Longer Participation in the Special Supplemental Nutrition Program for Women, Infants, and Children Is Not Associated with Reduced Sugar-Sweetened Beverage Intake among Black Participants
Abstract
:1. Introduction
2. Materials and Methods
2.1. Setting and Sample
2.2. Data Sources
2.3. Outcome
2.4. Exposure
2.5. Covariates
2.6. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Ogden, C.L.; Carroll, M.D.; Lawman, H.G.; Fryar, C.D.; Kruszon-Moran, D.; Kit, B.K.; Flegal, K.M. Trends in Obesity Prevalence Among Children and Adolescents in the United States, 1988–1994 through 2013–2014. JAMA 2016, 315, 2292–2299. [Google Scholar] [CrossRef] [PubMed]
- Sanyaolu, A.; Okorie, C.; Qi, X.; Locke, J.; Rehman, S. Childhood and Adolescent Obesity in the United States: A Public Health Concern. Glob. Pediatr. Health 2019, 6, 2333794X19891305. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ogden, C.L.; Carroll, M.D.; Kit, B.K.; Flegal, K.M. Prevalence of childhood and adult obesity in the United States, 2011–2012. JAMA 2014, 311, 806–814. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Skinner, A.C.; Ravanbakht, S.N.; Skelton, J.A.; Perrin, E.M.; Armstrong, S.C. Prevalence of Obesity and Severe Obesity in US Children, 1999–2016. Pediatrics 2018, 141, e20173. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lange, S.J.; Kompaniyets, L.; Freedman, D.S.; Kraus, E.M.; Porter, R.; Blanck, H.M.; Goodman, A.B. Longitudinal Trends in Body Mass Index Before and During the COVID-19 Pandemic Among Persons Aged 2–19 Years—United States, 2018–2020. MMWR Morb. Mortal. Wkly. Rep. 2021, 70, 1278–1283. [Google Scholar] [CrossRef]
- Pan, L.; Freedman, D.S.; Sharma, A.J.; Castellanos-Brown, K.; Park, S.; Smith, R.B.; Blanck, H.M. Trends in Obesity Among Participants Aged 2–4 Years in the Special Supplemental Nutrition Program for Women, Infants, and Children—United States, 2000–2014. MMWR Morb. Mortal. Wkly. Rep. 2016, 65, 1256–1260. [Google Scholar] [CrossRef] [Green Version]
- Food and Nutrition Service, United States Department of Agriculture. WIC Eligibility and Coverage Rates; USDA: Washington, DC, USA, 2017. Available online: https://www.fns.usda.gov/wic/national-state-level-estimates-wic-eligibles-program-reach-2014-and-updated-estimates-2005-2013 (accessed on 2 January 2022).
- Grimes, C.A.; Szymlek-Gay, E.A.; Nicklas, T.A. Beverage Consumption among U.S. Children Aged 0–24 Months: National Health and Nutrition Examination Survey (NHANES). Nutrients 2017, 9, 264. [Google Scholar] [CrossRef]
- Drewnowski, A.; Rehm, C.D.; Constant, F. Water and beverage consumption among children age 4–13y in the United States: Analyses of 2005–2010 NHANES data. Nutr. J. 2013, 12, 85. [Google Scholar] [CrossRef] [Green Version]
- Gorelick, M.H.; Gould, L.; Nimmer, M.; Wagner, D.; Heath, M.; Bashir, H.; Brousseau, D.C. Perceptions about water and increased use of bottled water in minority children. Arch. Pediatr. Adolesc. Med. 2011, 165, 928–932. [Google Scholar] [CrossRef] [Green Version]
- Beck, A.L.; Martinez, S.; Patel, A.I.; Fernandez, A. Trends in sugar-sweetened beverage consumption among California children. Public Health Nutr. 2020, 23, 2864–2869. [Google Scholar] [CrossRef]
- Lioret, S.; Betoko, A.; Forhan, A.; Charles, M.A.; Heude, B.; de Lauzon-Guillain, B. Dietary patterns track from infancy to preschool age: Cross-sectional and longitudinal perspectives. J. Nutr. 2015, 145, 775–782. [Google Scholar] [PubMed]
- Au, L.E.; Paolicelli, C.; Gurzo, K.; Ritchie, L.D.; Weinfield, N.S.; Plank, K.R.; Whaley, S.E. Contribution of WIC-Eligible Foods to the Overall Diet of 13- and 24-Month-Old Toddlers in the WIC Infant and Toddler Feeding Practices Study-2. J. Acad. Nutr. Diet. 2019, 119, 435–448. [Google Scholar] [CrossRef]
- Borger, C.; Weinfield, N.; Zimmerman, T.; MacAllum, C.; DeMatteis, J.; Whaley, S.; Ritchie, L.; Sallack, L.; Au, L.; Jenkins, F.; et al. WIC Infant and Toddler Feeding Practices Study-2: Second Year Report; Food and Nutrition Service of the United States Department of Agriculture: Alexandria, VA, USA, 2018. Available online: https://fns-prod.azureedge.net/sites/default/files/ops/WIC-ITFPS2-Year2Report.pdf (accessed on 2 January 2022).
- Anderson, C.E.; O’Malley, K.; Martinez, C.E.; Ritchie, L.D.; Whaley, S.E. Longer family participation in WIC is associated with lower childhood sugar-sweetened beverage intake. J. Nutr. Educ. Behav. 2022. [Google Scholar] [CrossRef] [PubMed]
- Data Mining Project. Los Angeles County WIC Survey Instruments 2020. Available online: https://lawicdata.org/survey/ (accessed on 2 January 2022).
- Koleilat, M.; Whaley, S.E. Reliability and Validity of Food Frequency Questions to Assess Beverage and Food Group Intakes among Low-Income 2- to 4-Year-Old Children. J. Acad. Nutr. Diet. 2016, 116, 931–939. [Google Scholar] [CrossRef] [PubMed]
- U.S. Department of Agriculture; U.S. Department of Health and Human Services. Dietary Guidelines for Americans, 2020–2025, 9th ed.; U.S. Department of Agriculture: Alexandria, VA, USA, 2020. Available online: dietaryguidelines.gov (accessed on 2 January 2022).
- Patel, A.I.; Hecht, C.E.; Cradock, A.; Edwards, M.A.; Ritchie, L.D. Drinking Water in the United States: Implications of Water Safety, Access, and Consumption. Annu. Rev. Nutr. 2020, 40, 345–373. [Google Scholar] [CrossRef]
- Grummon, A.H.; Cabana, M.D.; Hecht, A.A.; Alkon, A.; McCulloch, C.E.; Brindis, C.D.; Patel, A.I. Effects of a multipronged beverage intervention on young children’s beverage intake and weight: A cluster-randomized pilot study. Public Health Nutr. 2019, 22, 2856–2867. [Google Scholar] [CrossRef] [Green Version]
- Demmer, E.; Cifelli, C.J.; Houchins, J.A.; Fulgoni, V.L., 3rd. Ethnic disparities of beverage consumption in infants and children 0–5 years of age; National Health and Nutrition Examination Survey 2011 to 2014. Nutr. J. 2018, 17, 78. [Google Scholar] [CrossRef] [Green Version]
- Mochari-Greenberger, H.; Terry, M.B.; Mosca, L. Sex, age, and race/ethnicity do not modify the effectiveness of a diet intervention among family members of hospitalized cardiovascular disease patients. J. Nutr. Educ. Behav. 2011, 43, 366–373. [Google Scholar] [CrossRef] [Green Version]
- Tussing-Humphreys, L.; Thomson, J.L.; Goodman, M.; Landry, A. Enhanced vs Standard Parents as Teacher Curriculum on Factors Related to Infant Feeding among African American Women. South. Med. J. 2019, 112, 512–519. [Google Scholar] [CrossRef]
- Broyles, S.T.; Myers, C.A.; Drazba, K.T.; Marker, A.M.; Church, T.S.; Newton, R.L., Jr. The Influence of Neighborhood Crime on Increases in Physical Activity during a Pilot Physical Activity Intervention in Children. J. Urban Health 2016, 93, 271–278. [Google Scholar] [CrossRef] [Green Version]
- Anderson, C.E.; Crespi, C.M.; Wang, M.C.; Whaley, S.E.; Chaparro, M.P. The neighborhood food environment modifies the effect of the 2009 WIC food package change on childhood obesity in Los Angeles County, California. BMC Public Health 2020, 20, 678. [Google Scholar] [CrossRef] [PubMed]
- California WIC Association, PHFE WIC Program. WIC Works: Better Foods and Clear Messages Improve Nutrition. September 2011. Available online: http://calwic.org/storage/WIC_WORKS_Better_Foods_and_Clear_Messages.pdf (accessed on 2 January 2022).
- Beckman, M.; Harris, J. Understanding individual and socio-cultural factors associated with hispanic parents’ provision of sugar-sweetened beverages to young children. Appetite 2021, 161, 105139. [Google Scholar] [CrossRef] [PubMed]
- Krieger, J.; Kwon, T.; Ruiz, R.; Walkinshaw, L.P.; Yan, J.; Roberto, C.A. Countermarketing About Fruit Drinks, alone or with Water Promotion: A 2019 Randomized Controlled Trial in Latinx Parents. Am. J. Public Health 2021, 111, 1997–2007. [Google Scholar] [CrossRef] [PubMed]


| Variable | Asian | Black | Hispanic, EN | Hispanic, SP | White | ||
|---|---|---|---|---|---|---|---|
| N = 634 | N = 1141 | N = 5281 | N = 3548 | N = 878 | p-Value | ||
| Child characteristics | |||||||
| Male | 337 (53.2) | 545 (47.8) | 2699 (51.1) | 1840 (51.9) | 447 (50.9) | 0.14 | |
| Age | <0.0001 | ||||||
| 4 to <12 m | 83 (13.1) | 171 (15.0) | 770 (14.6) | 391 (11.0) | 99 (11.3) | ||
| 12 to <24 m | 184 (29.0) | 297 (26.0) | 1393 (26.4) | 718 (20.2) | 197 (22.4) | ||
| 20 to <36 m | 142 (22.4) | 240 (21.0) | 1145 (21.7) | 769 (21.7) | 184 (21.0) | ||
| 36 to <48 m | 133 (21.0) | 239 (20.9) | 1073 (20.3) | 858 (24.2) | 203 (23.1) | ||
| 48 to <60 m | 92 (14.5) | 194 (17.0) | 900 (17.0) | 812 (22.9) | 195 (22.2) | ||
| Prenatal enrollment | 255 (40.2) | 401 (35.1) | 1568 (29.7) | 1073 (30.2) | 314 (35.8) | <0.0001 | |
| Current childcare use | 155 (24.6) | 556 (48.8) | 2349 (44.5) | 883 (24.9) | 257 (29.3) | <0.0001 | |
| Daily servings | |||||||
| Water | 4.1 ± 2.3 | 3.5 ± 2.0 | 3.9 ± 2.2 | 4.1 ± 2.1 | 4.1 ± 2.2 | <0.0001 | |
| Total SSB | 0.5 ± 0.9 | 1.0 ± 1.5 | 0.7 ± 1.2 | 1.0 ± 1.4 | 0.9 ± 1.3 | <0.0001 | |
| Fruit-flavored SSB | 0.2 ± 0.6 | 0.5 ± 0.9 | 0.3 ± 0.7 | 0.4 ± 0.7 | 0.4 ± 0.7 | <0.0001 | |
| Park/playground visits | <0.0001 | ||||||
| ≥3 days/week | 250 (39.5) | 638 (56.2) | 3340 (63.4) | 1823 (51.5) | 447 (50.9) | ||
| ≤2 days/week | 383 (60.5) | 497 (43.8) | 1931 (36.6) | 1719 (48.5) | 431 (49.1) | ||
| Survey year | <0.0001 | ||||||
| 2014 | 26 (4.1) | 377 (33.0) | 1769 (33.5) | 952 (26.8) | 520 (59.2) | ||
| 2017 | 78 (12.3) | 246 (21.6) | 1915 (36.3) | 1308 (36.9) | 111 (12.6) | ||
| 2020 | 530 (83.6) | 518 (45.4) | 1597 (30.2) | 1288 (36.3) | 247 (28.1) | ||
| Maternal characteristcs | |||||||
| Maternal education | <0.0001 | ||||||
| <HS | 23 (3.6) | 113 (9.9) | 769 (14.6) | 1994 (56.2) | 294 (33.5) | ||
| HS grad | 138 (21.8) | 359 (31.5) | 1673 (31.7) | 999 (28.2) | 246 (28.0) | ||
| >HS | 473 (74.6) | 669 (58.6) | 2839 (53.8) | 555 (15.6) | 338 (38.5) | ||
| Maternal BMI | 26.4 ± 6.0 | 30.3 ± 7.6 | 29.4 ± 6.7 | 28.7 ± 6.2 | 28.2 ± 6.4 | <0.0001 | |
| Household characteristics | |||||||
| Food security | <0.0001 | ||||||
| Low | 138 (21.8) | 268 (23.5) | 956 (18.1) | 821 (23.1) | 203 (23.1) | ||
| Very low | 22 (3.5) | 100 (8.8) | 310 (5.9) | 203 (5.7) | 76 (8.7) | ||
| Income, USD/m | <0.0001 | ||||||
| <1200 | 148 (23.3) | 602 (52.8) | 1939 (36.7) | 899 (25.3) | 309 (35.2) | ||
| 1200 to <1800 | 167 (26.3) | 245 (21.5) | 1390 (26.3) | 1415 (39.9) | 271 (30.9) | ||
| 1800 to <2400 | 174 (27.4) | 176 (15.4) | 1025 (19.4) | 738 (20.8) | 171 (19.5) | ||
| ≥2400 | 145 (22.9) | 118 (10.3) | 927 (17.6) | 496 (14.0) | 127 (14.5) | ||
| Older child present | 367 (57.9) | 719 (63.0) | 3470 (65.7) | 2790 (78.6) | 638 (72.7) | <0.0001 | |
| Multiple WIC children | 140 (22.1) | 278 (24.4) | 1291 (24.4) | 702 (19.8) | 189 (21.5) | <0.0001 | |
| SNAP | 250 (39.4) | 766 (67.1) | 2247 (42.5) | 1674 (47.2) | 462 (52.6) | <0.0001 | |
| Household size | 4.5 ± 1.5 | 4.0 ± 1.5 | 4.6 ± 1.6 | 4.8 ± 1.5 | 4.6 ± 1.5 | <0.0001 | |
| Duration on WIC, m | 3.5 ± 2.6 | 4.7 ± 3.7 | 4.6 ± 3.4 | 6.3 ± 3.9 | 5.6 ± 3.7 | <0.0001 | |
| 1 Year | 2 Years c | 5 Years d | 10 Years e | ||
|---|---|---|---|---|---|
| Total SSB a | |||||
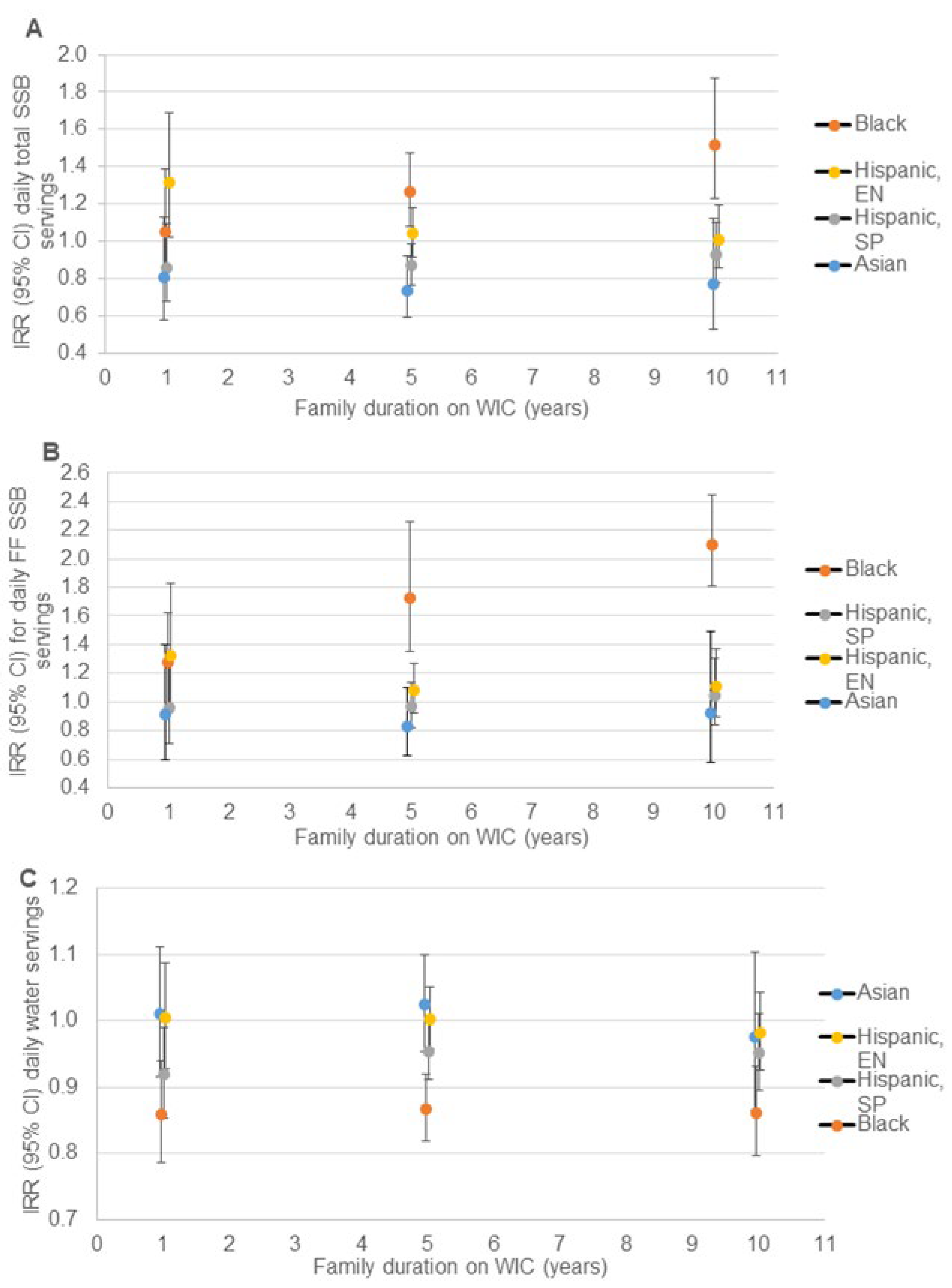
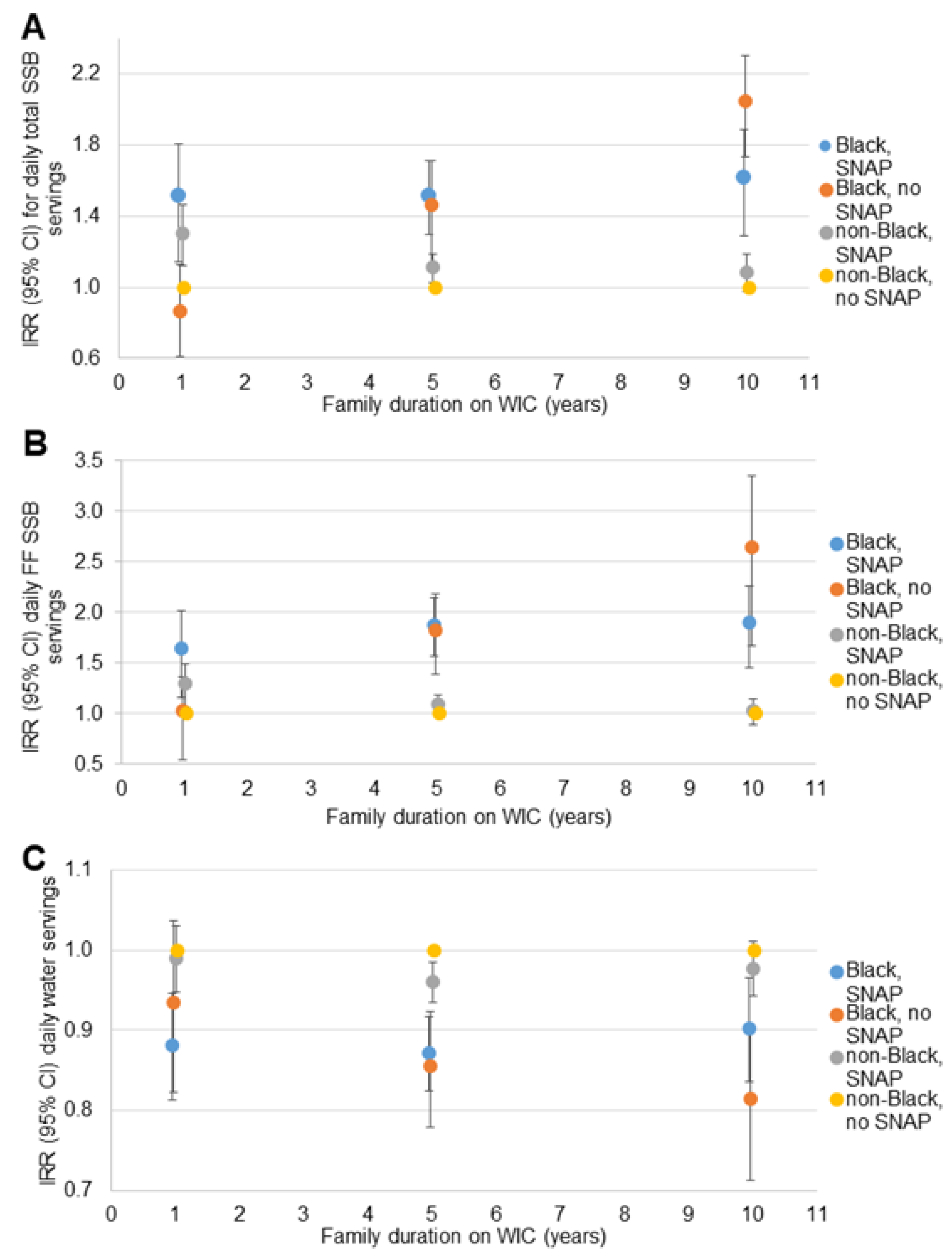
| Asian | 1.00 | 0.96 (0.85, 1.08) | 0.87 (0.62, 1.23) | 0.83 (0.52, 1.33) | |
| Black | 1.00 | 1.04 (0.97, 1.11) | 1.14 (0.93, 1.40) | 1.26 (0.96, 1.64) | |
| Hispanic, SP | 1.00 | 0.99 (0.95, 1.02) | 0.96 (0.86, 1.08) | 0.94 (0.81, 1.09) | |
| Hispanic, EN | 1.00 | 0.92 (0.88, 0.95) | 0.75 (0.67, 0.85) | 0.67 (0.57, 0.79) | |
| White | 1.00 | 0.99 (0.92, 1.07) | 0.95 (0.75, 1.21) | 0.87 (0.63, 1.20) | |
| Fruit-flavored SSB a | |||||
| Asian | 1.00 | 0.96 (0.83, 1.12) | 0.89 (0.57, 1.39) | 0.89 (0.49, 1.62) | |
| Black | 1.00 | 1.09 (1.02, 1.18) | 1.33 (1.06, 1.68) | 1.45 (1.07, 1.96) | |
| Hispanic, SP | 1.00 | 1.00 (0.95, 1.04) | 0.99 (0.86, 1.14) | 0.96 (0.80, 1.15) | |
| Hispanic, EN | 1.00 | 0.94 (0.89, 0.98) | 0.80 (0.69, 0.94) | 0.73 (0.60, 0.90) | |
| White | 1.00 | 1.00 (0.91, 1.11) | 0.98 (0.72, 1.34) | 0.88 (0.59, 1.32) | |
| Water b | |||||
| Asian | 1.00 | 0.99 (0.96, 1.02) | 0.97 (0.88, 1.06) | 0.93 (0.81, 1.06) | |
| Black | 1.00 | 0.99 (0.96, 1.01) | 0.96 (0.90, 1.04) | 0.96 (0.88, 1.06) | |
| Hispanic, SP | 1.00 | 1.00 (0.98, 1.01) | 0.99 (0.95, 1.02) | 0.99 (0.95, 1.04) | |
| Hispanic, EN | 1.00 | 0.98 (0.97, 1.00) | 0.95 (0.91, 0.99) | 0.94 (0.89, 0.99) | |
| White | 1.00 | 0.98 (0.96, 1.01) | 0.95 (0.88, 1.03) | 0.96 (0.86, 1.06) | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Anderson, C.E.; Martinez, C.E.; O’Malley, K.; Ritchie, L.D.; Whaley, S.E. Longer Participation in the Special Supplemental Nutrition Program for Women, Infants, and Children Is Not Associated with Reduced Sugar-Sweetened Beverage Intake among Black Participants. Nutrients 2022, 14, 1048. https://doi.org/10.3390/nu14051048
Anderson CE, Martinez CE, O’Malley K, Ritchie LD, Whaley SE. Longer Participation in the Special Supplemental Nutrition Program for Women, Infants, and Children Is Not Associated with Reduced Sugar-Sweetened Beverage Intake among Black Participants. Nutrients. 2022; 14(5):1048. https://doi.org/10.3390/nu14051048
Chicago/Turabian StyleAnderson, Christopher E., Catherine E. Martinez, Keelia O’Malley, Lorrene D. Ritchie, and Shannon E. Whaley. 2022. "Longer Participation in the Special Supplemental Nutrition Program for Women, Infants, and Children Is Not Associated with Reduced Sugar-Sweetened Beverage Intake among Black Participants" Nutrients 14, no. 5: 1048. https://doi.org/10.3390/nu14051048
APA StyleAnderson, C. E., Martinez, C. E., O’Malley, K., Ritchie, L. D., & Whaley, S. E. (2022). Longer Participation in the Special Supplemental Nutrition Program for Women, Infants, and Children Is Not Associated with Reduced Sugar-Sweetened Beverage Intake among Black Participants. Nutrients, 14(5), 1048. https://doi.org/10.3390/nu14051048







