99,999 | 66 (15.9) | 14.0 | 59 (20.3) | 7 (5.6) | 3 (5.0) | 4 (6.6) | |
| USD 100,000–149,999 | 66 (15.9) | 16.0 | 62 (21.3) | 4 (3.2) | 1 (1.7) | 3 (4.9) | |
| USD 150,000–199,999 | 27 (6.5) | 5.6 | 24 (8.2) | 3 (2.4) | 1 (1.7) | 2 (3.3) | |
| USD 200,000+ | 11 (2.6) | 5.5 | 11 (3.8) | 0 (0.0) | 0 (0.0) | 0 (0.0) | |
| Children in household | Yes | 127 (29.7) | 25.2 | 70 (23.3) | 57 (44.9) | 30 (51.7) | 26 (38.2) |
| No | 301 (70.3) | 74.8 | 231 (76.7) | 70 (53.4) | 28 (48.3) | 42 (61.8) | |
| Rural/urban classification | Urban | 234 (54.2) | 33.3 | 167 (55.5) | 67 (51.1) | 26 (42.6) | 40 (58.0) |
| Large rural | 60 (13.9) | 20.1 | 37 (12.3) | 23 (17.6) | 10 (16.4) | 13 (18.8) | |
| Small rural | 51 (11.8) | 18.0 | 34 (11.3) | 17 (13.0) | 10 (16.4) | 7 (10.1) | |
| Isolated | 87 (20.1) | 28.6 | 63 (20.9) | 24 (18.3) | 15 (24.6) | 9 (13.0) | |
| Variable | n | Mean | Std Error | Std Dev | 95% Confidence Interval | |
|---|---|---|---|---|---|---|
| Food-insecure previous 12 months | 432 | 0.148 | 0.017 | 0.356 | 0.115 | 0.182 |
| Food-insecure March 2020 | 427 | 0.241 | 0.021 | 0.428 | 0.200 | 0.282 |
| p = 0.0006 | ||||||
| Variable | n | Mean | Std Error | Std Dev | 95% Confidence Interval | |
|---|---|---|---|---|---|---|
| Food-insecure March 2020 | 427 | 0.241 | 0.021 | 0.428 | 0.200 | 0.282 |
| Food-insecure May/June 2020 | 436 | 0.174 | 0.018 | 0.380 | 0.139 | 0.210 |
| p = 0.0153 | ||||||
| Variable | n | Mean | Std Error | Std Dev | 95% Confidence Interval | |
|---|---|---|---|---|---|---|
| Food-insecure March 2020 | 427 | 0.241 | 0.021 | 0.428 | 0.200 | 0.282 |
| Food-insecure March 2021 | 428 | 0.182 | 0.019 | 0.386 | 0.146 | 0.219 |
| p = 0.0348 | ||||||
| Variable | n | Mean | Std Error | Std Dev | 95% Confidence Interval | |
|---|---|---|---|---|---|---|
| Food-insecure previous 12 months | 432 | 0.148 | 0.017 | 0.356 | 0.115 | 0.182 |
| Food-insecure March 2021 | 428 | 0.182 | 0.019 | 0.386 | 0.146 | 0.219 |
| p = 0.1786 | ||||||
| Variable | n | Mean | Std Error | Std Dev | 95% Confidence Interval | |
|---|---|---|---|---|---|---|
| Food-secure | 307 | 0.459 | 0.028 | 0.499 | 0.403 | 0.515 |
| Food-insecure | 134 | 0.731 | 0.038 | 0.445 | 0.655 | 0.807 |
| p = 0.0000 | ||||||
| Variable | n | Mean | Std Error | Std Dev | 95% Confidence Interval | |
|---|---|---|---|---|---|---|
| Food-secure | 306 | 0.144 | 0.020 | 0.351 | 0.104 | 0.183 |
| Food-insecure | 130 | 0.285 | 0.040 | 0.453 | 0.206 | 0.363 |
| p = 0.0005 | ||||||
| Variable | n | Mean | Std Error | Std Dev | 95% Confidence Interval | |
|---|---|---|---|---|---|---|
| Food-secure | 298 | 0.198 | 0.023 | 0.399 | 0.152 | 0.243 |
| Food-insecure | 123 | 0.317 | 0.042 | 0.467 | 0.234 | 0.400 |
| p = 0.0085 | ||||||
| Variable | n | Mean | Std Error | Std Dev | 95% Confidence Interval | |
|---|---|---|---|---|---|---|
| First year of COVID-19 pandemic | 438 | 0.073 | 0.012 | 0.261 | 0.049 | 0.098 |
| March 2021 | 438 | 0.037 | 0.009 | 0.188 | 0.019 | 0.054 |
| p = 0.0175 | ||||||
| Variable | n | Mean | Std Error | Std Dev | 95% Confidence Interval | |
|---|---|---|---|---|---|---|
| Food-secure | 306 | 0.163 | 0.021 | 0.370 | 0.122 | 0.205 |
| Food-insecure | 132 | 0.674 | 0.041 | 0.470 | 0.593 | 0.755 |
| p = 0.0000 | ||||||
References
- USDA. Food Security in the U.S.: Overview. Available online: https://www.ers.usda.gov/topics/food-nutrition-assistance/food-security-in-the-us/ (accessed on 22 September 2021).
- Coleman-Jensen, A.; Rabbitt, M.P.; Gregory, C.A.; Singh, A. Household Food Security in the United States in 2019; U.S. Department of Agriculture, Economic Research Service: Washington, DC, USA, 2020.
- Huang, J.; Birkenmaier, J.; Kim, Y. Unemployment and household food hardship in the economic recession. Public Health Nutr. 2016, 19, 511–519. [Google Scholar] [CrossRef] [PubMed]
- Nord, M.; Coleman-Jensen, A.; Gregory, C. Prevalence of U.S. Food Insecurity is Related to Changes in Unemployment, Inflation, and the Price of Food; U.S. Department of Agriculture, Economic Research Service: Washington, DC, USA, 2014.
- Beaulac, J.; Kristjansson, E.; Cummins, S. A Systematic Review of Food Deserts, 1966–2007. Prev. Chronic. Dis. 2009, 6, 105. [Google Scholar]
- Powell, L.M.; Slater, S.; Mirtcheva, D.; Bao, Y.; Chaloupka, F.J. Food store availability and neighborhood characteristics in the United States. Prev. Med. 2007, 44, 189–195. [Google Scholar] [CrossRef]
- Ver Ploeg, M.; Breneman, V.; Farrigan, T.; Hamrick, K.; Hopkins, D.; Kaufman, P.; Lin, B.H.; Nord, M.; Smith, T.; Williams, R.; et al. Access to Affordable and Nutritious Food: Measuring and Understanding Food Deserts and Their Consequences; U.S. Department of Agriculture, Economic Research Service: Washington, DC, USA, 2009; p. 160.
- Garcia, S.P.; Haddix, A.; Barnett, K. Incremental Health Care Costs Associated with Food Insecurity and Chronic Conditions Among Older Adults. Prev. Chronic. Dis. 2018, 15, 108. [Google Scholar] [CrossRef]
- Gundersen, C.; Tarasuk, V.; Cheng, J.; de Oliveira, C.; Kurdyak, P. Food insecurity status and mortality among adults in Ontario, Canada. PLoS ONE 2018, 13, 1–10. [Google Scholar] [CrossRef]
- Gundersen, C.; Ziliak, J.P. Food Insecurity And Health Outcomes. Health Aff. Millwood 2015, 34, 1830–1839. [Google Scholar] [CrossRef] [PubMed]
- Seligman, H.K.; Laraia, B.A.; Kushel, M.B. Food Insecurity is Associated with Chronic Disease among Low-Income NHANES Participants. J. Nutr. 2010, 140, 304–310. [Google Scholar] [CrossRef]
- Walker, R.J.; Chawla, A.; Garacci, E.; Williams, J.S.; Mendez, C.; Ozieh, M.N.; Egede, L.E. Assessing the relationship between food insecurity and mortality among U.S. adults. Ann. Epidemiol. 2019, 32, 43–48. [Google Scholar] [CrossRef]
- Hanson, K.L.; Connor, L.M. Food insecurity and dietary quality in US adults and children: A systematic review. Am. J. Clin. Nutr. 2014, 100, 684–692. [Google Scholar] [CrossRef]
- Niles, M.T.; Wirkkala, K.B.; Belarmino, E.H.; Bertmann, F. Home food procurement impacts food security and diet quality during COVID-19. BMC Public Health 2021, 21, 945. [Google Scholar] [CrossRef]
- Berkowitz, S.A.; Basu, S.; Meigs, J.B.; Seligman, H.K. Food insecurity and health care expenditures in the United States, 2011–2013. Health Serv. Res. 2017, 53, 1600–1620. [Google Scholar] [CrossRef] [PubMed]
- Berkowitz, S.A.; Seligman, H.K.; Meigs, J.B.; Basu, S. Food insecurity, healthcare utilization, and high cost: A longitudinal cohort study. Am. J. Manag. Care 2018, 24, 399. [Google Scholar] [PubMed]
- Tarasuk, V.; Cheng, J.; de Oliveira, C.; Dachner, N.; Gundersen, C.; Kurdyak, P. Association between household food insecurity and annual health care costs. Can. Med. Assoc. J. 2015, 187, 429–436. [Google Scholar] [CrossRef]
- Burke, M.P.; Martini, L.H.; Çayır, E.; Hartline-Grafton, H.L.; Meade, R.L. Severity of Household Food Insecurity Is Positively Associated with Mental Disorders among Children and Adolescents in the United States. J. Nutr. 2016, 146, 2019–2026. [Google Scholar] [CrossRef] [PubMed]
- Kimbro, R.T.; Denney, J.T. Transitions into Food Insecurity Associated With Behavioral Problems and Worse Overall Health Among Children. Health Aff. Millwood 2015, 34, 1949–1955. [Google Scholar] [CrossRef]
- Adams, E.L.; Caccavale, L.J.; Smith, D.; Bean, M.K. Longitudinal patterns of food insecurity, the home food environment, and parent feeding practices during COVID-19. Obes. Sci. Pract. 2021, 7, 415–424. [Google Scholar] [CrossRef]
- Niles, M.T.; Bertmann, F.; Belarmino, E.H.; Wentworth, T.; Biehl, E.; Neff, R. The early food insecurity impacts of COVID-19. Nutrients 2020, 12, 2096. [Google Scholar]
- Wolfson, J.A.; Leung, C.W. Food insecurity and COVID-19: Disparities in early effects for US adults. Nutrients 2020, 12, 1648. [Google Scholar]
- Rogers, A.M.; Lauren, B.N.; Woo Baidal, J.A.; Ozanne, E.M.; Hur, C. Persistent effects of the COVID-19 pandemic on diet, exercise, risk for food insecurity, and quality of life: A longitudinal study among U.S. adults. Appetite 2021, 167, 105639. [Google Scholar] [CrossRef]
- Menasce Horowitz, J.; Brown, A.; Minkin, R. The COVID-19 Pandemic’s Long-Term Financial Impact; Pew Research Center: Washington, DC, USA, 2021. [Google Scholar]
- US Census Bureau. U.S. Census Bureau Household Pulse Survey Data Tables. Available online: https://www.census.gov/programs-surveys/household-pulse-survey/data.html (accessed on 28 September 2021).
- US Census Bureau. Urban and Rural; US Census Bureau: Washington, DC, USA, 2010.
- Niles, M.T.; Neff, R.; Biehl, E.; Bertmann, F.; Morgan, E.H.; Wentworth, T. Food Access and Security during Coronavirus Survey—Version 1.0; University of Vermont: Burlington, VT, USA; Johns Hopkins University: Baltimore, MD, USA, 2020. [Google Scholar]
- Engard, N.C. LimeSurvey; Public Service Q: Hamburg, Germany, 2009. [Google Scholar]
- Front Porch Forum Paid. Campaign Posting. Available online: https://frontporchforum.com/advertise-on-fpf/pcp (accessed on 22 September 2021).
- Qualtrics; Qualtrics: Provo, UT, USA, 2021.
- USDA. U.S. Household Food Security Module: Six-Item Short Form 2012. Available online: https://www.ers.usda.gov/media/8282/short2012.pdf (accessed on 22 September 2021).
- USDA. Rural-Urban Commuting Area Codes. Available online: https://www.ers.usda.gov/data-products/rural-urban-commuting-area-codes.aspx (accessed on 22 September 2021).
- Rural Health Research Center. Map Classification. Available online: http://depts.washington.edu/uwruca/ruca-maps.php (accessed on 22 September 2021).
- StataCorp LLC. StataCorp Stata Statistical Software: Release 17; StataCorp LLC: College Station, TX, USA, 2021. [Google Scholar]
- Coleman-Jensen, A.; Rabbitt, M.P.; Gregory, C.A.; Singh, A. Household Food Security in the United States in 2020; U.S. Department of Agriculture, Economic Research Service: Washington, DC, USA, 2021; p. 55.
- Fitzpatrick, K.M.; Harris, C.; Drawve, G.; Willis, D.E. Assessing Food Insecurity among US Adults during the COVID-19 Pandemic. J. Hunger Environ. Nutr. 2021, 16, 1–18. [Google Scholar] [CrossRef]
- Parekh, N.; Ali, S.H.; O’Connor, J.; Tozan, Y.; Jones, A.M.; Capasso, A.; Foreman, J.; DiClemente, R.J. Food insecurity among households with children during the COVID-19 pandemic: Results from a study among social media users across the United States. Nutr. J. 2021, 20, 1–11. [Google Scholar] [CrossRef]
- Balasuriya, L.; Berkowitz, S.A.; Seligman, H.K. Federal Nutrition Programs after the Pandemic: Learning from P-EBT and SNAP to Create the Next Generation of Food Safety Net Programs. Inq. J. Med. Care Organ. Provis. Financ. 2021, 58, 469580211005190. [Google Scholar] [CrossRef]
- Chen, E.; Martin, A.D.; Matthews, K.A. Understanding Health Disparities: The Role of Race and Socioeconomic Status in Children’s Health. Am. J. Public Health 2006, 96, 702–708. [Google Scholar] [CrossRef] [PubMed]
- Clay, L.A.; Rogus, S. Primary and Secondary Health Impacts of COVID-19 among Minority Individuals in New York State. Int. J. Environ. Res. Public. Health 2021, 18, 683. [Google Scholar] [CrossRef]
- Williams, D.R.; Mohammed, S.A.; Leavell, J.; Collins, C. Race, Socioeconomic Status and Health: Complexities, Ongoing Challenges and Research Opportunities. Ann. N. Y. Acad. Sci. 2010, 1186, 69–101. [Google Scholar] [CrossRef]
- Kaiser, L. Why do low-income women not use food stamps? Findings from the California Women’s Health Survey. Public Health Nutr. 2008, 11, 1288–1295. [Google Scholar] [CrossRef]
- Pinard, C.A.; Bertmann, F.M.W.; Byker Shanks, C.; Schober, D.J.; Smith, T.M.; Carpenter, L.C.; Yaroch, A.L. What Factors Influence SNAP Participation? Literature Reflecting Enrollment in Food Assistance Programs from a Social and Behavioral Science Perspective. J. Hunger Environ. Nutr. 2017, 12, 151–168. [Google Scholar] [CrossRef]
- LendingClub Reality Check: The Paycheck-To-Paycheck Report; LendingClub Corporation: San Francisco, CA, USA, 2021.
- U.S. Department of Agriculture, Economic Research Service. Does SNAP Decrease Food Insecurity? Untangling the Self-Selection Effect; US Department of Agriculture, Economic Research Service: Washington, DC, USA, 2009.
- Wilde, P.E. Measuring the Effect of Food Stamps on Food Insecurity and Hunger: Research and Policy Considerations. J. Nutr. 2007, 137, 307–310. [Google Scholar] [CrossRef]
- Balistreri, K.S. A Decade of Change: Measuring the Extent, Depth and Severity of Food Insecurity. J. Fam. Econ. Issues 2016, 37, 373–382. [Google Scholar] [CrossRef][Green Version]
- USDA. Food Price Outlook, 2021; U.S. Department of Agriculture, Economic Research Service: Washington, DC, USA, 2021.
- USDA. USDA Modernizes the Thrifty Food Plan, Updates SNAP Benefits. Available online: https://www.usda.gov/media/press-releases/2021/08/16/usda-modernizes-thrifty-food-plan-updates-snap-benefits (accessed on 22 September 2021).
- Feeding America Map the Meal Gap 2019. Available online: https://www.feedingamerica.org/sites/default/files/2019-04/2017-map-the-meal-gap-technical-brief.pdf (accessed on 13 July 2020).
- WCAX. People Stocking Up on Toilet Paper; Shelves Empty. Available online: https://www.wcax.com/content/news/People-stocking-up-on-568696561.html (accessed on 13 July 2020).
- US Census Bureau. CP02: Comparative Social Characteristics in the United States. Available online: https://data.census.gov/cedsci/profile?g=0400000US50 (accessed on 5 October 2021).
| Food Security Category | |||||||
|---|---|---|---|---|---|---|---|
| Characteristic | Respondents (n = 441) | Vermont Population 1 | Food-Secure (n = 307) | Food-Insecure (n = 134) | Consistently Food-Insecure (n = 61) | Newly Food-Insecure (n = 69) | |
| no. (%) | (%) | no. (%) | |||||
| Age | 18 to 62 | 274 (62.1) | 73.2 | 167 (54.4) | 107 (79.9) | 51 (83.6) | 56 (81.2) |
| 63 and over | 167 (37.9) | 26.8 | 140 (45.6) | 27 (20.1) | 10 (16.4) | 13 (18.8) | |
| Gender | Female | 347 (79.8) | 50.7 | 231 (76.0) | 116 (88.5) | 52 (85.2) | 63 (91.3) |
| Not female | 88 (20.2) | 49.3 | 73 (24.0) | 15 (11.5) | 9 (14.8) | 6 (8.7) | |
| Race and ethnicity | White, non-Hispanic | 407 (96.0) | 92.6 | 289 (97.3) | 118 (92.9) | 56 (93.3) | 62 (93.9) |
| BIPOC and/or Hispanic | 17 (4.0) | 7.4 | 8 (2.7) | 9 (7.1) | 4 (6.7) | 4 (6.1) | |
| Education level | No college degree | 95 (21.9) | 52.2 | 41 (13.5) | 54 (41.2) | 31 (51.7) | 22 (31.9) |
| College degree | 339 (78.1) | 47.8 | 263 (86.5) | 77 (58.8) | 29 (48.3) | 47 (68.1) | |
| Household income (2020) | Less than USD 50,000 | 175 (42.1) | 40.2 | 82 (28.2) | 93 (74.4) | 49 (81.7) | 41 (67.2) |
| USD 50,000 or more | 241 (57.9) | 59.8 | 209 (71.8) | 32 (25.6) | 11 (18.3) | 20 (32.8) | |
| Children in household | Yes | 127 (29.7) | 25.2 | 70 (23.3) | 57 (44.9) | 30 (51.7) | 26 (38.2) |
| No | 301 (70.3) | 74.8 | 231 (76.7) | 70 (53.4) | 28 (48.3) | 42 (61.8) | |
| Rural/urban classification | Urban | 234 (54.2) | 33.3 | 167 (55.5) | 67 (51.1) | 26 (42.6) | 40 (58.0) |
| Rural | 198 (45.8) | 66.7 | 134 (44.5) | 64 (48.9) | 35 (57.4) | 29 (42.0) | |
| Time Period | Food-Insecure (%) |
|---|---|
| Year prior to COVID-19 | 14.8 |
| Anytime during COVID-19 | 31.6 |
| March 2020 | 24.1 |
| May/June 2020 | 17.4 |
| July 2020–February 2021 | 20.8 |
| March 2021 | 18.2 |
| Food Security Category | ||||||
|---|---|---|---|---|---|---|
| Variable | All Respondents | Food- Secure | Food- Insecure | Consistently Food-Insecure | Newly Food-Insecure | |
| % | ||||||
| Any job disruption during COVID-19 pandemic | 54.2 | 45.9 | 73.1 | 78.7 | 68.1 | |
| Experiencing a job disruption in March 2021 | 18.7 | 14.4 | 28.5 | 33.3 | 25.8 | |
| Type of job disruption 1,2 | ||||||
| Job loss | 45.6 | 39.7 | 54.1 | 62.5 | 44.7 | |
| Loss of income/hours | 70.7 | 73.8 | 66.3 | 64.6 | 70.2 | |
| Furloughed | 25.1 | 28.4 | 20.4 | 18.8 | 21.3 | |
| Other | 18.4 | 16.3 | 21.4 | 22.9 | 19.1 | |
| Length of job disruption 1 | ||||||
| Less than 3 months | 45.6 | 48.6 | 41.2 | 35.4 | 47.8 | |
| 3–6 months | 19.8 | 19.3 | 20.6 | 22.9 | 15.2 | |
| More than 6 months | 35.6 | 32.1 | 38.1 | 41.7 | 37.0 | |
| Received unemployment | 23.3 | 19.8 | 31.7 | 36.8 | 26.2 | |
| Used any food assistance program 3 | 31.7 | 16.3 | 67.4 | 73.8 | 59.7 | |
| Variable | Odds Ratio | Standard Error | p = | 95% Confidence Interval | ||
|---|---|---|---|---|---|---|
| Race/ethnicity | ||||||
| Non-Hispanic White | ----------------------reference--------------------- | |||||
| BIPOC and/or Hispanic | 11.771 | 11.930 | 0.015 * | 1.615 | 85.805 | |
| Gender | ||||||
| Not female | ----------------------reference--------------------- | |||||
| Female | 8.070 | 6.230 | 0.007 ** | 1.777 | 36.647 | |
| Age | ||||||
| 18–62 | ----------------------reference--------------------- | |||||
| 63 and over | 0.046 | 0.032 | <0.001 *** | 0.012 | 0.180 | |
| Households with children | ||||||
| No | ----------------------reference--------------------- | |||||
| Yes | 5.494 | 3.156 | 0.003 ** | 1.782 | 16.936 | |
| Income | ||||||
| Under USD 50,000 | ----------------------reference--------------------- | |||||
| USD 50,000 or more | 0.010 | 0.007 | <0.001 *** | 0.003 | 0.038 | |
| Education | ||||||
| No college degree | ----------------------reference--------------------- | |||||
| College degree | 0.078 | 0.046 | <0.001 *** | 0.025 | 0.246 | |
| Rural/urban category | ||||||
| Rural | ----------------------reference--------------------- | |||||
| Urban | 0.668 | 0.365 | 0.461 | 0.229 | 1.948 | |
| Job disruption during COVID-19 | ||||||
| No | ----------------------reference--------------------- | |||||
| Yes | 5.034 | 2.971 | 0.006 ** | 1.583 | 16.005 | |
| Survey occasion | ||||||
| Survey 1 | ----------------------reference--------------------- | |||||
| Survey 2 | 0.249 | 0.082 | <0.001 *** | 0.131 | 0.474 | |
| Survey 3 | 0.522 | 0.171 | 0.048 * | 0.274 | 0.993 | |
| Variable | Odds Ratio | Standard Error | p = | 95% Confidence Interval | ||
|---|---|---|---|---|---|---|
| Race/ethnicity | ||||||
| Non-Hispanic White | ----------------------reference--------------------- | |||||
| BIPOC and/or Hispanic | 1.168 | 0.976 | 0.853 | 0.227 | 6.009 | |
| Gender | ||||||
| Not female | ----------------------reference--------------------- | |||||
| Female | 2.232 | 1.507 | 0.234 | 0.594 | 8.382 | |
| Age | ||||||
| 18–62 | ----------------------reference--------------------- | |||||
| 63 and older | 1.021 | 0.620 | 0.973 | 0.310 | 3.360 | |
| Households with children | ||||||
| No | ----------------------reference--------------------- | |||||
| Yes | 0.547 | 0.276 | 0.232 | 0.203 | 1.473 | |
| Income | ||||||
| Under USD 50,000 | ----------------------reference--------------------- | |||||
| USD 50,000 or more | 1.564 | 0.829 | 0.399 | 0.553 | 4.421 | |
| Education | ||||||
| No college degree | ----------------------reference--------------------- | |||||
| College degree | 1.969 | 0.853 | 0.118 | 0.843 | 4.602 | |
| Rural/urban category | ||||||
| Rural | ----------------------reference--------------------- | |||||
| Urban | 1.875 | 0.796 | 0.139 | 0.816 | 4.310 | |
| Any job disruption during COVID-19 | ||||||
| No | ----------------------reference--------------------- | |||||
| Yes | 0.547 | 0.276 | 0.232 | 0.204 | 1.471 | |
| Unemployment insurance | ||||||
| No | ----------------------reference--------------------- | |||||
| Yes | 0.950 | 0.440 | 0.912 | 0.384 | 2.353 | |
| Food assistance program use | ||||||
| No | ----------------------reference--------------------- | |||||
| Yes | 0.801 | 0.411 | 0.666 | 0.293 | 2.192 | |
| Variable | Odds Ratio | Standard Error | p = | 95% Confidence Interval | ||
|---|---|---|---|---|---|---|
| Race/ethnicity | ||||||
| Non-Hispanic White | ----------------------reference--------------------- | |||||
| BIPOC and/or Hispanic | 0.897 | 0.746 | 0.896 | 0.176 | 4.581 | |
| Gender | ||||||
| Not female | ----------------------reference--------------------- | |||||
| Female | 1.055 | 0.703 | 0.935 | 0.286 | 3.895 | |
| Age | ||||||
| 18–62 | ----------------------reference--------------------- | |||||
| 63 and over | 1.092 | 0.686 | 0.889 | 0.319 | 3.743 | |
| Households with children | ||||||
| No | ----------------------reference--------------------- | |||||
| Yes | 0.677 | 0.370 | 0.475 | 0.232 | 1.976 | |
| Income | ||||||
| Under USD 50,000 | ----------------------reference--------------------- | |||||
| USD 50,000 or more | 2.288 | 1.232 | 0.124 | 0.797 | 6.573 | |
| Education | ||||||
| No college degree | ----------------------reference--------------------- | |||||
| College degree | 0.914 | 0.403 | 0.838 | 0.385 | 2.168 | |
| Rural/urban category | ||||||
| Rural | ----------------------reference--------------------- | |||||
| Urban | 1.471 | 0.645 | 0.378 | 0.623 | 3.474 | |
| Any job disruption during COVID-19 | ||||||
| No | ----------------------reference--------------------- | |||||
| Yes | 1.551 | 0.848 | 0.422 | 0.531 | 4.526 | |
| Experiencing a job disruption in March 2021 | ||||||
| No | ----------------------reference--------------------- | |||||
| Yes | 0.398 | 0.210 | 0.080 | 0.142 | 1.117 | |
| Unemployment insurance | ||||||
| No | ----------------------reference--------------------- | |||||
| Yes | 1.705 | 0.817 | 0.265 | 0.667 | 4.359 | |
| Food assistance program use | ||||||
| No | ----------------------reference--------------------- | |||||
| Yes | 0.833 | 0.455 | 0.738 | 0.286 | 2.427 | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
McCarthy, A.C.; Belarmino, E.H.; Bertmann, F.; Niles, M.T. Food Security Impacts of the COVID-19 Pandemic: Longitudinal Evidence from a Cohort of Adults in Vermont during the First Year. Nutrients 2022, 14, 1358. https://doi.org/10.3390/nu14071358
McCarthy AC, Belarmino EH, Bertmann F, Niles MT. Food Security Impacts of the COVID-19 Pandemic: Longitudinal Evidence from a Cohort of Adults in Vermont during the First Year. Nutrients. 2022; 14(7):1358. https://doi.org/10.3390/nu14071358
Chicago/Turabian StyleMcCarthy, Ashley C., Emily H. Belarmino, Farryl Bertmann, and Meredith T. Niles. 2022. "Food Security Impacts of the COVID-19 Pandemic: Longitudinal Evidence from a Cohort of Adults in Vermont during the First Year" Nutrients 14, no. 7: 1358. https://doi.org/10.3390/nu14071358
APA StyleMcCarthy, A. C., Belarmino, E. H., Bertmann, F., & Niles, M. T. (2022). Food Security Impacts of the COVID-19 Pandemic: Longitudinal Evidence from a Cohort of Adults in Vermont during the First Year. Nutrients, 14(7), 1358. https://doi.org/10.3390/nu14071358






