Abstract
This study aimed to examine the associations between parenting practices and child health-related behaviors, and the moderating role of child body weight status in children with intellectual disability (ID). A cross-sectional study was conducted among a sample of children with ID in Hong Kong; 440 participants were included in this study. All the variables investigated were collected from questionnaires, except body weight status, which was objectively measured. Logistic regression analysis was used to examine the associations between parenting practices and children’s unhealthy behaviors. Interaction items were added to investigate the moderation effect of child body weight status, adjusting for significant background characteristics. Results showed that the parenting practices of “restricting access to unhealthy food and sedentary behaviors (RA)” (OR range: 0.63–0.64) and “using food or sedentary behaviors as rewards (UR)” (OR range: 1.28–1.60) were significantly associated with some eating behaviors, but not with sedentary behaviors. Body weight status significantly moderated these associations. Only RA showed favorable effects on some eating behaviors in children with overweight and obesity (OR range: 0.17–0.28), whereas the effects of UR differed by body weight status. Future research should focus on developing educational interventions which encourage parents to use practices that are tailored towards children’s individual characteristics.
1. Introduction
Overweight and obese status in children and adolescents is an imminent crisis in public health and prevalence rates continue to rise. Previous research has established that children with intellectual disability (ID) are more vulnerable to overweight and obese status and developing unhealthy behaviors. Children with ID may face more developmental problems in processing information (e.g., cognitive impairment, communication disorders, limited mental functioning), and consequently they have difficulties in understanding and learning health knowledge and developing healthy behaviors [,,,]. In Hong Kong, there were 7700 children with ID studying in special schools in 2014 []. Our previous study reported that the combined prevalence of overweight and obese status in children with ID was 31.3% (vs. non-ID counterparts: 18.7–19.9%), and was associated with unhealthy behaviors (i.e., longer durations of sedentary behavior, higher consumption of sweetened drinks and of fried food) []. These unhealthy behavioral patterns develop during childhood and tend to persist into adulthood, which further results in greater risks of serious health issues (e.g., adult obesity, cardiovascular disease) [,]. Substantial evidence suggests that actions and attitudes from parents can have a significant impact on children’s health-related behaviors in childhood. These actions and attitudes can support children in developing healthy habits or can use specific parenting practices to control the availability and accessibility of healthy eating and exercise opportunities []. For children with ID, they may need more help to achieve healthy behaviors, and thus parents have significant roles in parenting a child with ID [,].
Parental practices, referring to parental actions or behaviors, are more content-specific to the domain of children’s eating and exercise compared with general parenting styles, which focus on the values, beliefs, and the emotional climate that parents convey to children as they develop. In addition, parenting practices may be more changeable and promising for establishing healthy habits in childhood [,]. Many studies have investigated the associations between parenting practices and child health-related behaviors; however, these produced conflicting results. For example, some experimental and longitudinal studies suggest that restricting access to unhealthy food was associated with a higher consumption of unhealthy food (e.g., sweetened drinks, snacks) and lower intakes of fruits and vegetables [,,,]. Contradictory findings were noted from cross-sectional studies, demonstrating that food restriction had favorable effects on children’s eating behaviors [,,,]. Moreover, other parenting practices (e.g., pressure to eat, monitoring) regarding eating were reported to be associated with both desirable (e.g., [,,]) and undesirable (e.g., [,]) eating behaviors. In addition, parenting practices regarding physical activity (PA) and sedentary behaviors presented mixed findings. Restricting and monitoring children’s amounts of screen watching were found to be associated with less sedentary behavior and increased PA [,,,], whereas some findings did not support these associations []. In addition, a variation in parenting practices measures across studies may be another contributory factor to inconsistent findings []. In the current study, parenting practices regarding children’s eating and exercise were measured in five domains: monitoring food intake and PA; restricting access to unhealthy food and sedentary behaviors; pressure to eat; reinforcement regarding eating and PA; and using food or sedentary behaviors as rewards.
The solutions to interpret conflicting findings on associations between parenting practices and child health-related behaviors may lie in the interactions between certain child aspects and parenting practices. Some child characteristics (e.g., body weight status) may moderate these associations []. For instance, a previous study identified the moderation effect of child body weight status on associations between restriction and dietary behaviors, presenting favorable effects for eating in children with normal weights, but not in children with overweight status []. A further study found that the effects of parenting practices on child health-related behaviors were not affected by child body weight status []. Evidence of the moderation effect of child body weight on these associations is still lacking. Children with ID are more vulnerable to unhealthy behaviors, overweight and obese status, and parenting practices seem more significant in establishing healthy habits compared with typically developing peers []. However, no research clarifies the moderating role of child body weight status of these associations in children with ID.
We previously investigated the associations between parenting practices and the risk of developing overweight and obese status in children with ID [], whereas the effects of parenting practices on child health-related behaviors and the moderating role of child body weight status are unknown. Based on previous findings and evidence, we developed this study to firstly examine the associations between parenting practices and child health-related behaviors, and secondly, to examine whether these associations would be moderated by child body weight status in children with ID.
2. Methods
2.1. Study Design and Participants
We conducted a cross-sectional study among students in special schools for children with mild (intelligence quotient: 50–69) and moderate (intelligence quotient: 35–49) ID in Hong Kong between June and November 2015 []. Sample size was estimated using a sample size formula for comparing proportions between a sample and the population [,]. Using a significance level of 5% and a power level of 80%, a sample size of 397 was estimated. Invitation letters were sent to all schools (n = 31), of which 12 schools consented to participate. We then invited all eligible students in the 12 schools who provided written informed consent forms signed by parents or guardians to participate in this study. The Research Ethics Committee of Hong Kong Baptist University ethically approved the study (Ref. No.: FRG1/13-14/067). A detailed description of the study methodology has been reported elsewhere []. Participants who met the following criteria participated in this study: (1) non-boarding students (i.e., living with parents); (2) respondents were parents; (3) valid data of parenting practices, child body weight status and health-related behaviors.
2.2. Measures
The participants’ background characteristics, health-related behaviors (including PA, sedentary behaviors, and eating habits) and related parenting practices were reported by their parents/guardians together using a self-administered questionnaire. Children’s body weight status was determined from a calibrated weighing scale and height from a stadiometer []. The questionnaire used was reliable for the study population, with an average Kappa of 0.71 obtained in a test–retest evaluation.
2.2.1. Background Characteristics of the Participants
The participants’ gender, age, ID level, and comorbidities (including Autism, attention deficit hyperactivity disorder (ADHD), Down syndrome, and epilepsy) were collected using the self-administered questionnaire. In addition, their parents’ education, occupation, marital status, reported height and weight, as well as the respondent parents’ age, were also obtained. Parental obesity was defined using a body mass index (BMI) cutoff point of 25 kg/m2 for Asian adults, where BMI was calculated using the self-reported height and weight [].
2.2.2. Parenting Practices
Parenting practices on children’s PA, sedentary behaviors and eating were collected using a Chinese version of a 17-item 5-point Likert-type scale []. It consists of the following five subscales: diet and PA monitoring (MO, six items; example question: “How often do you keep track of sweetened snacks (e.g., candy, ice cream, cake) that your child eats?”); restricting access to unhealthy food and sedentary behaviors (RA, four items; example question: “On weekdays, I limit the amount of TV or videos my child is watching.”); pressure to eat more (PE, three items; example question: “My child eats less than what he/she should eat if I do not intervene.”); reinforcement regarding children’s eating and PA (RF, two items; example question: “I will praise my child if he/she actively increases PA.”); and using food or sedentary behaviors as rewards (UR, two items; example question: “I would offer TV, video, or video games to my child as a reward for good behaviors.”). The scale has sound validity and reliability in both Chinese and Caucasian populations [,]. Supplementary Table S1 lists all items and ratings for the scale. The average score of each subscale (ranged from 1 to 5) was calculated for each participant, with a higher score indicating more frequent practices.
2.2.3. Children’s Health-Related Behaviors
Health-related behaviors included PA, sedentary behaviors, and eating habits. Children’s PA and sedentary behaviors in a typical week were subjectively measured with the Chinese version of the Global Physical Activity Questionnaire (GPAQ) [], modified for school children. For example, the context of performing PA at “work” was replaced by “school”, and fitted examples, respectively. Then, daily minutes of moderate- to vigorous-intensity PA (MVPA) and those of sedentary behaviors were calculated. Insufficient PA was defined with MVPA < 60 min/day [], while more sedentary behaviors were determined with 4 h/day as a cutoff point. Eating habits in a typical week were reported on a frequency of food consumption questionnaire, which was developed and validated for children in Hong Kong []. Lower fruit consumption (<2 servings/day), lower vegetable consumption (<3 servings/day), higher fried food consumption (≥once/day), higher sweetened drink consumption (≥once/day), higher snack consumption (≥twice/day) and breakfast skipping (≤6 times/week) were then defined.
2.2.4. Child Body Weight Status
Well-trained investigators measured children’s height (in cm) and weight (in kg) at school in the morning following a standard protocol. Overweight and obese status was defined based on international age- and gender-specific BMI cutoff points recommended by Cole et al. [].
2.3. Data Analysis
Categorical variables were described with counts and percentages, while continuous variables were presented with means and standard deviations (SDs). Independent sample t-tests and chi-square tests were employed to compare: (1) differences in all study variables between the original sample of all participants and the selected sub-sample of those fulfilling the selection criteria for this paper; (2) differences in parenting practices and health-related behaviors between children with overweight and obese status and children with non-overweight and obese status in this sub-sample. Univariate logistic regression was performed to examine relationships between children’s background characteristics and their behaviors. Multivariate logistic regression was fitted to examine the moderating role of child body weight status on parenting practices and unhealthy behaviors, adjusting for children’s age, gender, and the background characteristics with p < 0.10 used in the univariate analysis. Main effects along with the adjusted variables were forcedly entered in Block 1; interaction items between child body weight status and parenting practices were forward selected in Block 2, with p = 0.10 and p = 0.15 as entry and removal criteria, respectively []. The moderating effect of child body weight status was then identified if an interaction item reached significance (p < 0.05). Finally, those multivariate regression models with significant interaction items were further performed after stratification by child body weight status with the same adjusted variables as the previous step. Crude odds ratios (CORs) and adjusted odds ratios (AORs), with 95% confidence intervals (95% CIs), were derived from the univariate analysis and multivariate analysis, respectively. The SPSS Statistics version 26.0 was used to conduct all analyses and statistical significance was defined as p < 0.05.
3. Results
There were 558 participants in the original sample, of which 118 did not fulfill the selection criteria and were therefore excluded. The remaining 440 participants in the sub-sample were included in data analysis (Figure 1). There was no significant difference in any study variable between the original sample (n = 558) and the sub-sample (n = 440).
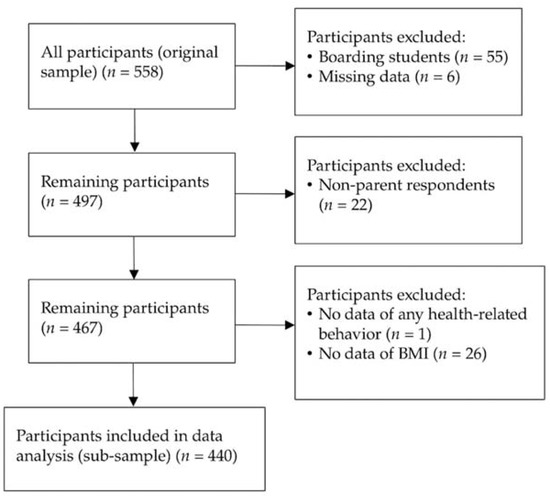
Figure 1.
Flow chart of participant selection.
Among the participants in the sub-sample, around two-thirds were male (69.8%); over half (54.8%) were aged from 6 to 12 years; 31.6% were overweight and obese. Table 1 lists all the background characteristics of the participants.

Table 1.
Background characteristics of the participants (n = 440).
Table 2 compared mean scores of parenting practices and the prevalence of unhealthy behaviors between the participants with and without overweight/obesity status. Significant differences were found in the PE subscale of parenting practices, as well as lower fruit, and higher fried food, consumption.

Table 2.
Distribution of scores of parenting practices (mean ± SD) and unhealthy behaviors (n and %) by child body weight status.
Results of the univariate analysis on the associations of the background characteristics with unhealthy behaviors are listed in Table 3. Female children were less likely to have higher snack consumption (COR: 0.54, 95% CI: 0.32–0.91, p < 0.05) but were more likely to skip breakfast (COR: 1.70, 95% CI: 1.04–2.76, p < 0.05). Adolescent children were less likely to have insufficient fruit (COR: 0.55, 95% CI: 0.35–0.85, p < 0.01) and higher snack consumption (COR: 0.51, 95% CI: 0.32–0.81, p < 0.01). In addition, children with overweight and obese status were more likely to have higher fried food consumption (COR: 1.98, 95% CI: 1.22–3.21, p < 0.01) but less likely to have insufficient fruit consumption (COR: 0.56, 95% CI: 0.36–0.88, p < 0.05). Children with moderate ID (compared to the mild level), those with autism, and those with ADHD are at an elevated risk for some unhealthy eating behaviors, while those with Down syndrome and epilepsy were at reduced risk for consuming less vegetables, more fried food, and more sweetened drinks. In terms of parental characteristics, significantly reduced risks for higher snack consumption were observed among parent respondents at older ages (compared to those aged < 40 years), and parents with higher education levels (compared to those with junior secondary and below) were also associated with lower risks for lower vegetable consumption and breakfast skipping, while other paternal occupations (compared to administrators and professionals), divorced/separated/widowed parents (compared to married/cohabiting), and maternal obesity (compared to non-obesity) were significantly associated with increased risks of some child unhealthy behavior variables.

Table 3.
Associations between background characteristics and children’s unhealthy behaviors (CORs, 95% CIs).
Table 4 presents the results of the multivariate logistic regression on associations of child body weight status and parenting practices with child unhealthy behaviors. In terms of main effects, children with overweight and obese status were more likely to engage in four out of seven unhealthy behaviors (including more sedentary behaviors, and higher fried food, higher sweetened drink, and higher snack consumption; AORs ranged from 1.51 to 1.96, p < 0.05), while they were at reduced risk for lower fruit consumption (AOR: 0.65, 95% CI: 0.43–0.99, p < 0.05). The RA subscale of parenting practices reduced the risks for higher fried food and sweetened drink consumption (AORs: 0.63 and 0.64, p < 0.05), while the UR subscale elevated the risk for higher fried food, higher sweetened drinks, and higher snack consumption, as well as breakfast skipping (AORs ranged from 1.28 to 1.60, p < 0.05). There were five interactions reaching significance, indicating that child body weight status moderated the associations between parenting practices and child behaviors, including RA with fried food, sweetened drinks, and breakfast skipping, and UR with vegetable intake and fried food (p < 0.05). The multivariate regression model for insufficient PA failed to build, as very few participants were available with sufficient MVPA (n = 34, Table 2).

Table 4.
Multivariate logistic regression on associations of child body weight status and parenting practices with child unhealthy behaviors (AORs, 95% CIs).
Table 5 further presents results of those multivariate models involving significant interactions after stratification by child body weight status. Among children with non-overweight and obese status, parenting practices were not significantly associated with any child behavior except lower vegetable consumption (AOR: 0.68, 95%CI: 0.44–0.98, p = 0.040). For those with overweight and obese status, the RA subscale significantly reduced risks for children’s higher fried food and higher sweetened drinks consumption, and breakfast skipping (AORs ranged from 0.17 to 0.28, p < 0.01), whilst the UR practices elevated the risk for higher fried food consumption (AOR: 2.50, 95% CI: 1.36–4.60, p < 0.05). These associations were not significant among children with non-overweight and obese status.

Table 5.
Associations between parenting practices and children’s unhealthy behaviors after stratification by child body weight status.
4. Discussion
The present study was conducted to investigate the associations between parenting practices and child health-related behaviors, including an examination of the moderating role of child body weight status in their associations in a sample of children with ID in Hong Kong. Findings suggest that children of parents who used the RA subscale of parenting practices were less likely to develop unhealthy eating behaviors and children were more likely to access to unhealthy food if their parents used UR subscale, compared with children of parents who less frequently used these parenting practices. In addition, results indicated that child body weight status moderated the associations between UR and RA subscales and four out of seven behaviors (i.e., lower vegetable, higher fried food, and higher sweetened drink consumptions, as well as breakfast skipping). Significant associations were observed in children with overweight and obese status after stratifying for body weight status, except that UR was found to lower the risk of insufficient vegetable intake in children with non-overweight and obese status.
Our study found that the mean score of each subscale of parenting practices was similar between children with non-overweight and obese status and those without, except for the PE subscale, where parents of children with non-overweight and obese status showed higher scores. This indicates that parents were more likely to encourage their children to eat more, which is comparable with previous findings in typically developing children [,,]. It is possible that parents of children with non-overweight and obese status have better knowledge of health and diet. As a result, they encourage children to consume more healthy food (e.g., vegetables), or eat food to maintain good weight status as a sign of health [,,]. Future research is needed to better understand the parental motivation of using the PE subscale, especially in children with ID.
The close relationships between these obesogenic eating and activity behaviors and risk of overweight and obese status in children with and without ID have been well-documented in previous research [,,]. Regarding the main effects of parenting practices, parents who used the RA subscale had children who consumed less fried food and less sweetened drinks; however, the use of UR made children more likely to consume fried food, sweetened drinks and snacks, and skip breakfast. Possible explanations may be that RA as a common adopted practice seems to be effective in reducing the opportunities to access unhealthy food. However, accumulating evidence showed that UR might promote overeating and interfere with children’s ability to self-regulate food consumption, leading to detrimental effects on eating behaviors []. There is little evidence examining these relationships in children with ID. In their counterparts, however, studies suggested conflicting results, with some studies confirming our results and some contradicting them [,,]. There are several explanations for these findings. One explanation may be that previous studies adopted a large variation of items and subscales to measure parenting practices, which may not be comparable with other studies. For example, a study by Arredondo et al. found that the use of control subscales by parents, combining both techniques of UR and PE subscales, was associated with undesirable eating behaviors []. Moreover, a study by Gubbels et al. found that parental restriction, which contained items of both RA and UR subscales used in our study, was not associated with any of the eating behaviors []. Thus, it is difficult to compare the isolated effect of specific items or subscales in those findings with the findings of our study. Further research is needed to confirm the effects of RA and UR practices. Interaction between children and parents might be another explanation, indicating that the effects of parenting practices on child behaviors depended on the characteristics of children (e.g., eating style) and parents (e.g., education level), which might further influence the associations observed []. For example, previous evidence has demonstrated that associations between restriction and undesirable eating behaviors were observed only in children with deviant eating styles, and monitoring was associated with desirable diet in children, except those with deviant eating styles [,].
In addition, no significant associations were observed regarding MO, PE, and RF subscales in children with ID. Previous studies have reported conflicting results in these three subscales in typically developing children (MO (e.g., [,,,]); PE (e.g., [,]); RF (e.g., [,])). For instance, Arredondo et al. identified that parental monitoring and reinforcement may have a favorable influence on children’s eating behaviors []. This might be explained by the fact that typically developing children may have better awareness and responsiveness compared with children with ID when parents monitor their behaviors (MO) and praise them for healthy behaviors (RF). Moreover, no conclusive results of the effects of PE were observed. A previous study reported that parents who used higher levels of PE subscale had detrimental effects on children’s eating behaviors (i.e., lower fruits and vegetables consumption, higher high-fat foods consumption) [,], while another study suggested that children who exposed higher levels of PE were less likely to consume high-fat foods []. Except for eating behaviors, our study found no associations between each subscale of parenting practices and sedentary behaviors. As too few cases were grouped into sufficient MVPA (6.2%), we failed to examine the effects of parenting practices on insufficient MVPA. Previous studies showed mixed results in typically developing children. In line with our study, no associations between parenting practices and children’s PA and sedentary behaviors were observed by Arredondo et al. []. In contrast, a cohort study illustrated that the restriction of sedentary behaviors by parents was related to increased sedentary behaviors and decreased PA []. Therefore, future research should put more effort on examining the effects of activity-related parenting practices to yield firm conclusions.
Findings indicated that child body weight status significantly moderated the associations between parenting practices and several unhealthy child behaviors. Parents using RA would reduce the risk of developing several unhealthy eating behaviors in children with overweight and obese status, but not in children with non-overweight and obese status. In addition, children with overweight and obese status were more likely to consume more fried food, whereas children with non-overweight and obese status were less likely to intake insufficient vegetables if parents were adopting UR. There are no conclusive results from previous studies. Associations between parental restriction and desirable eating behaviors were stronger in children with higher body weight, in agreement with previous studies [,]. By contrast, another study demonstrated that child body weight status did not moderate the associations []. Regarding the observed favorable effect of UR on insufficient vegetable intake among children with non-overweight and obese status, it is difficult to explain why UR played a protective role in this association based on the existing literature. Therefore, more studies are needed to confirm these associations.
Several limitations should be noted in the current study. First, this study provided hints of associations, but could not infer causation due to the nature of cross-sectional study design. Thus, whether the studied children’s behaviors are the consequences of specific parenting practices or vice versa could not be established. In addition, characteristics of children and parents, children’s behaviors, and parenting practices were self-reported, which may cause recall bias and reporting bias. Therefore, objectively measurements (e.g., wearing an Actigraph to measure PA and sedentary behaviors) are suggested in future studies. Third, parenting practice measures have varied widely across studies, making comparisons between previous studies and our study more difficult. There is no consensus about how to measure parenting practices in an appropriate way. Future research should be directed at the development and testing of comprehensive and valid parenting practices measures []. Finally, although the study sample of children with ID in Hong Kong may limit the generalizability to broader population of children, this special pediatric population who need more attention is understudied, and findings will add much-needed evidence to the limited knowledge base in this population.
Considering that children with ID are more vulnerable to unhealthy behaviors, future research on exploring effective parenting practices to promote healthy behaviors is urgently needed, which calls for more longitudinal studies to confirm causal inferences. If replicated and confirmed, findings from this study may add an important evidence base to the development of educational interventions and help understand the extent to which parenting practices can be modified through intervention. This will afford clinicians the opportunity to advise parents on how to monitor and reinforce child health-related behaviors [,,].
5. Conclusions
The current study found that child body weight status moderated the relationships between RA and UR parenting practices and some undesirable eating behaviors, but not sedentary behaviors. Significant effects of parenting practices were mostly observed in children with overweight and obese status, among whom appropriate restriction seems to have favorable effects on several eating behaviors, whereas the impact of UR practice depends on child body weight status. Overall, effective parenting practices worked particularly well for children with overweight and obese status, suggesting that parents should be encouraged to use RA and discouraged to use UR in children with overweight and obese status. Further research is needed to identify the effectiveness of parenting practices aimed at promoting healthy behaviors among children with and without ID. Then, research-based suggestions can be provided to parents regarding tailored practice for each individual child.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/nu14245206/s1. Table S1: Items and subscales of the scale of parenting practices.
Author Contributions
Conceptualization, Y.G.; methodology, Y.G.; software, Y.S.; validation, Y.S.; formal analysis, Y.S. and Y.G.; investigation, Y.G.; resources, R.S.; data curation, Y.S.; writing—original draft preparation, Y.S. and Y.G.; writing—review and editing, Y.S., Y.G., J.S.B., S.Y., A.W., X.O. and D.T.; supervision, Y.G. and J.S.B.; funding acquisition, Y.G. All authors have read and agreed to the published version of the manuscript.
Funding
This study has received funding support from the Health Care and Promotion Scheme under the Health and Medical Research Fund administered by the Food and Health Bureau of Hong Kong, Grant number: 01170068, and the Faculty Research Grant, Hong Kong Baptist University, Grant number: FRG1/13-14/067.
Institutional Review Board Statement
The study was ethically approved by the Research Ethics Committee of Hong Kong Baptist University (Ref. No.: FRG1/13-14/067).
Informed Consent Statement
Written consent from the parents or guardians of the participating children in this study was obtained.
Data Availability Statement
The data that support the findings of this study are available on request from the corresponding author [Y.G.]. The data are not publicly available due to restrictions (e.g., containing information that could compromise the privacy of research participants).
Acknowledgments
All authors would like to thank all the participants and their parents/guardians for their cooperation. Special thanks are given to the participating schools and teachers for their coordination and great support.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Hinckson, E.A.; Curtis, A. Measuring physical activity in children and youth living with intellectual disabilities: A sys-tematic review. Res. Dev. Disabil. 2013, 34, 72–86. [Google Scholar] [CrossRef] [PubMed]
- Rimmer, J.H.; Yamaki, K.; Lowry, B.M.D.; Wang, E.; Vogel, L.C. Obesity and obesity-related secondary conditions in adolescents with intellectual/developmental disabilities. J. Intellect. Disabil. Res. 2010, 54, 787–794. [Google Scholar] [CrossRef] [PubMed]
- Yuan, Y.Q.; Liu, Y.; Wang, M.J.; Hou, X.; Zhang, S.H.; Wang, X.L.; Han, Y.N.; Sang, P.; Bian, Y.; Roswal, G. Prevalence of overweight and obesity in children and adolescents with intellectual disabilities in China. J. Intellect. Disabil. Res. 2021, 65, 655–665. [Google Scholar] [CrossRef] [PubMed]
- Krahn, G.L.; Hammond, L.; Turner, A. A cascade of disparities: Health and health care access for people with intellectual disabilities. Ment. Retard. Dev. Disabil. Res. Rev. 2006, 12, 70–82. [Google Scholar] [CrossRef] [PubMed]
- Census and Statistics Department. Special Topics Report No.62, in Persons with Disabilities and Chronic Diseases; Census and Statistics Department: Hong Kong, China, 2014; pp. 249–250.
- Wang, J.; Gao, Y.; Kwok, H.H.; Huang, W.Y.; Li, S.; Li, L. Children with Intellectual Disability Are Vulnerable to Overweight and Obesity: A Cross-Sectional Study among Chinese Children. Child. Obes. 2018, 14, 316–326. [Google Scholar] [CrossRef] [PubMed]
- Yamaki, K.; Rimmer, J.H.; Lowry, B.D.; Vogel, L.C. Prevalence of obesity-related chronic health conditions in overweight adolescents with disabilities. Res. Dev. Disabil. 2011, 32, 280–288. [Google Scholar] [CrossRef] [PubMed]
- Mikulovic, J.; Vanhelst, J.; Salleron, J.; Marcellini, A.; Compte, R.; Fardy, P.S.; Bui-Xuan, G. Overweight in intellectually-disabled pop-ulation: Physical, behavioral and psychological characteristics. Res. Dev. Disabil. 2014, 35, 153–161. [Google Scholar] [CrossRef] [PubMed]
- Golan, M.; Crow, S. Parents are key players in the prevention and treatment of weight-related problems. Nutr Rev. 2004, 62, 39–50. [Google Scholar] [CrossRef] [PubMed]
- Beighton, C.; Wills, J. How parents describe the positive aspects of parenting their child who has intellectual disa-bilities: A systematic review and narrative synthesis. J. Appl. Res. Intellect. Disabil. 2019, 32, 1255–1279. [Google Scholar] [CrossRef] [PubMed]
- Boyd, M.J.; Iacono, T.; McDonald, R. The Perceptions of Fathers About Parenting a Child with Developmental Disability: A Scoping Review. J. Policy Pract. Intellect. Disabil. 2019, 16, 312–324. [Google Scholar] [CrossRef]
- Darling, N.; Steinberg, L. Parenting style as context: An integrative model. Psychol Bull. 1993, 113, 487. [Google Scholar] [CrossRef]
- Kiefner-Burmeister, A.; Hoffmann, D.; Zbur, S.; Musher-Eizenman, D. Implementation of parental feeding practices: Does parenting style matter? Public Health Nutr. 2016, 19, 2410–2414. [Google Scholar] [CrossRef] [PubMed]
- Loth, K.A. Associations Between Food Restriction and Pressure-to-Eat Parenting Practices and Dietary Intake in Children: A Selective Review of the Recent Literature. Curr. Nutr. Rep. 2016, 5, 61–67. [Google Scholar] [CrossRef]
- Faith, M.S.; Scanlon, K.S.; Birch, L.L.; Francis, L.A.; Sherry, B. Parent-Child Feeding Strategies and Their Relationships to Child Eating and Weight Status. Obes. Res. 2004, 12, 1711–1722. [Google Scholar] [CrossRef]
- Kiefner-Burmeister, A.E.; Hoffmann, D.A.; Meers, M.R.; Koball, A.M.; Musher-Eizenman, D.R. Food consumption by young children: A function of parental feeding goals and practices. Appetite 2014, 74, 6–11. [Google Scholar] [CrossRef]
- Peters, J.; Dollman, J.; Petkov, J.; Parletta, N. Associations between parenting styles and nutrition knowledge and 2–5-year-old children’s fruit, vegetable and non-core food consumption. Public Health Nutr. 2013, 16, 1979–1987. [Google Scholar] [CrossRef]
- Gevers, D.W.; van Assema, P.; Sleddens, E.F.; de Vries, N.K.; Kremers, S.P. Associations between general parenting, restrictive snacking rules, and adolescent’s snack intake. The roles of fathers and mothers and interparental congruence. Appetite 2015, 87, 184–191. [Google Scholar] [CrossRef]
- Villa, J.K.D.; Santos, T.S.S.; Ribeiro, A.Q.; e Silva, A.R.; Sant’Ana, L.F.D.R.; Pessoa, M.C. Dietary patterns of children and socioeconomical, behavioral and maternal determinants. Rev. Paul. Pediatr. 2015, 33, 302–309. [Google Scholar] [CrossRef]
- Wang, L.; Dalton, W.T.; Schetzina, K.E.; Fulton-Robinson, H.; Holt, N.; Ho, A.L.; Tudiver, F.; Wu, T. Home food environment, dietary intake, and weight among overweight and obese children in Southern Appalachia. South Med. J. 2013, 106, 550–557. [Google Scholar] [CrossRef]
- Van Der Horst, K.; Kremers, S.; Ferreira, I.; Singh, A.; Oenema, A.; Brug, J. Perceived parenting style and practices and the consumption of sugar-sweetened beverages by adolescents. Health Educ. Res. 2006, 22, 295–304. [Google Scholar] [CrossRef]
- Sleddens, E.F.; Kremers, S.P.; de Vries, N.K.; Thijs, C. Relationship between parental feeding styles and eating behaviors of Dutch children aged 6–7. Appetite 2010, 54, 30–36. [Google Scholar] [CrossRef] [PubMed]
- Arredondo, E.M.; Elder, J.P.; Ayala, G.X.; Campbell, N.; Baquero, B.; Duerksen, S. Is parenting style related to children’s healthy eating and physical activity in Latino families? Health Educ. Res. 2006, 21, 862–871. [Google Scholar] [CrossRef] [PubMed]
- Vereecken, C.; Rovner, A.; Maes, L. Associations of parenting styles, parental feeding practices and child characteristics with young children’s fruit and vegetable consumption. Appetite 2010, 55, 589–596. [Google Scholar] [CrossRef] [PubMed]
- Brown, K.A.; Ogden, J.; Vögele, C.; Gibson, E.L. The role of parental control practices in explaining children’s diet and BMI. Appetite 2008, 50, 252–259. [Google Scholar] [CrossRef] [PubMed]
- Salmon, J.; Timperio, A.; Telford, A.; Carver, A.; Crawford, D. Association of family environment with children’s television viewing and with low level of physical activity. Obes Res. 2005, 13, 1939–1951. [Google Scholar] [CrossRef] [PubMed]
- Spurrier, N.J.; Magarey, A.A.; Golley, R.; Curnow, F.; Sawyer, M.G. Relationships between the home environment and physical activity and dietary patterns of preschool children: A cross-sectional study. Int. J. Behav. Nutr. Phys. Act. 2008, 5, 31. [Google Scholar] [CrossRef]
- He, M.; Piché, L.; Beynon, C.; Harris, S. Screen-related sedentary behaviors: Children’s and parents’ attitudes, motivations, and practices. J. Nutr. Educ. Behav. 2010, 42, 17–25. [Google Scholar] [CrossRef]
- Ferreira, I.; van der Horst, K.; Wendel-Vos, W.; Kremers, S.; Van Lenthe, F.J.; Brug, J. Environmental correlates of physical activity in youth? A review and update. Obes. Rev. 2007, 8, 129–154. [Google Scholar] [CrossRef]
- Gubbels, J.S.; Kremers, S.P.J.; Stafleu, A.; de Vries, S.I.; Goldbohm, R.A.; Dagnelie, P.C.; de Vries, N.K.; van Buuren, S.; Thijs, C. Association between parenting practices and children’s dietary intake, activity behavior and development of body mass index: The KOALA Birth Cohort Study. Int. J. Behav. Nutr. Phys. Act. 2011, 8, 18. [Google Scholar] [CrossRef]
- Gubbels, J.S.; Kremers, S.P.; Stafleu, A.; Dagnelie, P.C.; Goldbohm, R.A.; de Vries, N.K.; Thijs, C. Diet-related restrictive parenting practices. Impact on dietary intake of 2-year-old children and interactions with child characteristics. Appetite 2009, 52, 423–429. [Google Scholar] [CrossRef]
- Min, J.; Wang, V.H.; Xue, H.; Mi, J.; Wang, Y. Maternal perception of child overweight status and its association with weight-related parenting practices, their children’s health behaviours and weight change in China. Public Health Nutr. 2017, 20, 2096–2103. [Google Scholar] [CrossRef] [PubMed]
- Su, H.; Cuskelly, M.; Gilmore, L.; Sullivan, K. Authoritative Parenting of Chinese Mothers of Children with and without Intellectual Disability. J. Child Fam. Stud. 2016, 26, 1173–1183. [Google Scholar] [CrossRef]
- WHO. Better Health, Better Lives: Children and Young People with Intellectual Disabilities and Their Families; The Case for Change; WHO: Geneva, Switzerland, 2010.
- Buehler, J.; Rothman, K.; Greenland, S. Modern Epidemiology; Lippencott-Raven: Philadelphia, PA, USA, 1998. [Google Scholar]
- Rowlands, A.V.; Eston, R.G.; Louie, L.; Ingledew, D.K.; Tong, K.K.; Fu, F.H. Physical Activity Levels of Hong Kong Chinese Children: Relationship with Body Fat. Pediatr. Exerc. Sci. 2002, 14, 286–296. [Google Scholar] [CrossRef]
- Pan, W.-H.; Yeh, W.-T. How to define obesity? Evidence-based multiple action points for public awareness, screening, and treatment: An extension of Asian-Pacific recommendations. Asia Pac. J. Clin. Nutr. 2008, 17, 370. [Google Scholar] [PubMed]
- Wen, X.; Hui, S.S.-C. Parenting Style as a Moderator of the Association Between Parenting Behaviors and the Weight Status of Adolescents. J. Early Adolesc. 2010, 32, 252–268. [Google Scholar] [CrossRef]
- WHO. Global Physical Activity Surveillance. 2014. Available online: https://www.who.int/teams/noncommunicable-diseases/surveillance/systems-tools/physical-activity-surveillance (accessed on 24 May 2022).
- WHO. WHO Guidelines on Physical Activity and Sedentary Behavior. 2020. Available online: https://www.who.int/publications/i/item/9789240015128 (accessed on 20 January 2022).
- A Qualitative Study on Dietary and Exercise Practice People in Hong Kong. 2005. Available online: http://www.ssrc.hku.hk/files/reports/health/grp-pmpdb-focus_group_e.pdf (accessed on 24 May 2022).
- Cole, T.J.; Bellizzi, M.C.; Flegal, K.M.; Dietz, W.H. Establishing a standard definition for child overweight and obesity worldwide: International survey. BMJ 2000, 320, 1240–1243. [Google Scholar] [CrossRef]
- Frazier, P.A.; Tix, A.P.; Barron, K.E. Testing moderator and mediator effects in counseling psychology research. J. Couns Psychol. 2004, 51, 115. [Google Scholar] [CrossRef]
- Scheffer, J. Dealing with missing data. Res. Lett. Inf. Math. Sci. 2002, 3, 153–160. [Google Scholar]
- Loth, K.A.; MacLehose, R.F.; Fulkerson, J.A.; Crow, S.; Neumark-Sztainer, D. Food-related parenting practices and ado-lescent weight status: A population-based study. Pediatrics 2013, 131, e1443–e1450. [Google Scholar] [CrossRef]
- Tschann, J.M.; Gregorich, S.E.; Penilla, C.; Pasch, L.A.; De Groat, C.L.; Flores, E.; Deardorff, J.; Greenspan, L.C.; Butte, N.F. Parental feeding practices in Mexican American families: Initial test of an expanded measure. Int. J. Behav. Nutr. Phys. Act. 2013, 10, 6. [Google Scholar] [CrossRef]
- Jansen, P.W.; Roza, S.J.; Jaddoe, V.W.; Mackenbach, J.; Raat, H.; Hofman, A.; Verhulst, F.C.; Tiemeier, H. Children’s eating behavior, feeding practices of parents and weight problems in early childhood: Results from the population-based Generation R Study. Int. J. Behav. Nutr. Phys. Act. 2012, 9, 130. [Google Scholar] [CrossRef] [PubMed]
- May, A.L.; Donohue, M.; Scanlon, K.S.; Sherry, B.; Dalenius, K.; Faulkner, P.; Birch, L.L. Child-feeding strategies are associated with maternal concern about children becoming overweight, but not children’s weight status. J. Am. Diet. Assoc. 2007, 107, 1167–1174. [Google Scholar] [CrossRef] [PubMed]
- Savage, J.S.; Fisher, J.O.; Birch, L.L. Parental Influence on Eating Behavior: Conception to Adolescence. J. Law Med. Ethic- 2007, 35, 22–34. [Google Scholar] [CrossRef] [PubMed]
- Sherry, B.; McDivitt, J.; Birch, L.L.; Cook, F.H.; Sanders, S.; Prish, J.L.; Francis, L.A.; Scanlon, K.S. Attitudes, practices, and concerns about child feeding and child weight status among socioeconomically diverse white, Hispanic, and African-American mothers. J. Am. Diet. Assoc. 2004, 104, 215–221. [Google Scholar] [CrossRef] [PubMed]
- Fang, K.; Mu, M.; Liu, K.; He, Y. Screen time and childhood overweight/obesity: A systematic review and meta-analysis. Child: Care Health Dev. 2019, 45, 744–753. [Google Scholar] [CrossRef]
- Liberali, R.; Kupek, E.; De Assis, M.A.A. Dietary Patterns and Childhood Obesity Risk: A Systematic Review. Child. Obes. 2020, 16, 70–85. [Google Scholar] [CrossRef]
- Olvera-Ezzell, N.; Power, T.G.; Cousins, J.H. Cousins, Maternal socialization of children’s eating habits: Strategies used by obese Mexican-American mothers. Child. Dev. 1990, 61, 395–400. [Google Scholar] [CrossRef]
- Moens, E.; Braet, C.; Soetens, B. Observation of family functioning at mealtime: A comparison between families of children with and without overweight. J. Pediatr. Psychol. 2007, 32, 52–63. [Google Scholar] [CrossRef]
- Vereecken, C.A.; Keukelier, E.; Maes, L. Influence of mother’s educational level on food parenting practices and food habits of young children. Appetite 2004, 43, 93–103. [Google Scholar] [CrossRef]
- Fisher, J.O.; Mitchell, D.C.; Smiciklas-Wright, H.; Birch, L.L. Parental influences on young girls’ fruit and vegetable, mi-cronutrient, and fat intakes. J. Am. Diet. Assoc. 2002, 102, 58–64. [Google Scholar] [CrossRef]
- Lee, H.; Keller, K.L. Children Who Are Pressured to Eat at Home Consume Fewer High-Fat Foods in Laboratory Test Meals. J. Acad. Nutr. Diet. 2012, 112, 271–275. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Stang, J.; Rehorst, J.; Golicic, M. Parental feeding practices and risk of childhood overweight in girls: Implications for dietetics practice. J. Am. Diet. Assoc. 2004, 104, 1076–1079. [Google Scholar] [CrossRef] [PubMed]
- Loth, K.; Fulkerson, J.A.; Neumark-Sztainer, D. Food-related parenting practices and child and adolescent weight and weight-related behaviors. Clin. Pract. 2014, 11, 207–220. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).