Diet Quality Scores and Cardiometabolic Risk Factors in Mexican Children and Adolescents: A Longitudinal Analysis
Abstract
1. Introduction
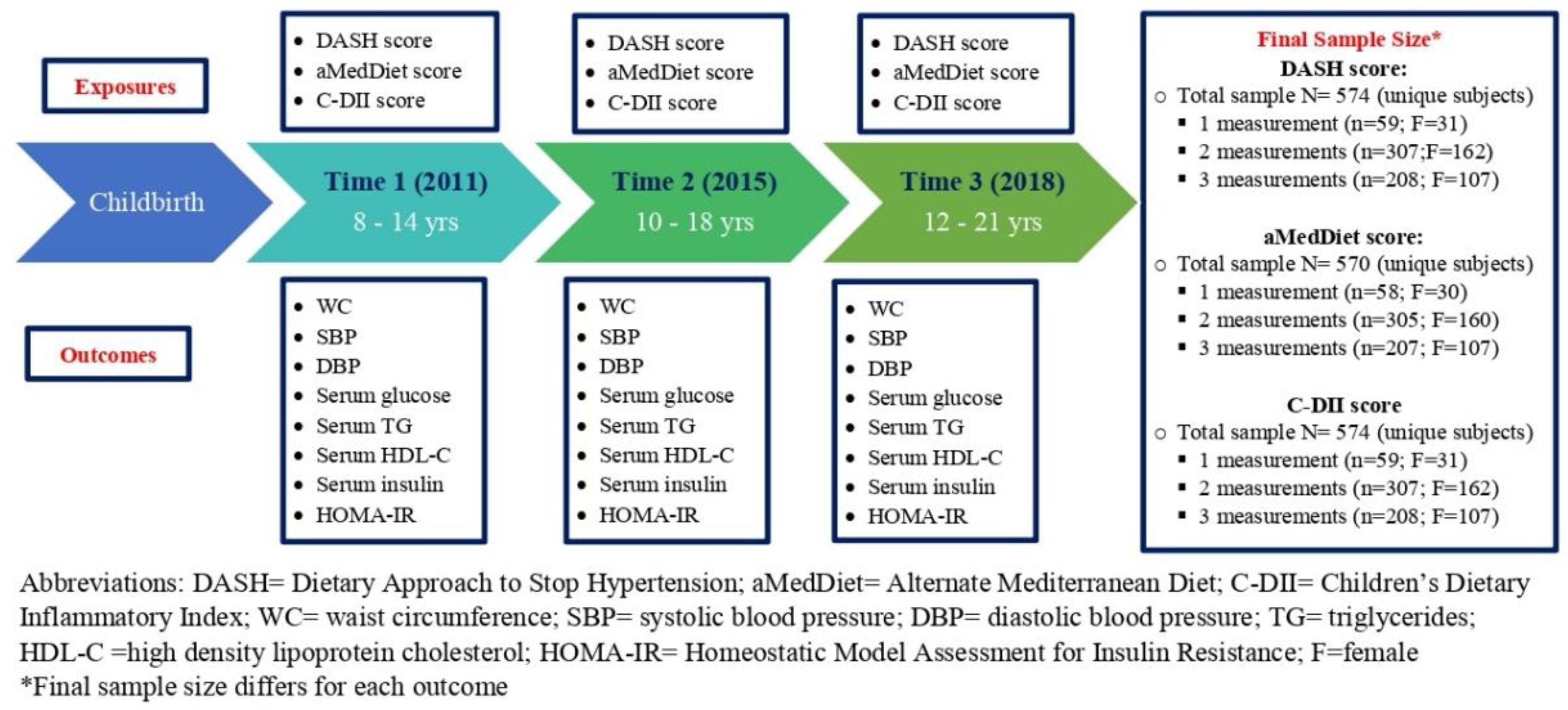
2. Materials and Methods
2.1. Study Population
2.2. Cardiometabolic Risk Factors
2.2.1. Anthropometric Measures
2.2.2. Cardiometabolic Biomarkers
2.3. Diet Quality Scores
2.4. Covariates
2.5. Statistical Analysis
3. Results
3.1. Association between DASH Diet Scores and Cardiometabolic Risk Factors
3.2. Association between aMedDiet Scores and Cardiometabolic Risk Factors
3.3. Association between C-DII Scores and Cardiometabolic Risk Factors
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Di Cesare, M.; Soric, M.; Bovet, P.; Miranda, J.J.; Bhutta, Z.; Stevens, G.A.; Laxmaiah, A.; Kengne, A.P.; Bentham, J. The epidemiological burden of obesity in childhood: A worldwide epidemic requiring urgent action. BMC Med. 2019, 17, 212. [Google Scholar] [CrossRef]
- Tavares Giannini, D.; Caetano Kuschnir, M.C.; Szklo, M. Metabolic syndrome in overweight and obese adolescents: A comparison of two different diagnostic criteria. Ann. Nutr. Metab. 2014, 64, 71–79. [Google Scholar] [CrossRef]
- Reinehr, T.; de Sousa, G.; Toschke, A.M.; Andler, W. Comparison of metabolic syndrome prevalence using eight different definitions: A critical approach. Arch. Dis. Child. 2007, 92, 1067–1072. [Google Scholar] [CrossRef] [PubMed]
- Flouris, A.D.; Bouziotas, C.; Christodoulos, A.D.; Koutedakis, Y. Longitudinal preventive-screening cutoffs for metabolic syndrome in adolescents. Int. J. Obes. 2008, 32, 1506–1512. [Google Scholar] [CrossRef]
- Sommer, A.; Twig, G. The Impact of Childhood and Adolescent Obesity on Cardiovascular Risk in Adulthood: A Systematic Review. Curr. Diab. Rep. 2018, 18, 91. [Google Scholar] [CrossRef] [PubMed]
- Galassi, A.; Reynolds, K.; He, J. Metabolic syndrome and risk of cardiovascular disease: A meta-analysis. Am. J. Med. 2006, 119, 812–819. [Google Scholar] [CrossRef] [PubMed]
- Gami, A.S.; Witt, B.J.; Howard, D.E.; Erwin, P.J.; Gami, L.A.; Somers, V.K.; Montori, V.M. Metabolic syndrome and risk of incident cardiovascular events and death: A systematic review and meta-analysis of longitudinal studies. J. Am. Coll. Cardiol. 2007, 49, 403–414. [Google Scholar] [CrossRef]
- Ford, E.S. Risks for all-cause mortality, cardiovascular disease, and diabetes associated with the metabolic syndrome: A summary of the evidence. Diabetes Care 2005, 28, 1769–1778. [Google Scholar] [CrossRef]
- Stocks, T.; Bjorge, T.; Ulmer, H.; Manjer, J.; Haggstrom, C.; Nagel, G.; Engeland, A.; Johansen, D.; Hallmans, G.; Selmer, R.; et al. Metabolic risk score and cancer risk: Pooled analysis of seven cohorts. Int. J. Epidemiol. 2015, 44, 1353–1363. [Google Scholar] [CrossRef]
- Eloranta, A.M.; Schwab, U.; Venalainen, T.; Kiiskinen, S.; Lakka, H.M.; Laaksonen, D.E.; Lakka, T.A.; Lindi, V. Dietary quality indices in relation to cardiometabolic risk among Finnish children aged 6–8 years—The PANIC study. Nutr. Metab. Cardiovasc. Dis. 2016, 26, 833–841. [Google Scholar] [CrossRef]
- Hoyas, I.; Leon-Sanz, M. Nutritional Challenges in Metabolic Syndrome. J. Clin. Med. 2019, 8, 1301. [Google Scholar] [CrossRef] [PubMed]
- Hu, F.B. Dietary pattern analysis: A new direction in nutritional epidemiology. Curr. Opin. Lipidol. 2002, 13, 3–9. [Google Scholar] [CrossRef]
- Gil, A.; Martinez de Victoria, E.; Olza, J. Indicators for the evaluation of diet quality. Nutr. Hosp. 2015, 31 (Suppl. 3), 128–144. [Google Scholar] [CrossRef]
- Moore, L.L.; Singer, M.R.; Bradlee, M.L.; Daniels, S.R. Adolescent dietary intakes predict cardiometabolic risk clustering. Eur. J. Nutr. 2016, 55, 461–468. [Google Scholar] [CrossRef] [PubMed]
- Fornari, E.; Maffeis, C. Treatment of Metabolic Syndrome in Children. Front. Endocrinol. 2019, 10, 702. [Google Scholar] [CrossRef]
- Pallazola, V.A.; Davis, D.M.; Whelton, S.P.; Cardoso, R.; Latina, J.M.; Michos, E.D.; Sarkar, S.; Blumenthal, R.S.; Arnett, D.K.; Stone, N.J.; et al. A Clinician’s Guide to Healthy Eating for Cardiovascular Disease Prevention. Mayo. Clin. Proc. Innov. Qual. Outcomes 2019, 3, 251–267. [Google Scholar] [CrossRef]
- Health, N.I.O. Your Guide to Lowering Your Blood Pressure with DASH; Smashbooks: Los Gatos, CA, USA, 2006. [Google Scholar]
- Iaccarino Idelson, P.; Scalfi, L.; Valerio, G. Adherence to the Mediterranean Diet in children and adolescents: A systematic review. Nutr. Metab. Cardiovasc. Dis. 2017, 27, 283–299. [Google Scholar] [CrossRef]
- Franquesa, M.; Pujol-Busquets, G.; Garcia-Fernandez, E.; Rico, L.; Shamirian-Pulido, L.; Aguilar-Martinez, A.; Medina, F.X.; Serra-Majem, L.; Bach-Faig, A. Mediterranean Diet and Cardiodiabesity: A Systematic Review through Evidence-Based Answers to Key Clinical Questions. Nutrients 2019, 11, 655. [Google Scholar] [CrossRef]
- Martinez-Gonzalez, M.A.; Gea, A.; Ruiz-Canela, M. The Mediterranean Diet and Cardiovascular Health. Circ. Res. 2019, 124, 779–798. [Google Scholar] [CrossRef]
- Shivappa, N.; Hebert, J.R.; Marcos, A.; Diaz, L.E.; Gomez, S.; Nova, E.; Michels, N.; Arouca, A.; González-Gil, E.; Frederic, G. Association between dietary inflammatory index and inflammatory markers in the HELENA study. Mol. Nutr. Food Res. 2017, 61, 1600707. [Google Scholar] [CrossRef]
- Almeida-de-Souza, J.; Santos, R.; Barros, R.; Abreu, S.; Moreira, C.; Lopes, L.; Mota, J.; Moreira, P. Dietary inflammatory index and inflammatory biomarkers in adolescents from LabMed physical activity study. Eur. J. Clin. Nutr. 2018, 72, 710–719. [Google Scholar] [CrossRef] [PubMed]
- Cavicchia, P.P.; Steck, S.E.; Hurley, T.G.; Hussey, J.R.; Ma, Y.; Ockene, I.S.; Hébert, J.R. A new dietary inflammatory index predicts interval changes in serum high-sensitivity C-reactive protein. J. Nutr. 2009, 139, 2365–2372. [Google Scholar] [CrossRef] [PubMed]
- Kotemori, A.; Sawada, N.; Iwasaki, M.; Yamaji, T.; Shivappa, N.; Hebert, J.R.; Ishihara, J.; Inoue, M.; Tsugane, S. Validating the dietary inflammatory index using inflammatory biomarkers in a Japanese population: A cross-sectional study of the JPHC-FFQ validation study. Nutrition 2020, 69, 110569. [Google Scholar] [CrossRef] [PubMed]
- Vahid, F.; Shivappa, N.; Faghfoori, Z.; Khodabakhshi, A.; Zayeri, F.; Hebert, J.R.; Davoodi, S.H. Validation of a Dietary Inflammatory Index (DII) and Association with Risk of Gastric Cancer: A Case-Control Study. Asian Pac. J. Cancer Prev. 2018, 19, 1471–1477. [Google Scholar] [CrossRef] [PubMed]
- Shivappa, N.; Steck, S.E.; Hurley, T.G.; Hussey, J.R.; Ma, Y.; Ockene, I.S.; Tabung, F.; Hébert, J.R. A population-based dietary inflammatory index predicts levels of C-reactive protein in the Seasonal Variation of Blood Cholesterol Study (SEASONS). Public Health Nutr. 2014, 17, 1825–1833. [Google Scholar] [CrossRef] [PubMed]
- Shivappa, N.; Hébert, J.R.; Rietzschel, E.R.; De Buyzere, M.L.; Langlois, M.; Debruyne, E.; Marcos, A.; Huybrechts, I. Associations between dietary inflammatory index and inflammatory markers in the Asklepios Study. Br. J. Nutr. 2015, 113, 665–671. [Google Scholar] [CrossRef]
- Tilg, H.; Moschen, A.R. Inflammatory mechanisms in the regulation of insulin resistance. Mol. Med. 2008, 14, 222–231. [Google Scholar] [CrossRef]
- Galassetti, P. Inflammation and oxidative stress in obesity, metabolic syndrome, and diabetes. Exp. Diabetes Res. 2012, 2012, 943706. [Google Scholar] [CrossRef]
- DeBoer, M.D. Obesity, systemic inflammation, and increased risk for cardiovascular disease and diabetes among adolescents: A need for screening tools to target interventions. Nutrition 2013, 29, 379–386. [Google Scholar] [CrossRef]
- Donath, M.Y.; Meier, D.T.; Boni-Schnetzler, M. Inflammation in the Pathophysiology and Therapy of Cardiometabolic Disease. Endocr. Rev. 2019, 40, 1080–1091. [Google Scholar] [CrossRef]
- Sukhato, K.; Akksilp, K.; Dellow, A.; Vathesatogkit, P.; Anothaisintawee, T. Efficacy of different dietary patterns on lowering of blood pressure level: An umbrella review. Am. J. Clin. Nutr. 2020, 112, 1584–1598. [Google Scholar] [CrossRef] [PubMed]
- Aljuraiban, G.S.; Gibson, R.; Oude Griep, L.M.; Okuda, N.; Steffen, L.M.; Van Horn, L.; Chan, Q. Perspective: The Application of A Priori Diet Quality Scores to Cardiovascular Disease Risk-A Critical Evaluation of Current Scoring Systems. Adv. Nutr. 2020, 11, 10–24. [Google Scholar] [CrossRef]
- Giannini, C.; Diesse, L.; D’Adamo, E.; Chiavaroli, V.; de Giorgis, T.; Di Iorio, C.; Chiarelli, F.; Mohn, A. Influence of the Mediterranean diet on carotid intima-media thickness in hypercholesterolaemic children: A 12-month intervention study. Nutr. Metab. Cardiovasc. Dis. 2014, 24, 75–82. [Google Scholar] [CrossRef]
- Cohen, J.F.W.; Lehnerd, M.E.; Houser, R.F.; Rimm, E.B. Dietary Approaches to Stop Hypertension Diet, Weight Status, and Blood Pressure among Children and Adolescents: National Health and Nutrition Examination Surveys 2003–2012. J. Acad. Nutr. Diet. 2017, 117, 1437–1444. [Google Scholar] [CrossRef] [PubMed]
- Farhadnejad, H.; Asghari, G.; Mirmiran, P.; Azizi, F. Dietary approach to stop hypertension diet and cardiovascular risk factors among 10- to 18-year-old individuals. Pediatr. Obes. 2018, 13, 185–194. [Google Scholar] [CrossRef] [PubMed]
- Asghari, G.; Yuzbashian, E.; Mirmiran, P.; Hooshmand, F.; Najafi, R.; Azizi, F. Dietary Approaches to Stop Hypertension (DASH) Dietary Pattern Is Associated with Reduced Incidence of Metabolic Syndrome in Children and Adolescents. J. Pediatr. 2016, 174, 178–184.e171. [Google Scholar] [CrossRef] [PubMed]
- Betanzos-Robledo, L.; Rodriguez-Carmona, Y.; Contreras-Manzano, A.; Lamadrid-Figueroa, H.; Jansen, E.; Tellez-Rojo, M.M.; Perng, W.; Peterson, K.; Hebert, J.R.; Shivappa, N.; et al. Greater cumulative exposure to a pro-inflammatory diet is associated with higher metabolic syndrome score and blood pressure in young Mexican adults. Nutr. Res. 2020, 81, 81–89. [Google Scholar] [CrossRef]
- Sethna, C.B.; Alanko, D.; Wirth, M.D.; Shivappa, N.; Hebert, J.R.; Khan, S.; Sen, S. Dietary inflammation and cardiometabolic health in adolescents. Pediatr. Obes. 2021, 16, e12706. [Google Scholar] [CrossRef]
- Paula Bricarello, L.; Poltronieri, F.; Fernandes, R.; Retondario, A.; de Moraes Trindade, E.B.S.; de Vasconcelos, F.A.G. Effects of the Dietary Approach to Stop Hypertension (DASH) diet on blood pressure, overweight and obesity in adolescents: A systematic review. Clin. Nutr. ESPEN 2018, 28, 1–11. [Google Scholar] [CrossRef]
- Casazza, K.; Dulin-Keita, A.; Gower, B.A.; Fernandez, J.R. Differential influence of diet and physical activity on components of metabolic syndrome in a multiethnic sample of children. J. Am. Diet. Assoc. 2009, 109, 236–244. [Google Scholar] [CrossRef][Green Version]
- Lewis, R.C.; Meeker, J.D.; Peterson, K.E.; Lee, J.M.; Pace, G.G.; Cantoral, A.; Tellez-Rojo, M.M. Predictors of urinary bisphenol A and phthalate metabolite concentrations in Mexican children. Chemosphere 2013, 93, 2390–2398. [Google Scholar] [CrossRef]
- Ettinger, A.S.; Lamadrid-Figueroa, H.; Mercado-Garcia, A.; Kordas, K.; Wood, R.J.; Peterson, K.E.; Hu, H.; Hernandez-Avila, M.; Tellez-Rojo, M.M. Effect of calcium supplementation on bone resorption in pregnancy and the early postpartum: A randomized controlled trial in Mexican women. Nutr. J. 2014, 13, 116. [Google Scholar] [CrossRef] [PubMed]
- Perng, W.; Tamayo-Ortiz, M.; Tang, L.; Sanchez, B.N.; Cantoral, A.; Meeker, J.D.; Dolinoy, D.C.; Roberts, E.F.; Martinez-Mier, E.A.; Lamadrid-Figueroa, H.; et al. Early Life Exposure in Mexico to ENvironmental Toxicants (ELEMENT) Project. BMJ Open 2019, 9, e030427. [Google Scholar] [CrossRef] [PubMed]
- Wu, Y.; Goodrich, J.M.; Dolinoy, D.C.; Sanchez, B.N.; Ruiz-Narvaez, E.A.; Banker, M.; Cantoral, A.; Mercado-Garcia, A.; Tellez-Rojo, M.M.; Peterson, K.E. Accelerometer-measured Physical Activity, Reproductive Hormones, and DNA Methylation. Med. Sci. Sports Exerc. 2020, 52, 598–607. [Google Scholar] [CrossRef] [PubMed]
- Perng, W.; Fernandez, C.; Peterson, K.E.; Zhang, Z.; Cantoral, A.; Sanchez, B.N.; Solano-Gonzalez, M.; Tellez-Rojo, M.M.; Baylin, A. Dietary Patterns Exhibit Sex-Specific Associations with Adiposity and Metabolic Risk in a Cross-Sectional Study in Urban Mexican Adolescents. J. Nutr. 2017, 147, 1977–1985. [Google Scholar] [CrossRef]
- Bonora, E.; Formentini, G.; Calcaterra, F.; Lombardi, S.; Marini, F.; Zenari, L.; Saggiani, F.; Poli, M.; Perbellini, S.; Raffaelli, A. HOMA-estimated insulin resistance is an independent predictor of cardiovascular disease in type 2 diabetic subjects: Prospective data from the Verona Diabetes Complications Study. Diabetes Care 2002, 25, 1135–1141. [Google Scholar] [CrossRef]
- Rodriguez-Ramirez, S.; Mundo-Rosas, V.; Jimenez-Aguilar, A.; Shamah-Levy, T. Methodology for the analysis of dietary data from the Mexican National Health and Nutrition Survey 2006. Salud Publica Mex. 2009, 51 (Suppl. 4), S523–S529. [Google Scholar] [CrossRef]
- INSP; National Institute of Public Health. The Compiled México-INSP Food Composition Data Bank; National Institute of Public Health: Saitama, Japan, 2002. [Google Scholar]
- Fung, T.T.; Chiuve, S.E.; McCullough, M.L.; Rexrode, K.M.; Logroscino, G.; Hu, F.B. Adherence to a DASH-style diet and risk of coronary heart disease and stroke in women. Arch. Intern. Med. 2008, 168, 713–720. [Google Scholar] [CrossRef]
- Fung, T.T.; McCullough, M.L.; Newby, P.K.; Manson, J.E.; Meigs, J.B.; Rifai, N.; Willett, W.C.; Hu, F.B. Diet-quality scores and plasma concentrations of markers of inflammation and endothelial dysfunction. Am. J. Clin. Nutr. 2005, 82, 163–173. [Google Scholar] [CrossRef]
- Tognon, G.; Moreno, L.A.; Mouratidou, T.; Veidebaum, T.; Molnar, D.; Russo, P.; Siani, A.; Akhandaf, Y.; Krogh, V.; Tornaritis, M.; et al. Adherence to a Mediterranean-like dietary pattern in children from eight European countries. The IDEFICS study. Int. J. Obes. 2014, 38 (Suppl. 2), S108–S114. [Google Scholar] [CrossRef]
- Khan, S.; Wirth, M.D.; Ortaglia, A.; Alvarado, C.R.; Shivappa, N.; Hurley, T.G.; Hebert, J.R. Design, Development and Construct Validation of the Children’s Dietary Inflammatory Index. Nutrients 2018, 10, 993. [Google Scholar] [CrossRef]
- Kim, Y.; Chen, J.; Wirth, M.D.; Shivappa, N.; Hebert, J.R. Lower Dietary Inflammatory Index Scores Are Associated with Lower Glycemic Index Scores among College Students. Nutrients 2018, 10, 182. [Google Scholar] [CrossRef] [PubMed]
- Kasper, N.; Peterson, K.E.; Zhang, Z.; Ferguson, K.K.; Sanchez, B.N.; Cantoral, A.; Meeker, J.D.; Tellez-Rojo, M.M.; Pawlowski, C.M.; Ettinger, A.S. Association of Bisphenol A Exposure with Breastfeeding and Perceived Insufficient Milk Supply in Mexican Women. Matern. Child Health J. 2016, 20, 1713–1719. [Google Scholar] [CrossRef] [PubMed]
- Hernández, B.; Gortmaker, S.L.; Laird, N.M.; Colditz, G.A.; Parra-Cabrera, S.; Peterson, K.E. Validez y reproducibilidad de un cuestionario de actividad e inactividad física para escolares de la ciudad de México. Salud Pública De México 2000, 42, 315–323. [Google Scholar] [CrossRef]
- Ainsworth, B.E.; Haskell, W.L.; Whitt, M.C.; Irwin, M.L.; Swartz, A.M.; Strath, S.J.; O’Brien, W.L.; Bassett, D.R., Jr.; Schmitz, K.H.; Emplaincourt, P.O.; et al. Compendium of physical activities: An update of activity codes and MET intensities. Med. Sci. Sports Exerc. 2000, 32, S498–S504. [Google Scholar] [CrossRef] [PubMed]
- Chavarro, J.E.; Watkins, D.J.; Afeiche, M.C.; Zhang, Z.; Sanchez, B.N.; Cantonwine, D.; Mercado-Garcia, A.; Blank-Goldenberg, C.; Meeker, J.D.; Tellez-Rojo, M.M.; et al. Validity of Self-Assessed Sexual Maturation Against Physician Assessments and Hormone Levels. J. Pediatr. 2017, 186, 172–178. [Google Scholar] [CrossRef]
- Marshall, W.A.; Tanner, J.M. Variations in pattern of pubertal changes in girls. Arch. Dis. Child. 1969, 44, 291–303. [Google Scholar] [CrossRef]
- Marshall, W.A.; Tanner, J.M. Variations in the pattern of pubertal changes in boys. Arch. Dis. Child. 1970, 45, 13–23. [Google Scholar] [CrossRef]
- LaBarre, J.L.; Peterson, K.E.; Kachman, M.T.; Perng, W.; Tang, L.; Hao, W.; Zhou, L.; Karnovsky, A.; Cantoral, A.; Tellez-Rojo, M.M.; et al. Mitochondrial Nutrient Utilization Underlying the Association Between Metabolites and Insulin Resistance in Adolescents. J. Clin. Endocrinol. Metab. 2020, 105, dgaa260. [Google Scholar] [CrossRef] [PubMed]
- Taylor, R.W.; Grant, A.M.; Williams, S.M.; Goulding, A. Sex differences in regional body fat distribution from pre- to postpuberty. Obesity (Silver Spring) 2010, 18, 1410–1416. [Google Scholar] [CrossRef] [PubMed]
- Shirani, F.; Salehi-Abargouei, A.; Azadbakht, L. Effects of Dietary Approaches to Stop Hypertension (DASH) diet on some risk for developing type 2 diabetes: A systematic review and meta-analysis on controlled clinical trials. Nutrition 2013, 29, 939–947. [Google Scholar] [CrossRef]
- Saneei, P.; Hashemipour, M.; Kelishadi, R.; Rajaei, S.; Esmaillzadeh, A. Effects of recommendations to follow the Dietary Approaches to Stop Hypertension (DASH) diet v. usual dietary advice on childhood metabolic syndrome: A randomised cross-over clinical trial. Br. J. Nutr. 2013, 110, 2250–2259. [Google Scholar] [CrossRef]
- Veronese, N.; Watutantrige-Fernando, S.; Luchini, C.; Solmi, M.; Sartore, G.; Sergi, G.; Manzato, E.; Barbagallo, M.; Maggi, S.; Stubbs, B. Effect of magnesium supplementation on glucose metabolism in people with or at risk of diabetes: A systematic review and meta-analysis of double-blind randomized controlled trials. Eur. J. Clin. Nutr. 2016, 70, 1354–1359. [Google Scholar] [CrossRef]
- Lind, M.V.; Lauritzen, L.; Kristensen, M.; Ross, A.B.; Eriksen, J.N. Effect of folate supplementation on insulin sensitivity and type 2 diabetes: A meta-analysis of randomized controlled trials. Am. J. Clin. Nutr. 2019, 109, 29–42. [Google Scholar] [CrossRef]
- Akhlaghi, M. Dietary Approaches to Stop Hypertension (DASH): Potential mechanisms of action against risk factors of the metabolic syndrome. Nutr. Res. Rev. 2020, 33, 1–18. [Google Scholar] [CrossRef] [PubMed]
- Barbosa-Cortes, L.; Villasis-Keever, M.A.; Del Prado-Manriquez, M.; Lopez-Alarcon, M. Adiposity and Insulin Resistance in Children from a Rural Community in Mexico. Arch. Med. Res. 2015, 46, 214–220. [Google Scholar] [CrossRef] [PubMed]
- Weiss, R.; Kaufman, F.R. Metabolic complications of childhood obesity: Identifying and mitigating the risk. Diabetes Care 2008, 31 (Suppl. 2), S310–S316. [Google Scholar] [CrossRef]
- Bray, G.A.; Heisel, W.E.; Afshin, A.; Jensen, M.D.; Dietz, W.H.; Long, M.; Kushner, R.F.; Daniels, S.R.; Wadden, T.A.; Tsai, A.G.; et al. The Science of Obesity Management: An Endocrine Society Scientific Statement. Endocr. Rev. 2018, 39, 79–132. [Google Scholar] [CrossRef] [PubMed]
- Bricarello, L.P.; de Moura Souza, A.; de Almeida Alves, M.; Retondario, A.; Fernandes, R.; Santos de Moraes Trindade, E.B.; Zanette Ramos Zeni, L.A.; de Assis Guedes de Vasconcelos, F. Association between DASH diet (Dietary Approaches to Stop Hypertension) and hypertension in adolescents: A cross-sectional school-based study. Clin. Nutr. ESPEN 2020, 36, 69–75. [Google Scholar] [CrossRef] [PubMed]
- Laufs, U.; Parhofer, K.G.; Ginsberg, H.N.; Hegele, R.A. Clinical review on triglycerides. Eur. Heart J. 2020, 41, 99–109c. [Google Scholar] [CrossRef] [PubMed]
- Valaiyapathi, B.; Sunil, B.; Ashraf, A.P. Approach to Hypertriglyceridemia in the Pediatric Population. Pediatr. Rev. 2017, 38, 424–434. [Google Scholar] [CrossRef] [PubMed]
- Williams, L.A.; Wilson, D.P. Nutritional Management of Pediatric Dyslipidemia. In Endotext; 2020. Available online: https://www.ncbi.nlm.nih.gov/books/NBK395582/ (accessed on 5 January 2022).
- Morrison, A.; Hokanson, J.E. The independent relationship between triglycerides and coronary heart disease. Vasc. Health Risk Manag. 2009, 5, 89–95. [Google Scholar] [CrossRef] [PubMed]
- Hokanson, J.E.; Austin, M.A. Plasma triglyceride level is a risk factor for cardiovascular disease independent of high-density lipoprotein cholesterol level: A meta-analysis of population-based prospective studies. J. Cardiovasc. Risk 1996, 3, 213–219. [Google Scholar] [CrossRef]
- Nordestgaard, B.G.; Varbo, A. Triglycerides and cardiovascular disease. Lancet 2014, 384, 626–635. [Google Scholar] [CrossRef]
- Sarwar, N.; Danesh, J.; Eiriksdottir, G.; Sigurdsson, G.; Wareham, N.; Bingham, S.; Boekholdt, S.M.; Khaw, K.T.; Gudnason, V. Triglycerides and the risk of coronary heart disease: 10,158 incident cases among 262,525 participants in 29 Western prospective studies. Circulation 2007, 115, 450–458. [Google Scholar] [CrossRef]
- Velázquez-López, L.; Santiago-Díaz, G.; Nava-Hernández, J.; Muñoz-Torres, A.V.; Medina-Bravo, P.; Torres-Tamayo, M. Mediterranean-style diet reduces metabolic syndrome components in obese children and adolescents with obesity. BMC Pediatrics 2014, 14, 175. [Google Scholar] [CrossRef]
- Grao-Cruces, E.; Varela, L.M.; Martin, M.E.; Bermudez, B.; Montserrat-de la Paz, S. High-Density Lipoproteins and Mediterranean Diet: A Systematic Review. Nutrients 2021, 13, 955. [Google Scholar] [CrossRef]
- Barragan-Vazquez, S.; Ariza, A.C.; Ramirez Silva, I.; Pedraza, L.S.; Rivera Dommarco, J.A.; Ortiz-Panozo, E.; Zambrano, E.; Reyes Castro, L.A.; Shivappa, N.; Hebert, J.R.; et al. Pro-Inflammatory Diet Is Associated with Adiposity during Childhood and with Adipokines and Inflammatory Markers at 11 Years in Mexican Children. Nutrients 2020, 12, 3658. [Google Scholar] [CrossRef]
- Taylor, R.W.; Jones, I.E.; Williams, S.M.; Goulding, A. Evaluation of waist circumference, waist-to-hip ratio, and the conicity index as screening tools for high trunk fat mass, as measured by dual-energy X-ray absorptiometry, in children aged 3-19 y. Am. J. Clin. Nutr. 2000, 72, 490–495. [Google Scholar] [CrossRef]
- Matsushita, Y.; Nakagawa, T.; Shinohara, M.; Yamamoto, S.; Takahashi, Y.; Mizoue, T.; Yokoyama, T.; Noda, M. How can waist circumference predict the body composition? Diabetol. Metab. Syndr. 2014, 6, 11. [Google Scholar] [CrossRef]
- Eissa, M.A.; Dai, S.; Mihalopoulos, N.L.; Day, R.S.; Harrist, R.B.; Labarthe, D.R. Trajectories of fat mass index, fat free-mass index, and waist circumference in children: Project HeartBeat! Am. J. Prev. Med. 2009, 37, S34–S39. [Google Scholar] [CrossRef]
- Hebert, J.J.; Senechal, M.; Fairchild, T.; Moller, N.C.; Klakk, H.; Wedderkopp, N. Developmental Trajectories of Body Mass Index, Waist Circumference, and Aerobic Fitness in Youth: Implications for Physical Activity Guideline Recommendations (CHAMPS Study-DK). Sports Med. 2020, 50, 2253–2261. [Google Scholar] [CrossRef]
- Bricarello, L.P.; de Almeida Alves, M.; Retondario, A.; de Moura Souza, A.; de Vasconcelos, F.A.G. DASH diet (Dietary Approaches to Stop Hypertension) and overweight/obesity in adolescents: The ERICA study. Clin. Nutr. ESPEN 2021, 42, 173–179. [Google Scholar] [CrossRef] [PubMed]
- Golpour-Hamedani, S.; Mohammadifard, N.; Khosravi, A.; Feizi, A.; Safavi, S.M. Dietary approaches to stop hypertension diet and obesity: A cross-sectional study of Iranian children and adolescents. ARYA Atheroscler. 2017, 13, 7–13. [Google Scholar]
- Jansen, E.C.; Marcovitch, H.; Wolfson, J.A.; Leighton, M.; Peterson, K.E.; Tellez-Rojo, M.M.; Cantoral, A.; Roberts, E.F.S. Exploring dietary patterns in a Mexican adolescent population: A mixed methods approach. Appetite 2020, 147, 104542. [Google Scholar] [CrossRef] [PubMed]
- Jayanama, K.; Theou, O.; Godin, J.; Cahill, L.; Shivappa, N.; Hébert, J.R.; Wirth, M.D.; Park, Y.-M.; Fung, T.T.; Rockwood, K. Relationship between diet quality scores and the risk of frailty and mortality in adults across a wide age spectrum. BMC Med. 2021, 19, 1–13. [Google Scholar] [CrossRef] [PubMed]
- Fallaize, R.; Livingstone, K.M.; Celis-Morales, C.; Macready, A.L.; San-Cristobal, R.; Navas-Carretero, S.; Marsaux, C.F.M.; O’Donovan, C.B.; Kolossa, S.; Moschonis, G.; et al. Association between Diet-Quality Scores, Adiposity, Total Cholesterol and Markers of Nutritional Status in European Adults: Findings from the Food4Me Study. Nutrients 2018, 10, 49. [Google Scholar] [CrossRef]
- Jacobs, S.; Harmon, B.E.; Ollberding, N.J.; Wilkens, L.R.; Monroe, K.R.; Kolonel, L.N.; Le Marchand, L.; Boushey, C.J.; Maskarinec, G. Among 4 Diet Quality Indexes, Only the Alternate Mediterranean Diet Score Is Associated with Better Colorectal Cancer Survival and Only in African American Women in the Multiethnic Cohort. J. Nutr. 2016, 146, 1746–1755. [Google Scholar] [CrossRef] [PubMed]
- Harmon, B.E.; Boushey, C.J.; Shvetsov, Y.B.; Ettienne, R.; Reedy, J.; Wilkens, L.R.; Le Marchand, L.; Henderson, B.E.; Kolonel, L.N. Associations of key diet-quality indexes with mortality in the Multiethnic Cohort: The Dietary Patterns Methods Project. Am. J. Clin. Nutr. 2015, 101, 587–597. [Google Scholar] [CrossRef]
- Sotos-Prieto, M.; Bhupathiraju, S.N.; Mattei, J.; Fung, T.T.; Li, Y.; Pan, A.; Willett, W.C.; Rimm, E.B.; Hu, F.B. Changes in Diet Quality Scores and Risk of Cardiovascular Disease Among US Men and Women. Circulation 2015, 132, 2212–2219. [Google Scholar] [CrossRef]
- Tabung, F.K.; Smith-Warner, S.A.; Chavarro, J.E.; Fung, T.T.; Hu, F.B.; Willett, W.C.; Giovannucci, E.L. An Empirical Dietary Inflammatory Pattern Score Enhances Prediction of Circulating Inflammatory Biomarkers in Adults. J. Nutr. 2017, 147, 1567–1577. [Google Scholar] [CrossRef] [PubMed]
- Chinapaw, M.; Klakk, H.; Moller, N.C.; Andersen, L.B.; Altenburg, T.; Wedderkopp, N. Total volume versus bouts: Prospective relationship of physical activity and sedentary time with cardiometabolic risk in children. Int. J. Obes. 2018, 42, 1733–1742. [Google Scholar] [CrossRef]
- Stamatakis, E.; Coombs, N.; Tiling, K.; Mattocks, C.; Cooper, A.; Hardy, L.L.; Lawlor, D.A. Sedentary time in late childhood and cardiometabolic risk in adolescence. Pediatrics 2015, 135, e1432–e1441. [Google Scholar] [CrossRef]
- Winpenny, E.M.; van Sluijs, E.M.F.; Forouhi, N.G. How do short-term associations between diet quality and metabolic risk vary with age? Eur. J. Nutr. 2021, 60, 517–527. [Google Scholar] [CrossRef]
- Wynder, E.L.; Hebert, J.R. Homogeneity in nutritional exposure: An impediment in cancer epidemiology. J. Natl. Cancer Inst. 1987, 79, 605–607. [Google Scholar]
- Hebert, J.R.; Shivappa, N.; Wirth, M.D.; Hussey, J.R.; Hurley, T.G. Perspective: The Dietary Inflammatory Index (DII)-Lessons Learned, Improvements Made, and Future Directions. Adv. Nutr. 2019, 10, 185–195. [Google Scholar] [CrossRef]
- Rosato, V.; Temple, N.J.; La Vecchia, C.; Castellan, G.; Tavani, A.; Guercio, V. Mediterranean diet and cardiovascular disease: A systematic review and meta-analysis of observational studies. Eur. J. Nutr. 2019, 58, 173–191. [Google Scholar] [CrossRef] [PubMed]
- Trichopoulou, A.; Kouris-Blazos, A.; Wahlqvist, M.L.; Gnardellis, C.; Lagiou, P.; Polychronopoulos, E.; Vassilakou, T.; Lipworth, L.; Trichopoulos, D. Diet and overall survival in elderly people. BMJ (Clin. Res. Ed.) 1995, 311, 1457–1460. [Google Scholar] [CrossRef]
- Tong, T.Y.; Wareham, N.J.; Khaw, K.T.; Imamura, F.; Forouhi, N.G. Prospective association of the Mediterranean diet with cardiovascular disease incidence and mortality and its population impact in a non-Mediterranean population: The EPIC-Norfolk study. BMC Med. 2016, 14, 135. [Google Scholar] [CrossRef] [PubMed]
- Shivappa, N.; Steck, S.E.; Hurley, T.G.; Hussey, J.R.; Hebert, J.R. Designing and developing a literature-derived, population-based dietary inflammatory index. Public Health Nutr. 2014, 17, 1689–1696. [Google Scholar] [CrossRef]
- Livingstone, M.B.; Robson, P.J.; Wallace, J.M. Issues in dietary intake assessment of children and adolescents. Br. J. Nutr. 2004, 92 (Suppl. 2), S213–S222. [Google Scholar] [CrossRef]
- Perez-Rodrigo, C.; Artiach Escauriaza, B.; Artiach Escauriaza, J.; Polanco Allue, I. Dietary assessment in children and adolescents: Issues and recommendations. Nutr. Hosp. 2015, 31 (Suppl. 3), 76–83. [Google Scholar] [CrossRef]
- Ocke, M.C. Evaluation of methodologies for assessing the overall diet: Dietary quality scores and dietary pattern analysis. Proc. Nutr. Soc. 2013, 72, 191–199. [Google Scholar] [CrossRef] [PubMed]
- Tapsell, L.C.; Neale, E.P.; Satija, A.; Hu, F.B. Foods, Nutrients, and Dietary Patterns: Interconnections and Implications for Dietary Guidelines. Adv. Nutr. 2016, 7, 445–454. [Google Scholar] [CrossRef] [PubMed]
- Poulain, T.; Spielau, U.; Vogel, M.; Korner, A.; Kiess, W. CoCu: A new short questionnaire to evaluate diet composition and culture of eating in children and adolescents. Clin. Nutr. 2019, 38, 2858–2865. [Google Scholar] [CrossRef] [PubMed]
- Malik, V.S.; Fung, T.T.; van Dam, R.M.; Rimm, E.B.; Rosner, B.; Hu, F.B. Dietary patterns during adolescence and risk of type 2 diabetes in middle-aged women. Diabetes Care 2012, 35, 12–18. [Google Scholar] [CrossRef] [PubMed]
- Moubarac, J. Ultra-Processed Food and Drink Products in Latin America: Trends, Impact on Obesity, Policy Implications; PAHO: Washington, DC, USA, 2015; pp. 1–58. [Google Scholar]
- Baker, P.; Machado, P.; Santos, T.; Sievert, K.; Backholer, K.; Hadjikakou, M.; Russell, C.; Huse, O.; Bell, C.; Scrinis, G.; et al. Ultra-processed foods and the nutrition transition: Global, regional and national trends, food systems transformations and political economy drivers. Obes. Rev. 2020, 21, e13126. [Google Scholar] [CrossRef]
| Time 1 N = 250 | Time 2 N = 554 | Time 3 N = 518 | |
|---|---|---|---|
| Maternal Characteristics (at time of child’s birth) | |||
| Years of education, % | |||
| <12 years | 123 (49.20) 1 | 284 (51.26) 2 | 265 (51.16) 2 |
| 12 years | 91 (36.40) 1 | 187 (33.75) 2 | 171 (33.01) 2 |
| >12 years | 35 (14.00) 1 | 78 (14.08) 2 | 77 (14.86) 2 |
| Age at childbirth, (years) | 26.80 (5.63) 1 | 26.36 (5.40) 3 | 26.38 (5.44) 3 |
| Parity, % | |||
| 1 | 93 (37.20) 1 | 209 (37.73) 2 | 194 (37.45) 2 |
| 2 | 89 (35.60) 1 | 194 (35.02) 2 | 183 (35.02) 2 |
| ≥3 | 67 (26.80) 1 | 146 (26.35) 2 | 136 (26.25) 2 |
| Marital status, % | |||
| Married | 178 (71.20) 1 | 390 (70.40) 4 | 363 (70.08) 4 |
| Others | 71 (28.40) 1 | 157 (28.34) 4 | 148 (28.57) 4 |
| Enrollment in calcium supplementation study, % | |||
| Not enrolled | 154 (61.60) 1 | 399 (72.02) 2 | 375 (72.39) 2 |
| Enrolled | 95 (38.00) 1 | 150 (27.08) 2 | 138 (26.64) 2 |
| Child characteristics (at birth) | |||
| Female, % | 132 (52.80) | 286 (51.62) | 273 (52.70) |
| Gestation age, (weeks) | 38.85 (1.49) 5 | 38.76 (1.61) 6 | 38.75 (1.60) 6 |
| Mode of delivery, % | |||
| Vaginal delivery | 144 (57.60) 7 | 352 (63.54) 8 | 329 (63.51) 8 |
| C-Section | 103 (41.20) 7 | 194 (35.02) 8 | 181 (34.94) 8 |
| Birth weight, (kg) | 3.15 (0.45) 9 | 3.15 (0.49) 4 | 3.15 (0.48) 4 |
| Breastfeeding duration, (months) | 8.10 (5.88) 1 | 8.05 (6.07) 2 | 8.00 (5.98) 2 |
| Child characteristics (at follow-up visits) | |||
| Age, (years) | 10.32 (1.67) | 14.50 (2.12) | 16.43 (2.14) |
| Body mass index, (kg/m2) | 19.38 (3.60) | 21.62 (4.15) | 22.81 (4.46) |
| Body mass Z score for age | 0.84 (1.24) | 0.50 (1.25) 8 | 0.50 (1.25) 10 |
| Pubertal onset, % | 175 (70.00) | 545 (98.38) | 515 (99.42) 11 |
| Metabolic equivalents, (METs/week) | 31.39 (19.82) | 57.23 (39.01) | 44.95 (35.18) 1 |
| Cardiometabolic risk factors | |||
| Waist circumference, (cm) | 70.75 (10.67) | 79.56 (11.38) | 85.53 (11.80) 1 |
| Systolic blood pressure, (mmHg) | 102.68 (10.20) | 98.66 (9.92) | 101.53 (9.83) 1 |
| Diastolic blood pressure, (mmHg) | 65.52 (7.32) | 63.03 (6.86) | 64.14 (7.20) 1 |
| Glucose, (mg/dL) | 87.02 (9.36) | 77.81 (7.27) 12 | 90.22 (8.41) 13 |
| TG, (mg/dL) | 87.54(44.41) | 103.97 (55.85) 12 | 105.52 (50.09) 13 |
| HDL-C, (mg/dL) | 58.68 (11.94) | 43.06 (8.60) 12 | 44.70 (9.03) 13 |
| Insulin, (μIU/mL) | 6.26 (11.03) 14 | 19.06 (11.84) 12 | 19.21 (12.62) 15 |
| HOMA-IR | 1.59 (3.51) 14 | 3.69 (2.31) 12 | 4.32 (2.94) 15 |
| Diet quality scores | |||
| DASH diet scores | 24.84 (4.06) | 24.23 (3.99) | 24.00 (4.00) |
| aMedDiet scores | 4.26 (1.83) | 3.81 (1.67) | 3.77 (1.69) |
| C-DII scores | −0.16 (1.35) | −0.11 (1.43) | −0.10 (1.46) |
| DASH Score 1 | Waist Circumference (cm) | Systolic Blood Pressure (mmHg) | Diastolic Blood Pressure (mmHg) | Glucose (mg/dL) | Log TG (mg/dL) | HDL-C (mg/dL) | Log Insulin (μIU/mL) | Log HOMA-IR | |||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| All N = 574 | Boys N = 274 | Girls N = 300 | All N = 574 | Boys N = 274 | Girls N = 300 | All N = 574 | Boys N = 274 | Girls N = 300 | All N = 435 | Boys N = 213 | Girls N = 222 | All N = 435 | Boys N = 213 | Girls N = 222 | All N = 435 | Boys N = 213 | Girls N = 222 | All N = 410 | Boys N = 202 | Girls N = 208 | All N = 410 | Boys N = 202 | Girls N = 208 | ||
| # obs. = 1297 | # obs. = 621 | # obs. = 676 | # obs. = 1296 | # obs. = 621 | # obs.= 675 | # obs. = 1296 | # obs. = 621 | # obs.= 675 | # obs. = 1012 | # obs.= 495 | # obs.= 517 | # obs. = 1012 | # obs. = 495 | # obs.= 517 | # obs. = 1012 | # obs. = 495 | # obs.= 517 | # obs. = 840 | # obs. = 402 | # obs.= 438 | # obs. = 840 | # obs. = 402 | # obs.= 438 | ||
| Crude model 2 | |||||||||||||||||||||||||
| Quartile 1 Median = 19 | (Ref) | (Ref) | (Ref) | (Ref) | (Ref) | (Ref) | (Ref) | (Ref) | (Ref) | (Ref) | (Ref) | (Ref) | (Ref) | (Ref) | (Ref) | (Ref) | (Ref) | (Ref) | (Ref) | (Ref) | (Ref) | (Ref) | (Ref) | (Ref) | |
| Quartile 2 Median = 23 | β SE | 0.3290 0.7379 | −1.7641 0.9053 | 2.6736 1.1428 | −0.2851 0.7010 | −1.1086 1.0205 | 0.5242 0.9425 | 0.1422 0.5197 | −0.3087 0.7595 | 0.6257 0.7036 | −0.01814 0.01028 | −0.03199 0.01421 | −0.00497 0.01462 | −0.02739 0.03915 | −0.03320 0.05055 | −0.00404 0.05795 | 0.3166 0.9464 | 2.5288 1.3624 | −1.7406 1.2842 | −0.1135 0.06004 | −0.1376 0.08008 | −0.09521 0.08672 | −0.1357 0.06520 | −0.1861 0.08607 | −0.09082 0.09513 |
| p-value | 0.6557 | 0.0520 | 0.0197 | 0.6843 | 0.2778 | 0.5783 | 0.7844 | 0.6846 | 0.3741 | 0.0779 | 0.0249 | 0.7342 | 0.4843 | 0.5118 | 0.9445 | 0.7380 | 0.0640 | 0.1760 | 0.0591 | 0.0865 | 0.2730 | 0.0377 | 0.0312 | 0.3403 | |
| Quartile 3 Median = 26 | β SE | 0.09201 0.7617 | −2.7801 0.9663 | 2.8635 1.1434 | −0.6746 0.7160 | −2.1720 1.0700 | 0.9136 0.9372 | 0.1368 0.5285 | −0.8724 0.7908 | 1.2081 0.6986 | −0.00357 0.01012 | −0.01102 0.01431 | 0.003340 0.01406 | −0.04297 0.04017 | −0.08885 0.05455 | −0.00079 0.05725 | 0.8016 0.9592 | 2.6308 1.4055 | −1.0614 1.2775 | −0.02292 0.05840 | −0.1146 0.08184 | 0.04391 0.08160 | −0.03110 0.06276 | −0.1482 0.08715 | 0.05679 0.08886 |
| p-value | 0.9039 | 0.0042 * | 0.0125 | 0.3463 | 0.0428 | 0.3300 | 0.7958 | 0.2704 | 0.0842 | 0.7242 | 0.4417 | 0.8123 | 0.2851 | 0.1041 | 0.9891 | 0.4035 | 0.0618 | 0.4065 | 0.0591 | 0.1623 | 0.5908 | 0.6203 | 0.0899 | 0.5231 | |
| Quartile 4 Median = 29 | β SE | −0.9829 0.8514 | −2.5003 1.1382 | 0.5892 1.2309 | −0.4748 0.7877 | −0.3090 1.2243 | −0.05971 0.9996 | 0.003925 0.5772 | −0.6580 0.8948 | 0.8226 0.7432 | −0.02344 0.01078 | −0.02786 0.01572 | −0.01465 0.01458 | −0.07407 0.04518 | −0.06178 0.06286 | −0.08139 0.06342 | 1.0313 1.0494 | 3.4680 1.5760 | −1.2203 1.3620 | −0.1721 0.07142 | −0.2227 0.1047 | −0.1375 0.09639 | −0.2218 0.07850 | −0.2619 0.1118 | −0.1895 0.1084 |
| p-value | 0.2485 | 0.0285 | 0.6323 | 0.5468 | 0.8008 | 0.9524 | 0.9946 | 0.4624 | 0.2687 | 0.0300 | 0.0771 | 0.3153 | 0.1015 | 0.3262 | 0.1999 | 0.3260 | 0.0282 | 0.3707 | 0.0162 | 0.0340 | 0.1546 | 0.0048 * | 0.0197 | 0.0810 | |
| Linear | β SE | −0.08280 0.08159 | −0.2866 0.1078 | 0.07905 0.1193 | −0.05908 0.07507 | −0.1037 0.1157 | 0.01289 0.09584 | 0.002651 0.05492 | −0.08367 0.08410 | 0.09677 0.07117 | −0.00164 0.001019 | −0.00197 0.001488 | −0.00100 0.001378 | −0.00708 0.004278 | −0.00823 0.006007 | −0.00661 0.005922 | 0.1084 0.1000 | 0.3329 0.1490 | −0.09810 0.1309 | −0.01183 0.006560 | −0.01964 0.009345 | −0.00729 0.008975 | −0.01537 0.007096 | −0.02392 0.01002 | −0.01054 0.009819 |
| p-value | 0.3104 | 0.0081 | 0.5077 | 0.4314 | 0.3705 | 0.8930 | 0.9615 | 0.3202 | 0.1744 | 0.1081 | 0.1873 | 0.4704 | 0.0985 | 0.1715 | 0.2652 | 0.2787 | 0.0259 | 0.4539 | 0.0718 | 0.0362 | 0.4173 | 0.0306 | 0.0174 | 0.2835 | |
| Adjusted model 3,4,5 | |||||||||||||||||||||||||
| Quartile 1 Median = 19 | (Ref) | (Ref) | (Ref) | (Ref) | (Ref) | (Ref) | (Ref) | (Ref) | (Ref) | (Ref) | (Ref) | (Ref) | (Ref) | (Ref) | (Ref) | (Ref) | (Ref) | (Ref) | (Ref) | (Ref) | (Ref) | (Ref) | (Ref) | (Ref) | |
| Quartile 2 Median = 23 | β SE | 0.5597 0.2438 | 0.1253 0.2953 | 1.1055 0.3838 | −0.3056 0.6906 | −0.7790 1.0089 | 0.4733 0.9382 | 0.1631 0.5152 | −0.07641 0.7473 | 0.6637 0.7018 | −0.01824 0.01016 | −0.02924 0.01417 | −0.00462 0.01460 | −0.02871 0.03882 | −0.02728 0.04990 | 0.006651 0.05742 | 0.3541 0.7539 | 1.7154 1.0650 | −1.3066 1.0386 | −0.1192 0.05586 | −0.1711 0.07680 | −0.09504 0.08028 | −0.1502 0.06118 | −0.2224 0.08116 | −0.1166 0.09012 |
| p-value | 0.0219 | 0.6716 | 0.0041 * | 0.6582 | 0.4403 | 0.6141 | 0.7517 | 0.9186 | 0.3447 | 0.0730 | 0.0396 | 0.7519 | 0.4597 | 0.5850 | 0.9078 | 0.6387 | 0.1080 | 0.2091 | 0.0332 | 0.0265 | 0.2372 | 0.0143 | 0.0065 | 0.1966 | |
| Quartile 3 Median = 26 | β SE | −0.03468 0.2509 | −0.3516 0.3155 | 0.3894 0.3828 | −0.5741 0.7030 | −1.6714 1.0605 | 0.9477 0.9303 | 0.1587 0.5221 | −0.4328 0.7793 | 1.2149 0.6949 | −0.00317 0.01002 | −0.01045 0.01442 | 0.004289 0.01412 | −0.04299 0.03956 | −0.08448 0.05358 | 0.01517 0.05701 | 0.9758 0.7707 | 1.8873 1.1168 | −0.2532 1.0372 | −0.05021 0.05519 | −0.1367 0.07799 | 0.000769 0.07804 | −0.06758 0.05980 | −0.1734 0.08134 | −0.00826 0.08641 |
| p-value | 0.8901 | 0.2657 | 0.3095 | 0.4143 | 0.1155 | 0.3087 | 0.7613 | 0.5789 | 0.0809 | 0.7520 | 0.4691 | 0.7615 | 0.2775 | 0.1156 | 0.7903 | 0.2058 | 0.0917 | 0.8073 | 0.3633 | 0.0805 | 0.9921 | 0.2588 | 0.0337 | 0.9239 | |
| Quartile 4 Median = 29 | β SE | −0.01519 0.2811 | −0.2061 0.3711 | 0.2409 0.4103 | −0.1163 0.7730 | 0.08917 1.2070 | 0.1322 0.9899 | 0.1862 0.5695 | −0.3518 0.8722 | 0.9279 0.7372 | −0.02130 0.01076 | −0.02664 0.01584 | −0.01395 0.01466 | −0.06989 0.04442 | −0.05062 0.06156 | −0.07330 0.06244 | 1.0360 0.8555 | 3.1918 1.2780 | −0.9157 1.1101 | −0.1943 0.06607 | −0.3012 0.1027 | −0.1310 0.08773 | −0.2482 0.07341 | −0.3569 0.1085 | −0.1934 0.1006 |
| p-value | 0.9569 | 0.5790 | 0.5574 | 0.8804 | 0.9411 | 0.8938 | 0.7437 | 0.6868 | 0.2086 | 0.0481 | 0.0933 | 0.3417 | 0.1160 | 0.4114 | 0.2410 | 0.2262 | 0.0128 | 0.4099 | 0.0034 * | 0.0036 * | 0.1363 | 0.0008 * | 0.0011 * | 0.0553 | |
| Linear | β SE | −0.01519 0.02697 | −0.03387 0.03519 | 0.004382 0.03969 | −0.02563 0.07361 | −0.05473 0.1142 | 0.03158 0.09487 | 0.01777 0.05413 | −0.04452 0.08211 | 0.1047 0.07058 | −0.00144 0.001019 | −0.00192 0.001505 | −0.00091 0.001387 | −0.00672 0.004210 | −0.00729 0.005891 | −0.00565 0.005834 | 0.1149 0.08184 | 0.2951 0.1214 | −0.05378 0.1069 | −0.01475 0.006133 | −0.02550 0.009040 | −0.00870 0.008334 | −0.01893 0.006733 | −0.03099 0.009520 | −0.01338 0.009395 |
| p-value | 0.5735 | 0.3361 | 0.9121 | 0.7277 | 0.6319 | 0.7393 | 0.7427 | 0.5878 | 0.1384 | 0.1571 | 0.2032 | 0.5108 | 0.1106 | 0.2166 | 0.3336 | 0.1608 | 0.0154 | 0.6153 | 0.0164 | 0.0050 * | 0.2970 | 0.0050 * | 0.0012 * | 0.1550 | |
| aMedDiet Score 1 | Waist Circumference (cm) | Systolic Blood Pressure (mmHg) | Diastolic Blood Pressure (mmHg) | Log Glucose (mg/dL) | Log TG (mg/dL) | HDL-C (mg/dL) | Log Insulin (μIU/mL) | Log HOMA-IR | |||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| All N = 570 | Boys N = 273 | Girls N = 297 | All N = 570 | Boys N = 273 | Girls N = 297 | All N = 570 | Boys N = 273 | Girls N = 297 | All N = 432 | Boys N = 212 | Girls N = 220 | All N = 432 | Boys N = 212 | Girls N = 220 | All N = 432 | Boys N = 212 | Girls N = 220 | All N = 407 | Boys N = 201 | Girls N = 206 | All N = 407 | Boys N = 201 | Girls N = 206 | ||
| # obs. = 1289 | # obs. = 618 | # obs. = 671 | # obs. = 1289 | # obs. = 618 | # obs. = 670 | # obs. = 1289 | # obs. = 618 | # obs.= 670 | # obs. = 1006 | # obs. = 492 | # obs. = 514 | # obs. = 1006 | # obs. = 492 | # obs. = 514 | # obs. = 1006 | # obs. = 492 | # obs. = 514 | # obs. = 835 | # obs. = 400 | # obs.= 435 | # obs. = 835 | # obs. = 400 | # obs. = 435 | ||
| Crude model 2 | |||||||||||||||||||||||||
| Quartile 1 Median = 2 | (Ref) | (Ref) | (Ref) | (Ref) | (Ref) | (Ref) | (Ref) | (Ref) | (Ref) | (Ref) | (Ref) | (Ref) | (Ref) | (Ref) | (Ref) | (Ref) | (Ref) | (Ref) | (Ref) | (Ref) | (Ref) | (Ref) | (Ref) | (Ref) | |
| Quartile 2 Median = 3 | β SE | −0.00397 0.7844 | 0.7594 0.9800 | −0.9840 1.2059 | 0.4164 0.7559 | 1.3783 1.1285 | −0.5512 0.9909 | −0.08385 0.5620 | −0.05524 0.8456 | −0.07809 0.7386 | −0.00357 0.01151 | −0.00018 0.01632 | −0.00761 0.01583 | −0.00385 0.04129 | 0.005047 0.05501 | −0.02006 0.05928 | −0.2450 1.0179 | 0.7166 1.5139 | −1.4923 1.3510 | 0.000894 0.06484 | 0.08904 0.09242 | −0.06589 0.08965 | −0.00519 0.07099 | 0.1151 0.09868 | −0.1035 0.1005 |
| p-value | 0.9960 | 0.4388 | 0.4149 | 0.5818 | 0.2225 | 0.5783 | 0.8814 | 0.9479 | 0.9158 | 0.7563 | 0.9914 | 0.6311 | 0.9258 | 0.9270 | 0.7351 | 0.8099 | 0.6362 | 0.2699 | 0.9890 | 0.3360 | 0.4628 | 0.9417 | 0.2442 | 0.3036 | |
| Quartile 3 Median = 5 | β SE | −0.2745 0.7210 | 0.02010 0.9054 | −0.6808 1.1045 | 0.2544 0.6813 | 2.1387 1.0115 | −1.7062 0.8957 | −0.2516 0.5025 | 0.4121 0.7494 | −0.9031 0.6661 | −0.01308 0.009827 | −0.01314 0.01400 | −0.01469 0.01345 | −0.06952 0.03794 | −0.03186 0.05027 | −0.1064 0.05467 | −0.2306 0.9057 | 1.2595 1.3255 | −1.8469 1.2221 | −0.03687 0.05918 | 0.06432 0.08509 | −0.1130 0.08125 | −0.05262 0.06449 | 0.06291 0.09156 | −0.1444 0.08958 |
| p-value | 0.7035 | 0.9823 | 0.5379 | 0.7089 | 0.0349 | 0.0572 | 0.6167 | 0.5826 | 0.1756 | 0.1834 | 0.3482 | 0.2756 | 0.0672 | 0.5266 | 0.0522 | 0.7991 | 0.3425 | 0.1314 | 0.5334 | 0.4502 | 0.1649 | 0.4148 | 0.4924 | 0.1077 | |
| Quartile 4 Median = 6 | β SE | −2.2631 0.9080 | −1.6717 1.1817 | −3.0287 1.3487 | 0.1265 0.8487 | 0.4668 1.2956 | −0.2324 1.0866 | 0.1132 0.6229 | −0.5120 0.9521 | 0.7676 0.8072 | −0.00235 0.01160 | −0.01952 0.01708 | 0.01022 0.01546 | −0.1193 0.04854 | −0.08361 0.06650 | −0.1565 0.06809 | 4.0263 1.1043 | 4.9457 1.6492 | 2.8388 1.4559 | −0.1290 0.07998 | 0.02699 0.1122 | −0.2499 0.1114 | −0.1118 0.08538 | −0.01289 0.1232 | −0.1937 0.1163 |
| p-value | 0.0128 | 0.1578 | 0.0251 | 0.8815 | 0.7187 | 0.8307 | 0.8558 | 0.5910 | 0.3420 | 0.8397 | 0.2536 | 0.5089 | 0.0141 | 0.2093 | 0.0220 | 0.0003 * | 0.0028 * | 0.0518 | 0.1073 | 0.8100 | 0.0254 | 0.1906 | 0.9167 | 0.0965 | |
| Linear | β SE | −0.3730 0.1952 | −0.2823 0.2557 | −0.4632 0.2881 | 0.02046 0.1813 | 0.3241 0.2771 | −0.2624 0.2326 | −0.01863 0.1329 | 0.008106 0.2023 | −0.02874 0.1732 | −0.00207 0.002493 | −0.00511 0.003611 | 0.000150 0.003373 | −0.02878 0.01019 | −0.01741 0.01398 | −0.03914 0.01431 | 0.6025 0.2403 | 0.8655 0.3553 | 0.3395 0.3192 | −0.02406 0.01609 | 0.006684 0.02284 | −0.04782 0.02216 | −0.02430 0.01743 | −0.00129 0.02443 | −0.04287 0.02429 |
| p-value | 0.0563 | 0.2700 | 0.1085 | 0.9101 | 0.2426 | 0.2597 | 0.8885 | 0.9681 | 0.8682 | 0.4075 | 0.1574 | 0.9645 | 0.0048 * | 0.2137 | 0.0064 | 0.0123 | 0.0152 | 0.2881 | 0.1353 | 0.7700 | 0.0315 | 0.1635 | 0.9579 | 0.0783 | |
| Adjusted model 3,4,5 | |||||||||||||||||||||||||
| Quartile 1 Median = 2 | (Ref) | (Ref) | (Ref) | (Ref) | (Ref) | (Ref) | (Ref) | (Ref) | (Ref) | (Ref) | (Ref) | (Ref) | (Ref) | (Ref) | (Ref) | (Ref) | (Ref) | (Ref) | (Ref) | (Ref) | (Ref) | (Ref) | (Ref) | (Ref) | |
| Quartile 2 Median = 3 | β SE | −0.1404 0.2602 | 0.03642 0.3208 | −0.3207 0.4021 | 0.5814 0.7470 | 1.4833 1.1171 | −0.3454 0.9877 | −0.05008 0.5595 | 0.02250 0.8350 | −0.05735 0.7394 | −0.00098 0.01132 | 0.001653 0.01611 | −0.00258 0.01568 | −0.01424 0.04090 | −0.00912 0.05498 | −0.03828 0.05885 | 0.1217 0.8142 | 1.7105 1.1721 | −1.4624 1.0979 | −0.01011 0.06014 | 0.1039 0.08814 | −0.05645 0.08246 | −0.01370 0.06598 | 0.1340 0.09244 | −0.09206 0.09332 |
| p-value | 0.5896 | 0.9097 | 0.4256 | 0.4366 | 0.1848 | 0.7267 | 0.9287 | 0.9785 | 0.9382 | 0.9310 | 0.9183 | 0.8691 | 0.7277 | 0.8684 | 0.5157 | 0.8812 | 0.1453 | 0.1836 | 0.8666 | 0.2392 | 0.4941 | 0.8356 | 0.1482 | 0.3245 | |
| Quartile 3 Median = 5 | β SE | −0.3892 0.2458 | −0.4985 0.3045 | −0.3532 0.3777 | 0.4154 0.6912 | 2.3554 1.0291 | −1.4118 0.9170 | −0.2620 0.5134 | 0.4335 0.7584 | −0.8423 0.6846 | −0.00785 0.01002 | −0.00725 0.01441 | −0.00760 0.01375 | −0.08973 0.03858 | −0.05247 0.05128 | −0.1248 0.05545 | −0.00216 0.7566 | 2.2068 1.0793 | −2.2225 1.0264 | −0.03920 0.05608 | 0.04363 0.08402 | −0.09581 0.07563 | −0.05244 0.06160 | 0.04249 0.08899 | −0.1275 0.08504 |
| p-value | 0.1136 | 0.1023 | 0.3501 | 0.5479 | 0.0224 | 0.1242 | 0.6099 | 0.5678 | 0.2190 | 0.4331 | 0.6151 | 0.5805 | 0.0203 | 0.3069 | 0.0249 | 0.8812 | 0.0415 | 0.0309 | 0.4847 | 0.6039 | 0.2060 | 0.3948 | 0.6333 | 0.1345 | |
| Quartile 4 Median = 6 | β SE | 0.1856 0.3214 | −0.3103 0.4056 | 0.4716 0.4887 | 0.4930 0.8973 | 1.2086 1.3530 | 0.06617 1.1824 | 0.2122 0.6643 | −0.1003 0.9897 | 0.7708 0.8820 | 0.007172 0.01254 | −0.01295 0.01842 | 0.02358 0.01711 | −0.1316 0.05127 | −0.09615 0.06949 | −0.1723 0.07298 | 1.8205 0.9718 | 4.1344 1.4027 | −0.3810 1.3088 | −0.06270 0.07777 | 0.03936 0.1130 | −0.1385 0.1071 | −0.03106 0.08427 | 0.009474 0.1220 | −0.06554 0.1154 |
| p-value | 0.5638 | 0.4446 | 0.3350 | 0.5828 | 0.3721 | 0.9554 | 0.7495 | 0.9193 | 0.3825 | 0.5674 | 0.4825 | 0.1688 | 0.0104 | 0.1672 | 0.0186 | 0.0614 | 0.0034 * | 0.7711 | 0.4204 | 0.7279 | 0.1966 | 0.7126 | 0.9381 | 0.5703 | |
| Linear | β SE | −0.03578 0.06906 | −0.1396 0.08783 | 0.03408 0.1043 | 0.08428 0.1912 | 0.4670 0.2898 | −0.2201 0.2515 | −0.01518 0.1414 | 0.06694 0.2103 | −0.04865 0.1880 | −0.00025 0.002693 | −0.00331 0.003920 | 0.002248 0.003706 | −0.03302 0.01077 | −0.02147 0.01470 | −0.04273 0.01533 | 0.2389 0.2097 | 0.8033 0.3041 | −0.2907 0.2818 | −0.01457 0.01600 | 0.003412 0.02338 | −0.03102 0.02186 | −0.01332 0.01759 | −0.00353 0.02468 | −0.02637 0.02466 |
| p-value | 0.6045 | 0.1127 | 0.7440 | 0.6594 | 0.1076 | 0.3818 | 0.9145 | 0.7504 | 0.7959 | 0.9251 | 0.3995 | 0.5444 | 0.0022 * | 0.1449 | 0.0055 | 0.2548 | 0.0085 | 0.3027 | 0.3628 | 0.8840 | 0.1567 | 0.4491 | 0.8864 | 0.2856 | |
| C-DII Score 1 | Waist Circumference (cm) | Systolic Blood Pressure (mmHg) | Diastolic Blood Pressure (mmHg) | Log Glucose (mg/dL) | Log TG (mg/dL) | HDL-C (mg/dL) | Log Insulin (μIU/mL) | Log HOMA-IR | |||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| All N = 574 | Boys N = 274 | Girls N = 300 | All N = 574 | Boys N = 274 | Girls N = 300 | All N = 574 | Boys N = 274 | Girls N = 300 | All N = 435 | Boys N = 213 | Girls N = 222 | All N = 435 | Boys N = 213 | Girls N = 222 | All N = 435 | Boys N = 213 | Girls N = 222 | All N = 410 | Boys N = 202 | Girls N = 208 | All N = 410 | Boys N = 202 | Girls N = 208 | ||
| # obs. = 1297 | # obs. = 621 | # obs. = 676 | # obs. = 1296 | # obs. = 621 | # obs. = 675 | # obs. = 1296 | # obs. = 621 | # obs. = 675 | # obs. = 1012 | # obs. = 495 | # obs. = 517 | # obs. = 1012 | # obs. = 495 | # obs. = 517 | # obs. = 1012 | # obs. = 495 | # obs. = 517 | # obs. = 840 | # obs. = 402 | # obs. = 438 | # obs. = 840 | # obs. = 402 | # obs. = 438 | ||
| Crude model 2 | |||||||||||||||||||||||||
| Quartile 1 Median = −1.809 | (Ref) | (Ref) | (Ref) | (Ref) | (Ref) | (Ref) | (Ref) | (Ref) | (Ref) | (Ref) | (Ref) | (Ref) | (Ref) | (Ref) | (Ref) | (Ref) | (Ref) | (Ref) | (Ref) | (Ref) | (Ref) | (Ref) | (Ref) | (Ref) | |
| Quartile 2 Median = −0.630 | β SE | −1.7767 0.7480 | −1.5876 0.9488 | −1.6627 1.1287 | −0.8237 0.7132 | −0.8569 1.0841 | −1.0464 0.9262 | −0.8375 0.5289 | −1.2088 0.8073 | −0.5412 0.6915 | 0.01185 0.01037 | 0.01802 0.01502 | 0.006933 0.01401 | 0.02667 0.04125 | 0.05751 0.05467 | 0.01242 0.05944 | 1.2633 0.9442 | 1.4994 1.4080 | 1.1387 1.2547 | −0.01112 0.06234 | 0.02392 0.08838 | −0.03165 0.08618 | −0.00900 0.06819 | 0.04720 0.09667 | −0.04518 0.09444 |
| p-value | 0.0177 | 0.0950 | 0.1413 | 0.2484 | 0.4296 | 0.2590 | 0.1136 | 0.1349 | 0.4341 | 0.2536 | 0.2306 | 0.6209 | 0.5181 | 0.2935 | 0.8346 | 0.1812 | 0.2875 | 0.3646 | 0.8585 | 0.7868 | 0.7137 | 0.8951 | 0.6256 | 0.6326 | |
| Quartile 3 Median = 0.367 | β SE | −0.7154 0.7746 | 0.9719 0.9874 | −2.3282 1.1678 | −0.01267 0.7302 | 0.8179 1.1069 | −1.0997 0.9509 | −0.3229 0.5389 | 0.006068 0.8185 | −0.7512 0.7087 | 0.01915 0.01040 | 0.03382 0.01487 | 0.003251 0.01429 | 0.06592 0.04183 | 0.05300 0.05595 | 0.09213 0.05973 | 0.3462 0.9700 | 0.1860 1.4195 | 0.5931 1.3192 | 0.02611 0.06237 | 0.1313 0.08391 | −0.06484 0.09243 | 0.03706 0.06781 | 0.1720 0.09130 | −0.07919 0.1010 |
| p-value | 0.3559 | 0.3255 | 0.0467 | 0.9862 | 0.4603 | 0.2479 | 0.5492 | 0.9941 | 0.2895 | 0.0660 | 0.0234 | 0.8201 | 0.1154 | 0.3441 | 0.1236 | 0.7212 | 0.8958 | 0.6532 | 0.6756 | 0.1184 | 0.4834 | 0.5849 | 0.0604 * | 0.4336 | |
| Quartile 4 Median = 1.627 | β SE | −0.4730 0.8139 | 0.5592 1.0580 | −1.3017 1.2065 | 0.3410 0.7557 | 1.0353 1.1543 | −0.5672 0.9737 | −0.1045 0.5543 | 0.06080 0.8452 | −0.3924 0.7246 | 0.009471 0.01064 | 0.02123 0.01554 | −0.00136 0.01427 | 0.09871 0.04350 | 0.1510 0.05866 | 0.05567 0.06214 | 0.4201 1.0196 | 0.8044 1.5123 | 0.4001 1.3566 | −0.04730 0.06760 | −0.07156 0.09781 | −0.01034 0.09126 | −0.05217 0.07365 | −0.04971 0.1064 | −0.03442 0.09976 |
| p-value | 0.5613 | 0.5974 | 0.2811 | 0.6519 | 0.3701 | 0.5604 | 0.8505 | 0.9427 | 0.5883 | 0.3734 | 0.1725 | 0.9239 | 0.0235 | 0.0104 | 0.3708 | 0.6804 | 0.5950 | 0.7682 | 0.4844 | 0.4648 | 0.9099 | 0.4789 | 0.6405 | 0.7302 | |
| Linear | β SE | −0.02710 0.2294 | 0.3636 0.3003 | −0.4014 0.3386 | 0.1637 0.2122 | 0.4279 0.3244 | −0.1571 0.2728 | 0.01930 0.1556 | 0.1336 0.2373 | −0.1228 0.2030 | 0.003109 0.002951 | 0.006803 0.004292 | −0.00061 0.003976 | 0.02965 0.01220 | 0.04082 0.01655 | 0.02089 0.01724 | 0.03564 0.2862 | 0.09435 0.4231 | 0.06718 0.3815 | −0.00938 0.01870 | −0.00948 0.02598 | −0.00578 0.02622 | −0.00984 0.02027 | −0.00293 0.02794 | −0.01262 0.02865 |
| p-value | 0.9060 | 0.2266 | 0.2363 | 0.4406 | 0.1876 | 0.5650 | 0.9013 | 0.5736 | 0.5452 | 0.2923 | 0.1137 | 0.8789 | 0.0152 | 0.0141 | 0.2263 | 0.9009 | 0.8236 | 0.8603 | 0.6162 | 0.7154 | 0.8258 | 0.6273 | 0.9166 | 0.6598 | |
| Adjusted model 3,4,5 | |||||||||||||||||||||||||
| Quartile 1 Median = −1.809 | (Ref) | (Ref) | (Ref) | (Ref) | (Ref) | (Ref) | (Ref) | (Ref) | (Ref) | (Ref) | (Ref) | (Ref) | (Ref) | (Ref) | (Ref) | (Ref) | (Ref) | (Ref) | (Ref) | (Ref) | (Ref) | (Ref) | (Ref) | (Ref) | |
| Quartile 2 Median = −0.630 | β SE | −0.1622 0.2481 | −0.4641 0.3073 | 0.1158 0.3783 | −0.9515 0.7032 | −0.9685 1.0724 | −0.9390 0.9205 | −0.8455 0.5245 | −1.2116 0.7953 | −0.4926 0.6885 | 0.01326 0.01025 | 0.02101 0.01484 | 0.01012 0.01392 | 0.02897 0.04094 | 0.06968 0.05402 | 0.003959 0.05863 | 0.7208 0.7511 | 0.5212 1.0902 | 0.8175 1.0117 | −0.00072 0.05866 | 0.04457 0.08694 | −0.02456 0.07993 | −0.00165 0.06456 | 0.08241 0.09388 | −0.04292 0.08926 |
| p-value | 0.5133 | 0.1317 | 0.7597 | 0.1763 | 0.3669 | 0.3081 | 0.1072 | 0.1282 | 0.4746 | 0.1958 | 0.1575 | 0.4678 | 0.4794 | 0.1978 | 0.9462 | 0.3376 | 0.6329 | 0.4196 | 0.9902 | 0.6086 | 0.7588 | 0.9797 | 0.3807 | 0.6309 | |
| Quartile 3 Median = 0.367 | β SE | −0.05138 0.2572 | 0.1094 0.3210 | −0.2653 0.3921 | −0.4100 0.7205 | 0.3755 1.0970 | −1.2512 0.9455 | −0.5400 0.5348 | −0.2713 0.8052 | −0.8539 0.7058 | 0.01760 0.01033 | 0.03426 0.01475 | 0.003487 0.01428 | 0.07035 0.04149 | 0.05348 0.05512 | 0.07973 0.05913 | −0.2508 0.7793 | −0.2023 1.1102 | −0.02910 1.0755 | 0.03325 0.05918 | 0.1630 0.08286 | −0.07402 0.08592 | 0.03778 0.06475 | 0.2121 0.08928 | −0.09819 0.09589 |
| p-value | 0.8417 | 0.7333 | 0.4990 | 0.5694 | 0.7322 | 0.1862 | 0.3128 | 0.7363 | 0.2268 | 0.0886 | 0.0206 | 0.8072 | 0.0903 | 0.3325 | 0.1781 | 0.7477 | 0.8555 | 0.9784 | 0.5744 | 0.0499 | 0.3895 | 0.5598 | 0.0180 | 0.3065 | |
| Quartile 4 Median = 1.627 | β SE | −0.06379 0.2710 | 0.2387 0.3430 | −0.3789 0.4077 | −0.1990 0.7460 | 0.4404 1.1387 | −0.9106 0.9770 | −0.4396 0.5500 | −0.3937 0.8245 | −0.6105 0.7282 | 0.007480 0.01061 | 0.02143 0.01547 | −0.00365 0.01452 | 0.09054 0.04314 | 0.1463 0.05779 | 0.03924 0.06192 | 0.5218 0.8310 | 0.6096 1.2068 | 0.7541 1.1187 | −0.04283 0.06388 | −0.03861 0.09624 | −0.04039 0.08593 | −0.05409 0.06986 | −0.00900 0.1034 | −0.06534 0.09521 |
| p-value | 0.8139 | 0.4868 | 0.3531 | 0.7897 | 0.6990 | 0.3517 | 0.4243 | 0.6332 | 0.4021 | 0.4811 | 0.1665 | 0.8015 | 0.0361 | 0.0117 | 0.5265 | 0.5302 | 0.6137 | 0.5006 | 0.5028 | 0.6885 | 0.6386 | 0.4389 | 0.9307 | 0.4929 | |
| Linear | β SE | −0.00700 0.07627 | 0.1167 0.09747 | −0.1327 0.1143 | −0.00199 0.2097 | 0.2405 0.3203 | −0.2696 0.2738 | −0.08756 0.1545 | −0.01362 0.2313 | −0.1931 0.2041 | 0.002315 0.002950 | 0.006580 0.004281 | −0.00142 0.004051 | 0.02739 0.01206 | 0.03837 0.01626 | 0.01612 0.01723 | 0.05919 0.2340 | 0.1014 0.3391 | 0.1344 0.3152 | −0.00876 0.01766 | −0.00146 0.02556 | −0.01473 0.02453 | −0.01133 0.01925 | 0.005503 0.02711 | −0.02213 0.02726 |
| p-value | 0.9269 | 0.2319 | 0.2461 | 0.9924 | 0.4531 | 0.3253 | 0.5711 | 0.9531 | 0.3444 | 0.4327 | 0.1250 | 0.7259 | 0.0233 | 0.0187 | 0.3498 | 0.8003 | 0.7651 | 0.6700 | 0.6199 | 0.9546 | 0.5483 | 0.5563 | 0.8393 | 0.4174 | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Aljahdali, A.A.; Peterson, K.E.; Cantoral, A.; Ruiz-Narvaez, E.; Tellez-Rojo, M.M.; Kim, H.M.; Hébert, J.R.; Wirth, M.D.; Torres-Olascoaga, L.A.; Shivappa, N.; et al. Diet Quality Scores and Cardiometabolic Risk Factors in Mexican Children and Adolescents: A Longitudinal Analysis. Nutrients 2022, 14, 896. https://doi.org/10.3390/nu14040896
Aljahdali AA, Peterson KE, Cantoral A, Ruiz-Narvaez E, Tellez-Rojo MM, Kim HM, Hébert JR, Wirth MD, Torres-Olascoaga LA, Shivappa N, et al. Diet Quality Scores and Cardiometabolic Risk Factors in Mexican Children and Adolescents: A Longitudinal Analysis. Nutrients. 2022; 14(4):896. https://doi.org/10.3390/nu14040896
Chicago/Turabian StyleAljahdali, Abeer Ali, Karen E. Peterson, Alejandra Cantoral, Edward Ruiz-Narvaez, Martha M. Tellez-Rojo, Hyungjin Myra Kim, James R. Hébert, Michael D. Wirth, Libni A. Torres-Olascoaga, Nitin Shivappa, and et al. 2022. "Diet Quality Scores and Cardiometabolic Risk Factors in Mexican Children and Adolescents: A Longitudinal Analysis" Nutrients 14, no. 4: 896. https://doi.org/10.3390/nu14040896
APA StyleAljahdali, A. A., Peterson, K. E., Cantoral, A., Ruiz-Narvaez, E., Tellez-Rojo, M. M., Kim, H. M., Hébert, J. R., Wirth, M. D., Torres-Olascoaga, L. A., Shivappa, N., & Baylin, A. (2022). Diet Quality Scores and Cardiometabolic Risk Factors in Mexican Children and Adolescents: A Longitudinal Analysis. Nutrients, 14(4), 896. https://doi.org/10.3390/nu14040896









