Differentiation of Nutritional Risk among Polish Seniors Based on Selected Lifestyle Characteristics
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Sample
2.2. Questionnaire
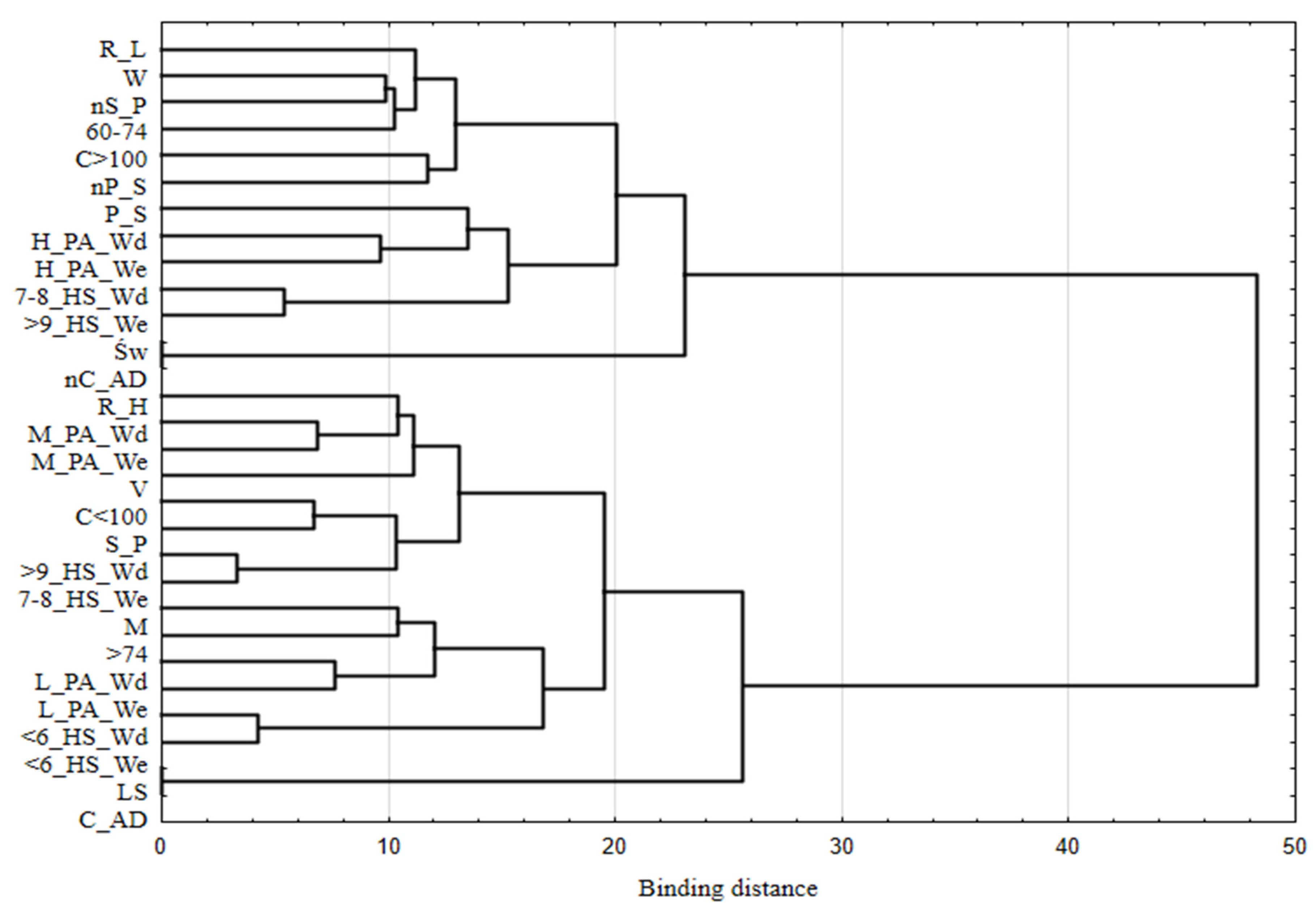
2.3. Statistical Analysis
3. Results
3.1. Characteristics of the Study Sample
3.2. Nutritional Risk
4. Discussion
Strengths and Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Sharkey, J.R.; Schoenberg, N.E. Variations in nutritional risk among black and white women who receive home-delivered meals. J. Women Aging 2002, 14, 99–119. [Google Scholar] [CrossRef] [PubMed]
- Margetts, B.M.; Thompson, R.L.; Elia, M.; Jackson, A.A. Prevalence of risk of undernutrition is associated with poor health status in older people in the UK. Eur. J. Clin. Nutr. 2003, 57, 69–74. [Google Scholar] [CrossRef] [PubMed]
- Morrison, J.M.; Laur, C.V.; Keller, H.H. SCREEN III: Working towards a condensed screening tool to detect nutrition risk in community-dwelling older adults using CLSA date. Europ. J. Clin. Nutr. 2019, 73, 1260–1269. [Google Scholar] [CrossRef] [PubMed]
- Sharkey, J.R. Nutrition risk screening: The interrelationship of food insecurity, food intake, and unintentional weight change among homebound elders. J. Nutr. Elder 2004, 24, 19–34. [Google Scholar] [CrossRef]
- Cederholm, T.; Jensen, G.L. To create a consensus on malnutrition diagnostic criteria: A report from the Global Leadership Initiative on Malnutrition (GLIM) meeting at the ESPEN Congress. Clin. Nutr. 2016, 36, 7–10. [Google Scholar] [CrossRef]
- Older Adult Nutrition Screening. Available online: https://olderadultnutritionscreening.com (accessed on 3 August 2021).
- Eckert, C.; Gell, N.M.; Wingood, M.; Schollmeyer, J.; Tarleton, E.K. Malnutrition risk, rurality, and falls among community dwelling older adults. J. Nutr. Health Aging 2021, 25, 624–627. [Google Scholar] [CrossRef]
- Keller, H.H.; Goy, R.; Kane, S.L. Validity and reliability of SCREEN II (Seniors in the community: Risk evaluation for eating and nutrition, Version II). Eur. J. Clin. Nutr. 2005, 59, 1149–1157. [Google Scholar] [CrossRef]
- Keller, H.H.; Østbye, T.; Goy, R. Nutritional risk predicts quality of life in elderly community-living Canadians. J. Gerontol. A Biol. Sci. Med. Sci. 2004, 59, 68–74. [Google Scholar] [CrossRef]
- Keller, H.H.; Hedley, M.R.; Wong Brownlee, S. The development of Seniors in the Community: Risk Evaluation for Eating and Nutrition (SCREEN). Can. J. Diet. Pract. Res. 2000, 61, 67–72. [Google Scholar]
- Keller, H.H.; McKenzie, J.D.; Goy, R.E. Construct validation and testretest reliability of the Seniors in the Community: Risk Evaluation for Eating and Nutrition questionnaire. J. Gerontol. A Biol. Sci. Med. Sci. 2001, 56, M552–M558. [Google Scholar] [CrossRef]
- Ramage-Morin, P.L.; Gilmour, H.; Rotermann, M. Nutritional risk, hospitalization and mortality among community-dwelling Canadians aged 65 or older. Health Rep. 2017, 28, 17–27. [Google Scholar] [PubMed]
- Power, L.; Mullally, D.; Gibney, E.R.; Clarke, M.; Visser, M.; Volkert, D. A review of the validity of malnutrition screening tools used in older adults in community and healthcare settings—A MaNuEL study. Clin. Nutr. Espen 2018, 24, 1–13. [Google Scholar] [CrossRef] [PubMed]
- Bernstein, M.; Munoz, N. Position of the Academy of Nutrition and Dietetics: Food and nutrition for older adults: Promoting health and wellness. J. Acad. Nutr. Diet. 2012, 112, 1255–1277. [Google Scholar] [CrossRef] [PubMed]
- Ahmed, T.; Haboubi, N. Assessment and management of nutrition in older people and its importance to health. Clin. Interv. Aging 2010, 5, 207–216. [Google Scholar]
- Keller, H.H.; Østbye, T. Nutritional risk and time to death: Predictive validity of SCREEN (Seniors in the Community Risk Evaluation for Eating and Nutrition). J. Nutr. Health Aging 2003, 7, 274–279. [Google Scholar]
- Hays, J.C.; Keller, H.H.; Østbye, T. The effects of nutrition-related factors on four-year mortality among a biracial sample of community-dwelling elders in the North Carolina piedmont. J. Nutr. Elder 2005, 25, 41–67. [Google Scholar] [CrossRef]
- Krzymińska-Siemaszko, R.; Chudek, J.; Suwalska, A. Health status correlates on malnutrition in the Polish elderly population—Results of the Polsenior study. Eur. Rev. Med. Pharmacol. Sci. 2016, 20, 4565–4573. [Google Scholar]
- Favaro-Moreira, N.C.; Krausch-Hofmann, S.; Matthys, C. Risk factors for malnutrition in older adults: A systematic review of the literature based on longitudinal data. Adv. Nutr. 2016, 7, 507–522. [Google Scholar] [CrossRef]
- OʼKeeffe, M.; Kelly, M.; OʼHerlihy, E. Potentially modifiable determinants of malnutrition in older adults: A systematic review. Clin. Nutr. 2019, 38, 2477–2498. [Google Scholar] [CrossRef]
- Ramage-Morin, P.L.; Garriguet, D. Nutritional risk among older Canadians. Health Rep. 2013, 24, 3–13. [Google Scholar]
- Donini, L.M.; Scardella, P.; Piombo, L.; Neri, B.; Asprino, R.; Proietti, A.R. Malnutrition in elderly: Social and economic determinants. J. Nutr. Health Aging 2013, 17, 9–15. [Google Scholar] [CrossRef] [PubMed]
- Borkent, J.W.; Keller, H.; Wham, C.; Wijers, F.; de van der Schueren, M.A.E. Cross-country differences and similarities in undernutrition prevalence and risk as measured by SCREEN II in community-dwelling older adults. Healthcare 2020, 8, 151. [Google Scholar] [CrossRef] [PubMed]
- Volkert, D. Nutrition and lifestyle of the elderly in Europe. J. Public Health 2005, 13, 56–61. [Google Scholar] [CrossRef]
- World Medical Association Declaration of Helsinki: Ethical principles for medical research involving human subjects. JAMA J. Am. Med. Assoc. 2013, 310, 2191–2194. [CrossRef]
- Stanisz, A. Przystępny Kurs Statystyki z Zastosowaniem STATISTICA PL na Przykładach z Medycyny. Tom 2. Modele Liniowe i Nieliniowe; StatSoft Polska: Kraków, Poland, 2007; ISBN 978-83-88724-30-5. (In Polish) [Google Scholar]
- StatSoft Poland. Statistica 13.1. Available online: https://www.statsoft.pl/statistica_13/ (accessed on 3 August 2021).
- Lee, K.S.; Cheong, H.K.; Kim, E.A.; Kim, K.R.; Oh, B.H.; Hong, C.H. Nutritional risk and cognitive impairment in the elderly. Arch. Gerontol. Geriatr. 2009, 48, 95–99. [Google Scholar] [CrossRef]
- Felder, S.; Lechtenboehmer, C.; Bally, M.; Fehr, R.; Deiss, M.; Faessler, L.; Kutz, A.; Steiner, D.; Rast, A.C.; Laukemann, S.; et al. Association of nutritional risk and adverse medical outcomes across different medical inpatient populations. Nutrition 2015, 31, 1385–1393. [Google Scholar] [CrossRef] [PubMed]
- Kanda, E.; Kato, A.; Masakane, I.; Kanno, Y.A. New nutritional risk index for predicting mortality in hemodialysis patients: Nationwide cohort study. PLoS ONE 2019, 14, e0214524. [Google Scholar] [CrossRef] [PubMed]
- Roberts, K.C.; Wolfson, C.; Payette, H. Predictors of nutritional risk in community-dwelling seniors. Can. J. Public Health 2007, 98, 331–336. [Google Scholar] [CrossRef] [PubMed]
- Porter Starr, K.N.; McDonald, S.R.; Bales, C.W. Nutritional vulnerability in older adults: A continuum of concerns. Curr. Nutr. Rep. 2015, 4, 176–184. [Google Scholar] [CrossRef]
- Leslie, W.; Hankey, C. Aging, nutritional status and health. Healthcare 2015, 3, 648–658. [Google Scholar] [CrossRef]
- De Morais, C.; Oliveira, B.; Afonso, C.; Lumbers, M.; Raats, M.; de Almeida, M.D.V. Nutritional risk of European elderly. Eu. J. Clin. Nutr. 2013, 67, 1215–1219. [Google Scholar] [CrossRef] [PubMed]
- Locher, J.L.; Ritchie, C.S.; Roth, D.L. Social isolation, support, and capital and nutritional risk in an older sample: Ethnic and gender differences. Soc. Sci. Med. 2005, 60, 747–761. [Google Scholar] [CrossRef] [PubMed]
- Locher, J.L.; Robinson, C.O.; Roth, D.L. The effect of the presence of others on caloric intake in homebound older adults. J. Gerontol. A Biol. Sci. Med. Sci. 2005, 60, 1475–1478. [Google Scholar] [CrossRef] [PubMed]
- Wham, C.; Teh, R.; Robinson, M.; Kerse, N. What is associated with nutrition risk in very old age? J. Nutr. Health Aging 2011, 15, 247–251. [Google Scholar] [CrossRef] [PubMed]
- Tkatch, M.T.; Towers, A.J.; Keller, H.H.; Wham, C.A. Nutrition risk prevalence and associated health and social risk factors in Māori and non- Māori: Results from the New Zealand Health, Work and Retirement Study. Australas. J. on Ageing 2021, 1–11. [Google Scholar] [CrossRef]
- De Castro, J. Age-related changes in the social, psychological, and temporal influences on food intake in free-living, healthy, adult humans. J. Gerontol A Biol. Sci. Med. Sci. 2002, 57A, M368–M377. [Google Scholar] [CrossRef]
- Crichton, M.; Craven, D.; Mackay, H.; Marx, W.; de van der Schueren, M.; Marshall, S. A systematic review, meta-analysis and meta-regression of the prevalence of protein-energy malnutrition: Associations with geographical region and sex. Age Ageing 2018, 48, 38–48. [Google Scholar] [CrossRef]
- Marshall, S.; Young, A.; Bauer, J.; Isenring, E. Malnourished older adults admitted to rehabilitation in rural New South Wales remain malnourished throughout rehabilitation and once discharged back to the community: A prospective cohort study. J. Aging Res. Clin. Pract. 2015, 4, 197–204. [Google Scholar] [CrossRef]
- Australian Government Response: Productivity Commission’s Caring for Older Australians Report; Australian Government Department of Health and Ageing: Canberra, Australia, 2012.
- Damayanthi, H.D.W.T.; Moy, F.M.; Abdullah, K.L.; Dharmaratne, S.D. Prevalence of malnutrition and associated factors among community-dwelling older persons in Sri Lanka: A cross-sectional study. BMC Geriatrics 2018, 18, 199. [Google Scholar] [CrossRef]
- Mathew, A.; Das, D.; Sampath, S.; Vijayakumar, M.; Ramakrishnan, N.; Ravishankar, S.L. Prevalence and correlates of malnutrition among elderly in an urban area in Coimbatore. IJPH 2016, 60, 112–117. [Google Scholar] [CrossRef]
- Al-Zeidaneen, S.; Al-Bayyari, N.; Ismali, Y. Effect of physical activity and gender on malnutrition risk among a group of elderly Jordanians. Pak. J. Nutr. 2017, 16, 9. [Google Scholar] [CrossRef][Green Version]
- Enriquez-Reyna, M.C.; Bautista, D.C.; Orcio, R.N. Physical activity level, muscle mass and strength of community elderly women: Differences by age group. Retos 2019, 35, 121–125. [Google Scholar] [CrossRef]
- Jyvakorpi, S.K.; Urtamo, A.; Kivimaki, M.; Stranberg, T.E. Associations of sleep quality, quantity and nutrition in oldest-old men: The Helsinki Businessmen Study (HBS). Eur. Geriatr. Med. 2021, 12, 117–122. [Google Scholar] [CrossRef] [PubMed]
- Kushkestani, M.; Parvani, M. Malnutrition is associated with cognitive function, tiredness and sleep quality in elderly living nursing home. J. Aging Sci. 2020, 8, 2. [Google Scholar] [CrossRef]
| Part of the Questionnaire | Survey Questions |
|---|---|
| The SCREEN-14 questionnaire | Has your weight changed in the past 6 months? Have you been trying to change your weight in the past 6 months? Do you think your weight is….? Do you skip meals? Do you limit or avoid certain foods? How would you describe your appetite? How many pieces or servings of vegetables and fruit do you eat in a day? How often do you eat meat, eggs, fish, cold cuts and legumes? How often do you have milk or milk products such as cheese, yogurt, or kefir? How much fluid do you drink in a day? Examples are water, tea, coffee, herbal drinks, juice, and soft drinks, but NOT alcohol Do you cough, choke or have pain when swallowing food or fluids? Is biting or chewing food difficult for you? Do you use commercial meal replacements or supplements? Examples are shakes, puddings, or energy bars. Do you eat one or more meals a day with someone? Who usually prepares your meals? Which statement best describes meal preparation for you? Do you have any problems getting your groceries? Problems can be poor health or disability, limited income, lack of transportation, weather conditions, or finding someone to shop. |
| Personal data | Gender Age Place of residence Region of residence What is the composition of your household? Do you consume alcoholic beverages? Do you currently smoke cigarettes, a pipe or other forms of tobacco? Have you smoked cigarettes, a pipe or other tobacco in the past? How many hours per night do you spend sleeping during the week, on average? How many hours per night do you spend sleeping at weekends, on average? How would you rate your physical activity doing everyday activities on weekdays? How would you rate your physical activity doing everyday activities on weekend days? |
| Variables | N = 320 | [%] |
|---|---|---|
| Gender | ||
| Female | 236 | 73.6 |
| Male | 84 | 26.4 |
| Age | ||
| 60–74 years | 236 | 73.6 |
| 75 years or older | 84 | 26.4 |
| Place of residence | ||
| Rural area | 92 | 28.8 |
| City < 100,000 residents | 25 | 7.8 |
| City > 100,000 residents | 203 | 63.4 |
| Region of residence | ||
| Świętokrzyskie voivodeship * | 181 | 56.6 |
| Silesia voivodeship | 139 | 43.4 |
| Variables | N = 320 | [%] |
|---|---|---|
| Consumption of alcoholic beverages | ||
| No | 181 | 56.6 |
| Yes | 139 | 43.4 |
| Currently a smoker | ||
| No | 296 | 92.5 |
| Yes | 24 | 7.5 |
| Previously a smoker | ||
| No | 183 | 57.2 |
| Yes | 137 | 42.8 |
| Number of hours of sleep on weeknights | ||
| 6 h or less | 104 | 32.5 |
| 7 or 8 h | 182 | 56.9 |
| 9 or more hours | 34 | 10.6 |
| Number of hours of sleep on weekend nights | ||
| 6 h or less | 88 | 27.5 |
| 7 or 8 h | 189 | 59.1 |
| 9 or more hours | 43 | 13.4 |
| Physical activity on weekdays | ||
| Low | 74 | 23.1 |
| Moderate | 173 | 54.1 |
| High | 73 | 22.8 |
| Physical activity on weekend days | ||
| Low | 126 | 39.4 |
| Moderate | 152 | 47.5 |
| High | 42 | 13.1 |
| Household composition | ||
| I live alone | 121 | 37.8 |
| I live with my partner | 124 | 38.8 |
| I live without a partner but with my family | 40 | 12.5 |
| I live with my partner and my family | 35 | 10.9 |
| Variables | Level of Nutritional Risk | p | |||
|---|---|---|---|---|---|
| High | Low | ||||
| N | % | N | % | ||
| Total | 238 | 74.4 | 82 | 25.5 | |
| Consumption of alcoholic beverages | |||||
| No | 125 | 52.5 | 56 | 68.3 | 1 |
| Yes | 113 | 47.5 | 26 | 31.7 | 0.047 |
| Currently a smoker | |||||
| No | 217 | 91.2 | 79 | 96.3 | 1 |
| Yes | 21 | 8.8 | 3 | 3.7 | 0.041 |
| Previously a smoker | |||||
| No | 130 | 54.6 | 53 | 64.6 | 1 |
| Yes | 108 | 45.4 | 29 | 35.4 | 0.963 |
| Number of hours of sleep on weeknights | |||||
| 6 h or less | 81 | 34 | 23 | 28 | 1 |
| 7 or 8 h | 131 | 55 | 51 | 62.2 | 0.998 |
| 9 h or more | 26 | 11 | 8 | 9.7 | <0.001 |
| Number of hours of sleep at weekends | |||||
| 6 h or less | 67 | 28.2 | 21 | 25.6 | 1 |
| 7 or 8 h | 141 | 59.2 | 48 | 58.5 | 0.996 |
| 9 h or more | 30 | 12.6 | 13 | 15.9 | <0.001 |
| Physical activity on weekdays | 1 | ||||
| Low | 62 | 26.1 | 13 | 15.9 | 0.986 |
| Moderate | 134 | 56.3 | 39 | 47.6 | |
| High | 42 | 17.6 | 31 | 36.5 | <0.001 |
| Physical activity at weekends | |||||
| Low | 105 | 44.1 | 21 | 25.6 | 1 |
| Moderate | 109 | 45.7 | 43 | 52.4 | 0.996 |
| High | 24 | 10.2 | 18 | 22 | <0.001 |
| Household composition | |||||
| I live alone | 96 | 40.3 | 25 | 30.5 | <0.001 |
| I live with my partner | 88 | 37.3 | 36 | 43.9 | <0.001 |
| I live without a partner but with my family | 29 | 12.3 | 11 | 13.4 | <0.001 |
| I live with my partner and my family | 25 | 10.1 | 10 | 12.2 | <0.001 |
| Variables | Level of Nutritional Risk | ||
|---|---|---|---|
| Low | High | ||
| OR b | p | ||
| Consumption of alcoholic beverages | |||
| No | Ref a | 1 | |
| Yes | 1.94 (1.14–3.12) | 0.014 | |
| Currently a smoker | |||
| No | Ref | 1 | |
| Yes | 2.54 (0.70–9.25) | 0.037 | |
| Previously a smoker | |||
| No | Ref | 1 | |
| Yes | 1.51 (0.90–2.56) | 0.115 | |
| Number of hours of sleep on weeknights | |||
| 6 h or less | Ref | 1 | |
| 7 or 8 h | 0.73 (0.41–1.29) | 0.273 | |
| 9 h or more | 0.96 (0.60–1.53) | 0.864 | |
| Number of hours of sleep at weekends | |||
| 6 h or less | Ref | 1 | |
| 7 or 8 h | 0.92 (0.51–1.66) | 0.783 | |
| 9 h or more | 0.85 (0.56–1.28) | 0.436 | |
| Physical activity on weekdays | |||
| Low | Ref | 1 | |
| Moderate | 0.67 (0.32–1.36) | 0.263 | |
| High | 0.51 (0.35–0.76) | <0.001 | |
| Physical activity at weekends | |||
| Low | Ref | 1 | |
| Moderate | 0.51 (0.28–0.91) | 0.023 | |
| High | 0.52 (0.35–0.76) | <0.001 | |
| Household composition | Ref | ||
| I live alone | 1 | ||
| I live with my partner | 0.44 (0.22–0.88) | <0.001 | |
| I live without a partner but with my family | 0.79 (0.44–1.30) | 0.044 | |
| I live with my partner and my family | 0.66 (0.30–1.42) | 0.021 | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gajda, R.; Raczkowska, E.; Mazurkiewicz, D.; Suliga, E. Differentiation of Nutritional Risk among Polish Seniors Based on Selected Lifestyle Characteristics. Nutrients 2022, 14, 607. https://doi.org/10.3390/nu14030607
Gajda R, Raczkowska E, Mazurkiewicz D, Suliga E. Differentiation of Nutritional Risk among Polish Seniors Based on Selected Lifestyle Characteristics. Nutrients. 2022; 14(3):607. https://doi.org/10.3390/nu14030607
Chicago/Turabian StyleGajda, Robert, Ewa Raczkowska, Dominika Mazurkiewicz, and Edyta Suliga. 2022. "Differentiation of Nutritional Risk among Polish Seniors Based on Selected Lifestyle Characteristics" Nutrients 14, no. 3: 607. https://doi.org/10.3390/nu14030607
APA StyleGajda, R., Raczkowska, E., Mazurkiewicz, D., & Suliga, E. (2022). Differentiation of Nutritional Risk among Polish Seniors Based on Selected Lifestyle Characteristics. Nutrients, 14(3), 607. https://doi.org/10.3390/nu14030607







