Staple Food Preference and Obesity Phenotypes: The Regional Ethnic Cohort Study in Northwest China
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design and Population
2.2. Assessment of Staple Food Preference
2.3. Definition of Outcomes
2.4. Statistical Analysis
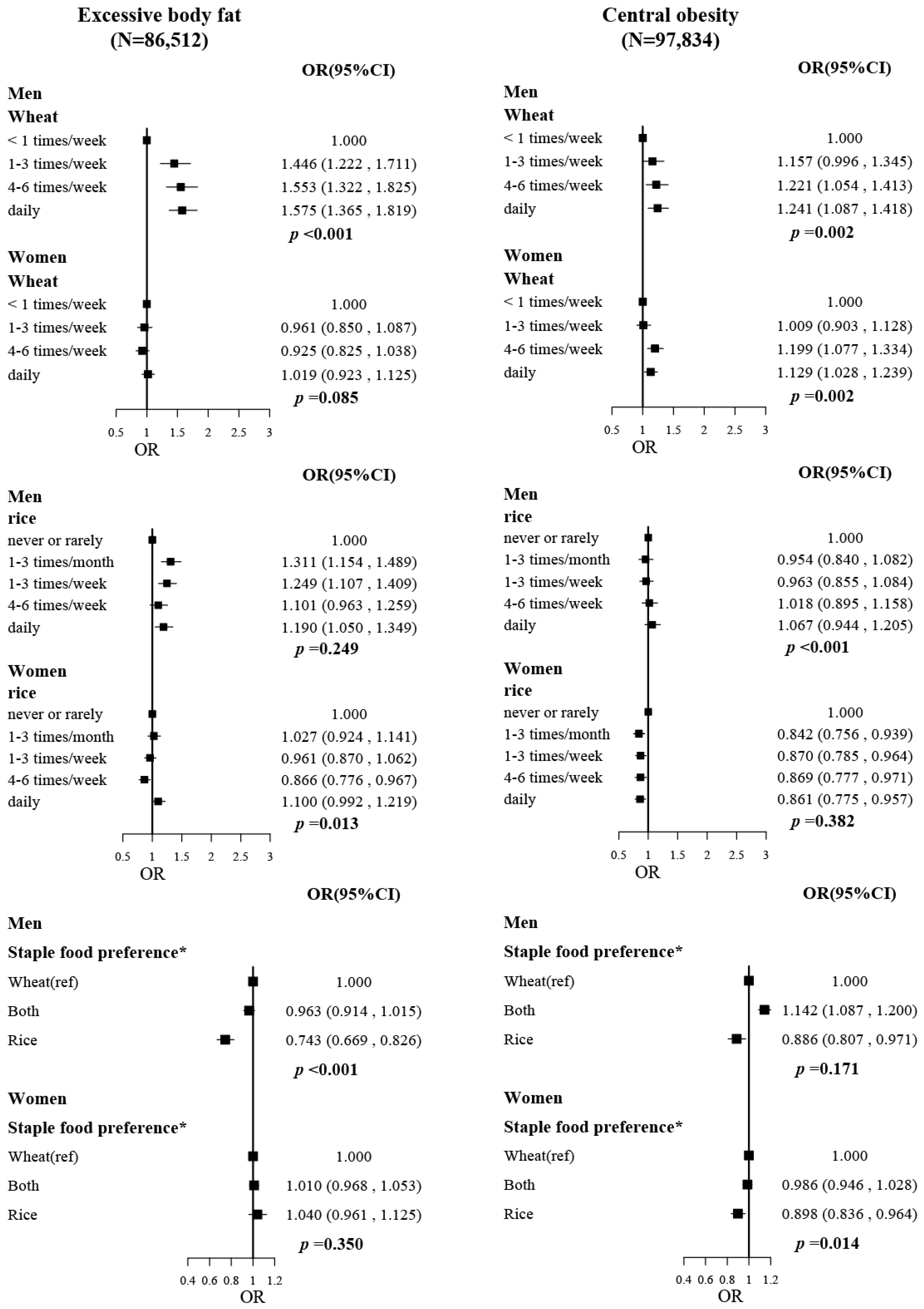
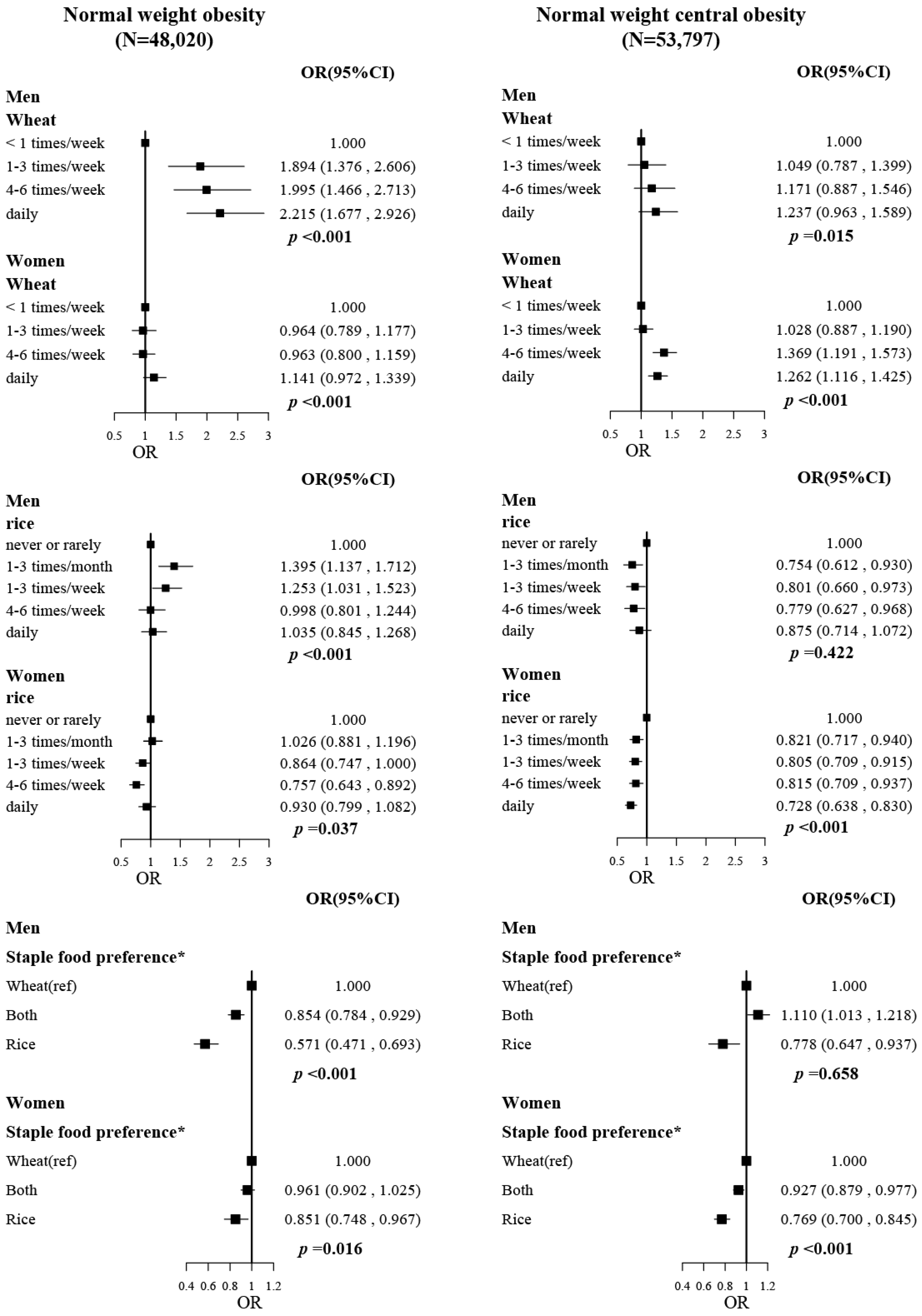
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Harrison, S.; Dixon, P.; Jones, H.E.; Davies, A.R.; Howe, L.D.; Davies, N.M. Long-term cost-effectiveness of interventions for obesity: A mendelian randomisation study. PLoS Med. 2021, 18, e1003725. [Google Scholar] [CrossRef] [PubMed]
- Bragg, F.; Tang, K.; Guo, Y.; Iona, A.; Du, H.; Holmes, M.V.; Bian, Z.; Kartsonaki, C.; Chen, Y.; Yang, L.; et al. Associations of General and Central Adiposity with Incident Diabetes in Chinese Men and Women. Diabetes Care 2018, 41, 494–502. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pang, Y.; Kartsonaki, C.; Guo, Y.; Chen, Y.; Yang, L.; Bian, Z.; Bragg, F.; Millwood, I.Y.; Yu, C.; Lv, J.; et al. Central adiposity in relation to risk of liver cancer in Chinese adults: A prospective study of 0.5 million people. Int. J. Cancer 2019, 145, 1245–1253. [Google Scholar] [CrossRef] [Green Version]
- Huai, P.; Liu, J.; Ye, X.; Li, W.Q. Association of Central Obesity With All Cause and Cause-Specific Mortality in US Adults: A Prospective Cohort Study. Front. Cardiovasc. Med. 2022, 9, 816144. [Google Scholar] [CrossRef]
- Xu, S.; Ming, J.; Jia, A.; Yu, X.; Cai, J.; Jing, C.; Liu, C.; Ji, Q. Normal weight obesity and the risk of diabetes in Chinese people: A 9-year population-based cohort study. Sci. Rep. 2021, 11, 6090. [Google Scholar] [CrossRef]
- Padwal, R.; Leslie, W.D.; Lix, L.M.; Majumdar, S.R. Relationship Among Body Fat Percentage, Body Mass Index, and All-Cause Mortality: A Cohort Study. Ann. Intern. Med. 2016, 164, 532–541. [Google Scholar] [CrossRef]
- Sahakyan, K.R.; Somers, V.K.; Rodriguez-Escudero, J.P.; Hodge, D.O.; Carter, R.E.; Sochor, O.; Coutinho, T.; Jensen, M.D.; Roger, V.L.; Singh, P.; et al. Normal-Weight Central Obesity: Implications for Total and Cardiovascular Mortality. Ann. Intern. Med. 2015, 163, 827–835. [Google Scholar] [CrossRef] [Green Version]
- Hamer, M.; O’Donovan, G.; Stensel, D.; Stamatakis, E. Normal-Weight Central Obesity and Risk for Mortality. Ann. Intern. Med. 2017, 166, 917–918. [Google Scholar] [CrossRef]
- Neeland, I.J.; Poirier, P.; Despres, J.P. Cardiovascular and Metabolic Heterogeneity of Obesity: Clinical Challenges and Implications for Management. Circulation 2018, 137, 1391–1406. [Google Scholar] [CrossRef] [PubMed]
- Xu, K.; Shi, L.; Zhang, B.; Mi, B.; Yang, J.; Sun, X.; Liao, X.; Dai, X.; Zeng, L.; Liu, X.; et al. Distinct metabolite profiles of adiposity indices and their relationships with habitual diet in young adults. Nutr. Metab. Cardiovasc. Dis. 2021, 31, 2122–2130. [Google Scholar] [CrossRef]
- Cirulli, E.T.; Guo, L.; Leon Swisher, C.; Shah, N.; Huang, L.; Napier, L.A.; Kirkness, E.F.; Spector, T.D.; Caskey, C.T.; Thorens, B.; et al. Profound Perturbation of the Metabolome in Obesity Is Associated with Health Risk. Cell Metab. 2019, 29, 488–500.e482. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nguyen, D.M.; El-Serag, H.B. The epidemiology of obesity. Gastroenterol. Clin. N. Am. 2010, 39, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Malik, V.S.; Hu, F.B. The role of sugar-sweetened beverages in the global epidemics of obesity and chronic diseases. Nat. Rev. Endocrinol. 2022, 18, 205–218. [Google Scholar] [CrossRef] [PubMed]
- Pan, X.F.; Wang, L.; Pan, A. Epidemiology and determinants of obesity in China. Lancet Diabetes Endocrinol. 2021, 9, 373–392. [Google Scholar] [CrossRef]
- Cui, L.; Chen, T.; Li, Z.; Yu, Z.; Liu, X.; Li, J.; Guo, Y.; Xu, D.; Wang, X. Association between dietary related factors and central obesity among married women: China Health and Nutrition Survey. Appetite 2022, 168, 105785. [Google Scholar] [CrossRef]
- Kakoschke, N.; Hawker, C.; Castine, B.; de Courten, B.; Verdejo-Garcia, A. Smartphone-based cognitive bias modification training improves healthy food choice in obesity: A pilot study. Eur. Eat. Disord. Rev. 2018, 26, 526–532. [Google Scholar] [CrossRef]
- Zhang, X.; Zhang, M.; Zhao, Z.; Huang, Z.; Deng, Q.; Li, Y.; Pan, A.; Li, C.; Chen, Z.; Zhou, M.; et al. Geographic Variation in Prevalence of Adult Obesity in China: Results From the 2013-2014 National Chronic Disease and Risk Factor Surveillance. Ann. Intern. Med. 2020, 172, 291–293. [Google Scholar] [CrossRef]
- Fitzgerald, M.A.; McCouch, S.R.; Hall, R.D. Not just a grain of rice: The quest for quality. Trends Plant Sci. 2009, 14, 133–139. [Google Scholar] [CrossRef]
- Chang, X.; DeFries, R.S.; Liu, L.; Davis, K. Understanding dietary and staple food transitions in China from multiple scales. PLoS ONE 2018, 13, e0195775. [Google Scholar] [CrossRef] [Green Version]
- You, W.; Henneberg, M. Cereal Crops Are not Created Equal: Wheat Consumption Associated with Obesity Prevalence Globally and Regionally. AIMS Public Health 2016, 3, 313–328. [Google Scholar] [CrossRef]
- Zhang, J.G.; Wang, Z.H.; Wang, H.J.; Du, W.W.; Su, C.; Zhang, J.; Jiang, H.R.; Zhai, F.Y.; Zhang, B. Dietary patterns and their associations with general obesity and abdominal obesity among young Chinese women. Eur. J. Clin. Nutr. 2015, 69, 1009–1014. [Google Scholar] [CrossRef] [PubMed]
- Yuan, Y.Q.; Li, F.; Meng, P.; You, J.; Wu, M.; Li, S.G.; Chen, B. Gender Difference on the Association between Dietary Patterns and Obesity in Chinese Middle-Aged and Elderly Populations. Nutrients 2016, 8, 448. [Google Scholar] [CrossRef] [PubMed]
- Shu, L.; Zheng, P.F.; Zhang, X.Y.; Si, C.J.; Yu, X.L.; Gao, W.; Zhang, L.; Liao, D. Association between Dietary Patterns and the Indicators of Obesity among Chinese: A Cross-Sectional Study. Nutrients 2015, 7, 7995–8009. [Google Scholar] [CrossRef]
- Zhang, J.; Wang, Z.; Du, W.; Huang, F.; Zhang, B.; Wang, H. Differential Association of Wheat and Rice Consumption With Overweight/Obesity in Chinese Adults: China Health and Nutrition Survey 1991–2015. Front. Nutr. 2022, 9, 808301. [Google Scholar] [CrossRef]
- Li, C.; Liu, Y.; Shi, G.; Mi, B.; Zeng, L.; Li, Q.; Shen, Y.; Zhao, Y.; Pei, L.; Kang, Y.; et al. Cohort Profile: Regional Ethnic Cohort Study in Northwest China. Int. J. Epidemiol. 2022, 51, e18–e26. [Google Scholar] [CrossRef] [PubMed]
- Qin, C.; Guo, Y.; Pei, P.; Du, H.; Yang, L.; Chen, Y.; Shen, X.; Shi, Z.; Qi, L.; Chen, J.; et al. The Relative Validity and Reproducibility of Food Frequency Questionnaires in the China Kadoorie Biobank Study. Nutrients 2022, 14, 794. [Google Scholar] [CrossRef]
- Romero-Corral, A.; Somers, V.K.; Sierra-Johnson, J.; Jensen, M.D.; Thomas, R.J.; Squires, R.W.; Allison, T.G.; Korinek, J.; Lopez-Jimenez, F. Diagnostic performance of body mass index to detect obesity in patients with coronary artery disease. Eur. Heart J. 2007, 28, 2087–2093. [Google Scholar] [CrossRef]
- Alberti, K.G.; Zimmet, P.; Shaw, J.; IDF Epidemiology Task Force Consensus Group. The metabolic syndrome—A new worldwide definition. Lancet 2005, 366, 1059–1062. [Google Scholar] [CrossRef]
- Mekary, R.A.; Willett, W.C.; Hu, F.B.; Ding, E.L. Isotemporal substitution paradigm for physical activity epidemiology and weight change. Am. J. Epidemiol. 2009, 170, 519–527. [Google Scholar] [CrossRef] [Green Version]
- Liu, X.; Lai, H.; Mi, B.; Qi, X.; Gan, W.; Du, H. Associations of Coarse Grain Intake with Undiagnosed Hypertension among Chinese Adults: Results from the China Kadoorie Biobank. Nutrients 2020, 12, 3814. [Google Scholar] [CrossRef]
- Zhen, S.; Ma, Y.; Zhao, Z.; Yang, X.; Wen, D. Dietary pattern is associated with obesity in Chinese children and adolescents: Data from China Health and Nutrition Survey (CHNS). Nutr. J. 2018, 17, 68. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lee, Y.H.; Chang, Y.C.; Ang, T.F.A.; Chiang, T.; Shelley, M.; Liu, C.T. Associations of staple food consumption and types of cooking oil with waist circumference and body mass index in older Chinese men and women: A panel analysis. Int. Health 2021, 13, 178–187. [Google Scholar] [CrossRef] [PubMed]
- Sarwar, H. The importance of cereals (Poaceae: Gramineae) nutrition in human health: A review. J. Cereals Oilseeds 2013, 4, 32–35. [Google Scholar] [CrossRef]
- Freire, R.H.; Fernandes, L.R.; Silva, R.B.; Coelho, B.S.; de Araujo, L.P.; Ribeiro, L.S.; Andrade, J.M.; Lima, P.M.; Araujo, R.S.; Santos, S.H.; et al. Wheat gluten intake increases weight gain and adiposity associated with reduced thermogenesis and energy expenditure in an animal model of obesity. Int. J. Obes. 2016, 40, 479–486. [Google Scholar] [CrossRef]
- Yang, L.; Chen, J.H.; Lv, J.; Wu, Q.; Xu, T.; Zhang, H.; Liu, Q.H.; Yang, H.K. Rice protein improves adiposity, body weight and reduces lipids level in rats through modification of triglyceride metabolism. Lipids Health Dis. 2012, 11, 24. [Google Scholar] [CrossRef] [Green Version]
- Yuexin, Y. Chinese Food Composition Table, 6th ed.; Peking University Medical Press: Beijing, China, 2020. [Google Scholar]
- Mendoza, J.A.; Drewnowski, A.; Christakis, D.A. Dietary energy density is associated with obesity and the metabolic syndrome in U.S. adults. Diabetes Care 2007, 30, 974–979. [Google Scholar] [CrossRef] [Green Version]
- Batres-Marquez, S.P.; Jensen, H.H.; Upton, J. Rice consumption in the United States: Recent evidence from food consumption surveys. J. Am. Diet. Assoc. 2009, 109, 1719–1727. [Google Scholar] [CrossRef]
- Zhang, N.; Ma, G. Noodles, traditionally and today. J. Ethn. Foods 2016, 3, 209–212. [Google Scholar] [CrossRef] [Green Version]
- Schlesinger, S.; Neuenschwander, M.; Schwedhelm, C.; Hoffmann, G.; Bechthold, A.; Boeing, H.; Schwingshackl, L. Food Groups and Risk of Overweight, Obesity, and Weight Gain: A Systematic Review and Dose-Response Meta-Analysis of Prospective Studies. Adv. Nutr. 2019, 10, 205–218. [Google Scholar] [CrossRef] [Green Version]
- Lee, M.; Kwon, D.Y.; Park, J. The impacts of the interaction of genetic variation, CYP11beta2 and NEDD4L, with sodium intake on pediatric obesity with gender difference: A 3-year panel study. Int. J. Obes. 2017, 41, 542–550. [Google Scholar] [CrossRef]
- Singh, P.; Covassin, N.; Marlatt, K.; Gadde, K.M.; Heymsfield, S.B. Obesity, Body Composition, and Sex Hormones: Implications for Cardiovascular Risk. Compr. Physiol. 2021, 12, 2949–2993. [Google Scholar] [CrossRef]
- Ma, S.; Xi, B.; Yang, L.; Sun, J.; Zhao, M.; Bovet, P. Trends in the prevalence of overweight, obesity, and abdominal obesity among Chinese adults between 1993 and 2015. Int. J. Obes. 2021, 45, 427–437. [Google Scholar] [CrossRef]
- Sun, X.; Liu, Z.; Du, T. Secular trends in the prevalence of abdominal obesity among Chinese adults with normal weight, 1993–2015. Sci. Rep. 2021, 11, 16404. [Google Scholar] [CrossRef] [PubMed]
- Jia, A.; Xu, S.; Xing, Y.; Zhang, W.; Yu, X.; Zhao, Y.; Ming, J.; Ji, Q. Prevalence and cardiometabolic risks of normal weight obesity in Chinese population: A nationwide study. Nutr. Metab. Cardiovasc. Dis. 2018, 28, 1045–1053. [Google Scholar] [CrossRef] [PubMed]
- Chen, X.; Duan, M.; Hou, R.; Zheng, M.; Li, H.; Singh, M.; Li, C.; Liu, K.; Zhang, F.; Yang, X.; et al. Prevalence of Abdominal Obesity in Chinese Middle-Aged and Older Adults with a Normal Body Mass Index and Its Association with Type 2 Diabetes Mellitus: A Nationally Representative Cohort Study from 2011 to 2018. Diabetes Metab. Syndr. Obes. 2021, 14, 4829–4841. [Google Scholar] [CrossRef] [PubMed]
| Men | Women | |||||||
|---|---|---|---|---|---|---|---|---|
| Wheat | Both | Rice | p | Wheat | Both | Rice | p | |
| N | 21,145 | 18,111 | 3340 | 32,273 | 25,737 | 5234 | ||
| Age (years, mean (SD)) | 53.90 (10.81) | 51.97 (13.02) | 49.02 (15.31) | <0.001 | 53.12 (9.71) | 52.07 (11.94) | 48.93 (14.77) | <0.001 |
| Ethnicity | ||||||||
| Han | 13,457 (63.64) | 15,073 (83.23) | 3202 (95.87) | <0.001 | 21,432 (66.41) | 21,008 (81.63) | 4994 (95.41) | <0.001 |
| Hui | 1768 (8.36) | 1766 (9.75) | 54 (1.62) | 2045 (6.34) | 2798 (10.87) | 114 (2.18) | ||
| Uygur | 4599 (21.75) | 864 (4.77) | 28 (0.84) | 7337 (22.73) | 1352 (5.25) | 62 (1.18) | ||
| Others | 1321 (6.25) | 408 (2.25) | 56 (1.68) | 1459 (4.52) | 579 (2.25) | 64 (1.22) | ||
| Education | ||||||||
| Primary school or less | 10,097 (47.75) | 5547 (30.63) | 866 (25.93) | <0.001 | 21,081 (65.32) | 11,493 (44.66) | 2103 (40.18) | <0.001 |
| Middle or high school | 9333 (44.14) | 7290 (40.25) | 965 (28.89) | 10,297 (31.91) | 9353 (36.34) | 1269 (24.25) | ||
| College or university | 1715 (8.11) | 5274 (29.12) | 1509 (45.18) | 895 (2.77) | 4891 (19.00) | 1862 (35.58) | ||
| Regular alcohol drinking a | 2773 (13.11) | 3615 (19.96) | 976 (29.22) | <0.001 | 165 (0.51) | 345 (1.34) | 251 (4.80) | <0.001 |
| Regular smokers b | 8677 (41.04) | 6570 (36.28) | 1257 (37.63) | <0.001 | 144 (0.45) | 144 (0.56) | 53 (1.01) | <0.001 |
| Physical activity c | ||||||||
| Low | 7487 (35.41) | 7547 (41.67) | 1041 (31.17) | <0.001 | 13,451 (41.68) | 11,812 (45.90) | 1821 (34.79) | <0.001 |
| Middle | 5173 (24.46) | 5467 (30.19) | 1262 (37.78) | 9074 (28.12) | 8020 (31.16) | 2005 (38.31) | ||
| High | 8485 (40.13) | 5097 (28.14) | 1037 (31.05) | 9748 (30.20) | 5905 (22.94) | 1408 (26.90) | ||
| Family income | ||||||||
| <20,000 yuan/year | 8765 (41.45) | 5309 (29.31) | 814 (24.37) | <0.001 | 14,285 (44.26) | 8156 (31.69) | 1295 (24.74) | <0.001 |
| 20,000–50,000 yuan/year | 7869 (37.21) | 5451 (30.10) | 696 (20.84) | 12,542 (38.86) | 8642 (33.58) | 1326 (25.33) | ||
| ≥50,000 yuan/year | 3985 (18.85) | 6285 (34.70) | 1471 (44.04) | 4684 (14.51) | 7131 (27.71) | 1939 (37.05) | ||
| Do not know | 526 (2.49) | 1066 (5.89) | 359 (10.75) | 762 (2.36) | 1808 (7.02) | 674 (12.88) | ||
| Province | ||||||||
| Shaanxi | 6626 (31.34) | 6927 (38.25) | 2597 (77.75) | <0.001 | 12,263 (38.00) | 9238 (35.89) | 3932 (75.12) | <0.001 |
| Gansu | 5062 (23.94) | 3242 (17.90) | 232 (6.95) | 6765 (20.96) | 4226 (16.42) | 252 (4.81) | ||
| Qinghai | 616 (2.91) | 281 (1.55) | 65(1.95) | 1025 (3.18) | 547 (2.13) | 142 (2.71) | ||
| Ningxia | 1074 (5.08) | 4552 (25.13) | 28 (0.84) | 1471 (4.56) | 6907 (26.84) | 73 (1.39) | ||
| Xinjiang | 7767 (36.73) | 3109 (17.17) | 418 (12.51) | 10,749 (33.31) | 4819 (18.72) | 835 (15.95) | ||
| Excessive body fat | 8833 (47.13) | 6545 (51.05) | 648 (34.27) | <0.001 | 15,181 (50.67) | 9598 (48.21) | 1347 (42.24) | <0.001 |
| BMI > 25 kg/m2 | 9102 (43.12) | 8461 (46.79) | 1369 (41.12) | <0.001 | 13,064 (40.55) | 9777 (38.03) | 1666 (31.89) | <0.001 |
| Central obesity | 8147 (40.28) | 6833 (43.54) | 887 (34.18) | <0.001 | 20,796 (65.65) | 14,732 (62.95) | 2285 (53.84) | <0.001 |
| Men | Women | |||
|---|---|---|---|---|
| OR (95%CI) | p | OR (95%CI) | p | |
| Excessive body fat | ||||
| Model 1 | 0.852 (0.787, 0.924) | <0.001 | 0.958 (0.901, 1.018) | 0.166 |
| Model 2 | 0.807 (0.743, 0.877) | <0.001 | 0.995 (0.935, 1.060) | 0.883 |
| Model 3 | 0.806 (0.743, 0.876) | <0.001 | 0.999 (0.939, 1.064) | 0.981 |
| Central obesity | ||||
| Model 1 | 1.118 (1.039, 1.203) | 0.003 | 0.840 (0.793, 0.890) | <0.001 |
| Model 2 | 0.982 (0.910, 1.059) | 0.634 | 0.916 (0.864, 0.973) | 0.004 |
| Model 3 | 0.975 (0.904, 1.052) | 0.518 | 0.918 (0.865, 0.975) | 0.005 |
| Participants with normal weight | ||||
| Normal weight obesity | ||||
| Model 1 | 0.640 (0.556, 0.737) | <0.001 | 0.844 (0.765, 0.931) | <0.001 |
| Model 2 | 0.635 (0.550, 0.733) | <0.001 | 0.837 (0.757, 0.926) | <0.001 |
| Model 3 | 0.635 (0.550, 0.733) | <0.001 | 0.843 (0.762, 0.932) | <0.001 |
| Normal weight central obesity | ||||
| Model 1 | 1.028 (0.895, 1.181) | 0.694 | 0.753 (0.698, 0.812) | <0.001 |
| Model 2 | 0.907 (0.785, 1.047) | 0.183 | 0.793 (0.734, 0.857) | <0.001 |
| Model 3 | 0.902 (0.780, 1.043) | 0.163 | 0.795 (0.736, 0.859) | <0.001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Xu, K.; Zhang, B.; Liu, Y.; Mi, B.; Wang, Y.; Shen, Y.; Shi, G.; Dang, S.; Liu, X.; Yan, H. Staple Food Preference and Obesity Phenotypes: The Regional Ethnic Cohort Study in Northwest China. Nutrients 2022, 14, 5243. https://doi.org/10.3390/nu14245243
Xu K, Zhang B, Liu Y, Mi B, Wang Y, Shen Y, Shi G, Dang S, Liu X, Yan H. Staple Food Preference and Obesity Phenotypes: The Regional Ethnic Cohort Study in Northwest China. Nutrients. 2022; 14(24):5243. https://doi.org/10.3390/nu14245243
Chicago/Turabian StyleXu, Kun, Binyan Zhang, Yezhou Liu, Baibing Mi, Yutong Wang, Yuefan Shen, Guoshuai Shi, Shaonong Dang, Xin Liu, and Hong Yan. 2022. "Staple Food Preference and Obesity Phenotypes: The Regional Ethnic Cohort Study in Northwest China" Nutrients 14, no. 24: 5243. https://doi.org/10.3390/nu14245243






