Inflammatory Response in Oral Biofilm during Pregnancy: A Systematic Review
Abstract
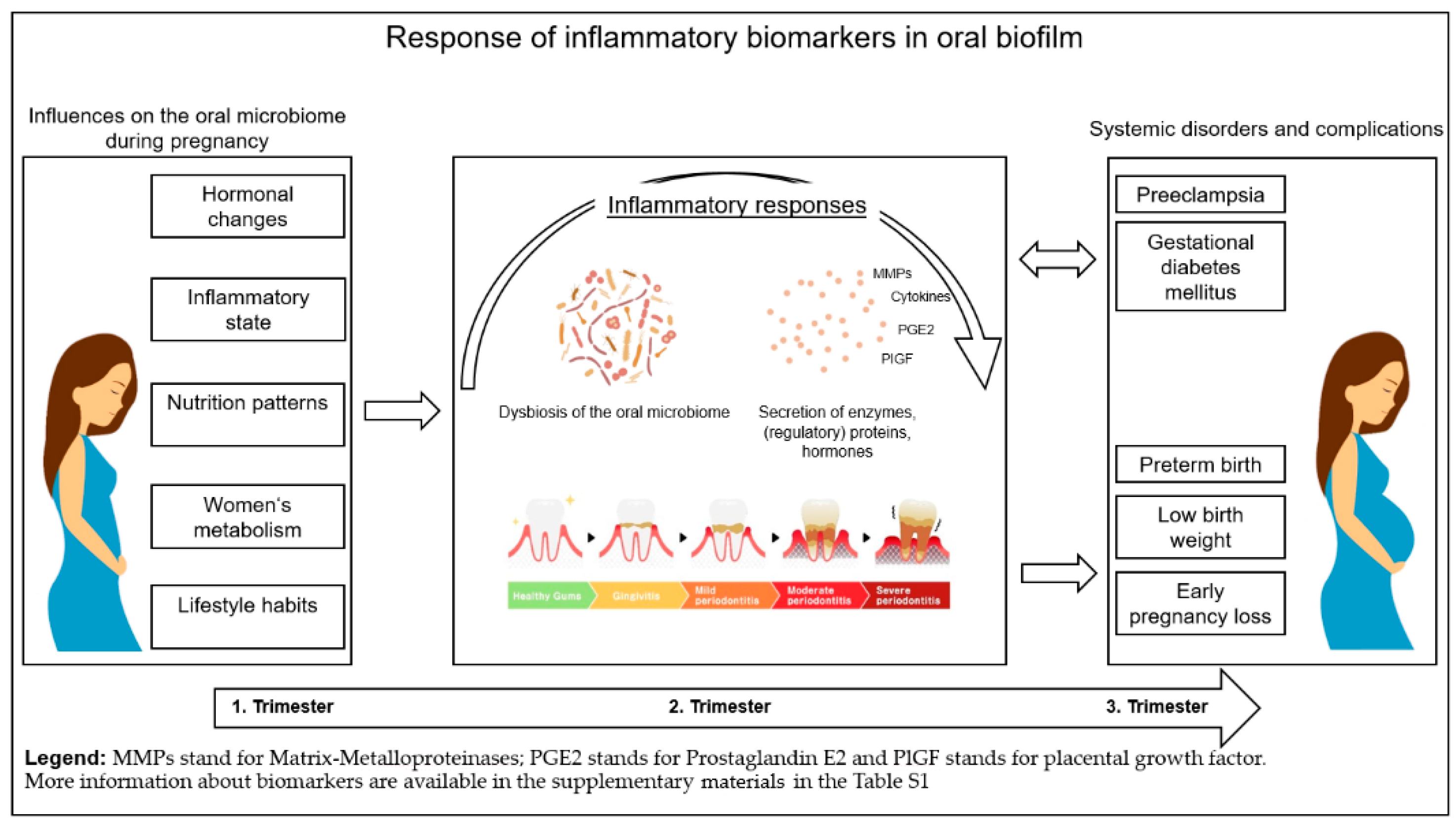
1. Introduction
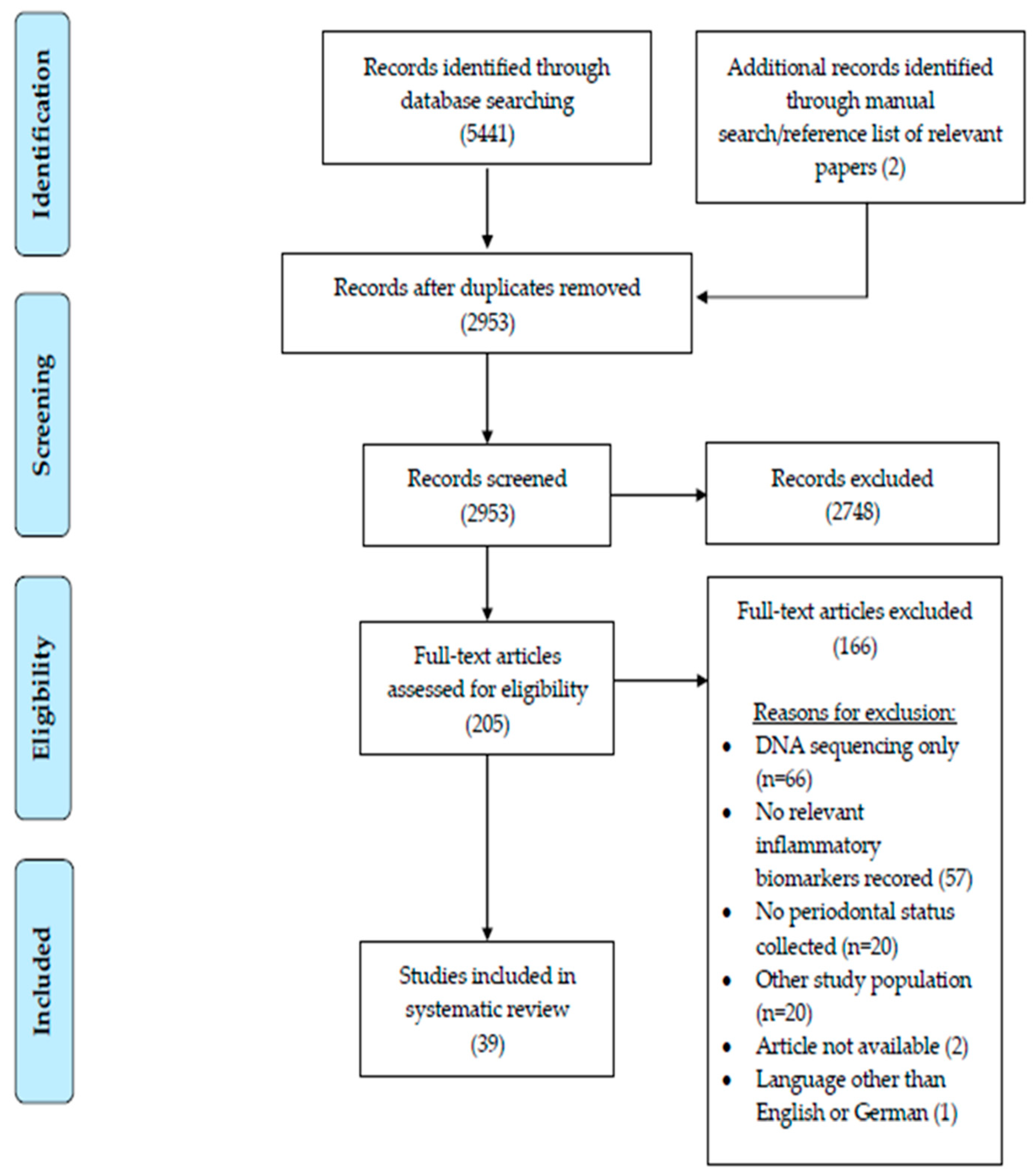
2. Materials and Methods
2.1. Literature Search Strategy
2.2. Inclusion and Exclusion Criteria
2.3. Data Extraction and Screening
2.4. Quality Assessment
3. Results
3.1. Study Characteristics
3.2. Association between Changes in Inflammatory Responses in the Oral Biofilm and Multisystemic Disorders or Health Conditions during Pregnancy (Table 1)
3.2.1. Gestational Diabetes Mellitus
3.2.2. Periodontitis
3.2.3. Preeclampsia
3.2.4. Obesity
3.2.5. Other Pregnancy Complications
| Author (year) | Country, Study Design | Investigated Groups (n of Subjects) | Measurement Interval | Periodontal Examination | Sample Collection | Sample Analysis | Evaluated Biomarkers | Main study Findings and Key Messages | Quality Assessment |
|---|---|---|---|---|---|---|---|---|---|
| Balan et al. (2021a) [26] | Singapore, cross-sectional study | Discovery dataset: Pregnant with gingivitis (10) Pregnant without gingivitis (10) Non-pregnant healthy controls (10) Validation dataset: Pregnant with gingivitis (16) Pregnant without gingivitis (16) Non-pregnant healthy controls (16) | One time-point: Week 21–28 GA; day 12–14 of menstrual cycle for non-pregnant women | PPD, BOP, PI, GBI | Saliva: Preparation: Subjects provided samples after thorough rinsing of the mouth and had refrained from food or drink for at least 1 h before collection Method: Passive drooling technique Processing: Protein precipitation using TCA at 4 °C Storage: Collected supernatants stored at −80 °C | iTRAQ, ELISA | Salivary cystatins, Protein profiles |
| Fair |
| Balan et al. (2021b) [41] | Singapore, cross-sectional case–control | Pregnant (20) Early pregnancy loss (10) Healthy pregnant (10) | One time-point | BOP, PI, DMFT | Saliva: Preparation: Subjects refrained from food or drink for at least one hour before sample collection Method: not specified Processing: Centrifuged at 2000 g for 15 min at 4 °C Storage: Supernatant was treated with TCA and stored at 4 °C | iTRAQ, LC-MS, ELISA | Protein profiles |
| Fair |
| Balan et al. (2022) [27] | Singapore, cross-sectional study | First sample set: Pregnant (24) Second sample set: Pregnant with gingivitis (10) Pregnant without gingivitis (10) Non-pregnant (10) | One time-point: Week 20–35 GA | BOP, PI, GBI | Saliva: Preparation: Subjects provided samples after thorough rinsing of the mouth and had refrained from food or drink for at least 1 h before collection Method: Spitting method Processing: Centrifuged at 2000 rpm for 15 min at 4 °C Storage: not specified | iTRAQ, ELISA, SEM | Protein profiles, NEs, MPOs, Nucleosomes | Salivary proteome shifts during pregnancy:
| Good |
| Canakci et al. (2007) [33] | Turkey, cross-sectional study | Pregnant women (40) Preeclampsia and periodontitis (10) Preeclampsia without periodontitis (10) Normotensive and periodontitis (10) Normotensive without periodontitis (10) | One time-point | PPD, CAL, BOP | GCF: Preparation? Method: Filter paper strips Site: Mesio-buccal and disto-palatal site on each tooth Collection time: 30 s. Processing: Eluted in phosphate-buffered saline Storage: Stored at −80 °C Saliva: Preparation: Subjects provided samples after an overnight fast Method: Expectorating into disposable tubes Processing: Centrifuged at 1000 rpm for for 10 min at 4 °C Storage: Supernatants stored at −80 °C | Assay for superoxide dismutase | GPx and superoxide dismutase, MDA, TAC | Preeclamptic women:
| Fair |
| Carta et al. (2004) [36] | Italy, cross-sectional study | Pregnant (92) Premature LBW (46) Uncomplicated pregnancy (46) | One time-point | PPD, BOP, PI, DMFT | GCF: Site: not specified Method: Paper strips Collection time: not specified Processing: not specified Storage: Stored in liquid nitrogen | ELISA | IL-1β, PGE2 |
| Poor |
| Chaparro et al. (2016) [32] | Chile, cross-sectional study | Pregnant (30) Preeclampsia (10) Normotensive (20) | One time-point | PPD, CAL, BOP | Saliva: Preparation: not specified Method: not specified Processing: Centrifuged at 1500× g for 10 min at 4 °C Storage: Collected supernatants stored in liquid nitrogen GCF: Method: Filter paper strips Site: not specified Collection time: 30 s. Processing: Eluted in 100 µL phosphate-buffered saline Storage: Stored in liquid nitrogen | ELISA, quantitative real-time poly-merase chain reaction | PLAP, PIGF, sflt1, EV-Cd63+ | Preeclamptic women:
| Fair |
| Chaparro et al. (2018) [22] | Chile, nested case–control with a prospective cohort | Pregnant (226) With GDM (14) Without GDM (212) | One time-point: Week 11–14 GA | PPD, CAL, BOP | Saliva: Preparation: not specified Method: not specified Processing: not specified Storage: Collected supernatants stored in liquid nitrogen GCF: Method: Filter paper strips Site: Four periodontal pockets (1 × quadrant) at the most affected periodontal site Collection time: 30 s. Processing: Eluted in 100 µL phosphate-buffered saline Storage: Stored in liquid nitrogen | ELISA | PlGF and sFlt-1 | Women with GDM:
| Good |
| Foratori et al. (2021) [34] | Brazil, prospective cohort study | Pregnant (50) Obese (25) Normal weight (25) | T1: Week 27–36 GA T2: 3 months postpartum | PPD, CAL BOP | Saliva: Preparation: Subjects were instructed to not consume any food or drink and to brush their teeth before the appointment Method: Subjects rinsed their mouths with 5 mL of deionized water. Afterwards, they were instructed to chew a piece of sterile rubber (0.5–1.0 cm of latex tube) attached to a 30 cm piece of dental floss. Stimulated saliva was collected in 5 min Processing: Saliva samples were lyophilized Storage: Collected supernatants stored at −80 °C | Luminex xMAP | IL-1β, TNF-α, leptin | Pregnant obese women:
| Fair |
| Gümüs et al. 2014 [21] | Turkey, cross-sectional study | Pregnant (167) GDM with gingivitis (71) GDM without gingivitis (390) Non-GDM with gingivitis (38) Non-GDM without gingivitis (28) | One time-point: Week 24–28 GA | PPD, CAL, BOP | Saliva: Preparation: Overnight fast during which subjects were requested not to drink (except water) or chew gum Method: Expectorating into polypropylene tubes Processing: Centrifuged at 13,000× g for 5 min at 4 °C Storage: Collected supernatants stored at −40 °C GCF: Method: Filter paper strips Site: Buccal aspects of two interproximal sites in single-rooted teeth Collection time: 30 s. Processing: Eluted in 1 mL phosphate-buffered saline Storage: Stored at −40 °C | ELISA | IL-6, IL-8, RANKL, OPG, APRIL, BAFF | Women with GDM:
Women with GDM + gingivitis:
| Fair |
| Machado et al. (2018) [28] | Portugal, cross-sectional study | Pregnant (44) Without periodontitis (15) Mild/moderate periodontitis (16) Severe periodontitis (13) | One-time-point | PPD, CAL | Saliva: Preparation: not specified Method: Passive drooling technique Processing: not specified Storage: Collected supernatants stored at −80 °C | ELISA | TNF-α, IL-6 |
| Fair |
| Mahilkar et al. (2021) [29] | India, case–control study | Pregnant (40) With periodontitis (20) Without periodontitis (20) | T1: 2nd trimester T2: postpartum | PPD, CAL, BOP, PI | Saliva: Preparation: Subjects were asked to refrain from eating or drinking for 2 h prior to saliva collection Method: Passive drooling technique Processing: Centrifuged at 2500 rpm for 10 min at 4 °C Storage: Collected supernatants stored at −80 °C | ELISA | IL-17 |
| Fair |
| Nikolic et al. (2020) [37] | Serbia, cross-sectional | Pregnant (112) Preterm birth (56) Term delivery (56) | One time-point:Within 48 h following delivery | PD, CAL, BOP, PI | Saliva: Preparation: No antiseptic mouth rinse was used prior to collection Method: not specified Processing: Centrifuged at 3500 rpm for 20 min at 4°C Storage: Two thirds of supernatant were stored at −70 °C, one third of supernatant was stored at −20 °C | ELISA | IL-1β PGE2 |
| Fair |
| Noack et al. (2005) [38] | Germany, cross-sectional study | Pregnant (101) Preterm LBW (59) Term delivery (42) | One time-point | PPD, CAL, BOP, PI | GCF: Method: Filter paper strips Site: Mesio-vesibular of each first or second molar Collection time: not specified Storage: Stored at −20 °C Elution/Processing: not specified | ELISA | IL-1β |
| Fair |
| Oettinger-Barak et al. (2005) [31] | Israel, cross-sectional study | Pregnant (30) Preeclampsia (15) Normotensive (15) | One time-point: 48 h before delivery | PPD, CAL, PI, GBI | GCF: Method: Periodontal paper strips Site: Periodontal sulci and pockets of the Ramfjord index teeth Collection time: 30 s. Processing: Insertion into an individual sterile tube containing 1.0 cc distilled water; Stand at room temperature for 30 min and shaken every 5 min to facilitate extraction of the sample Storage: Stored at −70 °C | ELISA | IL-1β, IL-6, TNF-α, PGE2 + | Preeclamptic women:
| Fair |
| Ozcaka et al. (2016) [20] | Turkey, cross-sectional study | Pregnant (161) With GDM (96) Without GDM (65) | One time-point: 24–28 weeks GA | PPD, BOP, PI | GCF: Method: Paper strips Site: not specified Collection time: not specified Processing: Eluted in 0.5 mL phosphate-buffered saline Storage: Stored at −40 °C | ELISA | IL10, TNF-α, IL-33 | Women with GDM:
| Fair |
| Stadelmann et al. (2015) [39] | Switzerland, prospective case–control study | Pregnant (56) Preterm premature rupture of membranes (PPROM) (32) Uncomplicated pregnancy (24) | T1: Week 20–35 GA T2: within 48 h after parturition T3: 4–6 weeks after parturition | PPD, CAL, BOP, PI | GCF: Method: Paper strips Site: Mesiobuccal site of each first molar in all quadrants Collection time: 15 s. Processing: Eluted in 750 μL phosphate-buffered saline containing proteinase inhibitor Storage: Stored at−80 °C | ELISA | IL-1β, CRP, IL-10, CRP | Women with PPROM:
| Fair |
| Surdacka et al. (2011) [23] | Poland, cross-sectional | Pregnant (63) Diabetes (30) Healthy (33) | One time-point: 1st trimester | PPD, CAL, API, GBI, SBI | Saliva:Preparation: Subjects were asked to rinse their mouths thoroughly with water. Saliva was collected at least 2 h after meal. Method: Passive drooling technique Processing: Centrifuged at 10,000× g for 5 min at 4 °C Storage: Supernatant stored at −30 °C | Elmman Test, Lowry method, TAS kit, Bioxytech assays, DuoSet Immunoassays | TP, SOD activity, Catalase activity, UA, Free -SH groups, TAC, MCP-1, GRO-α, IL-8, CSF, IL-6, IL-6sR, TNFα, TNF-R1, TNF-R2, IL-17, HGF, SDF-1, VEGF, sICAM-1 | Women with GDM:
| Poor |
| Yang et al. (2019) [30] | USA, cross-sectional pilot study | Pregnant (34) With Gingivitis (12) Without gingivitis (22) | One time-point: 3rd trimester | GBI | Saliva: Preparation: not specified Method: not specified Processing: not specified Storage: Collected supernatants stored at −80 °C | ELISA | IL-1β, MMP-8, CRP |
| Fair |
| Zalewska et al. (2013) [24] | Poland, cross-sectional study | Pregnant (50) With GDM (25) Without GDM (25) Non-pregnant (25) | One time-point | GBI, DMFT | Saliva: Preparation: Subjects were asked to refrain from food and beverages, except water, for one hour before saliva collection Method: Spitting method Processing: Centrifuged at 3000× g for 20 min at 4 °C Storage: Supernatant stored at −80 °C | Marciniak method, Zwierz method, Lowrys’s method, Spectrophotometry | HEX, GAL, MAN, FUC, GLU | Women with GDM:
| Fair |
| Zambon et al. (2018) [35] | Italy, cross-sectional study | Pregnant (62) Normal weight (27) Obese (35) | One time-point: 3rd trimester | PPD, CAL, BOP, PI | Saliva: Preparation: not specified Method: Passive drooling technique Processing: Centrifuged at 4000× g for 10 min at 4 °C Storage: not specified | Antioxidant Assay kit, ELISA | s-TAC, s-CRP | Pregnant obese women:
| Fair |
| Zygula et al. (2019) [25] | Poland, cross-sectional study | Pregnant (89) With GDM (59) Without GDM (30) | One time-point | PPD, CAL, PI, GBI | Saliva: Preparation: Subjects fasted overnight (at least 6 h) Method: Spitting method Processing: Centrifuged at 10,000× g for 10 min Storage: Supernatant stored at −80 °C | Fluorometric method for ALDH, ORAC-fluorescein fluorometric assay, MDA Assay | ALDH, ORAC, MDA | Women with GDM:
| Fair |
| Zygula et al. (2020) [40] | Poland, cross-sectional study | Pregnant (104) Pregnancy-induced hypertension (PIH) (27) Intrauterine growth restriction (IUGR) (30) Uncomplicated pregnancy (47) | One time-point | PPD, CAL, PI, GBI | Saliva: Preparation: Subjects fasted overnight (at least 6 h) Method: Spitting method Processing: centrifuged at 10,000× g for 10 min Storage: Supernatant stored at −80 °C | Fluorometric method for ALDH, ORAC-fluorescein fluorometric assay, MDA Assay | ALDH, ORAC, MDA | IUGR group:
| Fair |
3.3. Differences in Inflammatory Responses in Oral Biofilm between Healthy Pregnant and Non-Pregnant Women
| Author (year) | Country, Study Design | Investigated Groups (n of Subjects) | Measurement Interval | Periodontal Examination | Sample Collection | Sample Analysis | Evaluated Biomarker | Main study Findings and Key Messages | Quality Assessment |
|---|---|---|---|---|---|---|---|---|---|
| Ehlers et al. (2013) [45] | Germany, cross-sectional study | Pregnant (20) Non-pregnant (20) | One time-point | PPD, CAL, SBI, PI | GCF: Method: Filter paper strips Site: Gingival sulcus of all four first molars Collection time: 30 s. Processing: Eluted in 800 μL of HEPES buffer Storage: not specified | DentoAnalyzer | aMMP-8 |
| Fair |
| Gümüs et al. (2015) [49] | Turkey, case–control study | Pregnant (115) Non-pregnant (72) | T1: 1st or 2nd trimester T2: 6 months postpartum | PPD, CAL, BOP, PI | Saliva: Preparation: Subjects were asked to fast overnight and to rinse their mouth with tap water prior to sample collection Method: Expectoration into polypropylene tubes for 5 min Processing: Centrifuged at 10,000× g for 15 min at −4 °C Storage: Collected supernatants stored at −80 °C | ELISA, GPx assay kit, TBARS Parameter Assay Kit | GPx activity, 8-OHdG, TBARS | Oxidative stress markers:
Pregnant women:
| Good |
| Gürsoy et al. (2010a) [46] | Finland, prospective cohort study | Pregnant (30) Non-pregnant (24) | T1: Week 12 GA T2: Week 14 GA T3: Week 25–27 or Week 34–38 GA T4: 4–6 Weeks postpartum T5: after breastfeeding | PPD, CAL, BOP, PI | GCF: Method: Filter paper strips Site: Mesiobuccal sites of all first molars or, if missing, second molars Collection time: 30 s. Processing: Eluted in 75 mL of 50 mM Tris-HCl (pH 7.8), including 0.2 M NaCl and 1 mM CaCl2 Storage: Stored at −20 °C | ELISA | MMP-8, elastase, MPO, TIMP-1 | Pregnant women:
| Good |
| Gürsoy et al. (2010b) [47] | Finland, prospective cohort study | Pregnant (30) Non-pregnant (24) | Pregnant: T1: Week 12–14 GA T2: Week 25–27 GA T3: Week 34–38 GA T4: 4–6 weeks postpartum T5: After lactation Non-pregnant: T1-T3: once per subsequent month | PPD, CAL, BOP, PI | Saliva: Preparation: not specified Method: Paraffin-stimulated saliva was collected by expectoration for 5 min Processing: salivary samples were diluted in assay buffer for 1 h Storage: Collected supernatants stored at −20 °C | Immunofluorometric assay, Gelatin zymography, ELISA | MMP8, MMP2, MMP9, MPO, TIMP1 | MMP-8 concentrations:
| Good |
| Gürsoy et al. (2016) [50] | Finland, prospective cohort study | Pregnant (30) Non-pregnant (24) | Pregnant: T1: Week 12–14 GA T2: Week 25–27 GA T3: Week 34–38 GA T4: 4–6 weeks postpartum T5: After lactation Non-pregnant: T1: 1st month T2: 2nd month T3: 3rd month | BOP, PI | Saliva: Preparation:not specified Method: Paraffin-stimulated saliva was collected by expectoration for 5 min Processing: not specified Storage: Collected supernatants stored at −70 °C | ELISA | 17β-estradiol, Progesteron, Defensins (hBD-1, -2, -3, HNP-1) |
| Good |
| Öztürk et al. (2010) [48] | Turkey, longitudinal study | Pregnant (11)Non-pregnant (12) | T1: 1st trimester T2: 2nd trimester T3: 3rd trimester T4: 6–8 weeks postpartum | BOP, PI | Saliva: Preparation: Two hours prior to saliva collection, all subjects were instructed to eat a standard breakfast and to brush their teeth immediately afterwards Method: Passive drooling technique Processing: Centrifuged at 4 °C Storage: Collected supernatants stored at −24 °C | Ledwozyw’s method for LPO; Warren’s method for TSA; Lowry method for Total protein | LPO, TSA, Total protein level | LPO levels:
| Fair |
| Wu et al. (2016) [42] | China, Prospective case–control study | Pregnant (30) Non-pregnant (20) | Pregnant T1: Weeks 12–14 GA T2: Weeks 23–25 GA T3: Weeks 33–36 GA Non-pregnant T1: 1st month T2: 2nd month | PPD, CAL, BOP, PI, GBI | GCF: Method: Filter paper strips Site: Mesiobuccal sites of upper premolars Collection time: 30 s. Processing: Eluted in 200 μL phosphate-buffered saline and 2 μL of phenylmethanesulfonyl fluoride (20 mM) Storage: Stored at −70 °C | ELISA | IL-1β, TNF-α |
| Good |
| Yarkac et al. (2018) [43] | Turkey, case–control study with a periodontal therapy intervention | Pregnant (30) Non-pregnant (30) | T1: baseline T2: 3 weeks after periodontal treatment | PI, GI, PPD, CAL | Saliva: Preparation: Subjects were requested not to eat, brush, drink, or chew gum within 90 min of sample collection Method: Spitting into polypropylene tubes Processing: Centrifuged at 3220 rpm for 10 min Storage: Supernatants stored at −20 °C GCF: Method: Filter paper strips Site: Mesiobuccal sulcus of teeth in the anterior region Collection time: 30 s. Processing: not specified Storage: Stored at −20 °C | ELISA | IL-1β, IL-10 | Periodontal therapy:
| Strong |
| Yarkac et al. (2021) [44] | Turkey, case–control study with a periodontal therapy intervention | Pregnant (30) Non-pregnant (30) | T1: baseline T2: 3 weeks after periodontal treatment | PPD, CAL, PI, GBI | Saliva: Preparation: Subjects were requested not to eat, brush, drink, or chew gum within 90 min Method: Spitting into polypropylene tubes Processing: Centrifuged at 3220 rpm for 10 min Storage: Collected supernatants stored at −20 °C GCF: Method: Periopaper strips Site: Mesiobuccal sulcus of randomly selected single-rooted upper anterior teeth with gingivitis Collection time: 30 s. Processing: Eluted in 200 µL phosphate-buffered saline Storage: Stored at −20 °C | ELISA | IL-6, IL-10 | Periodontal therapy:
| Strong |
3.4. Differences in the Response of Inflammatory Biomarkers in Oral Biofilm between Pregnancy Stages
| Author (year) | Country, Study Design | Investigated Groups (n of Subjects) | Measurement Interval | Periodontal Examination | Sample Collection | Sample Analysis | Evaluated Biomarker | Main study Findings and Key Messages | Quality Assessment |
|---|---|---|---|---|---|---|---|---|---|
| Bieri (2013) [51] | Switzerland, prospective consecutive case series | Pregnant (19) | T1: Week 12 GA T2: 4–6 weeks postpartum | PPD, CAL, BOP | GCF: Method: Endodontic paper points Site: Mesiobuccal aspects of all first molars Collection time: 15 s. Processing: Eluted in a lysis buffer and ethanol Storage: Stored at −79 °C | Quantitative rtPCR | IL-1α, IL-1β, IL-8, TNF-α |
| Fair |
| Kaur et al. (2014) [54] | USA, clinical trial Intervention: Intensive one-on-one oral hygiene counselling and non-surgical periodontal therapy | Pregnant women with gingivitis (120) | T1: baseline T2: Week 4 GA (only PA examination) T3: Week 8 GA | PPD, CAL, BOP, PI, GI | GCF: Method: Filter paper strips Site: Gingival sulcus of two randomly selected sites on non-adjacent teeth Collection time: 30 s. Processing: Eluted in 100 μL phosphate-buffered saline Storage: Stored at −70 °C | ELISA | IL-1β, IL-6, TNF-α | Periodontal intervention:
| Weak |
| Gürsoy et al. (2014) [53] | Finland, longitudinal cohort study | Pregnant (30) | T1: Week 12–14 GA T2: Week 25–27 GA T3: Week 34–38 GA T4: 4–6 weeks postpartum T5: After lactation | PPD, CAL, BOP | Saliva: Preparation: not specified Method: Paraffin-stimulated saliva was collected by expectoration for 5 min Processing: Salivary samples were diluted in assay buffer for 1 h Storage: Supernatants stored at −20 °C | Immunofluorometric assay, Gelatin zymography, ELISA | IL-1β, IL-8, MMP8, MMP2, MMP9, MPO TIMP1, estradiol |
| Fair |
| Lasisi et al. (2018) [52] | Nigeria, longitudinal cohort study | Pregnant (47) | T1: 2nd or 3rd trimester T2: 3 months postpartum | PPD, CAL, BOP, PI | Saliva: Preparation: not specified Method: Spitting into a graduated universal bottle for a period of 10 min Processing: not specified Storage: Supernatants stored at −20 °C | ELISA | TNF-α, IFN-γ, IL-1β, Lactoferin, Lysozyme, β defensin-1 |
| Fair |
| Offen-bacher et al. (2006) [56] | USA, randomized two-arm clinical trial Intervention: Non-surgical periodontal therapy and oral health instructions on the use of a power toothbrush Control: Supragingival debridement and a manual toothbrush with no instructions | Pregnant (67) Intervention (35) Controls (32) | T1: baseline T2: 4–6 Weeks GA (intervention group) T3: 6 weeks postpartum (control group) | PPD, CAL, BOP, PI, GBI | GCF: Method: Filter paper strips Site: Mesio- and distobuccal sites from the two most posterior teeth in all four quadrants, excluding third molars Collection time: not specified Processing: Eluted in 100 μL phosphate-buffered saline Storage: Placed in liquid nitrogen | ELISA | IL-1β, IL-6, PGE2 | Periodontal intervention:
| Strong |
| Yalcin et al. (2002) [55] | Turkey, intervention pilot study Intervention: non-surgical periodontal therapy | Pregnant women (22) | T1: 1st trimester T2: 2nd trimester T3: 3rd trimester | PPD, PI, GBI | GCF: Method: Filter paper strips Site: Mesiobuccal aspects of 2 teeth in the anterior region Collection time: 30 s. Processing: Eluted in tris buffered saline Storage: Stored at −70 ° C | ELISA | PGE2 | Periodontal intervention:
| Weak |
3.5. Differences in Inflammatory Responses in Oral Biofilm between Pregnant and Non-Pregnant Women with Periodontitis
| Author (year) | Country, Study Design | Investigated Groups (n of Subjects) | Measurement Interval | Periodontal Examination | Sample Collection | Sample Analysis | Evaluated Biomarker | Main study Findings and Key Messages | Quality Assessment |
|---|---|---|---|---|---|---|---|---|---|
| Gümüs et al. (2016) [57] | Turkey, cross-sectional study | Pregnant women (59) Healthy (17) Gingivitis (25) Periodontitis (17) Non-pregnant women (70) Healthy (27) Gingivitis (28) Periodontitis (15) Postpartum women (47) Healthy (14) Gingivitis (21) Periodontitis (12) | One time-point: 2nd or 3rd trimester for pregnant groups, 6 months postpartum for postpartum groups | PPD, CAL, BOP, PI | Saliva: Preparation: Subjects were asked to fast overnight during which individuals were requested not to drink (except water) or chew gum Method: Expectoration into polypropylene tubes for 5 min Processing: not specified Storage: Supernatants stored at −40 °C | ELISA | 25-hydroxy-cholecalciferol (25(OH)D), PGE2, TNF-α | Pregnant women vs. postpartum group:
| Fair |
| Hassan et al. (2018) [58] | Turkey, cross-sectional study | Pregnant women (78) Healthy (22) Gingivitis (47) Periodontitis (9) Non-pregnant women (69) Healthy (30) Gingivitis (28) Periodontitis (11) | One time-point: 2nd or 3rd trimester | PPD, CAL, BOP, PI | Saliva: Preparation: Subjects were asked to fast overnight and to rinse their mouth with tap water 5 min prior to sample collection Method: not specified Processing: Centrifuged at 10,000× g for 15 min at 4 °C Storage: Supernatants stored at −80 °C | Protein assay kit, ELISA | Total protein, Annexin-1, IL-1𝛽 |
| Good |
4. Discussion
Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Nuriel-Ohayon, M.; Neuman, H.; Koren, O. Microbial changes during pregnancy, birth, and infancy. Front. Microbiol. 2016, 7, 1031. [Google Scholar] [CrossRef] [PubMed]
- Figueiredo, C.S.D.A.; Rosalem, C.G.C.; Cantanhede, A.L.C.; Thomaz, B.A.F.; Da Cruz, M.C.F.N. Systemic alterations and their oral manifestations in pregnant women. J. Obstet. Gynaecol. Res. 2017, 43, 16–22. [Google Scholar] [CrossRef] [PubMed]
- Marsh, P.D.; Do, T.; Devine, D. Oral biofilms: Molecular analysis, challenges, and future prospects in dental diagnostics. Clin. Cosmet. Investig. Dent. 2013, 5, 11–19. [Google Scholar] [CrossRef] [PubMed]
- Takahashi, N. Oral microbiome metabolism: From “who are they?” to “what are they doing?”. J. Dent. Res. 2015, 94, 1628–1637. [Google Scholar] [CrossRef]
- Jang, H.; Patoine, A.; Wu, T.T.; Castillo, D.A.; Xiao, J. Oral microflora and pregnancy: A systematic review and meta-analysis. Sci. Rep. 2021, 11, 16870. [Google Scholar] [CrossRef] [PubMed]
- Türkoğlu, O.; Barış, N.; Tervahartiala, T.; Şenarslan, Ö.; Sorsa, T.; Atilla, G. Evaluation of systemic levels of neutrophilic enzymes in patients with hypertension and chronic periodontitis. J. Periodontol. 2014, 85, 908–916. [Google Scholar] [CrossRef] [PubMed]
- Sanz, M.; Kornman, K. Periodontitis and adverse pregnancy outcomes: Consensus report of the Joint EFP/AAP Workshop on Periodontitis and Systemic Diseases. J. Clin. Periodontol. 2013, 40, S164–S169. [Google Scholar] [CrossRef]
- Mor, G.; Aldo, P.; Alvero, A.B. The unique immunological and microbial aspects of pregnancy. Nat. Rev. Immunol. 2017, 17, 469–482. [Google Scholar] [CrossRef]
- Saadaoui, M.; Singh, P.; Al Khodor, S. Oral microbiome and pregnancy: A bidirectional relationship. J. Reprod. Immunol. 2021, 145, 103293. [Google Scholar] [CrossRef]
- Corbella, S.; Taschieri, S.; Del Fabbro, M.; Francetti, L.; Weinstein, R.; Ferrazzi, E. Adverse pregnancy outcomes and periodontitis: A systematic review and meta-analysis exploring potential association. Quintessence Int. 2016, 47, 193–204. [Google Scholar]
- Daalderop, L.; Wieland, B.; Tomsin, K.; Reyes, L.; Kramer, B.; Vanterpool, S.; Been, J. Periodontal disease and pregnancy outcomes: Overview of systematic reviews. JDR Clin. Transl. Res. 2018, 3, 10–27. [Google Scholar] [CrossRef] [PubMed]
- McCullough, L.E.; Miller, E.E.; Calderwood, L.E.; Shivappa, N.; Steck, S.E.; Forman, M.R.; AMendez, M.; Maguire, R.; Fuemmeler, B.F.; Kollins, S.H.; et al. Maternal inflammatory diet and adverse pregnancy outcomes: Circulating cytokines and genomic imprinting as potential regulators? Epigenetics 2017, 12, 688–697. [Google Scholar] [CrossRef] [PubMed]
- Cho, G.J.; Kim, S.-Y.; Lee, H.C.; Kim, H.Y.; Lee, K.-M.; Han, S.W.; Oh, M.-J. Association between dental caries and adverse pregnancy outcomes. Sci. Rep. 2020, 10, 5309. [Google Scholar] [CrossRef] [PubMed]
- Rowińska, I.; Szyperska-Ślaska, A.; Zariczny, P.; Pasławski, R.; Kramkowski, K.; Kowalczyk, P. The influence of diet on oxidative stress and inflammation induced by bacterial biofilms in the human oral cavity. Materials 2021, 14, 1444. [Google Scholar] [CrossRef]
- Yenen, Z.; Ataçağ, T. Oral care in pregnancy. J. Turk. Ger. Gynecol. Assoc. 2019, 20, 264. [Google Scholar] [CrossRef]
- Shira Davenport, E. Preterm low birthweight and the role of oral bacteria. J. Oral. Microbiol. 2010, 2, 5779. [Google Scholar] [CrossRef]
- Liberati, A.; Altman, D.G.; Tetzlaff, J.; Mulrow, C.; Gøtzsche, P.C.; Ioannidis, J.P.A.; Clarke, M.; Devereaux, P.J.; Kleijnen, J.; Moher, D. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: Explanation and elaboration. J. Clin. Epidemiol. 2009, 62, e1–e34. [Google Scholar] [CrossRef]
- Thomas, B.; Ciliska, D.; Dobbins, M.; Micucci, S. A process for systematically reviewing the literature: Providing the research evidence for public health nursing interventions. Worldviews Evid.-Based Nurs. 2004, 1, 176–184. [Google Scholar] [CrossRef]
- National Heart, Lung and Blood Institute. NIH Quality Assessment Tool for Observational Cohort and Cross-Sectional Studies Systematic Review. 2013. Available online: https://www.nhlbi.nih.gov/health-topics/study-quality-assessment-tools (accessed on 15 May 2022).
- Özçaka; Ceyhan-Öztürk, B.; Gümüş, P.; Akcalı, A.; Nalbantsoy, A.; Buduneli, N. Clinical periodontal status and inflammatory cytokines in gestational diabetes mellitus. Arch. Oral. Biol. 2016, 72, 87–91. [Google Scholar] [CrossRef]
- Gümüş, P.; Özcaka, Ö.; Ceyhan-Öztürk, B.; Akcali, A.; Lappin, D.; Buduneli, N. Evaluation of Biochemical Parameters, Local and Systemic Levels of Osteoactive and B Cell Stimulatory Factors in Gestational Diabetes in the Presence or Absence of Gingivitis. J. Periodontology 2014, 86, 1–15. [Google Scholar] [CrossRef]
- Chaparro, A.; Zúñiga, E.; Varas-Godoy, M.; Albers, D.; Ramírez, V.; Hernández, M.; Kusanovic, J.P.; Acuña-Gallardo, S.; Rice, G.; Illanes, S.E. Periodontitis and placental growth factor in oral fluids are early pregnancy predictors of gestational diabetes mellitus. J. Periodontol. 2018, 89, 1052–1060. [Google Scholar] [CrossRef] [PubMed]
- Surdacka, A.; Ciężka, E.; Pioruńska-Stolzmann, M.; Wender-Ożegowska, E.; Korybalska, K.; Kawka, E.; Kaczmarek, E.; Witowski, J. Relation of salivary antioxidant status and cytokine levels to clinical parameters of oral health in pregnant women with diabetes. Arch. Oral. Biol. 2011, 56, 428–436. [Google Scholar] [CrossRef] [PubMed]
- Zalewska, A.; Knaś, M.; Gumiężny, G.; Niczyporuk, M.; Waszkiel, D.; Przystupa, A.W.; Zarzycki, W. Salivary exoglycosidases in gestational diabetes. Postepy Hig. Med. Dosw. (Online) 2013, 67, 315–320. [Google Scholar] [CrossRef] [PubMed]
- Zygula, A.; Kosinski, P.; Zwierzchowska, A.; Sochacka, M.; Wroczynski, P.; Makarewicz-Wujec, M.; Pietrzak, B.; Wielgos, M.; Rzentala, M.; Giebultowicz, J. Oxidative stress markers in saliva and plasma differ between diet-controlled and insulin-controlled gestational diabetes mellitus. Diabetes Res. Clin. Pr. 2019, 148, 72–80. [Google Scholar] [CrossRef]
- Balan, P.; Chong, Y.S.; Lin, Q.; Lim, T.K.; Li, H.; Wong, M.L.; Lopez, V.; He, H.G. Isobaric tags for relative and absolute quantification (iTRAQ)-based quantitative analysis of the salivary proteome during healthy pregnancy and pregnancy gingivitis. J. Clin. Periodontol. 2021, 48, 1559–1569. [Google Scholar] [CrossRef] [PubMed]
- Balan, P.; Chong, Y.S.; Lin, Q.; Lim, T.K.; Suriyanarayanan, T.; Udawatte, N.S.; Wong, M.L.; Lopez, V.; He, H.-G.; Seneviratne, C.J. Salivary Proteomic Profiling Identifies Role of Neutrophil Extracellular Traps Formation in Pregnancy Gingivitis. Immunol. Investig. 2022, 51, 103–119. [Google Scholar] [CrossRef]
- Machado, V.; Mesquita, M.F.; Bernardo, M.A.; Casal, E.; Proença, L.; Mendes, J.J. IL-6 and TNF-alpha salivary levels according to the periodontal status in Portuguese pregnant women. PeerJ 2018, 6, e4710. [Google Scholar] [CrossRef]
- Mahilkar, S.; Malagi, S.K.; Soni, A.; Abraham, D.V.; Johnson, L.; Pattanshetti, K.S. IL-17, A Possible Salivary Biomarker for Preterm Birth in Females with Periodontitis. J. Obstet. Gynecol. India 2021, 71, 262–267. [Google Scholar] [CrossRef]
- Yang, I.; Knight, A.K.; Dunlop, A.L.; Corwin, E.J. Characterizing the Subgingival Microbiome of Pregnant African American Women. Jognn-J. Obstet. Gynecol. Neonatal. Nurs. 2019, 48, 140–152. [Google Scholar] [CrossRef]
- Oettinger-Barak, O.; Barak, S.; Ohel, G.; Oettinger, M.; Kreutzer, H.; Peled, M.; Machtei, E.E. Severe pregnancy complication (preeclampsia) is associated with greater periodontal destruction. J. Periodontol. 2005, 76, 134–137. [Google Scholar] [CrossRef]
- Chaparro, A.; Gaedechens, D.; Ramírez, V.; Zuñiga, E.; Kusanovic, J.P.; Inostroza, C.; Varas-Godoy, M.; Silva, K.; Salomon, C.; Rice, G.; et al. Placental biomarkers and angiogenic factors in oral fluids of patients with preeclampsia. Prenat. Diagn. 2016, 36, 476–482. [Google Scholar] [CrossRef] [PubMed]
- Canakci, V.; Yildirim, A.; Canakci, C.F.; Eltas, A.; Cicek, Y.; Canakci, H.; Çiçek, Y. Total antioxidant capacity and antioxidant enzymes in serum, saliva, and gingival crevicular fluid of preeclamptic women with and without periodontal disease. J. Periodontol. 2007, 78, 1602–1611. [Google Scholar] [CrossRef] [PubMed]
- Foratori-Junior, G.A.; Mosquim, V.; Buzalaf, M.A.R.; de Carvalho Sales-Peres, S.H. Salivary cytokines levels, maternal periodontitis and infants’ weight at birth: A cohort study in pregnant women with obesity. Placenta 2021, 115, 151–157. [Google Scholar] [CrossRef]
- Zambon, M.; Mandò, C.; Lissoni, A.; Anelli, G.M.; Novielli, C.; Cardellicchio, M.; Leone, R.; Monari, M.N.; Massari, M.; Cetin, I.; et al. Inflammatory and Oxidative Responses in Pregnancies With Obesity and Periodontal Disease. Reprod Sci. 2018, 25, 1474–1484. [Google Scholar] [CrossRef]
- Carta, G.; Persia, G.; Falciglia, K.; Iovenitti, P. Periodontal disease and poor obstetrical outcome. Clin. Exp. Obs. Gynecol. 2004, 31, 47–49. [Google Scholar]
- Nikolic, L.; Cakic, S.; Perunovic, N.; Colak, E.; Kotur-Stevuljevic, J.; Jankovic, S.; Djuric, M.; Plecas, D. Salivary and plasma inflammatory mediators and secretory status in preterm delivery women with periodontitis—A cross sectional study. Vojnosanit. Pregl. 2020, 77, 247–255. [Google Scholar] [CrossRef]
- Noack, B.; Klingenberg, J.; Weigelt, J.; Hoffmann, T. Periodontal status and preterm low birth weight: A case control study. J Periodontal. Res. 2005, 40, 339–345. [Google Scholar] [CrossRef]
- Surbek, D.; Stadelmann, P.; Bürgin, W.B.; Ramseier, C.A.; Sculean, A.; Eick, S.; Mohr, S.; Salvi, G.E. Increased periodontal inflammation in women with preterm premature rupture of membranes. Clin. Oral. Investig. 2015, 19, 1537–1546. [Google Scholar]
- Zygula, A.; Kosinski, P.; Wroczynski, P.; Makarewicz-Wujec, M.; Pietrzak, B.; Wielgos, M.; Giebultowicz, J. Oxidative Stress Markers Differ in Two Placental Dysfunction Pathologies: Pregnancy-Induced Hypertension and Intrauterine Growth Restriction. Oxid. Med. Cell Longev. 2020, 2020, 1323891. [Google Scholar] [CrossRef]
- Balan, P.; Chong, Y.S.; Qingsong, L.; Lim, T.K.; Wong, M.L.; Lopez, V.; He, H.; Seneviratne, C.J. Quantitative proteomics analysis identifies salivary biomarkers for early detection of pregnancy loss in a Singaporean cohort-A pilot study. Proteom. Clin. Appl. 2021, 15, e2000068. [Google Scholar] [CrossRef]
- Wu, M.; Chen, S.W.; Su, W.L.; Zhu, H.Y.; Ouyang, S.Y.; Cao, Y.T.; Jiang, S.Y. Sex Hormones Enhance Gingival Inflammation without Affecting IL-1 beta and TNF-alpha in Periodontally Healthy Women during Pregnancy. Mediat. Inflamm. 2016, 2016, 4897890. [Google Scholar] [CrossRef] [PubMed]
- Yarkac, F.U.; Gokturk, O.; Demir, O. Effect of non-surgical periodontal therapy on the degree of gingival inflammation and stress markers related to pregnancy. J. Appl. Oral Sci. Rev. FOB 2018, 26, e20170630. [Google Scholar] [CrossRef] [PubMed]
- Yarkac, F.U.; Gokturk, O.; Demir, O. Demir, Interaction between stress, cytokines, and salivary cortisol in pregnant and non-pregnant women with gingivitis. Clin. Oral. Investig. 2021, 25, 1677–1684. [Google Scholar] [CrossRef]
- Ehlers, V.; Callaway, A.; Hortig, W.; Kasaj, A.; Willershausen, B. Clinical parameters and aMMP-8-concentrations in gingival crevicular fluid in pregnancy gingivitis. Clin. Lab. 2013, 59, 605–611. [Google Scholar] [CrossRef]
- Gürsoy, M.; Könönen, E.; Gursoy, U.K.; Tervahartiala, T.; Pajukanta, R.; Sorsa, T. Periodontal Status and Neutrophilic Enzyme Levels in Gingival Crevicular Fluid During Pregnancy and Postpartum. J. Periodontol. 2010, 81, 1790–1796. [Google Scholar] [CrossRef]
- Gürsoy, M.; Könönen, E.; Tervahartiala, T.; Gürsoy, U.K.; Pajukanta, R.; Sorsa, T. Longitudinal study of salivary proteinases during pregnancy and postpartum. J. Periodontal. Res. 2010, 45, 496–503. [Google Scholar] [CrossRef]
- Öztürk, L.K.; Akyüz, S.; Yarat, A.; Koç, S.; Gül, N.; Doğan, B. Salivary lipid peroxidation and total sialic acid levels during healthy gestation and postpartum: A longitudinal study. Clin. Biochem. 2010, 43, 430–434. [Google Scholar] [CrossRef] [PubMed]
- Gümüş, P.; Emingil, G.; Öztürk, V.-Ö.; Belibasakis, G.N.; Bostanci, N. Oxidative stress markers in saliva and periodontal disease status: Modulation during pregnancy and postpartum. BMC Infect. 2015, 15, 5261. [Google Scholar] [CrossRef]
- Gürsoy, M.; Gürsoy, U.K.; Liukkonen, A.; Kauko, T.; Penkkala, S.; Könönen, E. Salivary antimicrobial defensins in pregnancy. J. Clin. Periodontol. 2016, 43, 807–815. [Google Scholar] [CrossRef]
- Bieri, R.A.; Adriaens, L.; Spörri, S.; Lang, N.P.; Persson, G.R. Gingival fluid cytokine expression and subgingival bacterial counts during pregnancy and postpartum: A case series. Clin. Oral. Investig. 2013, 17, 19–28. [Google Scholar] [CrossRef][Green Version]
- Lasisi, T.J.; Abdus-Salam, R.A. Abdus-salam, Pregnancy-induced periodontal inflammation: Influence of salivary cytokines and antimicrobial proteins. Saudi Dent. J. 2018, 30, 306–311. [Google Scholar] [CrossRef] [PubMed]
- Gürsoy, M.; Zeidán-Chuliá, F.; Könönen, E.; Moreira, J.C.F.; Liukkonen, J.; Sorsa, T.; Gürsoy, U.K. Pregnancy-induced gingivitis and OMICS in dentistry: In silico modeling and in vivo prospective validation of estradiol-modulated inflammatory biomarkers. Omics 2014, 18, 582–590. [Google Scholar] [CrossRef] [PubMed]
- Kaur, M.; Geisinger, M.L.; Geurs, N.C.; Griffin, R.; Vassilopoulos, P.J.; Vermeulen, L.; Haigh, S.; Reddy, M.S. Effect of intensive oral hygiene regimen during pregnancy on periodontal health, cytokine levels, and pregnancy outcomes: A pilot study. J. Periodontol. 2014, 85, 1684–1692. [Google Scholar] [CrossRef] [PubMed]
- Yalcin, F.; Basegmez, C.; Isik, G.; Berber, L.; Eskinazi, E.; Soydinc, M.; Issever, H.; Onan, U.; Işık, G. The effects of periodontal therapy on intracrevicular prostaglandin E-2 concentrations and clinical parameters in pregnancy. J. Periodontol. 2002, 73, 173–177. [Google Scholar] [CrossRef]
- Offenbacher, S.; Lin, D.; Strauss, R.; McKaig, R.; Irving, J.; Barros, S.P.; Moss, K.; Barrow, D.A.; Hefti, A.; Beck, J.D. Effects of periodontal therapy during pregnancy on periodontal status, biologic parameters, and pregnancy outcomes: A pilot study. J. Periodontol. 2006, 77, 2011–2024. [Google Scholar] [CrossRef]
- Gümüş, P.; Öztürk, V.; Bozkurt, E.; Emingil, G. Evaluation of the gingival inflammation in pregnancy and postpartum via 25-hydroxy-vitamin D3, prostaglandin E2 and TNF-α levels in saliva. Arch. Oral. Biol. 2016, 63, 1–6. [Google Scholar] [CrossRef]
- Hassan, M.N.; Belibasakis, G.N.; Gumus, P.; Öztürk, V.; Emingil, G.; Bostanci, N. Annexin-1 as a salivary biomarker for gingivitis during pregnancy. J. Periodontol. 2018, 89, 875–882. [Google Scholar] [CrossRef]
- Hajishengallis, G.; Chavakis, T. Local and systemic mechanisms linking periodontal disease and inflammatory comorbidities. Nat. Rev. Immunol. 2021, 21, 426–440. [Google Scholar] [CrossRef]
- Robinson, D.P.; Klein, S.L. Pregnancy and pregnancy-associated hormones alter immune responses and disease pathogenesis. Horm. Behav. 2012, 62, 263–271. [Google Scholar] [CrossRef]
- Li, X.; Zhou, J.; Fang, M.; Yu, B. Pregnancy immune tolerance at the maternal-fetal interface. Int. Rev. Immunol. 2020, 39, 247–263. [Google Scholar] [CrossRef]
- Björkander, S.; Bremme, K.; Persson, J.-O.; van Vollenhoven, R.; Sverremark-Ekström, E.; Holmlund, U. Pregnancy-associated inflammatory markers are elevated in pregnant women with systemic lupus erythematosus. Cytokine 2012, 59, 392–399. [Google Scholar] [CrossRef] [PubMed]
- Raju, K.; Berens, L. Periodontology and pregnancy: An overview of biomedical and epidemiological evidence. Periodontol 2000 2021, 87, 132–142. [Google Scholar] [CrossRef] [PubMed]
- Lain, K.Y.; Catalano, P.M. Metabolic changes in pregnancy. Clin. Obstet. Gynecol. 2007, 50, 938–948. [Google Scholar] [CrossRef]
- Jarmund, A.H.; Giskeødegård, G.F.; Ryssdal, M.; Steinkjer, B.; Stokkeland, L.M.T.; Madssen, T.S.; Stafne, S.N.; Stridsklev, S.; Moholdt, T.; Heimstad, R.; et al. Cytokine patterns in maternal serum from first trimester to term and beyond. Front. Immunol. 2021, 12. [Google Scholar] [CrossRef] [PubMed]
- Chung, W.-C.; Huang, C.-F.; Feng, S.-W. Clinical Benefits of Minimally Invasive Non-Surgical Periodontal Therapy as an Alternative of Conventional Non-Surgical Periodontal Therapy—A Pilot Study. Int. J. Environ. Res. Public Health 2022, 19, 7456. [Google Scholar] [CrossRef] [PubMed]
- Yue, H.; Xu, X.; Liu, Q.; Li, X.; Xiao, Y.; Hu, B. Effects of non-surgical periodontal therapy on systemic inflammation and metabolic markers in patients undergoing haemodialysis and/or peritoneal dialysis: A systematic review and meta-analysis. BMC Oral Health 2020, 20, 18. [Google Scholar] [CrossRef]
- Mauri-Obradors, E.; Merlos, A.; Estrugo-Devesa, A.; Jané-Salas, E.; López-López, J.; Viñas, M. Benefits of non-surgical periodontal treatment in patients with type 2 diabetes mellitus and chronic periodontitis: A randomized controlled trial. J. Clin. Periodontol. 2018, 45, 345–353. [Google Scholar] [CrossRef]
- D’Isidoro, O.; Perrotti, V.; Hui, W.L.; Piattelli, A.; Iaculli, F.; Quaranta, A. The impact of non-surgical therapy of periodontal disease on surrogate markers for cardiovascular disease: A literature review. Am. J. Dent. 2019, 32, 191–200. [Google Scholar]
- Le, Q.A.; Eslick, G.D.; Coulton, K.M.; Akhter, R.; Condous, G.; Eberhard, J.; Nanan, R. Does Treatment of Gingivitis During Pregnancy Improve Pregnancy Outcomes? A Systematic Review and Meta-Analysis. Oral Health Prev. Dent. 2021, 19, 565–572. [Google Scholar]
- Schwendicke, F.; Karimbux, N.Y.; Allareddy, V.; Gluud, C. Periodontal treatment for preventing adverse pregnancy outcomes: A meta-and trial sequential analysis. PLoS ONE 2015, 10, e0129060. [Google Scholar] [CrossRef]
- Tarannum, F.; Faizuddin, M. Effect of periodontal therapy on pregnancy outcome in women affected by periodontitis. J. Periodontol. 2007, 78, 2095–2103. [Google Scholar] [CrossRef] [PubMed]
- Stadelmann, P.; Alessandri, R.; Eick, S.; Salvi, G.E.; Surbek, D.; Sculean, A. The potential association between gingival crevicular fluid inflammatory mediators and adverse pregnancy outcomes: A systematic review. Clin. Oral Investig. 2013, 17, 1453–1463. [Google Scholar] [CrossRef] [PubMed]
- Pantham, P.; Aye, I.; Powell, T. Inflammation in maternal obesity and gestational diabetes mellitus. Placenta 2015, 36, 709–715. [Google Scholar] [CrossRef] [PubMed]
- Hajianfar, H.; Esmaillzadeh, A.; Feizi, A.; Shahshahan, Z.; Azadbakht, L. The Association Between Major Dietary Patterns and Pregnancy-related Complications. Arch. Iran Med. 2018, 21, 443–451. [Google Scholar]
- Chapple, I.L.C.; Bouchard, P.; Cagetti, M.G.; Campus, G.; Carra, M.-C.; Cocco, F.; Nibali, L.; Hujoel, P.; Laine, M.L.; Lingström, P.; et al. Interaction of lifestyle, behaviour or systemic diseases with dental caries and periodontal diseases: Consensus report of group 2 of the joint EFP/ORCA workshop on the boundaries between caries and periodontal diseases. J. Clin. Periodontol. 2017, 44, S39–S51. [Google Scholar] [CrossRef]
- Hujoel, P.P.; Lingström, P. Nutrition, dental caries and periodontal disease: A narrative review. J. Clin. Periodontol. 2017, 44, S79–S84. [Google Scholar] [CrossRef]
- Ellulu, M.S.; Patimah, I.; Khaza’Ai, H.; Rahmat, A.; Abed, Y.; Ali, F. Atherosclerotic cardiovascular disease: A review of initiators and protective factors. Inflammopharmacology 2016, 24, 1–10. [Google Scholar] [CrossRef]
- Bennett, G.; Bardon, L.A.; Gibney, E.R. A Comparison of Dietary Patterns and Factors Influencing Food Choice among Ethnic Groups Living in One Locality: A Systematic Review. Nutrients 2022, 14, 941. [Google Scholar] [CrossRef]
- Patrick, D.L.; Lee, R.S.Y.; Nucci, M.; Grembowski, D.; Jolles, C.Z.; Milgrom, P. Reducing Oral Health Disparities: A Focus on Social and Cultural Determinants. BMC Oral Health 2006, 6, S4. [Google Scholar] [CrossRef]
- Martinez-Herrera, M.; Silvestre-Rangil, J.; Silvestre, F.J. Association between obesity and periodontal disease. A systematic review of epidemiological studies and controlled clinical trials. Med. Oral Patol. Oral Cir. Bucal. 2017, 22, e708. [Google Scholar] [CrossRef]
- Altun, E.; Walther, C.; Borof, K.; Petersen, E.; Lieske, B.; Kasapoudis, D.; Jalilvand, N.; Beikler, T.; Jagemann, B.; Zyriax, B.-C.; et al. Association between Dietary Pattern and Periodontitis—A Cross-Sectional Study. Nutrients 2021, 13, 4167. [Google Scholar] [CrossRef] [PubMed]
- Champion, M.L.; Harper, L.M. Gestational Weight Gain: Update on Outcomes and Interventions. Curr. Diab. Rep. 2020, 20, 11. [Google Scholar] [CrossRef] [PubMed]
- Bartha, V.; Exner, L.; Schweikert, D.; Woelber, J.P.; Vach, K.; Meyer, A.; Basrai, M.; Bischoff, S.C.; Meller, C.; Wolff, D. Effect of the Mediterranean diet on gingivitis: A randomized controlled trial. J. Clin. Periodontol. 2022, 49, 111–122. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lieske, B.; Makarova, N.; Jagemann, B.; Walther, C.; Ebinghaus, M.; Zyriax, B.-C.; Aarabi, G. Inflammatory Response in Oral Biofilm during Pregnancy: A Systematic Review. Nutrients 2022, 14, 4894. https://doi.org/10.3390/nu14224894
Lieske B, Makarova N, Jagemann B, Walther C, Ebinghaus M, Zyriax B-C, Aarabi G. Inflammatory Response in Oral Biofilm during Pregnancy: A Systematic Review. Nutrients. 2022; 14(22):4894. https://doi.org/10.3390/nu14224894
Chicago/Turabian StyleLieske, Berit, Nataliya Makarova, Bettina Jagemann, Carolin Walther, Merle Ebinghaus, Birgit-Christiane Zyriax, and Ghazal Aarabi. 2022. "Inflammatory Response in Oral Biofilm during Pregnancy: A Systematic Review" Nutrients 14, no. 22: 4894. https://doi.org/10.3390/nu14224894
APA StyleLieske, B., Makarova, N., Jagemann, B., Walther, C., Ebinghaus, M., Zyriax, B.-C., & Aarabi, G. (2022). Inflammatory Response in Oral Biofilm during Pregnancy: A Systematic Review. Nutrients, 14(22), 4894. https://doi.org/10.3390/nu14224894






