Iodine Status of 6–12-Year-Old Children in Russia over the Past 10 Years: A Scoping Review
Abstract
1. Introduction
2. Materials and Methods
2.1. Search Strategy
2.2. Record Screening
2.3. Selection
- (i)
- the study contained data on UIC in children;
- (ii)
- the age of children was between 6 and 12 years;
- (iii)
- the children lived on the territory of the Russian Federation.
2.4. Data Extraction
3. Results
3.1. Publication Selection
3.2. Description of Included Studies
- <20 μg/L—severe ID;
- 20–49 μg/L—moderate ID;
- 50–99 μg/L—mild ID;
- 100–300 μg/L—normal iodine intake;
- 200–299 μg/L—more than adequate;
- >300 μg/L—excess iodine intake.
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Monaghan, A.M.; Mulhern, M.S.; McSorley, E.M.; Strain, J.J.; Dyer, M.; van Wijngaarden, E.; Yeates, A.J. Associations between maternal urinary iodine assessment, dietary iodine intakes and neurodevelopmental outcomes in the child: A systematic review. Thyr. Res. 2021, 14, 14. [Google Scholar] [CrossRef] [PubMed]
- Ghassabian, A.; Trasande, L. Disruption in Thyroid Signaling Pathway: A Mechanism for the Effect of Endocrine-Disrupting Chemicals on Child Neurodevelopment. Front. Endocrinol. 2018, 9, 204. [Google Scholar] [CrossRef]
- World Health Organization. Assessment of Iodine Deficiency Disorders and Monitoring Their Elimination: A Guide for Programme Man-Agers. Third edition. 2007. Available online: http://apps.who.int/iris/bitstream/handle/10665/43781/9789241595827_eng.pdf?sequence=1 (accessed on 5 December 2021).
- Hynes, K.L.; Otahal, P.; Hay, I.; Burgess, J. Mild Iodine Deficiency During Pregnancy Is Associated With Reduced Educational Outcomes in the Offspring: 9-Year Follow-up of the Gestational Iodine Cohort. J. Clin. Endocrinol. Metab. 2013, 98, 1954–1962. [Google Scholar] [CrossRef]
- Bath, S.C.; Steer, C.D.; Golding, J.; Emmett, P.; Rayman, M.P. Effect of inadequate iodine status in UK pregnant women on cognitive outcomes in their children: Results from the Avon Longitudinal Study of Parents and Children (ALSPAC). Lancet 2013, 382, 331–337. [Google Scholar] [CrossRef]
- Iodine Global Network. Available online: https://www.ign.org/cm_data/IGN_Global_Scorecard_2021_7_May_2021.pdf (accessed on 5 December 2021).
- Gerasimov, G.A. New adventures of the median urinary iodine. Clin. Exp. Thyroidol. 2018, 14, 58–63. [Google Scholar] [CrossRef]
- Abusuev, S.A.; Alimetova, K.A.; Ataev, M.G. The effectiveness of the iodine deficiency prevention in the coastal and non-coastal towns in the Republic of Dagestan. Proc. DGPU. 2014, 29, 39–44. [Google Scholar]
- Tricco, A.C.; Lillie, E.; Zarin, W.; O’Brien, K.K.; Colquhoun, H.; Levac, D.; Moher, D.; Peters, M.D.J.; Horsley, T.; Weeks, L.; et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and Explanation. Ann. Intern. Med. 2018, 169, 467–473. [Google Scholar] [CrossRef]
- Bikmetova, E.; Golovatskikh, I.; Ivanova, G. Elementary provision of children in the south Ural region of the Republic of Bashkortostan. Mod. Med. New Approaches Relev. Stud. 2018, 11, 30–33. [Google Scholar]
- Danilenko, A.L.; Kamilov, F.K.; Mamtsev, A.N.; Kozlov, V.N.; Ponomarev, E.E. Effectiveness of the program “School Milk” for the prevention of iodine deficiency. Nutr. Issues 2015, 84, 53–58. [Google Scholar]
- Golovatskikh, I.V.; Kuznetsova, E.V.; Bikmetova, E.R.; Kozlov, V.N.; Kamilov, F.K.; Mamtsev, A.N. Efficiency of use iodized milk for group prevention iodine deficiency in prepubertal children. Omsk Sci. Bull. 2013, 118, 96–99. [Google Scholar]
- Kiyaev, A.V.; Platonova, N.M.; Abdulhabirova, F.M.; Troshina, E.A.; Gerasimov, G.A. Influence of excessive iodine intake on the thyroid function and spectrum of thyroid abnormalities in population of Turinsk, Sverdlovsk Region, of Russia. Clin. Exp. Thyroidol. 2015, 11, 43–49. [Google Scholar] [CrossRef][Green Version]
- Zahohov, R.; Uzdenova, Z.; Shogenova, F.; Shavaeva, V.; Berhamova, E.; Shavaeva, F.; Bichekueva, S. The differentiated prevention of iodic deficiency in the girls in the Kabardino-Balkarya. Bull. New Med. Technol. 2013, 20, 413–417. [Google Scholar]
- Skorodok, Y.L.; Mullachmetova, Z.I.; Bondarenko, V.L.; Novoselova, N.V.; Vochmjanina, N.V.; Zhalenina, L.A. Iodine deficiency in a megalopolis bordering the gulf of Finland: Myth or reality? Clin. Exp. Thyroidol. 2013, 9, 36–40. [Google Scholar] [CrossRef][Green Version]
- Troshina, E.; Mazurina, N.; Senyushkina, E.; Makolina, N.; Galieva, M.; Nikankina, L.; Malysheva, N.; Darzhaa, A.; Sengi, Y. Monitoring of iodine deficiency disorders in the Republic of Tyva. Probl. Endocrinol. 2021, 67, 60–68. [Google Scholar] [CrossRef] [PubMed]
- Troshina, E.A.; Makolina, N.P.; Senyushkina, E.S.; Nikankina, L.V.; Malysheva, N.M.; Fetisova, A.V. Iodine Deficiency Disorders: Current State of the Problem in the Bryansk Region. Probl. Endocrinol. 2021, 67, 84–93. [Google Scholar] [CrossRef]
- Troshina, E.A.; Abdulhabirova, F.M.; Makolina, N.P.; Senyushkina, E.S.; Nikankina, L.V.; Malysheva, N.M.; Repinskaya, I.N.; Divinskaya, V.A. Iodine Deficiency Disorders: Current State of the Problem in the Republic of Crimea. Clin. Exp. Thyroidol. 2020, 16, 19–27. [Google Scholar] [CrossRef]
- Tapeshkina, N.V.; Perevalov, A.Y. Assessment of the efficiency of prevention of iodine deficiency among the children’s population of the city of Mezhdurechensk of the Kemerovo region. Hyg. Sanit. 2016, 95, 471–476. [Google Scholar] [CrossRef]
- Krasnov, M.; Krasnov, B.; Budylina, M. The issue of iodine deficiency in Chuvash republic. Acta Medica Eurasica. 2015, 3, 23–35. [Google Scholar]
- Zhukov, A.O. Research findings as per IQ level across regions with different iodine shortage rates. Russ. Psychiatr. J. 2007, 2, 16–21. [Google Scholar]
- United Nations Children’s Fund (UNICEF); Iodine Global Network. Guidance on the monitoring of salt iodization programmes and determination of population iodine status: Russian language version. Clin. Exp. Thyroidol. 2018, 14, 100–112. [Google Scholar] [CrossRef]
- Abuye, C.; Berhane, Y.; Ersumo, T. The role of changing diet and altitude on goitre prevalence in five regional states in Ethiopia. East Afr. J. Public Heal. 2008, 5, 163–168. [Google Scholar] [CrossRef]
- Omar, M.S.; Desouky, D.E.-S. Environmental, urinary iodine status and prevalence of goitre among schoolchildren in a high altitude area of Saudi Arabia. Pak. J. Med Sci. 2015, 31, 414–419. [Google Scholar] [CrossRef]
- Antonova, M.S. Iodine deficiency in the territory of the Jewish Autonomous region and perception of this problem by stu-dent’s far Eastern state social and humanitarian academy. DVGSGA Bull. 2009, 3, 5–13. [Google Scholar]
- Melnichenko, G.A.; Troshina, E.A.; Platonova, N.; Panfilova, E.A.; Rybakova, A.A.; Abdulkhabirova, F.M.; Bostanova, F.A. Iodine deficiency thyroid disease in the Russian Federation: The current state of the problem. Analytical review of publications and data of official state statistics (Rosstat). Cons. Medicum 2019, 21, 14–20. [Google Scholar] [CrossRef]
- National Medical Research Center for Endocrinology. Available online: https://www.endocrincentr.ru/ (accessed on 19 November 2021).
- Draft Federal Law “On the Prevention of Iodine Deficiency Disorders” of 27 March 2019. Available online: https://www.endocrincentr.ru/sites/default/files/all/prikaz_doc/01.04.19/iod_rek.pdf (accessed on 13 April 2021).
- Jooste, P.L.; Strydom, E. Methods for determination of iodine in urine and salt. Best Pr. Res. Clin. Endocrinol. Metab. 2010, 24, 77–88. [Google Scholar] [CrossRef] [PubMed]
- Sobolev, N.; Ellingsen, D.G.; Belova, N.; Aksenov, A.; Sorokina, T.; Trofimova, A.; Varakina, Y.; Kotsur, D.; Grjibovski, A.M.; Chashchin, V.; et al. Essential and non-essential elements in biological samples of inhabitants residing in Nenets Autonomous Okrug of the Russian Arctic. Environ. Int. 2021, 152, 106510. [Google Scholar] [CrossRef]
- World Health Organization (WHO). 2019. Available online: https://www.who.int/ (accessed on 15 April 2021).

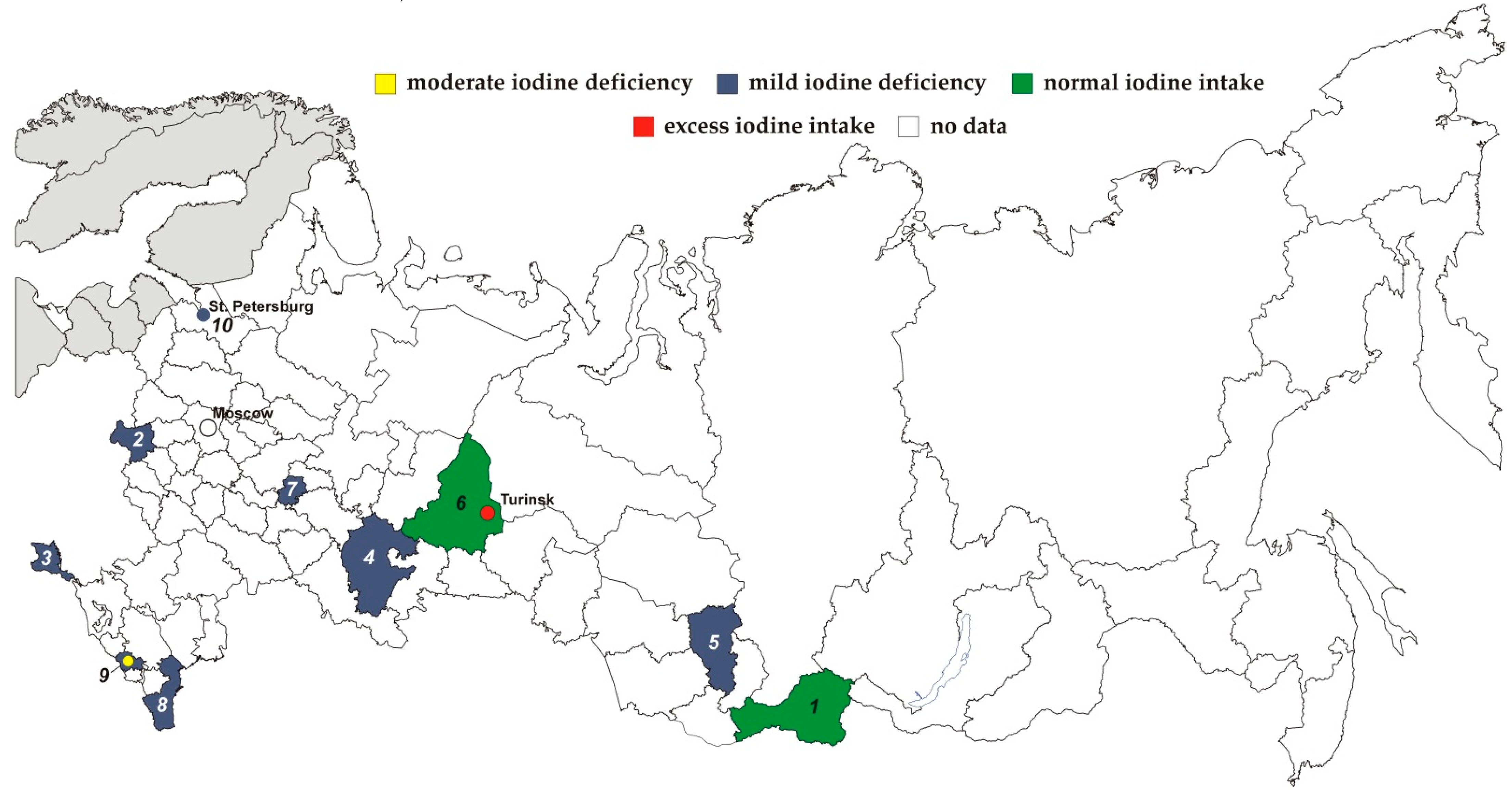
| Area of Residence (Number on the Map) | Year | n | Age, years | Indicator | UIC Assessment Methods | Reference | ||
|---|---|---|---|---|---|---|---|---|
| mUIC (μg/L) | Interquartile Range (Q1;Q3) | Note | ||||||
| Republic of Tyva (1) | 2021 | 227 | 8–10 | 153 | cerium-arsenite reaction | [16] | ||
| Bryansk region (2) | 2021 | 337 | 8–10 | 98 | cerium-arsenite reaction | [17] | ||
| Republic of Crimea (3) | 2020 | 356 | 8–10 | 97 | cerium-arsenite reaction | [18] | ||
| Republic of Bashkortostan (4) | 2018 | 180 | 8–9 | 89 52 | (45;144) (26;79) | town village | photometry (set of reagents «Merck», Germany) | [10] |
| Kemerovo region (5) | 2016 | 7–10 | 98 | potentiometry using ion-selective electrodes | [19] | |||
| Republic of Bashkortostan (4) | 2015 | 181 | 8–10 | 88 159 61 121 | (23;156) (60;191) (22;71) (98;162) | town after IS a village after IS | cerium-arsenite reaction | [11] |
| Sverdlovsk region (6) | 2015 | 97 100 | 8–12 8–11 | 121 b 719 | overall Turinsk | cerium-arsenite reaction | [13] | |
| Republic of Chuvash (7) | 2015 | 7–12 | 72 | cerium-arsenite reaction | [20] | |||
| Republic of Dagestan (8) | 2014 | 8–10 | 66–75 65–69 | coastal towns non-coastal towns | cerium-arsenite reaction | [8] | ||
| Republic of Bashkortostan (4) | 2013 | 181 | 8–10 | 89 159 52 121 | town: before IS after IS village: before IS after IS | colorimetry (set of reagents «Merck», Germany) | [12] | |
| Republic of Kabardino-Balkaria (9) | 2013 | 1782 | 7–11 | 79 c 71 d 46 e | (29;119) (39;132) (12;108) | cerium-arsenite by Saundell-Kolthoff reaction | [14] | |
| St. Petersburg (10) | 2013 | 883 | 6–10 | 68 65 61 | overall boys girls | cerium-arsenite reaction | [15] | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Korobitsyna, R.; Aksenov, A.; Sorokina, T.; Trofimova, A.; Grjibovski, A.M. Iodine Status of 6–12-Year-Old Children in Russia over the Past 10 Years: A Scoping Review. Nutrients 2022, 14, 897. https://doi.org/10.3390/nu14040897
Korobitsyna R, Aksenov A, Sorokina T, Trofimova A, Grjibovski AM. Iodine Status of 6–12-Year-Old Children in Russia over the Past 10 Years: A Scoping Review. Nutrients. 2022; 14(4):897. https://doi.org/10.3390/nu14040897
Chicago/Turabian StyleKorobitsyna, Rimma, Andrey Aksenov, Tatiana Sorokina, Anna Trofimova, and Andrej M. Grjibovski. 2022. "Iodine Status of 6–12-Year-Old Children in Russia over the Past 10 Years: A Scoping Review" Nutrients 14, no. 4: 897. https://doi.org/10.3390/nu14040897
APA StyleKorobitsyna, R., Aksenov, A., Sorokina, T., Trofimova, A., & Grjibovski, A. M. (2022). Iodine Status of 6–12-Year-Old Children in Russia over the Past 10 Years: A Scoping Review. Nutrients, 14(4), 897. https://doi.org/10.3390/nu14040897






