Adzuki Bean MY59 Extract Reduces Insulin Resistance and Hepatic Steatosis in High-Fat-Fed Mice via the Downregulation of Lipocalin-2
Abstract
1. Introduction
2. Materials and Methods
2.1. Plant Material
2.2. Preparation of the Adzuki Bean MY59 Extract (ABE)
2.3. Assay for α-Glucosidase Inhibitory Activity
2.4. Animals and Diet Model
2.5. Echo-MRI
2.6. Glucose Tolerance Test (GTT) and Insulin Tolerance Test (ITT)
2.7. Metabolic Parameters
2.8. Enzyme-Linked Immunosorbent Assay (ELISA)
2.9. Hepatic Triglyceride (TG) Colorimetric Assay
2.10. Hematoxylin and Eosin (H&E) Staining and NAFLD Activity Score Measurement
2.11. Nile Red Staining
2.12. Terminal Deoxynucleotidyl Transferase dUTP Nick End Labeling (TUNEL) Assay
2.13. Double Immunofluorescence
2.14. Protein Extraction
2.15. Western Blot Analysis
2.16. Statistical Analyses
3. Results
3.1. ABE Has a Strong α-Glucosidase Inhibitory Activity
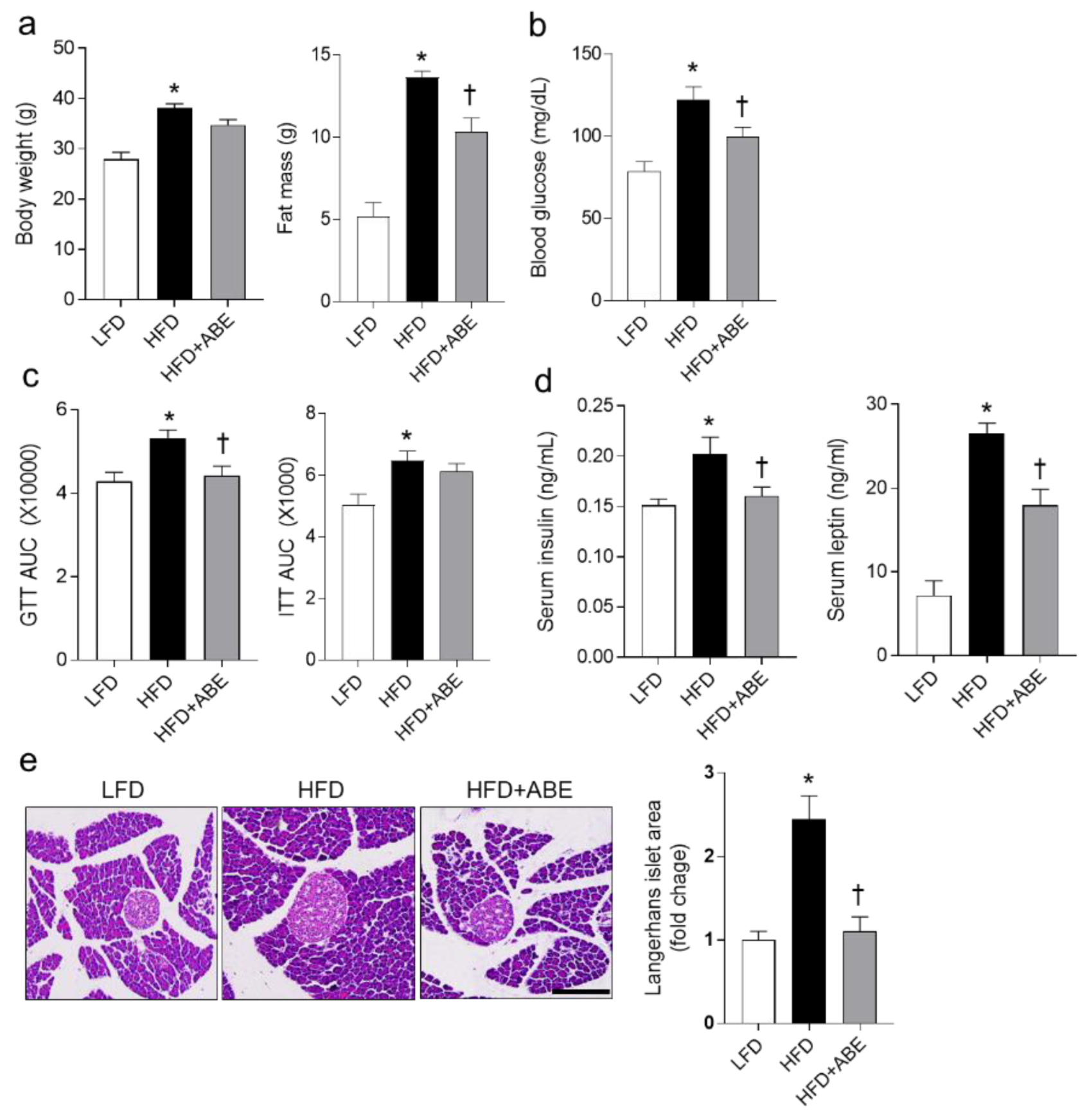
3.2. ABE Reduces Fat Mass and Insulin Resistance in HFD-Fed Mice
3.3. ABE Ameliorates Hepatic Steatosis in HFD-Fed Mice
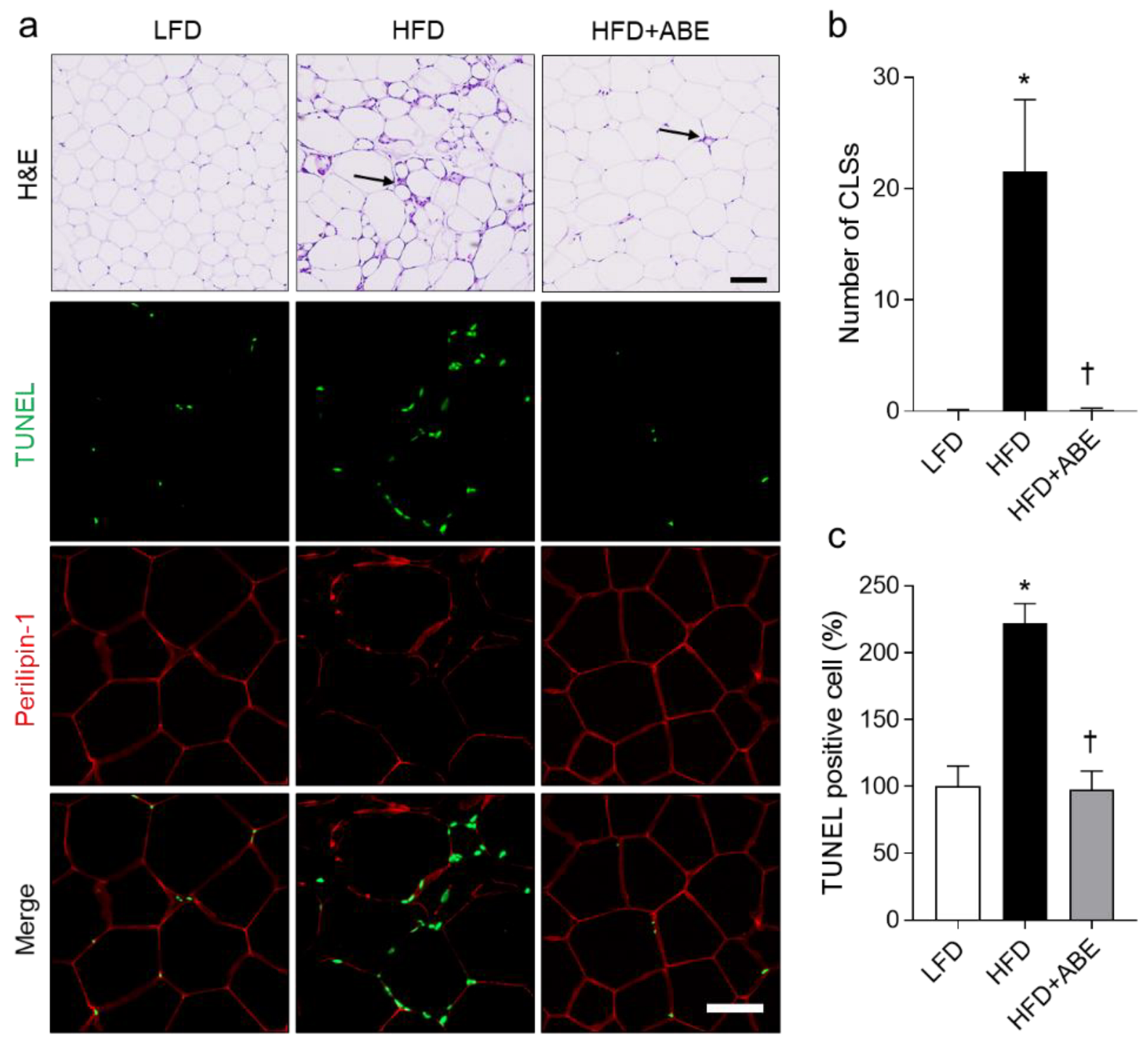
3.4. ABE Inhibits Apoptotic Adipocytes in HFD-Fed Mice
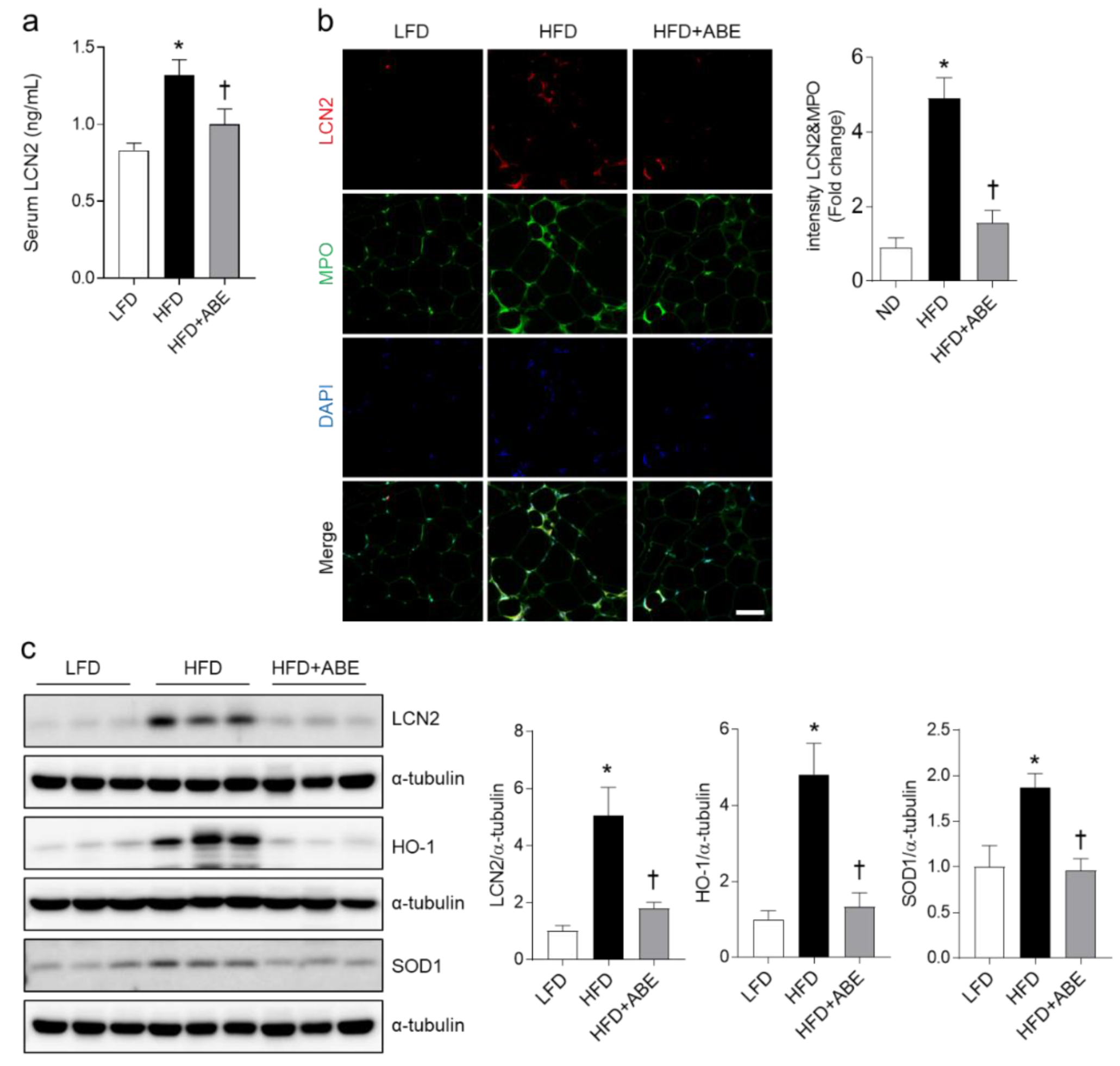
3.5. ABE Reduces LCN2, HO-1, and SOD1 Expressions in the Adipose Tissue of HFD-Fed Mice
3.6. ABE Reduces Hepatic Inflammation and Oxidative Stress in HFD-Fed Mice
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Blüher, M. Obesity: Global epidemiology and pathogenesis. Nat. Rev. Endocrinol. 2019, 15, 288–298. [Google Scholar] [CrossRef]
- Reilly, S.M.; Saltiel, A.R. Adapting to obesity with adipose tissue inflammation. Nat. Rev. Endocrinol. 2017, 13, 633–643. [Google Scholar] [CrossRef]
- Tilg, H.; Moschen, A.R. Adipocytokines: Mediators Linking Adipose Tissue, Inflammation and Immunity. Nat. Rev. Immunol. 2006, 6, 772–783. [Google Scholar] [CrossRef] [PubMed]
- Al Jaberi, S.; Cohen, A.; D’Souza, C.; Abdulrazzaq, Y.M.; Ojha, S.; Bastaki, S.; Adeghate, E.A. Lipocalin-2: Structure, function, distribution and role in metabolic disorders. Biomed. Pharmacother. 2021, 142, 112002. [Google Scholar] [CrossRef] [PubMed]
- Asimakopoulou, A.; Weiskirchen, S.; Weiskirchen, R. Lipocalin 2 (LCN2) Expression in Hepatic Malfunction and Therapy. Front. Physiol. 2016, 7, 430. [Google Scholar] [CrossRef]
- Wang, Y.; Lam, K.S.; Kraegen, E.W.; Sweeney, G.; Zhang, J.; Tso, A.W.; Chow, W.S.; Wat, N.M.; Xu, J.Y.; Hoo, R.L.; et al. Lipocalin-2 Is an Inflammatory Marker Closely Associated with Obesity, Insulin Resistance, and Hyperglycemia in Humans. Clin. Chem. 2007, 53, 34–41. [Google Scholar] [CrossRef] [PubMed]
- Ye, Z.; Wang, S.; Yang, Z.; He, M.; Zhang, S.; Zhang, W.; Wen, J.; Li, Q.; Huang, Y.; Wang, X.; et al. Serum lipocalin-2, cathepsin S and chemerin levels and nonalcoholic fatty liver disease. Mol. Biol. Rep. 2014, 41, 1317–1323. [Google Scholar] [CrossRef] [PubMed]
- Borkham-Kamphorst, E.; Drews, F.; Weiskirchen, R. Induction of Lipocalin-2 Expression in Acute and Chronic Experimental Liver Injury Moderated by Pro-Inflammatory Cytokines Interleukin-1β through Nuclear Factor-Kappab Activation. Liver Int. 2011, 31, 656–665. [Google Scholar] [CrossRef]
- Law, I.K.; Xu, A.; Lam, K.S.; Berger, T.; Mak, T.W.; Vanhoutte, P.M.; Liu, J.T.; Sweeney, G.; Zhou, M.; Yang, B.; et al. Lipocalin-2 Deficiency Attenuates Insulin Resistance Associated with Aging and Obesity. Diabetes 2010, 59, 872–882. [Google Scholar] [CrossRef]
- Ye, D.; Yang, K.; Zang, S.; Lin, Z.; Chau, H.T.; Wang, Y.; Wang, Y. Lipocalin-2 mediates non-alcoholic steatohepatitis by promoting neutrophil-macrophage crosstalk via the induction of CXCR2. J. Hepatol. 2016, 65, 988–997. [Google Scholar] [CrossRef]
- Fujino, R.S.; Tanaka, K.; Morimatsu, M.; Tamura, K.; Kogo, H.; Hara, T. Spermatogonial Cell-Mediated Activation of an Ikappabzeta-Independent Nuclear Factor-Kappab Pathway in Sertoli Cells Induces Transcription of the Lipocalin-2 Gene. Mol. Endocrinol. 2006, 20, 904–915. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Bu, D.X.; Hemdahl, A.L.; Gabrielsen, A.; Fuxe, J.; Zhu, C.; Eriksson, P.; Yan, Z.Q. Induction of Neutrophil Gelatinase-Associated Lipocalin in Vascular Injury via Activation of Nuclear Factor-Kappab. Am. J. Pathol. 2006, 169, 2245–2253. [Google Scholar] [CrossRef]
- Kitano-Okada, T.; Ito, A.; Koide, A.; Nakamura, Y.; Han, K.-H.; Shimada, K.; Sasaki, K.; Ohba, K.; Sibayama, S.; Fukushima, M. Anti-obesity role of adzuki bean extract containing polyphenols: In vivo and in vitro effects. J. Sci. Food Agric. 2012, 92, 2644–2651. [Google Scholar] [CrossRef] [PubMed]
- Baracho, N.C.D.V.; Monteiro, N.F.; Borges, M.G.; Arguelho, R.R.D.M. Effect of aqueous extract of the Vigna angularis in rats subjected to an experimental model of moderate chronic kidney disease. Acta Cir. Bras. 2016, 31, 527–532. [Google Scholar] [CrossRef] [PubMed]
- Durak, A.; Baraniak, B.; Jakubczyk, A.; Świeca, M. Biologically active peptides obtained by enzymatic hydrolysis of Adzuki bean seeds. Food Chem. 2013, 141, 2177–2183. [Google Scholar] [CrossRef] [PubMed]
- Jiang, Y.; Zeng, K.-W.; David, B.; Massiot, G. Constituents of Vigna angularis and their in vitro anti-inflammatory activity. Phytochemistry 2014, 107, 111–118. [Google Scholar] [CrossRef]
- Li, X.; Lu, Y.; Adams, G.G.; Zobel, H.; Ballance, S.; Wolf, B.; Harding, S.E. Characterisation of the molecular properties of scleroglucan as an alternative rigid rod molecule to xanthan gum for oropharyngeal dysphagia. Food Hydrocoll. 2020, 101, 105446. [Google Scholar] [CrossRef]
- Kim, S.; Hong, J.; Jeon, R.; Kim, H.-S. Adzuki bean ameliorates hepatic lipogenesis and proinflammatory mediator expression in mice fed a high-cholesterol and high-fat diet to induce nonalcoholic fatty liver disease. Nutr. Res. 2016, 36, 90–100. [Google Scholar] [CrossRef]
- Yao, Y.; Cheng, X.; Ren, G. Alpha-Glucosidase Inhibitory Activity of Protein-Rich Extracts from Extruded Adzuki Bean in Diabetic Kk-Ay Mice. Food Funct. 2014, 5, 966–971. [Google Scholar] [CrossRef]
- Itoh, T.; Kita, N.; Kurokawa, Y.; Kobayashi, M.; Horio, F.; Furuichi, Y. Suppressive Effect of a Hot Water Extract of Adzuki Beans (Vigna angularis) on Hyperglycemia after Sucrose Loading in Mice and Diabetic Rats. Biosci. Biotechnol. Biochem. 2004, 68, 2421–2426. [Google Scholar] [CrossRef]
- Ryu, H.W.; Lee, B.W.; Curtis-Long, M.J.; Jung, S.; Ryu, Y.B.; Lee, W.S.; Park, K.H. Polyphenols from Broussonetia Papyrifera Displaying Potent Alpha-Glucosidase Inhibition. J. Agric. Food Chem. 2010, 58, 202–208. [Google Scholar] [CrossRef] [PubMed]
- Jeon, B.T.; Heo, R.W.; Shin, H.J.; Yi, C.-O.; Lee, Y.H.; Joung, H.-N.; Jung, J.H.; Jung, J.; Kim, S.K.; Hahm, J.R.; et al. Attenuation by a Vigna nakashimae extract of nonalcoholic fatty liver disease in high-fat diet-fed mice. Biosci. Biotechnol. Biochem. 2014, 78, 482–489. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Jeon, B.T.; Jeong, E.A.; Shin, H.J.; Lee, Y.; Lee, D.H.; Kim, H.J.; Kang, S.S.; Cho, G.J.; Choi, W.S.; Roh, G.S. Resveratrol Attenuates Obesity-Associated Peripheral and Central Inflammation and Improves Memory Deficit in Mice Fed a High-Fat Diet. Diabetes 2012, 61, 1444–1454. [Google Scholar] [CrossRef] [PubMed]
- Kleiner, D.E.; Brunt, E.M.; Van Natta, M.; Behling, C.; Contos, M.J.; Cummings, O.W.; Ferrell, L.D.; Liu, Y.-C.; Torbenson, M.S.; Unalp-Arida, A.; et al. Design and validation of a histological scoring system for nonalcoholic fatty liver disease. Hepatology 2005, 41, 1313–1321. [Google Scholar] [CrossRef]
- Olefsky, J.M.; Glass, C.K. Macrophages, Inflammation, and Insulin Resistance. Annu. Rev. Physiol. 2010, 72, 219–246. [Google Scholar] [CrossRef]
- Talukdar, S.; Bandyopadhyay, G.; Li, D.; Xu, J.; McNelis, J.; Lu, M.; Li, P.; Yan, Q.; Zhu, Y.; Ofrecio, J.; et al. Neutrophils mediate insulin resistance in mice fed a high-fat diet through secreted elastase. Nat. Med. 2012, 18, 1407–1412. [Google Scholar] [CrossRef]
- Chan, Y.K.; Sung, H.K.; Sweeney, G. Iron metabolism and regulation by neutrophil gelatinase-associated lipocalin in cardiomyopathy. Clin. Sci. 2015, 129, 851–862. [Google Scholar] [CrossRef]
- Pereira, D.F.; Cazarolli, L.H.; Lavado, C.; Mengatto, V.; Figueiredo, M.S.; Guedes, A.; Pizzolatti, M.G.; Silva, F.R. Effects of Flavonoids on Alpha-Glucosidase Activity: Potential Targets for Glucose Homeostasis. Nutrition 2011, 27, 1161–1167. [Google Scholar] [CrossRef]
- Cazarolli, L.H.; Folador, P.; Pizzolatti, M.G.; Silva, F.R.M.B. Signaling pathways of kaempferol-3-neohesperidoside in glycogen synthesis in rat soleus muscle. Biochimie 2009, 91, 843–849. [Google Scholar] [CrossRef]
- Cinti, S.; Mitchell, G.; Barbatelli, G.; Murano, I.; Ceresi, E.; Faloia, E.; Wang, S.; Fortier, M.; Greenberg, A.S.; Obin, M.S. Adipocyte death defines macrophage localization and function in adipose tissue of obese mice and humans. J. Lipid Res. 2005, 46, 2347–2355. [Google Scholar] [CrossRef]
- Paschos, P.; Paletas, K. Non Alcoholic Fatty Liver Disease and Metabolic Syndrome. Hippokratia 2009, 13, 9–19. [Google Scholar] [PubMed]
- Farrell, G.C.; Larter, C.Z. Nonalcoholic fatty liver disease: From steatosis to cirrhosis. Hepatology 2006, 43, S99–S112. [Google Scholar] [CrossRef] [PubMed]
- Postic, C.; Girard, J. The role of the lipogenic pathway in the development of hepatic steatosis. Diabetes Metab. 2008, 34, 643–648. [Google Scholar] [CrossRef] [PubMed]
- Friedman, S.L.; Neuschwander-Tetri, B.A.; Rinella, M.; Sanyal, A.J. Mechanisms of NAFLD development and therapeutic strategies. Nat. Med. 2018, 24, 908–922. [Google Scholar] [CrossRef] [PubMed]
- Kjeldsen, L.; Johnsen, A.H.; Sengeløv, H.; Borregaard, N. Isolation and primary structure of NGAL, a novel protein associated with human neutrophil gelatinase. J. Biol. Chem. 1993, 268, 10425–10432. [Google Scholar] [CrossRef] [PubMed]
- Catalán, V.; Gómez-Ambrosi, J.; Rodríguez, A.; Ramírez, B.; Silva, C.; Rotellar, F.; Gil, M.J.; Cienfuegos, J.A.; Salvador, J.; Frühbeck, G. Increased adipose tissue expression of lipocalin-2 in obesity is related to inflammation and matrix metalloproteinase-2 and metalloproteinase-9 activities in humans. J. Mol. Med. 2009, 87, 803–813. [Google Scholar] [CrossRef]
- Zhao, P.; Elks, C.M.; Stephens, J.M. The Induction of Lipocalin-2 Protein Expression in Vivo and in Vitro. J. Biol. Chem. 2014, 289, 5960–5969. [Google Scholar] [CrossRef]
- Xu, M.J.; Feng, D.; Wu, H.; Wang, H.; Chan, Y.; Kolls, J.; Borregaard, N.; Porse, B.; Berger, T.; Mak, T.W.; et al. Liver Is the Major Source of Elevated Serum Lipocalin-2 Levels after Bacterial Infection or Partial Hepatectomy: A Critical Role for Il-6/Stat3. Hepatology 2015, 61, 692–702. [Google Scholar] [CrossRef]
- Kang, S.S.; Ren, Y.; Liu, C.-C.; Kurti, A.; Baker, K.E.; Bu, G.; Asmann, Y.; Fryer, J.D. Lipocalin-2 protects the brain during inflammatory conditions. Mol. Psychiatry 2018, 23, 344–350. [Google Scholar] [CrossRef]
- Zhou, L.; Wang, X.; Shao, L.; Yang, Y.; Shang, W.; Yuan, G.; Jiang, B.; Li, F.; Tang, J.; Jing, H.; et al. Berberine Acutely Inhibits Insulin Secretion from Beta-Cells through 3’,5’-Cyclic Adenosine 5’-Monophosphate Signaling Pathway. Endocrinology 2008, 149, 4510–4518. [Google Scholar] [CrossRef][Green Version]
- Li, L.; Li, R.; Zhu, R.; Chen, B.; Tian, Y.; Zhang, H.; Xia, B.; Jia, Q.; Wang, L.; Zhao, D.; et al. Salvianolic acid B prevents body weight gain and regulates gut microbiota and LPS/TLR4 signaling pathway in high-fat diet-induced obese mice. Food Funct. 2020, 11, 8743–8756. [Google Scholar] [CrossRef] [PubMed]
- Zhao, Q.; Hou, D.; Fu, Y.; Xue, Y.; Guan, X.; Shen, Q. Adzuki Bean Alleviates Obesity and Insulin Resistance Induced by a High-Fat Diet and Modulates Gut Microbiota in Mice. Nutrients 2021, 13, 3240. [Google Scholar] [CrossRef] [PubMed]


| α-Glucosidase Inhibitory Activity (IC50, μg/mL) | ||
|---|---|---|
| Bean Extracts and Compound | No Heat | Heat over 80 °C |
| Vigna nakashimae | 9.7 ± 0.38 | >500 |
| Chungju-pat | >500 | - |
| 1st adzuki bean MY59 extract | 6.4 ± 0.34 | >500 |
| 2nd adzuki bean MY59 extract | 1.9 ± 0.17 | 2.4 ± 0.16 |
| Acarbose | 140.5 ± 4.12 | - |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lee, J.; Lee, B.W.; Kim, K.E.; An, H.S.; Jeong, E.A.; Shin, H.J.; Song, S.B.; Roh, G.S. Adzuki Bean MY59 Extract Reduces Insulin Resistance and Hepatic Steatosis in High-Fat-Fed Mice via the Downregulation of Lipocalin-2. Nutrients 2022, 14, 5049. https://doi.org/10.3390/nu14235049
Lee J, Lee BW, Kim KE, An HS, Jeong EA, Shin HJ, Song SB, Roh GS. Adzuki Bean MY59 Extract Reduces Insulin Resistance and Hepatic Steatosis in High-Fat-Fed Mice via the Downregulation of Lipocalin-2. Nutrients. 2022; 14(23):5049. https://doi.org/10.3390/nu14235049
Chicago/Turabian StyleLee, Jaewoong, Byong Won Lee, Kyung Eun Kim, Hyeong Seok An, Eun Ae Jeong, Hyun Joo Shin, Seok Bo Song, and Gu Seob Roh. 2022. "Adzuki Bean MY59 Extract Reduces Insulin Resistance and Hepatic Steatosis in High-Fat-Fed Mice via the Downregulation of Lipocalin-2" Nutrients 14, no. 23: 5049. https://doi.org/10.3390/nu14235049
APA StyleLee, J., Lee, B. W., Kim, K. E., An, H. S., Jeong, E. A., Shin, H. J., Song, S. B., & Roh, G. S. (2022). Adzuki Bean MY59 Extract Reduces Insulin Resistance and Hepatic Steatosis in High-Fat-Fed Mice via the Downregulation of Lipocalin-2. Nutrients, 14(23), 5049. https://doi.org/10.3390/nu14235049





