Tracking of Dietary Patterns in the Secondary Prevention of Cardiovascular Disease after a Nutritional Intervention Program—A Randomized Clinical Trial
Abstract
1. Introduction
2. Materials and Methods
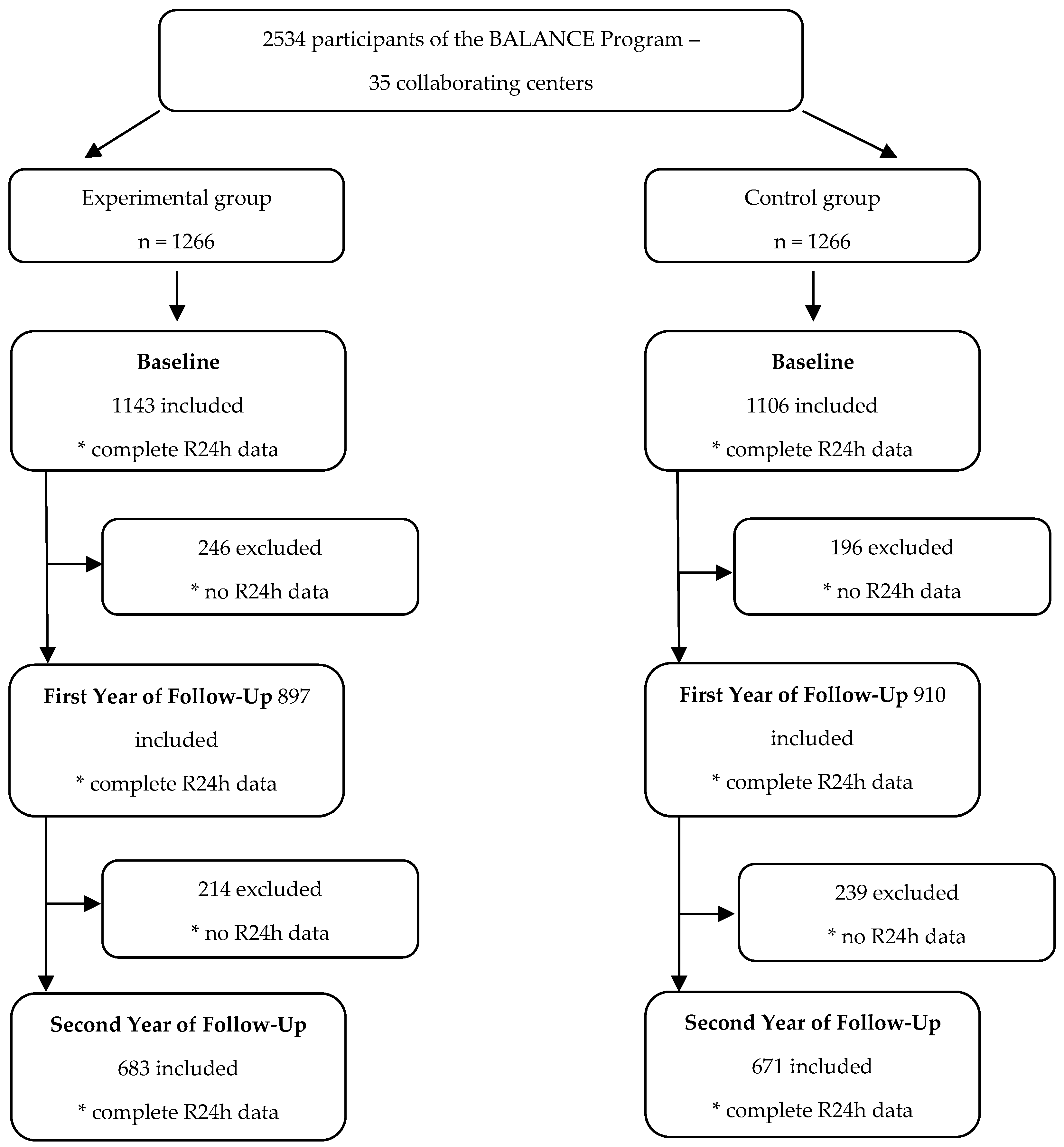
2.1. Study Design and Population
2.2. Intervention
2.2.1. Control Group
2.2.2. Experimental Group
2.3. Dietary Assessment
2.4. Dietary Patterns
2.5. Covariate Assessment
2.6. Statistical Analyses
2.7. Ethical Aspects
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Hobbs, F.D.R. Cardiovascular Disease: Different Strategies for Primary and Secondary Prevention? Heart 2004, 90, 1217–1223. [Google Scholar] [CrossRef] [PubMed]
- Li, J.; Gao, X.; Hao, X.; Kantas, D.; Mohamed, E.A.; Zheng, X.; Xu, H.; Zhang, L. Yoga for Secondary Prevention of Coronary Heart Disease: A Systematic Review and Meta-Analysis. Complement. Ther. Med. 2021, 57, 102643. [Google Scholar] [CrossRef] [PubMed]
- McEvoy, C.T.; Moore, S.E.; Appleton, K.M.; Cupples, M.E.; Erwin, C.; Kee, F.; Prior, L.; Young, I.S.; McKinley, M.C.; Woodside, J.V. Development of a Peer Support Intervention to Encourage Dietary Behaviour Change towards a Mediterranean Diet in Adults at High Cardiovascular Risk. BMC Public Health 2018, 18, 1194. [Google Scholar] [CrossRef] [PubMed]
- WHO Reveals Leading Causes of Death and Disability Worldwide: 2000–2019. Available online: https://www.who.int/news/item/09-12-2020-who-reveals-leading-causes-of-death-and-disability-worldwide-2000-2019 (accessed on 25 July 2022).
- Malta, D.C.; Teixeira, R.; de Oliveira, G.M.M.; Ribeiro, A.L.P. Mortalidade por Doenças Cardiovasculares Segundo o Sistema de Informação sobre Mortalidade e as Estimativas do Estudo Carga Global de Doenças no Brasil, 2000–2017. Arq. Bras. Cardiol. 2020, 115, 152–160. [Google Scholar] [CrossRef]
- Moreira, P.V.L.; de Arruda Neta, A.d.C.P.; Ferreira, S.S.; Ferreira, F.E.L.L.; de Lima, R.L.F.C.; de Toledo Vianna, R.P.; de Araújo, J.M.; de Alencar Rodrigues, R.E.; da Silva Neto, J.M.; O’Flaherty, M. Coronary Heart Disease and Stroke Mortality Trends in Brazil 2000–2018. PLoS ONE 2021, 16, e0253639. [Google Scholar] [CrossRef]
- Verschuren, W.M.M.; Boer, J.M.A.; Temme, E.H.M. Optimal Diet for Cardiovascular and Planetary Health. Heart 2022, 108, 1234–1239. [Google Scholar] [CrossRef]
- Casas, R.; Castro-Barquero, S.; Estruch, R.; Sacanella, E. Nutrition and Cardiovascular Health. Int. J. Mol. Sci. 2018, 19, 3988. [Google Scholar] [CrossRef]
- World Health Organization. Diet, Nutrition and the Prevention of Chronic Diseases: Report of a Joint WHO/FAO Expert Consultation, Geneva, 28 January–1 February 2002; World Health Organization: Geneva, Switzerland, 2003. [Google Scholar]
- Yu, E.; Malik, V.S.; Hu, F.B. Cardiovascular Disease Prevention by Diet Modification: JACC Health Promotion Series. J. Am. Coll. Cardiol. 2018, 72, 914–926. [Google Scholar] [CrossRef]
- Mahdavi, R.; Bagheri Asl, A.; Abadi, M.A.J.; Namazi, N. Perceived Barriers to Following Dietary Recommendations in Hypertensive Patients. J. Am. Coll. Nutr. 2017, 36, 193–199. [Google Scholar] [CrossRef]
- Précoma, D.B.; de Oliveira, G.M.M.; Simão, A.F.; Dutra, O.P.; Coelho, O.R.; Izar, M.C.O.; Póvoa, R.M.d.S.; Giuliano, I.d.C.B.; Alencar, A.C.d.; Machado, C.A.; et al. Atualização da Diretriz de Prevenção Cardiovascular da Sociedade Brasileira de Cardiologia-2019. Arq. Bras. Cardiol. 2019, 113, 787–891. [Google Scholar] [CrossRef]
- Lindholm, L.H.; Mendis, S. Prevention of Cardiovascular Disease in Developing Countries. Lancet 2007, 370, 720–722. [Google Scholar] [CrossRef]
- Abdelhamid, A.S.; Brown, T.J.; Brainard, J.S.; Biswas, P.; Thorpe, G.C.; Moore, H.J.; Deane, K.H.; Summerbell, C.D.; Worthington, H.V.; Song, F.; et al. Omega-3 Fatty Acids for the Primary and Secondary Prevention of Cardiovascular Disease. Cochrane Database Syst. Rev. 2020, 3, CD003177. [Google Scholar] [CrossRef] [PubMed]
- Widmer, R.J.; Flammer, A.J.; Lerman, L.O.; Lerman, A. The Mediterranean Diet, Its Components, and Cardiovascular Disease. Am. J. Med. 2015, 128, 229–238. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Joint FAO/WHO Consultation on Preparation and Use of Food-Based Dietary Guidelines (1995: Nicosia, Cyprus). Preparation and Use of Food-Based Dietary Guidelines; World Health Organization: Geneva, Switzerland, 1998. [Google Scholar]
- Hu, F.B. Dietary Pattern Analysis: A New Direction in Nutritional Epidemiology. Curr. Opin. Lipidol. 2002, 13, 3–9. [Google Scholar] [CrossRef] [PubMed]
- Rodrigues, P.R.M.; Pereira, R.A.; Cunha, D.B.; Sichieri, R.; Ferreira, M.G.; Vilela, A.A.F.; Gonçalves-Silva, R.M.V. Fatores associados a padrões alimentares em adolescentes: Um estudo de base escolar em Cuiabá, Mato Grosso. Rev. Bras. Epidemiol. 2012, 15, 662–674. [Google Scholar] [CrossRef]
- Stradling, C.; Hamid, M.; Taheri, S.; Thomas, G.N. A Review of Dietary Influences on Cardiovascular Health: Part 2: Dietary Patterns. Cardiovasc. Hematol. Disord. Drug Targets 2014, 14, 50–63. [Google Scholar] [CrossRef]
- Zhang, X.-Y.; Shu, L.; Si, C.-J.; Yu, X.-L.; Liao, D.; Gao, W.; Zhang, L.; Zheng, P.-F. Dietary Patterns, Alcohol Consumption and Risk of Coronary Heart Disease in Adults: A Meta-Analysis. Nutrients 2015, 7, 6582–6605. [Google Scholar] [CrossRef]
- Weber, B.; Bersch-Ferreira, Â.C.; Torreglosa, C.R.; Marcadenti, A.; Lara, E.S.; da Silva, J.T.; Costa, R.P.; Santos, R.H.N.; Berwanger, O.; Bosquetti, R.; et al. Implementation of a Brazilian Cardioprotective Nutritional (BALANCE) Program for Improvement on Quality of Diet and Secondary Prevention of Cardiovascular Events: A Randomized, Multicenter Trial. Am. Heart J. 2019, 215, 187–197. [Google Scholar] [CrossRef]
- Weber, B.; Bersch-Ferreira, Â.C.; Torreglosa, C.R.; Ross-Fernandes, M.B.; da Silva, J.T.; Galante, A.P.; de Sousa Lara, E.; Costa, R.P.; Soares, R.M.; Cavalcanti, A.B.; et al. The Brazilian Cardioprotective Nutritional Program to Reduce Events and Risk Factors in Secondary Prevention for Cardiovascular Disease: Study Protocol (The BALANCE Program Trial). Am. Heart J. 2016, 171, 73–81.e2. [Google Scholar] [CrossRef]
- Galante, A.P. Desenvolvimento e Validação de um Método Computadorizado Para Avaliação do Consumo Alimentar, Preenchido por Indivíduos Adultos Utilizando a Web. Doctoral Thesis, Human Applied Research Program, University of Sao Paulo, Sao Paulo, Brazil, 2007. [Google Scholar]
- Dodd, K.W.; Guenther, P.M.; Freedman, L.S.; Subar, A.F.; Kipnis, V.; Midthune, D.; Tooze, J.A.; Krebs-Smith, S.M. Statistical Methods for Estimating Usual Intake of Nutrients and Foods: A Review of the Theory. J. Am. Diet Assoc. 2006, 106, 1640–1650. [Google Scholar] [CrossRef]
- Marchioni, D.M.L.; Gorgulho, B.M.; Steluti, J. Consumo Alimentar: Guia Para Avaliação, 1st ed.; Editora Manole: Barueri, Brazil, 2019; ISBN 978-85-204-5618-7. [Google Scholar]
- Haubrock, J.; Nöthlings, U.; Volatier, J.-L.; Dekkers, A.; Ocké, M.; Harttig, U.; Illner, A.-K.; Knüppel, S.; Andersen, L.F.; Boeing, H.; et al. Estimating Usual Food Intake Distributions by Using the Multiple Source Method in the EPIC-Potsdam Calibration Study. J. Nutr. 2011, 141, 914–920. [Google Scholar] [CrossRef] [PubMed]
- Harttig, U.; Haubrock, J.; Knüppel, S.; Boeing, H. EFCOVAL Consortium The MSM Program: Web-Based Statistics Package for Estimating Usual Dietary Intake Using the Multiple Source Method. Eur. J. Clin. Nutr. 2011, 65 (Suppl. 1), S87–S91. [Google Scholar] [CrossRef]
- Hair, J.F., Jr.; Black, W.C.; Babin, B.J.; Anderson, R.E.; Tatham, R.L.; Gouvêa, M.A.; Sant’Anna, A.S. Análise Multivariada de Dados, 6th ed.; Bookman: Phoenix, AZ, USA, 2009; ISBN 978-85-7780-402-3. [Google Scholar]
- Lei n° 10.741, de 1° de Outubro de 2003, Dispõe Sobre o Estatuto do Idoso e dá Outras Providências. Available online: http://www.planalto.gov.br/ccivil_03/leis/2003/l10.741.htm (accessed on 14 June 2022).
- Critério de Classificação Econômica do Brasil. Available online: https://www.abep.org/criterio-brasil (accessed on 14 June 2022).
- WHO. Expert Committee on Physical Status: The Use and Interpretation of Anthropometry. Physical Status: The Use of and Interpretation of Anthropometry, Report of a WHO Expert Committee; World Health Organization: Geneva, Switzerland, 1995. [Google Scholar]
- Organización Panamericana de la Salud. Anales da 36ª Reunión del Comité Asesor de Investigaciones en Salud. Encuesta Multicentrica: Salud, Bien Estar y Envejecimiento (SABE) en América Latinay el Caribe, Mayo 2001; Organización Panamericana de la Salud: Washington, DC, USA, 2001. [Google Scholar]
- Waist Circumference and Waist-Hip Ratio: Report of a WHO Expert Consultation. Available online: https://www.who.int/publications-detail-redirect/9789241501491 (accessed on 29 July 2022).
- Dietary Reference Intakes for Energy, Carbohydrate, Fiber, Fat, Fatty Acids, Cholesterol, Protein, and Amino Acids|The National Academies Press. Available online: https://nap.nationalacademies.org/catalog/10490/dietary-reference-intakes-for-energy-carbohydrate-fiber-fat-fatty-acids-cholesterol-protein-and-amino-acids (accessed on 1 August 2022).
- Haskell, W.L.; Lee, I.-M.; Pate, R.R.; Powell, K.E.; Blair, S.N.; Franklin, B.A.; Macera, C.A.; Heath, G.W.; Thompson, P.D.; Bauman, A. Physical Activity and Public Health: Updated Recommendation for Adults from the American College of Sports Medicine and the American Heart Association. Med. Sci. Sports Exerc. 2007, 39, 1423–1434. [Google Scholar] [CrossRef] [PubMed]
- IBGE Pesquisa de Orçamentos Familiares: 2017–2018: Análise Do Consumo Alimentar Pessoal No Brasil/IBGE, Coordenação de Trabalho e Rendimento. Available online: https://biblioteca.ibge.gov.br/index.php/biblioteca-catalogo?view=detalhes&id=2101742 (accessed on 1 August 2022).
- BRASIL. Ministério da Saúde. Secretaria de Vigilância em Saúde. Departamento de Análise em Saúde e Vigilância de Doenças Não Transmissíveis. Vigitel Brasil 2021: Vigilância de Fatores de Risco e Proteção para Doenças Crônicas por Inquérito Telefônico: Estimativas sobre Frequência e Distribuição Sociodemográfica de Fatores de Risco e Proteção para Doenças Crônicas nas Capitais dos 26 Estados Brasileiros e no Distrito Federal em 2021. Brasilia, Brazil, 2021. Available online: https://www.gov.br/saude/pt-br/centrais-de-conteudo/publicacoes/publicacoes-svs/vigitel/relatorio-vigitel-2020-original.pdf/view (accessed on 1 August 2022).
- Crowe, F.L.; Key, T.J.; Appleby, P.N.; Overvad, K.; Schmidt, E.B.; Egeberg, R.; Tjønneland, A.; Kaaks, R.; Teucher, B.; Boeing, H.; et al. Dietary Fibre Intake and Ischaemic Heart Disease Mortality: The European Prospective Investigation into Cancer and Nutrition-Heart Study. Eur. J. Clin. Nutr. 2012, 66, 950–956. [Google Scholar] [CrossRef]
- Zazpe, I.; Santiago, S.; Gea, A.; Ruiz-Canela, M.; Carlos, S.; Bes-Rastrollo, M.; Martínez-González, M.A. Association between a Dietary Carbohydrate Index and Cardiovascular Disease in the SUN (Seguimiento Universidad de Navarra) Project. Nutr. Metab. Cardiovasc. Dis. 2016, 26, 1048–1056. [Google Scholar] [CrossRef] [PubMed]
- Lie, L.; Brown, L.; Forrester, T.E.; Plange-Rhule, J.; Bovet, P.; Lambert, E.V.; Layden, B.T.; Luke, A.; Dugas, L.R. The Association of Dietary Fiber Intake with Cardiometabolic Risk in Four Countries across the Epidemiologic Transition. Nutrients 2018, 10, 628. [Google Scholar] [CrossRef]
- He, F.J.; MacGregor, G.A. A Comprehensive Review on Salt and Health and Current Experience of Worldwide Salt Reduction Programmes. J. Hum. Hypertens. 2009, 23, 363–384. [Google Scholar] [CrossRef]
- Moubarac, J.-C.; Martins, A.P.B.; Claro, R.M.; Levy, R.B.; Cannon, G.; Monteiro, C.A. Consumption of Ultra-Processed Foods and Likely Impact on Human Health. Evidence from Canada. Public Health Nutr. 2013, 16, 2240–2248. [Google Scholar] [CrossRef]
- Dos Reis Padilha, G.; Sanches Machado d’Almeida, K.; Ronchi Spillere, S.; Corrêa Souza, G. Dietary Patterns in Secondary Prevention of Heart Failure: A Systematic Review. Nutrients 2018, 10, 828. [Google Scholar] [CrossRef]
- Srour, B.; Fezeu, L.K.; Kesse-Guyot, E.; Allès, B.; Méjean, C.; Andrianasolo, R.M.; Chazelas, E.; Deschasaux, M.; Hercberg, S.; Galan, P.; et al. Ultra-Processed Food Intake and Risk of Cardiovascular Disease: Prospective Cohort Study (NutriNet-Santé). BMJ 2019, 365, l1451. [Google Scholar] [CrossRef]
- Yang, Q.; Zhang, Z.; Steele, E.M.; Moore, L.V.; Jackson, S.L. Ultra-Processed Foods and Excess Heart Age Among U.S. Adults. Am. J. Prev. Med. 2020, 59, e197–e206. [Google Scholar] [CrossRef]
- Zhang, Z.; Jackson, S.L.; Martinez, E.; Gillespie, C.; Yang, Q. Association between Ultraprocessed Food Intake and Cardiovascular Health in US Adults: A Cross-Sectional Analysis of the NHANES 2011-2016. Am. J. Clin. Nutr. 2021, 113, 428–436. [Google Scholar] [CrossRef]
- Willett, W.C.; Sacks, F.; Trichopoulou, A.; Drescher, G.; Ferro-Luzzi, A.; Helsing, E.; Trichopoulos, D. Mediterranean Diet Pyramid: A Cultural Model for Healthy Eating. Am. J. Clin. Nutr. 1995, 61, 1402S–1406S. [Google Scholar] [CrossRef]
- Appel, L.J.; Sacks, F.M.; Carey, V.J.; Obarzanek, E.; Swain, J.F.; Miller, E.R.; Conlin, P.R.; Erlinger, T.P.; Rosner, B.A.; Laranjo, N.M.; et al. Effects of Protein, Monounsaturated Fat, and Carbohydrate Intake on Blood Pressure and Serum Lipids: Results of the OmniHeart Randomized Trial. JAMA 2005, 294, 2455–2464. [Google Scholar] [CrossRef]
- Nordmann, A.J.; Nordmann, A.; Briel, M.; Keller, U.; Yancy, W.S.; Brehm, B.J.; Bucher, H.C. Effects of Low-Carbohydrate vs Low-Fat Diets on Weight Loss and Cardiovascular Risk Factors: A Meta-Analysis of Randomized Controlled Trials. Arch. Intern. Med. 2006, 166, 285–293. [Google Scholar] [CrossRef]
- Thomazella, M.C.D.; Góes, M.F.S.; Andrade, C.R.; Debbas, V.; Barbeiro, D.F.; Correia, R.L.; Marie, S.K.N.; Cardounel, A.J.; daLuz, P.L.; Laurindo, F.R.M. Effects of High Adherence to Mediterranean or Low-Fat Diets in Medicated Secondary Prevention Patients. Am. J. Cardiol. 2011, 108, 1523–1529. [Google Scholar] [CrossRef]
- Mozaffarian, D.; Afshin, A.; Benowitz, N.L.; Bittner, V.; Daniels, S.R.; Franch, H.A.; Jacobs, D.R.; Kraus, W.E.; Kris-Etherton, P.M.; Krummel, D.A.; et al. Population Approaches to Improve Diet, Physical Activity, and Smoking Habits. Circulation 2012, 126, 1514–1563. [Google Scholar] [CrossRef]
- Rees, K.; Takeda, A.; Martin, N.; Ellis, L.; Wijesekara, D.; Vepa, A.; Das, A.; Hartley, L.; Stranges, S. Mediterranean-Style Diet for the Primary and Secondary Prevention of Cardiovascular Disease. Cochrane Database Syst. Rev. 2019, 3, CD009825. [Google Scholar] [CrossRef]
- Twisk, J.W.R. Applied Longitudinal Data Analysis for Epidemiology: A Practical Guide, 2nd ed.; Cambridge University Press: Cambridge, UK, 2013; ISBN 978-1-107-03003-9. [Google Scholar]
- Johns, D.J.; Lindroos, A.K.; Jebb, S.A.; Sjöström, L.; Carlsson, L.M.S.; Ambrosini, G.L. Tracking of a Dietary Pattern and Its Components over 10-Years in the Severely Obese. PLoS ONE 2014, 9, e97457. [Google Scholar] [CrossRef]
- Leal, D.B.; de Assis, M.A.A.; Hinnig, P.d.F.; Schmitt, J.; Soares Lobo, A.; Bellisle, F.; Di Pietro, P.F.; Vieira, F.K.; De Moura Araujo, P.H.; De Andrade, D.F. Changes in Dietary Patterns from Childhood to Adolescence and Associated Body Adiposity Status. Nutrients 2017, 9, 1098. [Google Scholar] [CrossRef]
- Luque, V.; Escribano, J.; Closa-Monasterolo, R.; Zaragoza-Jordana, M.; Ferré, N.; Grote, V.; Koletzko, B.; Totzauer, M.; Verduci, E.; ReDionigi, A.; et al. Unhealthy Dietary Patterns Established in Infancy Track to Mid-Childhood: The EU Childhood Obesity Project. J. Nutr. 2018, 148, 752–759. [Google Scholar] [CrossRef] [PubMed]
- Movassagh, E.Z.; Baxter-Jones, A.D.G.; Kontulainen, S.; Whiting, S.J.; Vatanparast, H. Tracking Dietary Patterns over 20 Years from Childhood through Adolescence into Young Adulthood: The Saskatchewan Pediatric Bone Mineral Accrual Study. Nutrients 2017, 9, 990. [Google Scholar] [CrossRef] [PubMed]
| Variables | Baseline Year | After 2 Years of Follow-Up | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Experimental | Control | Experimental | Control | |||||||||
| n (%) | n (%) | p | n (%) | n (%) | p | |||||||
| Sex | ||||||||||||
| Male | 705 (51.2) | 671 (48.8) | 0.270 * | 482 (51.1) | 462 (48.9) | 0.772 * | ||||||
| Female | 479 (48.9) | 500 (51.1) | 319 (50.3) | 315 (49.7) | ||||||||
| Age | ||||||||||||
| Adult | 684 (50.3) | 676 (49.7) | 0.983 * | 456 (49.6) | 464 (50.4) | 0.247 * | ||||||
| Elderly | 501 (50.3) | 496 (49.7) | 346 (52.5) | 310 (47.5) | ||||||||
| Economic Class | ||||||||||||
| A/B | 717 (50.1) | 714 (49.9) | 0.840 * | 475 (50.1) | 473 (49.9) | 0.832 * | ||||||
| C/D/E | 294 (50.6) | 287 (49.4) | 208 (50.7) | 202 (49.3) | ||||||||
| Acute Myocardial Infarction | ||||||||||||
| No | 587 (49.8) | 592 (50.2) | 0.635 * | 410 (49.9) | 411 (50.1) | 0.478 * | ||||||
| Yes | 597 (50.8) | 579 (49.2) | 389 (51.7) | 363 (48.2) | ||||||||
| Stroke | ||||||||||||
| No | 1041 (50.3) | 1030 (49.7) | 0.978 * | 702 (50.8) | 679 (49.2) | 0.935 * | ||||||
| Yes | 143 (50.3) | 141 (49.7) | 97 (50.5) | 95 (49.5) | ||||||||
| Aortic Aneurysm | ||||||||||||
| No | 1157 (50.2) | 1149 (49.8) | 0.495 * | 782 (50.6) | 763 (49.4) | 0.289 * | ||||||
| Yes | 27 (55.1) | 22 (44.9) | 17 (60.7) | 11 (39.3) | ||||||||
| Hypertension | ||||||||||||
| No | 111 (47.8) | 121 (52.2) | 0.427 * | 77 (45.3) | 93 (54.7) | 0.129 * | ||||||
| Yes | 1073 (50.6) | 1048 (49.4) | 722 (51.5) | 681 (48.5) | ||||||||
| Diabetes Mellitus | ||||||||||||
| No | 667 (50.9) | 643 (49.1) | 0.516 * | 459 (51.6) | 430 (48.4) | 0.449 * | ||||||
| Yes | 517 (49.6) | 526 (50.4) | 340 (49.7) | 344 (50.3) | ||||||||
| Total Cholesterol | ||||||||||||
| <190 mg/dL | 803 (49.6) | 817 (50.4) | 0.160 * | 455 (49.7) | 461 (50.3) | 0.635 * | ||||||
| ≥190 mg/dL | 382 (52.8) | 355 (47.2) | 173 (51.2) | 165 (48.8) | ||||||||
| LDL-Cholesterol | ||||||||||||
| <130 mg/dL | 951 (50.1) | 946 (49.9) | 0.454 * | 514 (49.8) | 519 (50.2) | 0.687 * | ||||||
| ≥130 mg/dL | 234 (52.3) | 226 (47.7) | 93 (51.4) | 88 (48.6) | ||||||||
| HDL-Cholesterol | ||||||||||||
| >40 mg/dL | 576 (49.1) | 598 (50.9) | 0.155 * | 349 (49.9) | 350 (50.1) | 0.851 * | ||||||
| ≤40 mg/dL | 571 (52.0) | 526 (48.0) | 270 (50.5) | 265 (49.5) | ||||||||
| Triglycerides | ||||||||||||
| <150 mg/dL | 617 (49.0) | 642 (51.0) | 0.097 * | 353 (49.5) | 360 (50.5) | 0.592 * | ||||||
| ≥150 mg/dL | 533 (52.5) | 482 (47.5) | 266 (51.1) | 255 (48.9) | ||||||||
| Glycemia | ||||||||||||
| <100 mg/dL | 498 (52.0) | 460 (48.0) | 0.216 * | 281 (51.6) | 263 (48.4) | 0.342 * | ||||||
| ≥100 mg/dL | 648 (49.3) | 665 (50.7) | 349 (48.9) | 364 (51.5) | ||||||||
| Body Mass Index | ||||||||||||
| Underweight | 25 (41.7) | 35 (58.3) | 16 (53.3) | 14 (46.7) | 0.428 * | |||||||
| Eutrophic | 278 (48.5) | 295 (51.5) | 0.196 * | 149 (47.1) | 167 (52.9) | |||||||
| Overweight/obesity | 877 (51.3) | 831 (48.7) | 502 (51.2) | 478 (48.8) | ||||||||
| Waist Circumference | ||||||||||||
| Adequate | 53 (47.3) | 59 (52.7) | 0.521 * | 32 (48.5) | 34 (51.5) | 0.753 * | ||||||
| Inadequate | 1122 (50.4) | 1133 (49.6) | 639 (50.5) | 627 (49.5) | ||||||||
| Physical Activity | ||||||||||||
| Active | 367 (49.5) | 374 (50.5) | 0.573 * | 448 (48.2) | 481 (51.8) | 0.012 | ||||||
| Inactive | 727 (50.8) | 704 (49.6) | 226 (55.7) | 180 (44.3) | ||||||||
| Smoking | ||||||||||||
| Never smoked | 461 (51.4) | 436 (48.6) | 0.638 * | 326 (53.3) | 286 (46.7) | 0.198 * | ||||||
| Former smoker | 632 (50.1) | 634 (49.9) | 428 (49.5) | 437 (50.5) | ||||||||
| Smoker | 87 (47.8) | 95 (52.2) | 44 (45.4) | 53 (54.6) | ||||||||
| Food Groups | Description |
|---|---|
| Rice and recipes | Rice and rice-based recipes |
| Olive oil | Extra virgin olive oil |
| Sugary drinks | Concentrated and pasteurized juices, natural and pulp juices with sugar, powdered juice, ready-made teas, soft drinks, milk with chocolate, chocolate drink, chocolate, fruit vitamin with sugar, milk with sugar (with or without coffee) |
| Meat and eggs | Beef, pork, goat meat, poultry and their recipes, eggs |
| Processed meats | Sausages, cold meats and canned meat |
| Cereals, breads and crackers | Polenta, couscous, pamonha (corn-paste wrapped in husks), cooked corn, oats, granola, quinoa, flaxseed, cereal bar, morning cereals with sugar, sugary children’s cereals, corn starch, porridges, salted biscuits, breads, sweet bread, stuffed bread, toast, panetone, sweet and homemade cookies, cakes |
| Sweets | Added sugar, sweets, chocolates, desserts, homemade and industrialized sweets |
| Beans | Beans and legumes |
| Fruits, natural juices | Fruit, dried fruit, natural juices or unsweetened pulp |
| Snacks | Pizza, sandwiches, chips. |
| Dairy products | Unsweetened milks, unsweetened fruit vitamin, yoghurts, dairy drinks |
| Butter and margarine | Butter and margarines with and without salt |
| Pasta | Pasta with or without sauce, stuffed pasta |
| Cheeses | White, yellow and processed cheeses |
| Vegetables | Raw, cooked or fried vegetables and their recipes |
| Food Groups | Food Patterns—Baseline Year | Food Patterns—First Year of Follow-Up | Food Patterns—Second Year of Follow-Up | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Traditional | Western | Snack | Cardioprotective | Traditional | Cardioprotective | Western | Snack | Traditional | Snack | Cardioprotective | Western | |
| Factor Load * | ||||||||||||
| Rice | 0.8193 | 0.0002 | −0.0289 | 0.0451 | 0.7367 | 0.0247 | −0.0293 | −0.0807 | 0.7833 | 0.0120 | 0.0937 | −0.0058 |
| Pasta | −0.3068 | 0.3377 | 0.0585 | 0.0265 | −0.0960 | −0.2391 | 0.3637 | 0.0703 | −0.4666 | −0.0135 | 0.2739 | 0.1628 |
| Beans | 0.6922 | −0.0085 | 0.0596 | −0.0004 | 0.6793 | 0.0572 | −0.1083 | 0.0581 | 0.6356 | 0.1701 | 0.2042 | 0.0200 |
| Vegetables | 0.1771 | −0.0806 | −0.0556 | 0.6897 | 0.2769 | 0.6732 | −0.1340 | −0.0299 | 0.1846 | −0.0154 | 0.5930 | −0.0623 |
| Fruits and juices | −0.2003 | −0.5305 | 0.0277 | 0.3315 | −0.2562 | 0.3863 | −0.5068 | 0.0351 | −0.1488 | 0.0036 | 0.2557 | −0.4343 |
| Meat and eggs | 0.4875 | 0.2725 | 0.0157 | 0.2178 | 0.6072 | 0.1762 | 0.3021 | −0.0317 | 0.3965 | −0.1931 | 0.5731 | 0.0854 |
| Fish | −0.0836 | −0.3108 | −0.2139 | −0.1851 | −0.1868 | −0.1126 | −0.2698 | −0.2100 | 0.0485 | −0.0576 | −0.3594 | −0.0147 |
| Processed meats | −0.0660 | 0.3438 | 0.0620 | 0.1281 | −0.0945 | 0.1996 | 0.4206 | 0.1589 | −0.0258 | 0.3502 | −0.0721 | 0.1580 |
| Butter and margarine | 0.0355 | 0.0189 | 0.6500 | −0.0746 | 0.0523 | 0.0121 | 0.1632 | 0.5826 | 0.1076 | 0.6051 | −0.0333 | 0.1782 |
| Breads, cereals and crackers | −0.0095 | 0.0138 | 0.7400 | −0.0124 | −0.0820 | −0.0322 | 0.0202 | 0.7324 | 0.0196 | 0.7421 | −0.0356 | −0.0279 |
| Sweets and desserts | −0.1255 | 0.4280 | 0.1581 | 0.0845 | −0.2056 | 0.1342 | 0.3564 | −0.0479 | −0.2163 | 0.1288 | 0.1328 | 0.4897 |
| Snacks | −0.1761 | 0.4003 | −0.3048 | 0.0792 | −0.3064 | 0.2026 | 0.2000 | −0.3542 | −0.2242 | −0.2037 | 0.0662 | 0.5412 |
| Sugary drinks | 0.0483 | 0.6404 | −0.0807 | −0.0791 | −0.0316 | 0.0418 | 0.6446 | 0.0057 | 0.096 | 0.0551 | −0.0066 | 0.7284 |
| Dairy products | −0.0401 | −0.1483 | 0.5637 | 0.1339 | −0.0261 | 0.1754 | −0.1603 | 0.5346 | 0.0199 | 0.4942 | 0.1519 | −0.2213 |
| Cheeses | −0.2155 | 0.1484 | 0.1091 | 0.5269 | −0.1951 | 0.4756 | 0.2175 | 0.1766 | −0.3495 | 0.2600 | 0.3486 | −0.0729 |
| Olive oil | 0.0840 | −0.1040 | −0.0137 | 0.6043 | 0.0516 | 0.6379 | 0.1038 | 0.0009 | −0.004 | 0.1101 | 0.5631 | 0.0240 |
| Variance (%) | 11.46% | 10.63% | 9.28% | 8.05% | 12.32% | 9.91% | 9.27% | 7.71% | 12.25% | 9.76% | 9.47% | 8.14% |
| Food Groups | Food Patterns—Baseline Year | Food Patterns—First Year of Follow-Up | Food Patterns—Second Year of Follow-Up | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Traditional | Snack | Cardioprotective | Western | Traditional | Cardioprotective | Western | Snack | Traditional | Cardioprotective | Snack | Western | |
| Factor Load * | ||||||||||||
| Rice | 0.8092 | −0.0353 | 0.1162 | −0.0107 | 0.7767 | 0.0023 | −0.0950 | −0.0262 | 0.7716 | 0.0429 | −0.0505 | 0.0297 |
| Pasta | −0.2046 | 0.0282 | −0.1869 | 0.3245 | −0.1580 | −0.2167 | 0.3478 | −0.0511 | −0.1962 | −0.0194 | −0.0467 | 0.2836 |
| Beans | 0.7871 | 0.0058 | −0.0509 | 0.0561 | 0.7139 | −0.0242 | −0.0059 | −0.0391 | 0.6801 | −0.0115 | −0.0300 | −0.036 |
| Vegetables | −0.1025 | 0.1168 | 0.5026 | −0.3194 | −0.1376 | 0.5521 | −0.1191 | −0.028 | −0.1377 | 0.5733 | 0.0615 | −0.2435 |
| Fruits and juices | 0.1776 | −0.0372 | 0.6898 | −0.0274 | 0.2136 | 0.5625 | 0.1217 | 0.0816 | 0.2673 | 0.6202 | 0.0055 | −0.0568 |
| Meat and eggs | 0.3919 | −0.2389 | 0.0321 | −0.0317 | 0.6020 | 0.0416 | 0.2101 | 0.0353 | 0.5985 | 0.0569 | −0.0019 | 0.0964 |
| Fish | 0.0720 | 0.0880 | 0.0682 | 0.6170 | −0.0427 | −0.0873 | 0.4692 | 0.3557 | 0.1395 | −0.2221 | 0.2431 | 0.3197 |
| Processed meats | 0.0201 | 0.0634 | 0.1355 | −0.0970 | −0.1483 | 0.1091 | −0.0864 | −0.0749 | −0.1195 | 0.2141 | −0.1711 | −0.0057 |
| Butter and margarine | 0.1285 | 0.5144 | 0.0061 | 0.3229 | 0.1121 | −0.0576 | 0.0168 | 0.5226 | 0.1571 | −0.1075 | 0.3842 | 0.2802 |
| Breads, cereals and crackers | −0.1105 | 0.6650 | 0.0951 | 0.1067 | −0.0398 | 0.1074 | −0.1102 | 0.7322 | −0.0445 | −0.0913 | 0.5289 | 0.1051 |
| Sweets and desserts | −0.0273 | −0.1202 | 0.0120 | 0.4320 | −0.1639 | 0.0991 | 0.4203 | 0.0415 | −0.093 | 0.0793 | −0.2381 | 0.4181 |
| Snacks | −0.1943 | −0.1542 | −0.0013 | 0.3006 | −0.2218 | 0.0197 | 0.4950 | −0.2359 | −0.1138 | 0.0415 | −0.2631 | 0.5664 |
| Sugary drinks | 0.0774 | −0.0930 | −0.1972 | 0.4945 | 0.1123 | −0.0252 | 0.7123 | −0.0732 | 0.1246 | −0.0205 | 0.1117 | 0.7166 |
| Dairy products | −0.0343 | 0.7033 | −0.0672 | −0.1694 | −0.1151 | 0.5571 | −0.2174 | 0.0641 | −0.1406 | 0.1762 | 0.7161 | −0.0482 |
| Cheeses | −0.1827 | 0.2461 | 0.3945 | 0.2735 | −0.2232 | 0.3950 | 0.2884 | 0.3782 | −0.1935 | 0.5815 | 0.1067 | 0.2725 |
| Coffee and tea | −0.1034 | −0.3592 | 0.1813 | 0.2296 | −0.0884 | −0.4414 | 0.0108 | 0.4326 | −0.0747 | −0.0496 | −0.5422 | 0.0677 |
| Olive oil | 0.0196 | −0.0603 | 0.6099 | 0.0820 | 0.2083 | 0.4024 | 0.1781 | 0.1634 | 0.2418 | 0.5639 | 0.0884 | 0.0478 |
| Variance (%) | 11.67% | 10% | 9.04% | 7.95% | 12.02% | 10.34% | 9.10% | 8.13% | 11.83% | 9.88% | 9.18% | 7.80% |
| Variables | Baseline Year | Second Year of Follow-Up | ||||||
|---|---|---|---|---|---|---|---|---|
| Western | p | Cardioprotective | p | Western | p | Cardioprotective | p | |
| Sex | ||||||||
| Male | 0.113 (1.06) | <0.001 * | 0.074 (1.03) | 0.002 * | 0.121 (1.03) | <0.001 * | 0.092 (1.02) | 0.001 * |
| Female | −0.166 (0.86) | −0.106 (0.93) | −0.179 (0.91) | −0.139 (0.94) | ||||
| Age | ||||||||
| Adult | 0.093 (1.05) | <0.001 * | 0.025 (1.01) | 0.312 | 0.056 (1.06) | 0.067 | 0.045 (0.98) | 0.142 |
| Elderly | −0.126 (0.90) | −0.034 (0.98) | −0.074 (0.90) | −0.059 (1.01) | ||||
| Economic Class | ||||||||
| A/B | 0.031 (1.01) | 0.215 | −0.049 (0.95) | 0.600 | −0.008 (0.94) | 0.361 | −0.121 (0.95) | 0.057 |
| C/D/E | −0.055 (1.02) | −0.084 (0.94) | −0.080 (0.95) | 0.030 (0.97) | ||||
| BMI | ||||||||
| Underweight | 0.129 (0.64) | 0.539 | −0.406 (0.70) | 0.037 * | 0.073 (0.99) | 0.154 | −0.181 (0.79) | 0.099 |
| Eutrophic | −0.050 (0.97) | −0.069 (1.00) | −0.134 (0.83) | 0.164 (0.96) | ||||
| Overweight /obesity | 0.001 (1.01) | 0.035 (1.00) a | 0.040 (1.01) | −0.014 (0.95) | ||||
| WC | ||||||||
| Adequate | 0.234 (0.82) | 0.071 | −0.308 (0.64) | 0.020 * | 0.221 (1.08) | 0.202 | 0.200 (1.10) | 0.248 |
| Inadequate | −0.016 (0.99) | 0.019 (1.01) | −0.009 (0.99) | −0.008 (0.99) | ||||
| FA | ||||||||
| Active | 0.044 (1.01) | 0.254 | −0.045 (0.95) | 0.924 | −0.042 (0.94) | 0.153 | 0.049 (0.93) | 0.269 |
| Inactive | −0.029 (0.99) | −0.039 (0.96) | 0.075 (1.01) | −0.037 (1.00) | ||||
| Smoking | ||||||||
| Never smoked | −0.056 (0.94) a | 0.011* | −0.019 (0.96) | 0.853 | −0.077 (1.00) | 0.178 | 0.077 (1.01) | 0.140 |
| Former smoker | 0.001 (1.01) | 0.013 (1.05) | 0.053 (0.99) | −0.065 (1.00) | ||||
| Smoker | 0.295 (1.17) | 0.016 (0.81) | 0.083 (1.01) | 0.059 (0.85) | ||||
| Variables | Baseline Year | Second Year of Follow-Up | ||||||
|---|---|---|---|---|---|---|---|---|
| Western | p | Cardioprotective | p | Western | p | Cardioprotective | p | |
| Sex | ||||||||
| Male | 0.158 (1.08) | <0.001 * | 0.049 (1.04) | 0.048 | 0.144 (1.08) | <0.001 * | 0.032 (1.07) | 0.268 |
| Female | −0.212 (0.83) | −0.067 (0.92) | −0.210 (0.828) | −0.047 (0.87) | ||||
| Age | ||||||||
| Adult | 0.078 (1.00) | 0.002 * | 0.003 (0.99) | 0.912 | 0.063 (1.02) | 0.031 * | −0.030 (0.98) | 0.309 |
| Elderly | −0.107 (0.98) | −0.004 (1.01) | −0.093 (0.95) | 0.044 (1.02) | ||||
| Economic Class | ||||||||
| A/B | −0.226 (0.98) | 0.414 | −0.030 (0.99) | 0.120 | −0.010 (1.01) | 0.704 | −0.045 (0.96) | 0.500 |
| C/D/E | 0.034 (1.010 | 0.078 (1.02) | −0.042 (0.90) | 0.008 (0.94) | ||||
| BMI | ||||||||
| Underweight | −0.122 (0.95) | 0.132 | 0.073 (1.01) | 0.326 | −0.268 (0.97) | 0.236 | 0.100 (0.90) | 0.763 |
| Eutrophic | −0.090 (1.00) | −0.072 (0.91) | 0.128 (1.04) | −0.027 (0.92) | ||||
| Overweight /obesity | 0.037 (0.99) | 0.025 (1.02) | −0.021 (0.98) | 0.031 (1.02) | ||||
| WC | ||||||||
| Adequate | −0.071 (0.88) | 0.566 | −0.001 (0.95) | 0.986 | 0.267 (1.13) | 0.182 | −0.211 (1.02) | 0.159 |
| Inadequate | 0.005 (1.01) | 0.002 (1.00) | 0.031 (0.99) | 0.031 (0.99) | ||||
| FA | ||||||||
| Active | 0.103 (1.07) | 0.009* | −0.028 (0.96) | 0.647 | 0.015 (0.98) | 0.281 | 0.041 (0.98) | 0.316 |
| Inactive | −0.062 (0.95) | 0.001 (1.02) | 0.110 (1.05) | −0.044 (0.96) | ||||
| Smoking | ||||||||
| Never smoked | −0.106 (0.90) a | <0.001 * | 0.006 (0.99) | 0.994 | −0.054 (0.98) | 0.012 * | 0.099 (1.03) | 0.090 |
| Former smoker | 0.022 (1.01) | 0.002 (0.98) | −0.010 (0.96) | −0.048 (0.98) | ||||
| Smoker | 0.332 (1.24) | −0.005 (1.13) | 0.385 (1.29) | −0.135 (0.89) | ||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Coura, A.G.L.; Arruda Neta, A.d.C.P.d.; Lima, R.L.F.C.d.; Bersch-Ferreira, Â.C.; Weber, B.; Vianna, R.P.d.T. Tracking of Dietary Patterns in the Secondary Prevention of Cardiovascular Disease after a Nutritional Intervention Program—A Randomized Clinical Trial. Nutrients 2022, 14, 4716. https://doi.org/10.3390/nu14224716
Coura AGL, Arruda Neta AdCPd, Lima RLFCd, Bersch-Ferreira ÂC, Weber B, Vianna RPdT. Tracking of Dietary Patterns in the Secondary Prevention of Cardiovascular Disease after a Nutritional Intervention Program—A Randomized Clinical Trial. Nutrients. 2022; 14(22):4716. https://doi.org/10.3390/nu14224716
Chicago/Turabian StyleCoura, Amanda Gonçalves Lopes, Adélia da Costa Pereira de Arruda Neta, Rafaela Lira Formiga Cavalcanti de Lima, Ângela Cristine Bersch-Ferreira, Bernardete Weber, and Rodrigo Pinheiro de Toledo Vianna. 2022. "Tracking of Dietary Patterns in the Secondary Prevention of Cardiovascular Disease after a Nutritional Intervention Program—A Randomized Clinical Trial" Nutrients 14, no. 22: 4716. https://doi.org/10.3390/nu14224716
APA StyleCoura, A. G. L., Arruda Neta, A. d. C. P. d., Lima, R. L. F. C. d., Bersch-Ferreira, Â. C., Weber, B., & Vianna, R. P. d. T. (2022). Tracking of Dietary Patterns in the Secondary Prevention of Cardiovascular Disease after a Nutritional Intervention Program—A Randomized Clinical Trial. Nutrients, 14(22), 4716. https://doi.org/10.3390/nu14224716







