A Decentralized Study Setup Enables to Quantify the Effect of Polymerization and Linkage of α-Glucans on Post-Prandial Glucose Response
Abstract
:1. Introduction
2. Materials and Methods
2.1. Samples
2.2. In-Vivo Study
2.3. Technical Aspects of Decentralization
2.4. Data Analyses
3. Results
3.1. Post-Prandial Glucose Response
3.2. Gastrointestinal Tolerance
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organisation. Guideline: Sugars Intake for Adults and Children; World Health Organisation: Geneva, Switzerland, 2015. [Google Scholar]
- Barclay, A.W.; Petocz, P.; McMillan-Price, J.; Flood, V.M.; Prvan, T.; Mitchell, P.; Brand-Miller, J.C. Glycemic index, glycemic load, and chronic disease risk—A metaanalysis of observational studies. Am. J. Clin. Nutr. 2008, 87, 627–637. [Google Scholar] [CrossRef] [PubMed]
- Mirrahimi, A.; Chiavaroli, L.; Srichaikul, K.; Augustin, L.S.A.; Sievenpiper, J.L.; Kendall, C.W.C.; Jenkins, D.J.A. The role of glycemic index and glycemic load in cardiovascular disease and its risk factors: A review of the recent literature. Curr. Atheroscler. Rep. 2014, 16, 380. [Google Scholar] [CrossRef] [PubMed]
- Brand-Miller, J.; Hayne, S.; Petocz, P.; Colagiuri, S. Low-glycemic index diets in the management of diabetes: A meta-analysis of randomized controlled trials. Diabetes Care 2003, 26, 2261–2267. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rytz, A.; Adeline, D.; Lê, K.-A.; Tan, D.; Lamothe, L.; Roger, O.; Macé, K. Predicting Glycemic Index and Glycemic Load from Macronutrients to Accelerate Development of Foods and Beverages with Lower Glucose Responses. Nutrients 2019, 11, 1172. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Magallanes-Cruz, P.A.; Flores-Silva, P.C.; Bello-Perez, L.A. Starch structure influences its digestibility: A review. J. Food Sci. 2017, 82, 2016–2023. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gangoiti, J.; Corwin, S.F.; Lamothe, L.M.; Vafiadi, C.; Hamaker, B.R.; Dijkhuizen, L. Synthesis of novel α-glucans with potential health benefits through controlled glucose release in the human gastrointestinal tract. Crit. Rev. Food Sci. Nutr. 2020, 60, 123–146. [Google Scholar] [CrossRef] [PubMed]
- Khozin, S.; Coravos, A. Decentralized Trials in the Age of Real-World Evidence and Inclusivity in Clinical Investigations. Clin. Pharmacol. Ther. 2019, 106, 25–27. [Google Scholar] [CrossRef] [PubMed]
- Van Norman, G.A. Decentralized Clinical Trials the Future of Medical Product Development? JACC Basic Transl. Sci. 2021, 6, 384–387. [Google Scholar] [CrossRef] [PubMed]
- Blum, A. Freestyle libre glucose monitoring system. Clin. Diabetes 2018, 36, 203–204. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Williams, E.J. Experimental Designs Balanced for the Estimation of Residual Effects of Treatments. Aust. J. Sci. Res. 1949, 2, 149–168. [Google Scholar] [CrossRef]
- International Standard Organization. Food Products-Determination of the Glycaemic Index (GI) and Recommendation for Food Classification; ISO 26642:2010(E); International Standard Organization: Geneva, Switzerland, 2010. [Google Scholar]
- Senn, S. Cross-Over Trials in Clinical Research; John Wiley & Sons: Hoboken, NJ, USA, 2002. [Google Scholar]
- Trumbo, P.; Schlicker, S.; Yates, A.; Poos, M. Nutrition Board of the Institute of Medicine TNA. Dietary reference intakes for energy, carbohydrate, fiber, fat, fatty acids, cholesterol, protein and amino acids. J. Am. Diet. Assoc. 2002, 102, 1621–1630. [Google Scholar] [CrossRef]
- Castro, J.P.; El-Atat, F.A.; McFarlane, S.I.; Aneja, A.; Sowers, J.R. Cardiometabolic syndrome: Pathophysiology and treatment. Curr. Hypertens. Rep. 2003, 5, 393–401. [Google Scholar] [CrossRef] [PubMed]
- Saavedra-Leos, Z.; Leyva-Porras, C.; Araujo-Díaz, S.B.; Toxqui-Terán, A.; Borrás-Enríquez, A.J. Technological application of maltodextrins according to the degree of polymerization. Molecules 2015, 20, 21067–21081. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hofman, D.L.; van Buul, V.J.; Brouns, F.J.P.H. Nutrition, Health, and Regulatory Aspects of Digestible Maltodextrins. Crit. Rev. Food Sci. Nutr. 2016, 56, 2091–2100. [Google Scholar] [CrossRef] [PubMed]
- Canene-Adams, K.; Spence, L.; Kolberg, L.W.; Karnik, K.; Liska, D.; Mah, E. A Randomized, Double-Blind, Crossover Study to Determine the Available Energy from Soluble Fiber. J. Am. Coll. Nutr. 2021, 40, 412–418. [Google Scholar] [CrossRef] [PubMed]
- Wolf, B.W.; Garleb, K.A.; Choe, Y.S.; Humphrey, P.M.; Maki, K.C. Pullulan is a slowly digested carbohydrate in humans. J. Nutr. 2003, 133, 1051–1055. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Spears, J.K.; Karr-Lilienthal, L.K.; Grieshop, C.M.; Flickinger, E.A.; Wolf, B.W.; Fahey, G.C. Glycemic, insulinemic, and breath hydrogen responses to pullulan in healthy humans. Nutr. Res. 2005, 25, 1029–1041. [Google Scholar] [CrossRef]
- Zhu, F. Relationships between amylopectin internal molecular structure and physicochemical properties of starch. Trends Food Sci. Technol. 2018, 78, 234–242. [Google Scholar] [CrossRef]
- Korompokis, K.; Verbeke, K.; Delcour, J.A. Structural factors governing starch digestion and glycemic responses and how they can be modified by enzymatic approaches: A review and a guide. Compr. Rev. Food Sci. Food Saf. 2021, 20, 5965–5991. [Google Scholar] [CrossRef] [PubMed]
| Name | Glycosidic Bonds | DP | Commercial Name |
|---|---|---|---|
| Dextrin DP 3 Dextrin DP 60 | α-1,4 α-1,4 | 3 60 | Roquette Glucidex 40 Roquette Glucidex 2 |
| Dextran DP 60 Resistant Dextrin | α-1,6 - | 60 ~5 | Pharmacosmos Dextran 10 Promitor 70 |
| Purpose | Technical Means |
|---|---|
| Recruitment and enrolment At-home consent discussion Product and material delivery Continuous glucose monitoring Safety oversight Product tolerance Product compliance Procedure compliance | Internal social media (Workplace) Skype meeting National mailing service (La Poste) Abbott, Freestyle Libre (with offline reader) ePRO ePRO ePRO ePRO |
| Data reconciliation and aggregation | SAS® Life Science Analytics Framework (LSAF) |
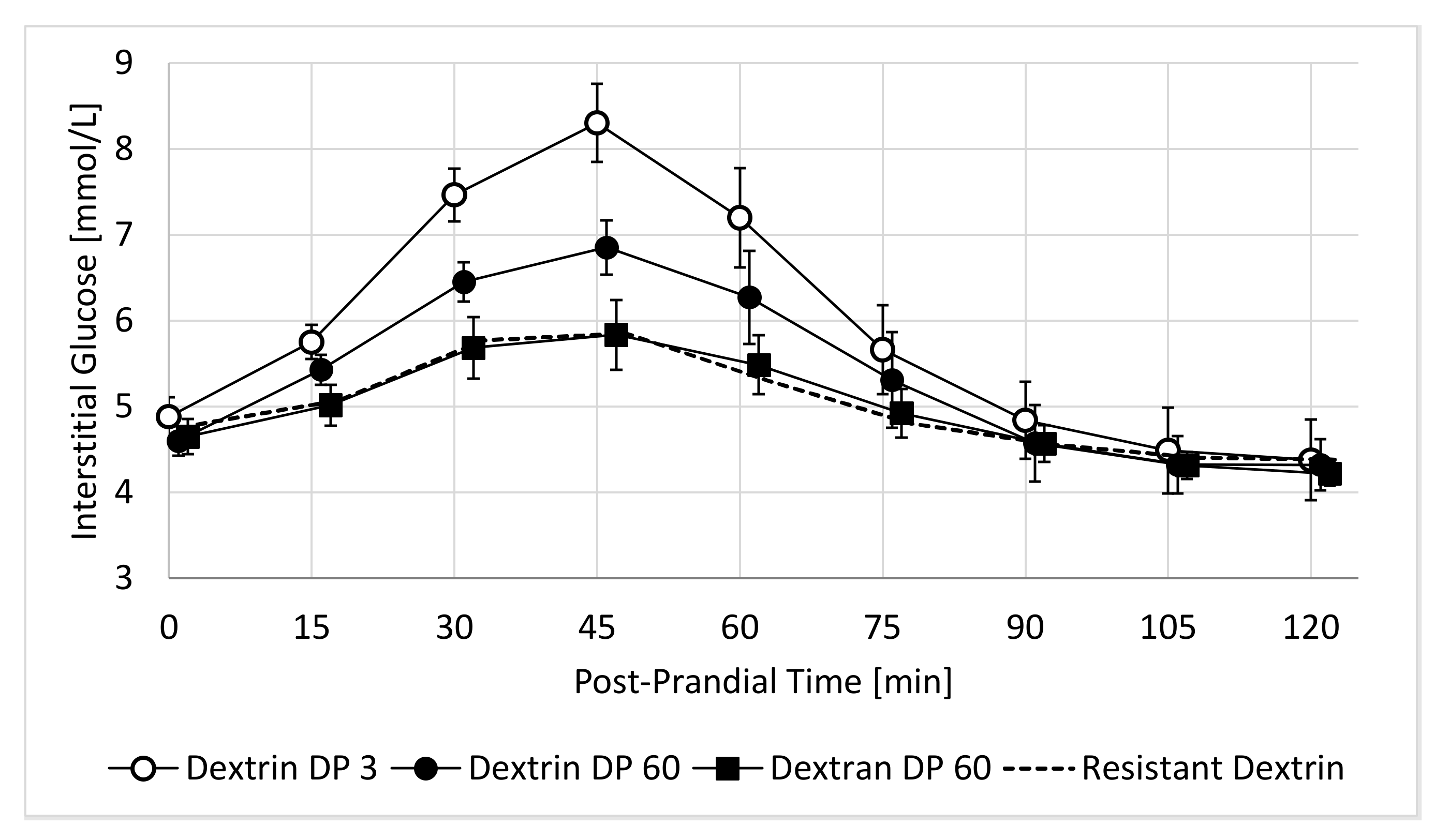
| Endpoint | Dextrin DP 3 | Dextrin DP 60 | Dextran DP60 | Resistant Dextrin |
|---|---|---|---|---|
| 2h-iAUC [mmol/L × min] iCmax [mmol/L] Tmax [min] | 163 ± 27 3.5 ± 0.36 46 ± 2.7 | 123 ± 15 (p = 0.208) 2.5 ± 0.23 (p = 0.019) 43 ± 4.2 (p = 0.555) | 67 ± 14 (p = 0.002) 1.3 ± 0.27 (p < 0.001) 38 ± 4.6 (p = 0.168) | 52 ± 13 (p = 0.002) 1.2 ± 0.19 (p < 0.001) 38 ± 3.4 (p = 0.051) |
| Endpoint | Dextrin DP 3 | Dextrin DP 60 | Dextran DP 60 | Resistant Dextrin |
|---|---|---|---|---|
| Abdominal discomfort Decreased appetite Gastric reflux Nausea Diarrhea Headache | 0 0 0 0 1 0 | 1 0 0 1 0 4 | 0 0 0 0 1 1 | 0 0 1 1 2 0 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Delodder, F.; Rytz, A.; Foltzer, F.; Lamothe, L.; d’Urzo, C.; Feraille-Naze, L.; Mauger, J.; Morlet, J.; Piccardi, N.; Philippe, L.; et al. A Decentralized Study Setup Enables to Quantify the Effect of Polymerization and Linkage of α-Glucans on Post-Prandial Glucose Response. Nutrients 2022, 14, 1123. https://doi.org/10.3390/nu14051123
Delodder F, Rytz A, Foltzer F, Lamothe L, d’Urzo C, Feraille-Naze L, Mauger J, Morlet J, Piccardi N, Philippe L, et al. A Decentralized Study Setup Enables to Quantify the Effect of Polymerization and Linkage of α-Glucans on Post-Prandial Glucose Response. Nutrients. 2022; 14(5):1123. https://doi.org/10.3390/nu14051123
Chicago/Turabian StyleDelodder, Frederik, Andreas Rytz, Fabien Foltzer, Lisa Lamothe, Carmine d’Urzo, Ludivine Feraille-Naze, Julia Mauger, Justine Morlet, Nathalie Piccardi, Lionel Philippe, and et al. 2022. "A Decentralized Study Setup Enables to Quantify the Effect of Polymerization and Linkage of α-Glucans on Post-Prandial Glucose Response" Nutrients 14, no. 5: 1123. https://doi.org/10.3390/nu14051123
APA StyleDelodder, F., Rytz, A., Foltzer, F., Lamothe, L., d’Urzo, C., Feraille-Naze, L., Mauger, J., Morlet, J., Piccardi, N., Philippe, L., Caijo, F., Schmitt, J., & Colombo Mottaz, S. (2022). A Decentralized Study Setup Enables to Quantify the Effect of Polymerization and Linkage of α-Glucans on Post-Prandial Glucose Response. Nutrients, 14(5), 1123. https://doi.org/10.3390/nu14051123






