Dietary Fat Intake among Chinese Adults and Their Relationships with Blood Lipids: Findings from China Nutrition and Health Surveillance and Comparison with the PURE Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Population
2.2. Assessment of Dietary Fats
2.3. Assessment of Blood Lipids
2.4. Covariates Assessment
2.5. Statistical Analysis
3. Results
3.1. Dietary Fats Intake Profile
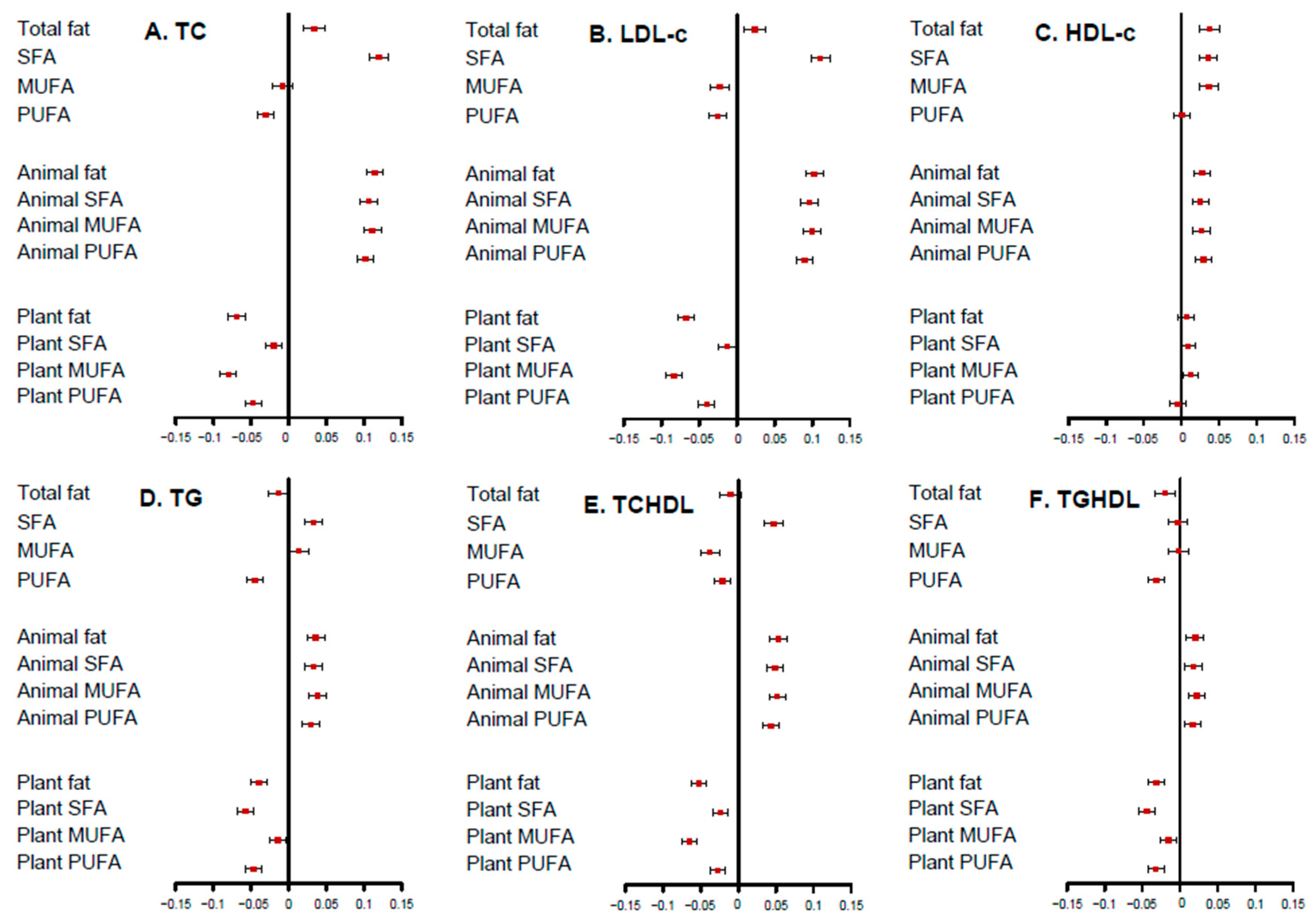
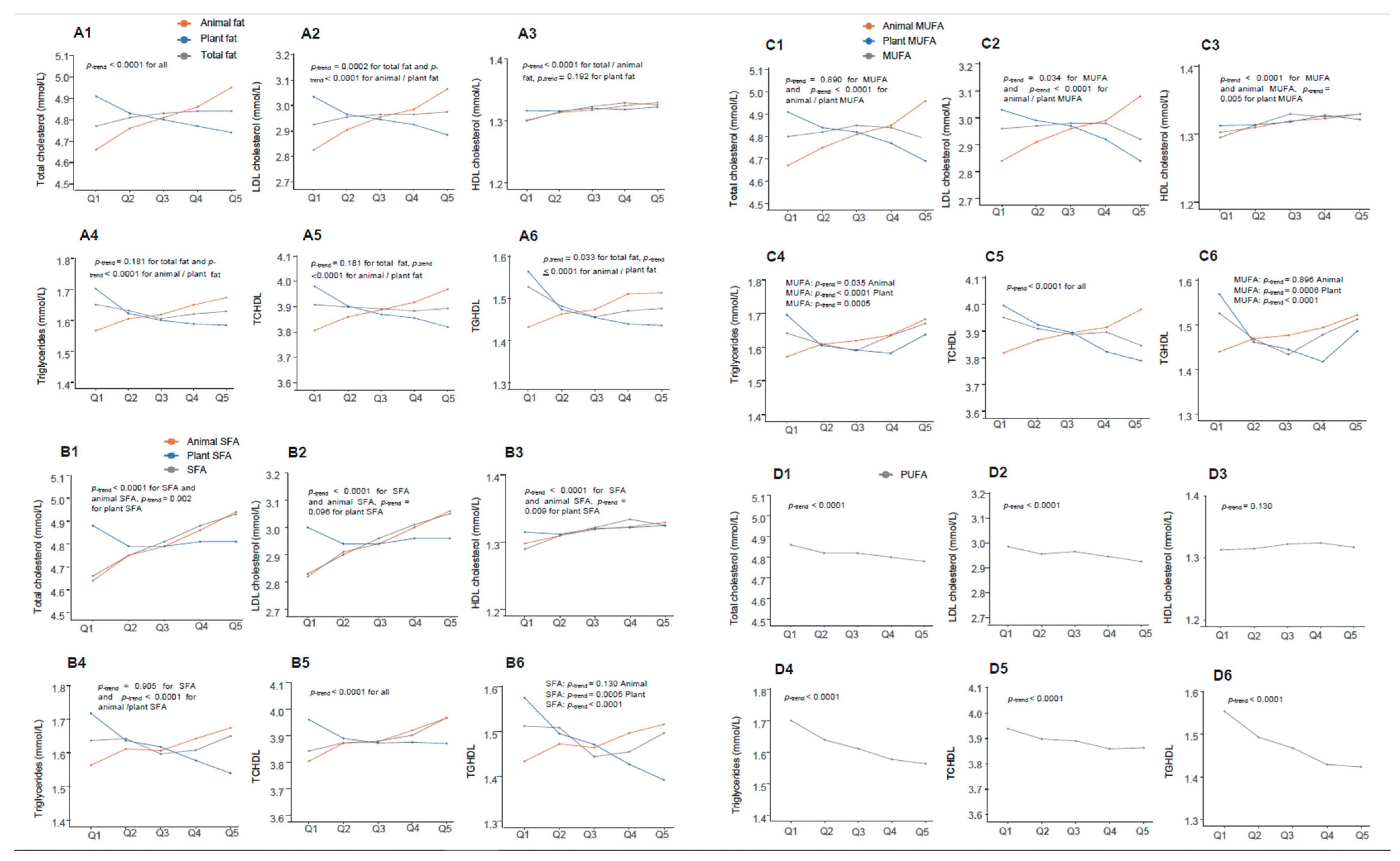
3.2. The Relationship of Dietary Fats and Blood Lipids
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- NCD Risk Factor Collaboration. Repositioning of the global epicentre of non-optimal cholesterol. Nature 2020, 582, 73–77. [Google Scholar] [CrossRef]
- Pirillo, A.; Casula, M.; Olmastroni, E.; Norata, G.D.; Catapano, A.L. Global epidemiology of dyslipidaemias. Nat. Rev. Cardiol. 2021, 18, 689–700. [Google Scholar] [CrossRef]
- Zhou, M.; Wang, H.; Zeng, X.; Yin, P.; Zhu, J.; Chen, W.; Li, X.; Wang, L.; Wang, L.; Liu, Y.; et al. Mortality, morbidity, and risk factors in China and its provinces, 1990–2017: A systematic analysis for the Global Burden of Disease Study 2017. Lancet 2019, 394, 1145–1158. [Google Scholar] [CrossRef]
- Catapano, A.L.; Graham, I.; De Backer, G.; Wiklund, O.; Chapman, M.J.; Drexel, H.; Hoes, A.W.; Jennings, C.S.; Landmesser, U.; Pedersen, T.R.; et al. 2016 ESC/EAS Guidelines for the Management of Dyslipidaemias. Eur. Heart J. 2016, 37, 2999–3058. [Google Scholar] [CrossRef]
- Arnett, D.K.; Blumenthal, R.S.; Albert, M.A.; Buroker, A.B.; Goldberger, Z.D.; Hahn, E.J.; Himmelfarb, C.D.; Khera, A.; Lloyd-Jones, D.; McEvoy, J.W.; et al. 2019 ACC/AHA Guideline on the Primary Prevention of Cardiovascular Disease: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation 2019, 140, e596–e646. [Google Scholar] [CrossRef] [PubMed]
- Mach, F.; Baigent, C.; Catapano, A.L.; Koskinas, K.C.; Casula, M.; Badimon, L.; Chapman, M.J.; De Backer, G.G.; Delgado, V.; Ference, B.A.; et al. 2019 ESC/EAS Guidelines for the management of dyslipidaemias: Lipid modification to reduce cardiovascular risk: The Task Force for the management of dyslipidaemias of the European Society of Cardiology (ESC) and European Atherosclerosis Society (EAS). Eur. Heart J. 2019, 41, 111–188. [Google Scholar] [CrossRef]
- Mente, A.; Dehghan, M.; Rangarajan, S.; McQueen, M.; Dagenais, G.; Wielgosz, A.; Lear, S.; Li, W.; Chen, H.; Yi, S.; et al. Association of dietary nutrients with blood lipids and blood pressure in 18 countries: A cross-sectional analysis from the PURE study. Lancet Diabetes Endocrinol. 2017, 5, 774–787. [Google Scholar] [CrossRef] [PubMed]
- Shen, X.; Fang, A.; He, J.; Liu, Z.; Guo, M.; Gao, R.; Li, K. Trends in dietary fat and fatty acid intakes and related food sources among Chinese adults: A longitudinal study from the China Health and Nutrition Survey (1997–2011). Public Health Nutr. 2017, 20, 2927–2936. [Google Scholar] [CrossRef]
- Willett, W.C. Dietary fats and coronary heart disease. J. Intern. Med. 2012, 272, 13–24. [Google Scholar] [CrossRef] [PubMed]
- Crescenzo, R.; Bianco, F.; Mazzoli, A.; Giacco, A.; Cancelliere, R.; di Fabio, G.; Zarrelli, A.; Liverini, G.; Iossa, S. Fat Quality Influences the Obesogenic Effect of High Fat Diets. Nutrients 2015, 7, 9475–9491. [Google Scholar] [CrossRef]
- Khaw, K.T.; Sharp, S.J.; Finikarides, L.; Afzal, I.; Lentjes, M.; Luben, R.; Forouhi, N.G. Randomised trial of coconut oil, olive oil or butter on blood lipids and other cardiovascular risk factors in healthy men and women. BMJ Open 2018, 8, e020167. [Google Scholar] [CrossRef] [PubMed]
- Zong, G.; Li, Y.; Sampson, L.; Dougherty, L.W.; Willett, W.C.; Wanders, A.J.; Alssema, M.; Zock, P.L.; Hu, F.B.; Sun, Q. Monounsaturated fats from plant and animal sources in relation to risk of coronary heart disease among US men and women. Am. J. Clin. Nutr. 2018, 107, 445–453. [Google Scholar] [CrossRef] [PubMed]
- Guasch-Ferré, M.; Zong, G.; Willett, W.C.; Zock, P.L.; Wanders, A.J.; Hu, F.B.; Sun, Q. Associations of Monounsaturated Fatty Acids From Plant and Animal Sources With Total and Cause-Specific Mortality in Two US Prospective Cohort Studies. Circ. Res. 2019, 124, 1266–1275. [Google Scholar] [CrossRef] [PubMed]
- Zhuang, P.; Zhang, Y.; He, W.; Chen, X.; Chen, J.; He, L.; Mao, L.; Wu, F.; Jiao, J. Dietary Fats in Relation to Total and Cause-Specific Mortality in a Prospective Cohort of 521 120 Individuals With 16 Years of Follow-Up. Circ. Res. 2019, 124, 757–768. [Google Scholar] [CrossRef] [PubMed]
- Liu, H.; Wang, F.; Liu, X.; Xie, Y.; Xia, H.; Wang, S.; Sun, G. Effects of marine-derived and plant-derived omega-3 polyunsaturated fatty acids on erythrocyte fatty acid composition in type 2 diabetic patients. Lipids Health Dis. 2022, 21, 20. [Google Scholar] [CrossRef]
- Zhu, Z.; Yang, X.; Fang, Y.; Zhang, J.; Yang, Z.; Wang, Z.; Liu, A.; He, L.; Sun, J.; Lian, Y.; et al. Trends and Disparities of Energy Intake and Macronutrient Composition in China: A Series of National Surveys, 1982–2012. Nutrients 2020, 12, 2168. [Google Scholar] [CrossRef]
- Yu, D.; Zhao, L.; Zhao, W. Status and trends in consumption of grains and dietary fiber among Chinese adults (1982–2015). Nutr. Rev. 2020, 78, 43–53. [Google Scholar] [CrossRef]
- Song, P.K.; Li, H.; Man, Q.Q.; Jia, S.S.; Li, L.X.; Zhang, J. Trends in Determinants of Hypercholesterolemia among Chinese Adults between 2002 and 2012: Results from the National Nutrition Survey. Nutrients 2017, 9, 279. [Google Scholar] [CrossRef]
- Song, P.; Man, Q.; Li, Y.; Jia, S.; Yu, D.; Zhang, J.; Ding, G. Association between Dietary Patterns and Low HDL-C among Community-Dwelling Elders in North China. Nutrients 2021, 13, 3308. [Google Scholar] [CrossRef]
- He, Y.; Zhao, W.; Zhang, J.; Zhao, L.; Yang, Z.; Huo, J.; Yang, L.; Wang, J.; He, L.; Sun, J.; et al. Data Resource Profile: China National Nutrition Surveys. Int. J. Epidemiol. 2019, 48, 368–368f. [Google Scholar] [CrossRef]
- Yu, D.; Zhao, L.; Zhang, J.; Yang, Z.; Yang, L.; Huang, J.; Fang, H.; Guo, Q.; Xu, X.; Ju, L.; et al. China Nutrition and Health Surveys (1982–2017). China CDC Wkly. 2021, 3, 193–195. [Google Scholar] [CrossRef] [PubMed]
- Yang, Y.; Wang, G.Y.; Pan, X. China Food Composition Tables 2009; Beijing Medical University Publishing House: Beijing, China, 2009. [Google Scholar]
- Yang, Y.; Wang, G.; Pan, X. Chinese Center for Disease Control and Prevention. China Food Composition Tables 2018; Beijing Medical University Publishing House: Beijing, China, 2018. [Google Scholar]
- Zhang, M.; Shi, Y.; Shi, O.; Zhao, Z.; Zhang, X.; Li, C.; Huang, Z.; Zhao, L.; Wang, L.; Li, Y.; et al. Geographical variations in cardiovascular health in China: A nationwide population-based survey of 74,726 adults. Lancet Reg. Health West Pac. 2020, 3, 100033. [Google Scholar] [CrossRef]
- Willett, W.C.; Howe, G.R.; Kushi, L.H. Adjustment for total energy intake in epidemiologic studies. Am. J. Clin. Nutr. 1997, 65, 1220S–1228S. [Google Scholar] [CrossRef] [PubMed]
- Mensink, R.P. Effects of Saturated Fatty Acids on Serum Lipids and Lipoproteins: A Systematic Review and Regression Analysis; World Health Organization: Geneva, Switzerland, 2016. [Google Scholar]
- Miller, V.; Mente, A.; Dehghan, M.; Rangarajan, S.; Zhang, X.; Swaminathan, S.; Dagenais, G.; Gupta, R.; Mohan, V.; Lear, S.; et al. Fruit, vegetable, and legume intake, and cardiovascular disease and deaths in 18 countries (PURE): A prospective cohort study. Lancet 2017, 390, 2037–2049. [Google Scholar] [CrossRef] [PubMed]
- USDA. What We Eat in American. Available online: https://www.ars.usda.gov/northeast-area/beltsville-md-bhnrc/beltsville-human-nutrition-research-center/food-surveys-research-group/docs/wweianhanes-overview/ (accessed on 30 October 2022).
- Eilander, A.; Harika, R.K.; Zock, P.L. Intake and sources of dietary fatty acids in Europe: Are current population intakes of fats aligned with dietary recommendations? Eur. J. Lipid Sci. Technol. 2015, 117, 1370–1377. [Google Scholar] [CrossRef]
- Song, S.; Song, W.O.; Song, Y. Dietary carbohydrate and fat intakes are differentially associated with lipid abnormalities in Korean adults. J. Clin. Lipidol. 2017, 11, 338–347.e333. [Google Scholar] [CrossRef]
- Steur, M.; Johnson, L.; Sharp, S.J.; Imamura, F.; Sluijs, I.; Key, T.J.; Wood, A.; Chowdhury, R.; Guevara, M.; Jakobsen, M.U.; et al. Dietary Fatty Acids, Macronutrient Substitutions, Food Sources and Incidence of Coronary Heart Disease: Findings From the EPIC-CVD Case-Cohort Study Across Nine European Countries. J. Am. Heart Assoc. 2021, 10, e019814. [Google Scholar] [CrossRef]
- Zhu, Y.; Bo, Y.; Liu, Y. Dietary total fat, fatty acids intake, and risk of cardiovascular disease: A dose-response meta-analysis of cohort studies. Lipids Health Dis. 2019, 18, 91. [Google Scholar] [CrossRef]
- Sacks, F.M.; Lichtenstein, A.H.; Wu, J.H.Y.; Appel, L.J.; Creager, M.A.; Kris-Etherton, P.M.; Miller, M.; Rimm, E.B.; Rudel, L.L.; Robinson, J.G.; et al. Dietary Fats and Cardiovascular Disease: A Presidential Advisory from the American Heart Association. Circulation 2017, 136, e1–e23. [Google Scholar] [CrossRef]
- Song, P.K.; Man, Q.Q.; Li, H.; Pang, S.J.; Jia, S.S.; Li, Y.Q.; He, L.; Zhao, W.H.; Zhang, J. Trends in Lipids Level and Dyslipidemia among Chinese Adults, 2002–2015. Biomed. Environ. Sci. 2019, 32, 559–570. [Google Scholar] [CrossRef]
- Katan, M.B.; Zock, P.L.; Mensink, R.P. Effects of fats and fatty acids on blood lipids in humans: An overview. Am. J. Clin. Nutr. 1994, 60, 1017S–1022S. [Google Scholar] [CrossRef] [PubMed]
- Wu, C.; Mi, B.; Luo, W.; Chen, B.; Ma, J.; Huang, H.; Zhang, Q.; Wang, Y.; Liu, H.; Yan, B.; et al. Association between Long-Term Changes in Dietary Percentage of Energy from Fat and Obesity: Evidence from over 20 Years of Longitudinal Data. Nutrients 2022, 14, 3373. [Google Scholar] [CrossRef] [PubMed]
- Vekic, J.; Zeljkovic, A.; Stefanovic, A.; Jelic-Ivanovic, Z.; Spasojevic-Kalimanovska, V. Obesity and dyslipidemia. Metabolism 2019, 92, 71–81. [Google Scholar] [CrossRef] [PubMed]
- Zhao, R.; Zhao, L.; Gao, X.; Yang, F.; Yang, Y.; Fang, H.; Ju, L.; Xu, X.; Guo, Q.; Li, S.; et al. Geographic Variations in Dietary Patterns and Their Associations with Overweight/Obesity and Hypertension in China: Findings from China Nutrition and Health Surveillance (2015–2017). Nutrients 2022, 14, 3949. [Google Scholar] [CrossRef]
- Tan, L.J.; Kim, S.A.; Shin, S. Association between Three Low-Carbohydrate Diet Scores and Lipid Metabolism among Chinese Adults. Nutrients 2020, 12, 1307. [Google Scholar] [CrossRef]
- Hodson, L.; Skeaff, C.M.; Chisholm, W.A. The effect of replacing dietary saturated fat with polyunsaturated or monounsaturated fat on plasma lipids in free-living young adults. Eur. J. Clin. Nutr. 2001, 55, 908–915. [Google Scholar] [CrossRef]
- Becker, N.; Illingworth, D.R.; Alaupovic, P.; Connor, W.E.; Sundberg, E.E. Effects of saturated, monounsaturated, and omega-6 polyunsaturated fatty acids on plasma lipids, lipoproteins, and apoproteins in humans. Am. J. Clin. Nutr. 1983, 37, 355–360. [Google Scholar] [CrossRef]
- Kanner, J. Dietary advanced lipid oxidation endproducts are risk factors to human health. Mol. Nutr. Food Res. 2007, 51, 1094–1101. [Google Scholar] [CrossRef]
| Number of Subjects (%) | Energy, kcal | Total Fat | Animal Fat | SFA | MUFA | PUFA | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| g | % kcal | g | % kcal | g | % kcal | g | % kcal | g | % kcal | |||
| All participants | 48,375 (100.0) | 1668.9 (1335.4–2066.1) 2 | 63.6 (45.1–86.6) | 34.8 (27.5–43.6) | 22.1 (10.2–38.3) | 12.3 (6.0–19.9) | 14.3 (9.8–20.3) | 7.9 (5.8–10.2) | 23.5 (15.6–34.2) | 12.7 (9.3–17.1) | 15.5 (10.2–23.1) | 8.4 (5.9–11.9) |
| Age group, year | ||||||||||||
| 30.0–44.9 | 12,306 (25.4) | 1661.9 (1328.9–2066.5) * | 63.5 (44.9–86.5) | 34.7 (27.8–42.7) | 24.3 (12.3–40.8) | 13.5 (7.2–21.1) * | 14.8 (10.1–20.8) | 8.1 (6.0–10.5) * | 23.4 (15.6–34.1) | 12.8 (9.5–16.9) | 14.8 (9.8–22.1) | 8.1 (5.8–11.4) † |
| 45.0–59.9 | 22,394 (46.3) | 1698.6 (1357.3–2088.0) * | 64.9 (46.2–87.9) | 35.0 (27.5–43.7) | 21.3 (9.6–37.2) | 11.7 (5.5–19.2) * | 14.3 (9.8–20.3) | 7.7 (5.8–10) * | 23.9 (16.0–34.8) | 12.7 (9.3–17.3) | 16.2 (10.7–24.2) | 8.8 (6.0–12.3) † |
| 60.0–69.9 | 13,675 (28.3) | 1624.2 (1301.8–2008.8) * | 60.5 (42.9–83.2) | 34.7 (26.5–43.3) | 17.9 (7.3–33.2) | 10.3 (4.4–17.9) * | 12.9 (8.7–18.5) | 7.3 (5.3–9.7) * | 22.4 (14.8–33.2) | 12.6 (8.9–17.3) | 15.7 (10.3–23.0) | 8.7 (6.1–12.2) † |
| Sex | ||||||||||||
| Male | 21,679 (44.8) | 1864.1 (1500.8–2278.3) † | 70.2 (50.5–94.6) | 34.5 (27.6–43.1) † | 26.0 (12.5–43.8) | 13.0 (6.5–20.8) † | 16.1 (11.1–22.6) | 7.9 (5.9–10.3) † | 26.2 (17.6–37.8) | 12.8 (9.5–17.2) | 16.9 (11.1–25.1) | 8.2 (5.8–11.6) † |
| Female | 26,696 (55.2) | 1517.3 (1225.8–1848.0) † | 57.8 (41.1–78.2) | 35.1 (27.4–43.3) † | 18.9 (8.8–33.2) | 11.8 (5.6–19.2) † | 12.8 (8.7–18.0) | 7.8 (5.7–10.1) † | 21.4 (14.1–30.7) | 12.7 (9.2–17.1) | 14.4 (9.5–21.2) | 8.6 (6–12.1) † |
| Location | ||||||||||||
| Urban | 19,981 (41.3) | 1628.7 (1306.2–2023.7) † | 62.5 (45.1–85.9) | 35.2 (28.5–43) | 23.9 (12.4–38.5) | 13.5 (7.5–20.3) † | 14.8 (10.4–20.4) | 8.2 (6.3–10.5) † | 23.1 (15.6–33.2) | 12.7 (9.6–16.8) | 15.2 (10.1–22.4) | 8.5 (6–11.6) |
| Rural | 28,394 (58.7) | 1716.4 (1366.5–2124.2) † | 64.3 (45.1–87.6) | 34.3 (26.4–43.4) | 19.8 (8.2–38.0) | 10.9 (4.6–19.3) † | 13.8 (9.1–20.0) | 7.4 (5.3–9.8) † | 24.0 (15.6–35.6) | 12.8 (9–17.5) | 15.9 (10.3–23.9) | 8.4 (5.7–12.2) |
| Region | ||||||||||||
| North | 20,090 (41.5) | 1606.3 (1272.6–2002.5) † | 53.2 (37.4–74.5) | 30.8 (23.5–38.8) † | 13.7 (5.8–25.7) | 8.1 (3.2–14.0) † | 11.7 (8.0–16.7) | 6.8 (4.9–8.8) † | 17.4 (11.5–25.6) | 10.0 (7.2–13.2) † | 16.2 (10.4–25.0) | 9.3 (6.2–13.4) † |
| South | 28,285 (58.5) | 1710.8 (1375.3–2100.5) † | 69.4 (51.4–92.9) | 37.4 (30.1–45.6) † | 28.1 (15.3–45.1) | 15.1 (8.8–22.9) † | 16.1 (11.2–22.3) | 8.5 (6.5–10.9) † | 27.4 (19.6–39.0) | 14.6 (11.2–19.2) † | 15.0 (10.1–22.1) | 8.1 (5.7–11.1) † |
| Education | ||||||||||||
| Illiteracy | 6338 (13.1) | 1573.2 (1255.3–1953.8) † | 58.2 (40.6–80.7) | 34.7 (25.6–43.9) | 15.0 (5.2–31.5) | 8.7 (3.1–17.7) * | 11.6 (7.5–17.2) | 6.9 (4.7–9.3) * | 22.5 (14.4–34.0) | 12.9 (8.9–18.7) * | 14.8 (9.6–22.3) | 8.6 (5.8–12.4) * |
| Primary school | 16,970 (35.1) | 1686.4 (1344.4–2085.8) † | 64.8 (45.9–88.4) | 35.5 (27.6–44.3) | 20.4 (8.8–38.2) | 11.5 (5.1–20) * | 13.8 (9.4–19.9) | 7.6 (5.5–10.1) * | 24.7 (16.3–37.1) | 13.4 (9.6–18.5) * | 15.7 (10.3–23.5) | 8.5 (5.8–12.1) * |
| Middle school | 15,466 (32.0) | 1726.0 (1374.9–2126.6) † | 65.5 (46.6–88.2) | 34.3 (27.4–42.7) | 22.2 (10.4–38.0) | 12.1 (6.0–19.1) * | 14.7 (10.0–20.5) | 7.8 (5.8–9.9) * | 23.9 (15.7–34.2) | 12.6 (9.2–16.6) * | 16.2 (10.8–24.0) | 8.5 (6.1–12.1) * |
| High school | 6417 (13.3) | 1656.5 (1330.5–2045.0) † | 62.0 (44.9–86.4) | 34.9 (28–43) | 23.5 (13.1–39.0) | 13.5 (7.5–20.7) * | 15.0 (10.3–21.2) | 8.4 (6.3–10.6) * | 23.0 (15.4–33.7) | 12.6 (9.3–16.6) * | 15.3 (10.1–22.9) | 8.5 (5.8–11.8) * |
| College and above | 3184 (6.6) | 1587.9 (1272.1–1962.8) † | 59.7 (43.4–81.9) | 34.5 (28.3–41.7) | 26.9 (15.8–41.6) | 15.6 (10.0–21.7) * | 15.3 (11.0–21.0) | 8.8 (7.1–10.9) * | 21.4 (14.8–29.9) | 12.2 (9.5–15.7) * | 13.7 (9.1–20.3) | 7.9 (5.7–10.8) * |
| Smoking status | ||||||||||||
| Never | 32,703 (67.6) | 1589.6 (1280.6–1954.7) * | 60.4 (42.8–82.1) | 34.9 (27.2–43.1) * | 20.4 (9.4–35.4) | 12.0 (5.8–19.4) * | 13.5 (9.1–18.9) | 7.8 (5.8–10.1) * | 22.2 (14.8–32.3) | 12.6 (9.2–16.9) * | 14.8 (9.8–22.2) | 8.6 (5.9–12) |
| Ever | 3057 (6.3) | 1833.3 (1476.7–2208.6) * | 67.9 (49.1–88.6) | 34.0 (27–42.3) * | 22.2 (9.7–37.5) | 11.4 (5.3–17.9) * | 15.4 (10.1–20.9) | 7.6 (5.7–9.7) * | 25.5 (17.1–35.4) | 12.5 (9.2–16.8) * | 17.1 (11.5–24.5) | 8.3 (6–11.9) |
| Current, <10 cigarettes/day | 2989 (6.2) | 1862.8 (1492.2–2230.1) * | 69.7 (51.0–93.6) | 34.5 (27.9–43.0) * | 26.8 (12.3–45.0) | 13.9 (6.5–21.5) * | 16.0 (11.0–22.9) | 8.1 (5.9–10.3) * | 26.6 (17.8–37.4) | 12.9 (9.6–17.2) * | 16.4 (10.9–23.9) | 8.0 (5.6–11.3) |
| Current, 10–19 cigarettes/day | 2882 (6.0) | 1849.4 (1494.2–2296.6) * | 68.9 (49.2–97.2) | 34.7 (28.4–43.7) * | 26.2 (13.8–43.3) | 13.3 (6.6–21.1) * | 16.3 (11.0–23.7) | 8.1 (6.2–10.9) * | 26.3 (17.2–37.8) | 12.8 (9.7–17.4) * | 16.7 (10.9–25.6) | 8.4 (5.8–12) |
| Current, ≥20 cigarettes/day | 6744 (9.4) | 1868.2 (1489.6–2309.5) * | 72.4 (52.1–97.3) | 35.4 (28.2–44.3) * | 28.0 (13.3–47.0) | 13.9 (6.9–22.0) * | 16.4 (11.2–23.1) | 8.2 (6.0–10.4) * | 27.4 (18.7–39.8) | 13.3 (9.9–17.9) * | 17.1 (11.2–25.2) | 8.2 (5.7–11.6) |
| Drinking status | ||||||||||||
| Never | 29,758 (61.5) | 1593.8 (1277.2–1969.2) * | 60.7 (42.9–82.4) | 35.0 (27.2–43.6) | 20.2 (9.0–36.0) | 12.0 (5.5–19.7) | 13.3 (9.0–19.1) | 7.7 (5.7–10.2) † | 22.4 (14.7–32.8) | 12.8 (9.2–17.3) | 14.9 (9.8–22.1) | 8.5 (6–12) |
| Moderate | 12,476 (25.8) | 1744.5 (1398.2–2122.2) * | 66.5 (47.5–89.3) | 34.7 (27.9–42.9) | 24.0 (12.3–39.6) | 13.0 (6.7–19.9) | 15.3 (10.5–21.1) | 8.1 (6.1–10.2) † | 24.5 (16.6–35.4) | 12.7 (9.6–16.9) | 15.9 (10.5–24.0) | 8.4 (5.8–11.9) |
| Excessive, 15–24.9 g/day | 1599 (3.3) | 1791.0 (1475.7–2197.4) * | 68.8 (47.5–93.9) | 34.1 (25.9–42.4) | 25.0 (13.4–43.6) | 13.0 (7.1–20.7) | 15.7 (10.2–22.4) | 7.7 (5.6–9.9) † | 25.2 (15.9–36.3) | 12.5 (8.6–17.5) | 15.5 (10.1–24.8) | 7.9 (5.5–11.3) |
| Excessive, ≥25.0 g/day | 4542 (9.4) | 1904.7 (1524.7–2352.9) * | 71.8 (53.0–94.9) | 34.4 (28.1–42.6) | 26.9 (11.8–44.8) | 12.7 (6.4–20.8) | 16.4 (11.7–22.7) | 7.9 (6–10.1) † | 26.9 (18.2–37.6) | 12.7 (9.7–16.8) | 17.8 (11.5–25.5) | 8.4 (5.8–11.9) |
| Family history | ||||||||||||
| Yes | 20,404 (42.2) | 1669.4 (1338.5–2064.1) | 63.0 (45.2–85.5) | 34.3 (27.2–42.7) | 21.4 (10.6–36.3) | 12.1 (6.1–18.9) † | 14.2 (9.9–20.1) | 7.8 (5.9–10) † | 22.8 (15.2–32.7) | 12.3 (9–16.4) † | 15.9 (10.6–23.8) | 8.6 (6.2–12.2) † |
| No | 27,971 (57.8) | 1668.2 (1330.9–2067.9) | 64.1 (45.0–87.5) | 35.3 (27.7–43.7) | 22.9 (10.0–39.9) | 12.7 (6–20.9) † | 14.4 (9.6–20.4) | 7.9 (5.8–10.3) † | 24.2 (15.9–35.5) | 13.2 (9.6–17.7) † | 15.1 (9.9–22.6) | 8.3 (5.7–11.6) † |
| Hypertension | ||||||||||||
| Yes | 21,370 (44.2) | 1661.7 (1333.3–2062.7) | 64.1 (45.7–86.9) | 34.1 (26.7–43.2) † | 23.6 (11.6–39.6) | 11.2 (5–18.5) † | 14.7 (10.0–20.7) | 7.5 (5.6–9.8) † | 23.7 (15.9–34.5) | 12.3 (8.9–17) | 15.0 (10.0–22.6) | 8.7 (6.1–12.3) |
| No | 27,005 (55.8) | 1684.0 (1338.2–2073.4) | 62.5 (44.4–86.0) | 35.3 (27.9–43.2) † | 20.0 (8.5–35.8) | 13.2 (6.7–20.8) † | 13.7 (9.3–19.6) | 8.1 (6–10.4) † | 23.0 (15.1–33.7) | 13.0 (9.6–17.2) | 16.1 (10.6–24.0) | 8.3 (5.8–11.6) |
| Food Group | In SFA, % | In MUFA, % | In PUFA, % | In Total Fat, % | |
|---|---|---|---|---|---|
| Major Animal sources | Pork | 30.4 ± 0.5 | 24.9 ± 0.5 | 9.8 ± 0.3 | 18.9 ± 0.5 |
| Other meats | 2.5 ± 0.1 | 1.5 ± 0.1 | 0.8 ± 0.0 | 1.5 ± 0.1 | |
| Processed meat | 1.3 ± 0.1 | 1.1 ± 0.1 | 0.5 ± 0.0 | 1.0 ± 0.1 | |
| Poultry | 3.4 ± 0.2 | 3.2 ± 0.3 | 1.9 ± 0.2 | 2.6 ± 0.2 | |
| Fish | 1.2 ± 0.1 | 1.1 ± 0.1 | 1.0 ± 0.1 | 1.0 ± 0.1 | |
| Dairy and eggs | 9.6 ± 0.3 | 3.2 ± 0.1 | 1.1 ± 0.0 | 3.9 ± 0.1 | |
| Major Plant sources | Nuts and soybeans | 5.7 ± 0.2 | 4.7 ± 0.2 | 8.9 ± 0.2 | 5.6 ± 0.1 |
| High MUFA oils | 6.6 ± 0.5 | 17.0 ± 1.1 | 16.3 ± 1.1 | 13.5 ± 0.9 | |
| MUFA–PUFA balanced oils | 11.5 ± 0.7 | 16.3 ± 1.0 | 21.7 ± 1.4 | 14.8 ± 0.9 | |
| High PUFA oils | 11.1 ± 0.7 | 13.9 ± 0.9 | 23.8 ± 1.3 | 15.5 ± 0.9 | |
| High SFA oils | 0.0 ± 0.0 | 0.0 ± 0.0 | 0.0 ± 0.0 | 0.0 ± 0.0 | |
| Other | 16.7 ± 0.5 | 13.0 ± 0.4 | 14.3 ± 0.4 | 21.7 ± 0.5 | |
| Fats | Lipid Markers | <Median, E% | ≥Median, E% | p-interaction |
|---|---|---|---|---|
| Total fat | TC, mmol/L | 0.015 (0.003–0.027) | −0.001 (−0.009–0.007) | 0.005 |
| LDL-c, mmol/L | 0.008 (−0.002–0.018) | −0.003 (−0.011–0.005) | 0.029 | |
| HDL-c, mmol/L | 0.007 (0.003–0.011) | 0.000 (−0.002–0.002) | 0.000 | |
| TG, mmol/L | −0.013 (−0.027–0.001) | 0.002 (−0.008–0.012) | 0.018 | |
| TCHDL | −0.009 (−0.021–0.003) | −0.004 (−0.014–0.006) | 0.345 | |
| TGHDL | −0.022 (−0.038–−0.006) | −0.001 (−0.0128–0.016) | 0.012 | |
| SFA | TC, mmol/L | 0.207 (0.162–0.252) | 0.066 (0.044–0.088) | <0.0001 |
| LDL-c, mmol/L | 0.163 (0.124–0.202) | 0.057 (0.039–0.075) | <0.0001 | |
| HDL-c, mmol/L | 0.041 (0.025–0.057) | −0.001 (−0.009–0.007) | <0.0001 | |
| TG, mmol/L | −0.032 (−0.085–0.021) | 0.033 (0.009–0.057) | 0.029 | |
| TCHDL | 0.057 (0.004–0.110) | 0.046 (0.022–0.070) | 0.801 | |
| TGHDL | −0.070 (−0.141–0.001) | 0.026 (−0.005–0.057) | 0.009 | |
| MUFA | TC, mmol/L | 0.054 (0.027–0.081) | −0.033 (−0.045–−0.021) | <0.0001 |
| LDL-c, mmol/L | 0.027 (0.004–0.051) | −0.034 (−0.046–−0.022) | <0.0001 | |
| HDL-c, mmol/L | 0.031 (0.0212–0.041) | 0.002 (−0.002–0.006) | <0.0001 | |
| TG, mmol/L | −0.032 (−0.063–−0.001) | 0.018 (0.004–0.032) | 0.000 | |
| TCHDL | −0.049 (−0.080–−0.018) | −0.031 (−0.045–−0.017) | 0.669 | |
| TGHDL | −0.065 (−0.106–−0.023) | 0.013 (−0.007–0.033) | 0.000 | |
| Plant MUFA | TC, mmol/L | −0.094 (−0.127–−0.061) | −0.044 (−0.056–−0.032) | 0.010 |
| LDL-c, mmol/L | −0.068 (−0.097–−0.039) | −0.045 (−0.055–−0.035) | 0.381 | |
| HDL-c, mmol/L | 0.006 (−0.006–0.018) | 0.001 (−0.003–0.005) | 0.854 | |
| TG, mmol/L | −0.107 (−0.148–−0.066) | 0.017 (0.003–0.031) | <0.0001 | |
| TCHDL | −0.104 (−0.143–−0.065) | −0.034 (−0.048–−0.020) | 0.010 | |
| TGHDL | −0.118 (−0.171–−0.065) | 0.017 (−0.001–0.035) | <0.0001 |
| Replacement | Lipid Biomarkers | Overall | p | <Median | >Median | p-interaction |
|---|---|---|---|---|---|---|
| Total fat to carbohydrate | TC, mmol/L | 0.004 (−0.002–0.010) | 0.091 | 0.000 (−0.009–0.008) | 0.009 (0.001–0.018) | 0.094 |
| LDL-c, mmol/L | 0.009 (0.005–0.013) | 0.000 | 0.010 (0.003–0.018) | 0.011 (0.003–0.018) | 0.967 | |
| HDL-c, mmol/L | −0.005 (−0.007–−0.003) | <0.0001 | −0.011 (−0.013–−0.008) | 0.000 (−0.003–0.003) | <0.0001 | |
| TG, mmol/L | 0.004 (−0.002–0.010) | 0.206 | 0.007 (−0.003–0.017) | −0.004 (−0.014–0.006) | 0.095 | |
| TCHDL | 0.017 (0.011–0.023) | <0.0001 | 0.028 (0.018–0.037) | 0.008 (−0.002–0.017) | 0.002 | |
| TGHDL | 0.008 (0.000–0.016) | 0.041 | 0.017 (0.004–0.029) | −0.002 (−0.015–0.010) | 0.028 | |
| Animal fat to carbohydrate | TC, mmol/L | −0.017 (−0.023–−0.011) | <0.0001 | −0.019 (−0.028–−0.010) | −0.012 (−0.021–−0.003) | 0.224 |
| LDL-c, mmol/L | −0.006 (−0.012–0.000) | 0.042 | −0.002 (−0.010–0.006) | −0.004 (−0.012–0.004) | 0.753 | |
| HDL-c, mmol/L | −0.008 (−0.01–−0.006) | <0.0001 | −0.013 (−0.016–−0.010) | −0.003 (−0.006–0.000) | <0.0001 | |
| TG, mmol/L | −0.013 (−0.021–−0.005) | 0.001 | −0.007 (−0.017–0.003) | −0.020 (−0.031–−0.010) | 0.049 | |
| TCHDL | 0.007 (0.000–0.014) | 0.053 | 0.019 (0.009–0.030) | −0.002 (−0.012–0.009) | 0.001 | |
| TGHDL | −0.005 (−0.015–0.005) | 0.266 | 0.005 (−0.008–0.019) | −0.015 (−0.029–−0.002) | 0.017 | |
| Plant fat to carbohydrate | TC, mmol/L | 0.012 (0.006–0.018) | <0.0001 | 0.004 (−0.005–0.012) | 0.019 (0.010–0.027) | 0.009 |
| LDL-c, mmol/L | 0.015 (0.011–0.019) | <0.0001 | 0.013 (0.006–0.021) | 0.018 (0.011–0.025) | 0.364 | |
| HDL-c, mmol/L | −0.005 (−0.007–−0.003) | <0.0001 | −0.010 (−0.013–−0.008) | 0.000 (−0.002–0.003) | 0.594 | |
| TG, mmol/L | 0.009 (0.003–0.015) | 0.003 | 0.009 (0.000–0.019) | 0.002 (−0.008–0.012) | 0.055 | |
| TCHDL | 0.022 (0.016–0.028) | <0.0001 | 0.030 (0.020–0.040) | 0.013 (0.004–0.023) | 0.011 | |
| TGHDL | 0.013 (0.005–0.021) | 0.002 | 0.019 (0.006–0.031) | 0.003 (−0.010–0.015) | 0.064 | |
| SFA to carbohydrate | TC, mmol/L | −0.040 (−0.05–−0.03) | <0.0001 | −0.037 (−0.047–−0.027) | −0.039 (−0.050–−0.027) | 0.794 |
| LDL-c, mmol/L | −0.018 (−0.026–−0.01) | <0.0001 | −0.013 (−0.022–−0.004) | −0.020 (−0.030–−0.01) | 0.148 | |
| HDL-c, mmol/L | −0.015 (−0.019–−0.011) | <0.0001 | −0.018 (−0.022–−0.015) | −0.010 (−0.014–−0.006) | <0.0001 | |
| TG, mmol/L | −0.007 (−0.017–0.003) | 0.217 | −0.003 (−0.015–0.009) | −0.014 (−0.027–0.000) | 0.116 | |
| TCHDL | 0.007 (−0.003–0.017) | 0.182 | 0.017 (0.005–0.029) | −0.007 (−0.020–0.007) | 0.000 | |
| TGHDL | 0.004 (−0.010–0.018) | 0.548 | 0.013 (−0.002–0.027) | −0.006 (−0.024–0.011) | 0.042 | |
| MUFA to carbohydrate | TC, mmol/L | 0.022 (0.014–0.030) | <0.0001 | 0.013 (0.004–0.023) | 0.030 (0.020–0.040) | 0.003 |
| LDL-c, mmol/L | 0.034 (0.028–0.040) | <0.0001 | 0.030 (0.021–0.038) | 0.038 (0.029–0.047) | 0.098 | |
| HDL-c, mmol/L | −0.011 (−0.013–−0.009) | <0.0001 | −0.015 (−0.018–−0.012) | −0.005 (−0.008–−0.001) | <0.0001 | |
| TG, mmol/L | −0.017 (−0.025–−0.009) | 0.000 | −0.010 (−0.021–0.002) | −0.025 (−0.037–−0.013) | 0.041 | |
| TCHDL | 0.044 (0.036–0.052) | <0.0001 | 0.048 (0.037–0.059) | 0.035 (0.023–0.046) | 0.047 | |
| TGHDL | −0.007 (−0.019–0.005) | 0.232 | 0.003 (−0.012–0.017) | −0.018 (−0.034–−0.003) | 0.015 | |
| PUFA to carbohydrate | TC, mmol/L | 0.011 (0.003–0.019) | 0.006 | 0.005 (−0.004–0.014) | 0.018 (0.007–0.028) | 0.028 |
| LDL-c, mmol/L | 0.017 (0.011–0.023) | <0.0001 | 0.016 (0.008–0.024) | 0.020 (0.010–0.029) | 0.485 | |
| HDL-c, mmol/L | −0.007 (−0.009–−0.005) | <0.0001 | −0.012 (−0.015–−0.008) | −0.002 (−0.005–0.002) | <0.0001 | |
| TG, mmol/L | 0.023 (0.013–0.033) | <0.0001 | 0.022 (0.010–0.033) | 0.017 (0.005–0.030) | 0.524 | |
| TCHDL | 0.024 (0.014–0.034) | <0.0001 | 0.031 (0.021–0.042) | 0.014 (0.002–0.026) | 0.008 | |
| TGHDL | 0.024 (0.012–0.036) | <0.0001 | 0.028 (0.013–0.042) | 0.014 (−0.002–0.030) | 0.119 |
| Replacement | Lipid Biomarkers | Overall | p | <Median | >Median | p-Interaction |
|---|---|---|---|---|---|---|
| Animal fat to plant fat | TC, mmol/L | −0.048 (−0.054–−0.042) | <0.0001 | −0.068 (−0.078–−0.058) | −0.045 (−0.051–−0.039) | 0.001 |
| LDL-c, mmol/L | −0.039 (−0.043–−0.035) | <0.0001 | −0.052 (−0.062–−0.042) | −0.037 (−0.043–−0.031) | 0.004 | |
| HDL-c, mmol/L | −0.002 (−0.004–0.000) | 0.007 | −0.006 (−0.01–−0.002) | −0.002 (−0.004–0.000) | 0.194 | |
| TG, mmol/L | −0.022 (−0.028–−0.016) | <0.0001 | −0.035 (−0.047–−0.023) | −0.018 (−0.024–−0.012) | 0.003 | |
| TCHDL | −0.032 (−0.038–−0.026) | <0.0001 | −0.043 (−0.055–−0.031) | −0.029 (−0.035–−0.023) | 0.038 | |
| TGHDL | −0.019 (−0.027–−0.011) | <0.0001 | −0.032 (−0.048–−0.016) | −0.015 (−0.023–−0.007) | 0.016 | |
| SFA to MUFA | TC, mmol/L | −0.160 (−0.178–−0.142) | <0.0001 | −0.170 (−0.221–−0.119) | −0.155 (−0.175–−0.135) | 0.599 |
| LDL-c, mmol/L | −0.145 (−0.159–−0.131) | <0.0001 | −0.158 (−0.203–−0.113) | −0.141 (−0.159–−0.123) | 0.228 | |
| HDL-c, mmol/L | −0.001 (−0.007–0.005) | 0.658 | 0.006 (−0.003–0.014) | −0.002 (−0.008–0.004) | 0.043 | |
| TG, mmol/L | 0.025 (0.005–0.045) | 0.012 | 0.017 (−0.012–0.047) | 0.027 (0.007–0.047) | 0.048 | |
| TCHDL | −0.122 (−0.142–−0.102) | <0.0001 | −0.149 (−0.178–−0.120) | −0.118 (−0.138–−0.098) | 0.017 | |
| TGHDL | 0.021 (−0.004–0.046) | 0.109 | −0.007 (−0.034–0.042) | 0.024 (−0.002–0.050) | 0.240 | |
| SFA to PUFA | TC, mmol/L | −0.140 (−0.154–−0.126) | <0.0001 | −0.157 (−0.182–−0.136) | −0.131 (−0.150–−0.120) | 0.036 |
| LDL-c, mmol/L | −0.113 (−0.125–−0.101) | <0.0001 | −0.123 (−0.147–−0.099) | −0.106 (−0.122–−0.09) | 0.106 | |
| HDL-c, mmol/L | −0.009 (−0.013–−0.005) | 0.000 | −0.011 (−0.019–−0.003) | −0.008 (−0.013–−0.003) | 0.523 | |
| TG, mmol/L | −0.047 (−0.065–−0.029) | <0.0001 | −0.067 (−0.094–−0.04) | −0.042 (−0.060–−0.024) | 0.076 | |
| TCHDL | −0.083 (−0.099–−0.067) | <0.0001 | −0.090 (−0.121–−0.059) | −0.088 (−0.110–−0.066) | 0.344 | |
| TGHDL | −0.034 (−0.056–−0.012) | 0.002 | −0.013 (−0.054–0.028) | −0.054 (−0.081–−0.027) | 0.263 |
| Replacement | Present, 11 g, Overall | Present, 11 g, <Median | Present, 11 g, >Median | WHO, 4% TE | PURE, Overall, 5% TE | PURE, China, 5% TE | |
|---|---|---|---|---|---|---|---|
| SFA to carbohydrate | TC | −0.040 (−0.050–−0.030) | −0.037 (−0.047–−0.027) | −0.039 (−0.050–−0.027) | −0.164 (−0.188–−0.140) | −0.085 (−0.089–−0.081) | −0.034 (−0.062–−0.007) |
| LDL-c | −0.018 (−0.026–−0.010) | −0.013 (−0.022–−0.004) | −0.020 (−0.030–−0.010) | −0.132 (−0.156–−0.108) | −0.093 (−0.097–−0.089) | −0.025 (−0.049–−0.001) | |
| HDL-c | −0.015 (−0.019–−0.011) | −0.018 (−0.022–−0.015) † | −0.010 (−0.014–−0.006) † | −0.040 (−0.048–−0.032) | −0.029 (−0.031–−0.028) | −0.020 (−0.030–−0.010) | |
| TG | NS | NS | −0.014 (−0.027–0.000) | 0.044 (0.028–0.056) | 0.022 (0.017–0.026) | 0.053 (0.020–0.085) | |
| TCHDL | NS | 0.017 (0.005–0.029) † | NS | NS | 0.120 (0.066–0.174) | 0.037 (0.004–0.070) | |
| TGHDL | NS | 0.013 (−0.002–0.027) † | NS | 0.056 (0.040–0.072) | 0.047 (0.041–0.053) | 0.067 (0.026–0.109) | |
| SFA to MUFA | TC | −0.160 (−0.178–−0.142) | −0.170 (−0.221–−0.119) | −0.155 (−0.175–−0.135) | −0.184 (−0.204–−0.160) | −0.133 (−0.143–−0.124) | NS |
| LDL-c | −0.145 (−0.159–−0.131) | −0.158 (−0.203–−0.113) | −0.141 (−0.159–−0.123) | −0.168 (−0.188–−0.148) | −0.182 (−0.192–−0.173) | −0.010 (−0.056–−0.036) | |
| HDL-c | NS | NS | NS | −0.008 (−0.016–0.000) | −0.028 (−0.031–−0.024) | NS | |
| TG | 0.025 (0.005–0.045) | NS | 0.027 (0.007–0.047) † | −0.016 (−0.028–−0.004) | 0.032 (0.021–0.043) | 0.094 (0.031–0.158) | |
| TCHDL | −0.122 (−0.142–−0.102) | −0.149 (−0.178–−0.120) † | −0.118 (−0.138–−0.098) † | −0.108 (−0.132–−0.088) | −0.045 (−0.058–−0.032) | NS | |
| TGHDL | NS | NS | NS | NS | 0.050 (0.036–0.064) | 0.085 (0.005–0.164) | |
| SFA to PUFA | TC | −0.140 (−0.154–−0.126) | −0.157 (−0.182–−0.136) † | −0.131 (−0.150–−0.120) † | −0.256 (−0.280–−0.232) | −0.045 (−0.053–−0.036) | −0.048 (−0.075–−0.027) |
| LDL-c | −0.113 (−0.125–−0.101) | −0.123 (−0.147–−0.099) | −0.106 (−0.122–−0.09) | −0.220 (−0.244–−0.200) | −0.016 (−0.024–−0.008) | −0.040 (−0.063–−0.016) | |
| HDL-c | −0.009 (−0.013–−0.005) | −0.011 (−0.019–−0.003) | −0.008 (−0.013–−0.003) | −0.020 (−0.024–−0.012) | −0.026 (−0.029–−0.023) | −0.025 (−0.034–−0.015) | |
| TG | −0.047 (−0.065–−0.029) | −0.067 (−0.094–−0.04) | −0.042 (−0.060–−0.024) | −0.040 (−0.056–−0.028) | 0.016 (0.006–0.025) | 0.064 (0.032–0.096) | |
| TCHDL | −0.083 (−0.099–−0.067) | −0.090 (−0.121–−0.059) | −0.088 (−0.110–−0.066) | −0.136 (−0.160–−0.112) | 0.035 (0.025–0.047) | 0.034 (0.002–0.066) | |
| TGHDL | −0.034 (−0.056–−0.012) | −0.013 (−0.054–0.028) | −0.054 (−0.081–−0.027) | −0.020 (−0.036–−0.008) | 0.034 (0.022–0.046) | 0.082 (0.042–0.122) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zhao, R.; Zhao, L.; Yang, F.; Ju, L.; Li, S.; Cheng, X.; Xu, X.; Guo, Q.; Cai, S.; Fang, H.; et al. Dietary Fat Intake among Chinese Adults and Their Relationships with Blood Lipids: Findings from China Nutrition and Health Surveillance and Comparison with the PURE Study. Nutrients 2022, 14, 5262. https://doi.org/10.3390/nu14245262
Zhao R, Zhao L, Yang F, Ju L, Li S, Cheng X, Xu X, Guo Q, Cai S, Fang H, et al. Dietary Fat Intake among Chinese Adults and Their Relationships with Blood Lipids: Findings from China Nutrition and Health Surveillance and Comparison with the PURE Study. Nutrients. 2022; 14(24):5262. https://doi.org/10.3390/nu14245262
Chicago/Turabian StyleZhao, Rongping, Liyun Zhao, Fan Yang, Lahong Ju, Shujuan Li, Xue Cheng, Xiaoli Xu, Qiya Guo, Shuya Cai, Hongyun Fang, and et al. 2022. "Dietary Fat Intake among Chinese Adults and Their Relationships with Blood Lipids: Findings from China Nutrition and Health Surveillance and Comparison with the PURE Study" Nutrients 14, no. 24: 5262. https://doi.org/10.3390/nu14245262
APA StyleZhao, R., Zhao, L., Yang, F., Ju, L., Li, S., Cheng, X., Xu, X., Guo, Q., Cai, S., Fang, H., Yu, D., & Ding, G. (2022). Dietary Fat Intake among Chinese Adults and Their Relationships with Blood Lipids: Findings from China Nutrition and Health Surveillance and Comparison with the PURE Study. Nutrients, 14(24), 5262. https://doi.org/10.3390/nu14245262




