Abstract
The relationship between neighborhood food environment and childhood obesity is complex and not yet well defined by current research in China, especially when considering the integrated effects with other relative factors. The main purpose of this article is to introduce a framework of children’s weight status, based on their neighborhood food environment, and to identify the impact of food environment on the children’s BMI and potential pathways. The participants of this cross-sectional study were students aged 8–16.5 years old and their parents. Two conceptual frameworks were tested using the structural equation modeling method, and two models were extracted. Model B added the neighborhood food environment based on model A. By comparing the two models, the neighborhood environment was potentially correlated with the children’s BMI directly and may have a positive impact on unhealthy-food eating behaviors, which were positively associated with the children’s BMI. The results suggest that the focus should be placed on the integrated effects of the potential risk factors of childhood obesity, based on considering the neighborhood food environment, which may relate to children’s unhealthy-food eating behaviors and weight status.
1. Introduction
An alarming increase in childhood obesity has attracted widespread interest in the fields of public health, nutrition, and psychology, during the past two decades. According to the World Health Organization’s latest report, nearly one-fifth of children and adolescent aged 5 to 18 have suffered from overweight and obesity [1]. In China, this rate has jumped by 17% in the last thirty-five years [2], and it is predicted that roughly one-third of children and adolescents will be overweight and obese by 2030 [3]. It is worth highlighting that the prevalence of childhood obesity differs in different areas due to discrepancies in economic development and the variety of eating habits. For example, some metropolitan areas such as the Jiangsu province, the Zhejiang province, and Shanghai witnessed significant increases in 2017 (31.6%) [4], 2015 (20.2%) [5], and 2014 (31.6%) [6], respectively. Despite much of the research in recent years having focused on identifying potential relative risk factors and practical intervention approaches, this increasing rate is still on an upward trend. This is because of the complexity of the risk factors of childhood obesity. It is generally recognized that genetics, behavior, diet, socioeconomic status, and physical activity are essential influencing aspects of childhood obesity. Among these, with the exception of genetic factors, the factors are believed to be easily modified and managed and have generated considerable research interest in obesity intervention.
Previous studies on childhood obesity modeling have pointed out that parental feeding behaviors [7], parental socioeconomic status [8,9,10], and the child’s food intake [11,12] are considered vital and fundamental potential factors. Moreover, nutritional education has been considered the most practical and financially friendly method to tackle the obesity pandemic around the world. A growing number of earlier works demonstrated that nutritional knowledge has a positive impact on reducing childhood obesity [13,14]. However, there is no research reporting the integrated effects of these factors on children’s weight in China. Consequently, it is difficult to understand the correlation between the potential risk factors and children’s weight status.
In addition, in recent years, several studies have revealed that environmental factors potentially increase the prevalence of obesity among children and adults, as these factors strongly impact people’s lifestyles [15,16,17,18]. Theoretically, an unhealthy neighborhood food environment leads to unhealthy-food eating. For example, the number of fast-food restaurants is significantly correlated to the fast-food intake of residents [19]. Similarly, the number of supermarket/convenience stores may increase access to unhealthy snacks, which can be directly associated with gain weight [20]. Unfortunately, there is little evidence reported from China regarding this. The research by Zhou M et al. [21] and the research by Zhang M et al. [22] reported that the food environment has an impact on obesity among middle-aged and older adults in China. However, there is little evidence for this among children and adolescents. Zhou PL and his colleagues discovered that Western-style fast-food is positively correlated with adolescents’ body mass index (BMI), while Chinese-style fast-food is negatively associated with the BMI of adolescents. They also pointed out that the positive impacts of Chinese-style fast-food and fresh vegetables and fruits have gradually disappeared in recent years [23]. Furthermore, no attention has been paid to the integrating effect of a healthy- or unhealthy-food environment on children’s weight status. Consequently, it is still unclear how neighborhood food environment impacts children’s food intake and weight. Fortunately, the structural equation modeling (SEM) method can be used to clarify the casual, direct, and indirect relationship between the latent and dependent variables [24].
Therefore, to bridge this gap, this study aimed to introduce two integrated models, applying a combination of four basic concepts (family socioeconomic status, neighborhood food environment, parental feeding behaviors, and children’s unhealthy-food intake) and the nutritional knowledge level of both the children and their parents (or caregivers). Additionally, these factors were compared to identify the relationship between neighborhood food environment and the children’s BMI.
2. Materials and Methods
2.1. Research Framework
To identify the effect of a child’s neighborhood environment on their BMI, we designed two different frameworks. Framework A presented the logical relationship between the family’s socioeconomic status, parental feeding behaviors, children’s unhealthy-food eating behaviors, nutritional knowledge level, and the children’s BMI. Framework B illustrated the additional effect of the child’s neighborhood food environment on their BMI, based on framework A. Family socioeconomic status was an independent variable, and the neighborhood food environment, parental feeding behaviors, children’s unhealthy-food eating behaviors, and parent’s and children’s nutrition knowledge levels were four mediators. The children’s BMI was the dependent variable. The research framework is demonstrated in Figure 1.

Figure 1.
Research framework. Framework a: the model demonstrated the integrated effects of family, parent, and children’s characteristics on the children’s BMI.; Framework b: the model included the potential impact of the neighborhood food environment based on framework a on the children’s BMI.Child’s BMI was calculated by this formula: BMI = weight(kg)/[height(m)]2).
2.2. Participants
The present study included 4970 children aged 8–16.5 years old, as well as their parents, from 36 schools participating in the National Surveillance of Nutritional Health Status of Rural Students in Compulsory Education project. This is a community-based children’s health survey that was conducted from October to December in 2021 in the coastal–rural area of Zhejiang, China. Fornell and his colleagues suggested that the minimum sample size for SEM analysis highly depends on the complexity of the model and the measurements of the model characteristics [25]. Consequently, this study required at least 300 participants, according to the characteristics of our theoretical model (Appendix A).
2.3. Measurement of Variables
As the dependent variable, the children’s BMI was calculated using the following formula: BMI = weight(kg)/[height(m)]2. Their weight was measured by trained investigators, using the Jian min Weight Scale (GMCS-I Type) (manufactured in China), and rounded to 0.1 kg. Their height was measured twice, with the Jian min Height Scale (GMCS-I Type) (manufactured in China), and recorded in meters (m), with an accuracy of 0.1 m. Each student’s weight and height were measured twice, and the average values were used to calculate the child’s BMI. According to the Chinese diagnostic method for overweight and obesity among school-aged children and adolescents, WS/T-2018 [26], the children’s weight was classified into four categories: underweight, normal, overweight, and obese (Table 1).

Table 1.
The socio-demographic characteristics of the children participants.
2.4. Family Socioeconomic Status
A family’ socioeconomic status was based on the family’s income level and parental education level. The families’ incomes were classified into six groups: “less than CNY 20,000/year”, “CNY 20,000–49,000/year”, ”CNY 50,000–99,000/year”, “CNY 100,000–199,000/year”, and “CNY ≥200,000/year” (CNY 10,000 = USD1389.7768). With respect to education level, the responses obtained were categorized as “less than primary school”, “elementary school”, “secondary school”, “high school”, “Bachelor’s”, and “Master’s and Ph.D.”.
2.5. Neighborhood Food Environment
The neighborhood food environment was assessed based on the number of fast-food restaurants, Chinese-style restaurants, fruit and vegetable stores, supermarkets/convenience stores, and milk tea shops/bakeries/dessert shops. The neighborhood was defined as being within the scope of 500 m from the resident’s home.
2.6. Children’s Unhealthy-Food Eating Behaviors
The frequency of eating snacks, sugary beverages, and deep-fried foods was categorized as “less than 1 time/week”, “1∼2 times/week”, “3∼4 times/week”, “5∼6 times/week”, “1 time/day” and “≥2 times/day”. The respondents were asked about the money spent on buying snacks, and the responses were denoted as “less than CNY 1/day”, “CNY 1∼3.9/day”, “CNY 4∼6.9/day”, “CNY 7∼9.9/day”, and “more than CNY 10/day”. (CNY 1 = USD 0.138).
2.7. Parental Feeding Behaviors and Nutritional Knowledge Level
The parental feeding behaviors only considered the behaviors that might be directly associated with the children’s unhealthy-food eating. These included buying snacks and sugar-sweetened drinks for the child. Parents indicated their responses on a four-point scale (“never”, “1∼2 times/month”, “3∼4 times/month” and “more than 2 times/week”), regarding how often they buy certain foods for their children. The nutritional knowledge level was measured based on the 10 standard questions. Appendix B presents the standard questions used for measuring the parents’ and children’s nutritional knowledge level.
2.8. Statistical Analysis
Proportions were calculated as percentages of the categorical variables. The multiple imputation method was used for the estimation of missing values in the SAS 9.4 software (the missing values included 1023 data from 14 variables, and the missing rate ranged from 1.32 to 13.9%).
Latent variables, such as family socioeconomic status, neighborhood food environment, parental feeding behaviors, and children’s unhealthy-food eating behaviors, were identified using exploratory factor analysis (EFA) with 14 nutrition questionnaire items. EFA and Cronbach’s α test were undertaken using the IBM SPSS Statistics Version 23.0 software. The Kaiser–Meyer–Olkin and Bartlett’s tests of sphericity were used to evaluate the data adequacy and suitability. A Kaiser–Meyer–Olkin value of >0.5 and a Bartlett’s test of sphericity with a p value of <0.05 indicated that the data were qualified for use in the principal component analysis [27]. To determine the number of factors, the Kaiser’s criterion (eigenvalues > 1.0), the screen test, and parallel analysis were used [28]. The items with absolute factor loadings > 0.3 were retained [27]. To determine the internal consistency, the ordinal α coefficient (ordinal equivalent of Cronbach’s α) was estimated [27], for which values greater than 0.6 were considered as acceptable [25]. Furthermore, the average variance extracted (AVE) was used to test the reliability of the study questionnaire; the AVE values of each latent variable should be equal or higher than 0.5.
After the EFA, confirmatory factor analysis was conducted to evaluate the measurement model. In addition, pathway analysis was used to test the hypothesized direct and indirect relationships between the latent variables and dependent variables [29], using the IBM AMOSTM Version 23.0 software(IBM (International Business Machines Corporation) and SPSS company, New York, NY, USA). In SEM, maximum likelihood is the foundational estimation technique required, as the data must meet the normality standard. Thus, a normality analysis was conducted. To evaluate the models’ fits, the following goodness-of-fit indices were assessed: Chi-square, the goodness-of-fit index (GFI), the comparative fit index (CFI) the Tucker–Lewis index [TLI], and the root mean square standard error of approximation (RMSEA). For GFI, CFI, and TLI, values greater than 0.9 implied an acceptable fit, and values greater than 0.95 were considered a good fit [30]. For RMSEA, values smaller than 0.08 indicated an acceptable fit, and values smaller than 0.06 meant a good fit. In the SEM method, the direct and indirect effects can be estimated, and, if their values were 0.1, 0.3, and 0.5, they were considered small, medium, and strong effects, respectively [31].
3. Results
3.1. Descriptive Statistical Analysis
This study consisted of 4970 students from 18 primary and 18 secondary schools (the third to ninth grades), which included 52.70% boys and 47.30% girls in the coastal–rural areas of the Zhejiang province. The number of primary school students accounted for 56.34% of the children who participated, and the number of students from secondary schools was 43.66%. The average age of students was approximately 11.8 years old, and their average weight was 43.98 Kg. Concerning the children’s weight status, 6.62% of the children were underweight, 72.60% of the children were normal weight, and 27.41% of the children were overweight and obese (overweight: 15.86% and obese: 11.55%) (Table 1).
In terms of the neighborhood food environment, more than half of the students responded that there were no fast-food restaurants in their neighborhood, while merely 2.2% of the students reported that there were more than five fast-food restaurants local to them. Similarly, the proportion of students living in areas without bakeries/milk tea shop/cafés in the neighborhood was 41.95%; however, for the students who lived in areas with more bakeries/milk tea shops/cafés, this figure was only 6.22%. A total of 15.88% of the students ate snacks daily; however, the figure for students who drank sugar-sweetened beverages was only about 4.35%. Regarding family conditions, most of the parent’s educational levels were at secondary school and high school levels (fathers: 68.25% and mothers: 65.49%). Moreover, 64.95% of the students’ families’ yearly income was between CNY 50,000–199,000. In terms of parental feeding, 88.85% and 90.42% of the parents bought snacks and sugary beverages for their children less than 2 times/month, respectively (Appendix A).
3.2. SEM Analysis
Validity and Reliability
In terms of the study’s validity, the Cronbach’s alpha of the four latent variables ranged from 0.601 to 0.864, and all of them met the acceptable criteria of internal consistency. Additionally, in terms of the reliability of the latent constructs, with the exception of the children’s unhealthy-food eating behaviors, the other construct values were higher than 0.5 and considered to be acceptable (Table 2).

Table 2.
The average variance extracted (AVE), Cronbach’s alpha, and composite reliabilities of the latent constructs in the model of neighborhood food environment correlates of childhood and adolescent obesity.
3.3. Exploratory Factor Analysis
Table 3 presents the results of the EFA conducted on 14 items, which extracted four factors with eigenvalues > 1.0 and explained 61.09% of the total variance. The Kaiser–Meyer–Olkin value (0.768) indicated sampling adequacy, and Bartlett’s test of sphericity (χ2 = 19393.89, p < 0.0001) satisfied the required criteria (p < 0.05) and supported the factorability of the dataset. The items with absolute factor loadings > 0.3 were retained.

Table 3.
Exploratory factor analysis with Varimax rotation and internal consistency for factors and their respective items.
3.4. The Model Fit Analysis
The values of the model A fit indices were as follows: GFI = 0.986, TLI = 0.946, and CFI = 0.960, The model’s goodness-of-fit was accepted (χ2/df = 5.706, p < 0.001, RMSEA = 0.022, 90% CI: 0.020–0.023). The values of the model B fit indices were as follows: GFI = 0.98, TLI = 0.966, and CFI = 0.972. The model’s goodness-of-fit was accepted (χ2/df = 4.480, p < 0.001, RMSEA = 0.019, 90% CI: 0.018–0.020).
3.5. Structural Model
To identify the effect of the neighborhood food environment on children’s BMI and potential pathways, two structural models were applied in this study; they are presented in Figure 2 and Figure 3.
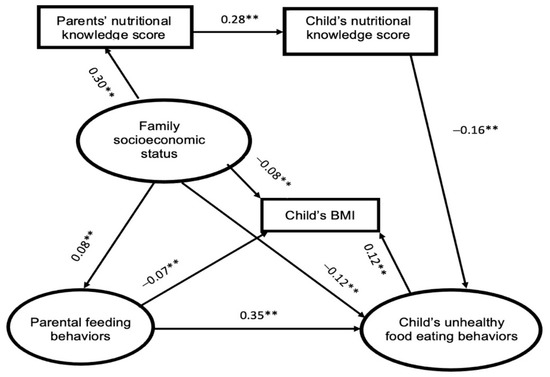
Figure 2.
Model A (the solid line represents statistically significant values. ** p < 0.0001).
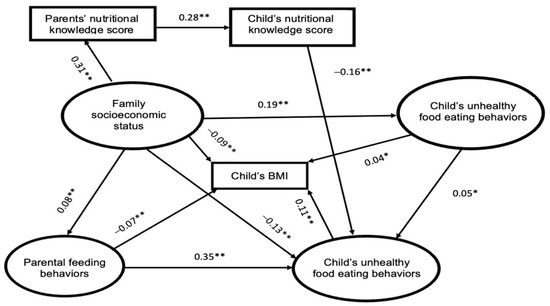
Figure 3.
Model B (the solid line represents statistically significant values. * p < 0.05; ** p < 0.0001).
The data shown in Figure 2 revealed that family socioeconomic status has a positive impact on parents’ nutritional knowledge levels and parental feeding behaviors, while it has a negative influence on children’s unhealthy-food eating behaviors and children’s BMI. Similarly, the parents’ nutritional knowledge level was positively associated with the children’s nutritional knowledge, which was negatively correlated with the unhealthy-food eating behaviors of children. However, a converse relationship also appeared between the parental feeding behaviors and the children’s BMI. Moreover, children’s unhealthy-food eating behaviors significantly increased the children’s BMI. Medium effects can be seen between the parental feeding behaviors and the children’s unhealthy-food eating behaviors, as well as between the family’s socioeconomic status and the parents’ nutritional knowledge level.
Figure 3 shows that the neighborhood food environment was related to the children’s BMI in direct and indirect ways. Two pathways were mapped out: in the first pathway, the neighborhood food environment was a mediator between the family’s socioeconomic status and the unhealthy-food eating habits of children; it is evident that the socioeconomic status was positively associated with the neighborhood food environment, which has a positive impact on the children’s unhealthy eating behaviors. The second pathway demonstrated the direct and positive relationship between the neighborhood food environment and the children’s BMI. The relationship between the other constructs was similar to that of the results shown in Figure 2.
The indirect effect of the family’s socioeconomic status, in regard to parents’ nutrition knowledge, significantly decreased the children’s BMI (model A: −0.0016, p < 0.001; model B: −0.0015, p < 0.001). Moreover, the indirect effect of the family’s socioeconomic status, in terms of parental feeding behaviors, also decreased the children’s BMI (model A: −0.0056, p < 0.001; model B: −0.0056, p < 0.001). In addition, the indirect effect of the family’s socioeconomic status, through the children’s unhealthy-food eating behaviors, reduced the children’s BMI. (model A: −0.014, p < 0.001; model B: −0.014, p < 0.001). However, the indirect effect of the family’s socioeconomic status, through parental feeding behaviors and the children’s unhealthy-food eating behaviors, increased the children’s BMI (model A: 0.0034, p < 0.001; model B: 0.0031, p < 0.001). The indirect effect of the family’s socioeconomic status, in terms of the neighborhood environment, significantly increased the children’s BMI (model B: 0.0076, p < 0.001). Similar results can also be seen in the indirect effect of the family’s socioeconomic status via the neighborhood environment and the children’s unhealthy-food eating behaviors (model B: 0.0076, 0.0001, p < 0.001). Moreover, the indirect effect of parental feeding behaviors, in terms of the children’s unhealthy-food eating, dramatically increased the children’s BMI (model A: 0.042, p < 0.001; model B: 0.0385, p < 0.001). With the exception of the indirect impacts, the parents’ nutritional knowledge, in regard to the children’s nutritional knowledge levels and the children’s unhealthy-food eating behaviors, was found to have a positive impact on reducing the children’s BMI in both models (model A: −0.0054, p < 0.001; model B: −0.0049, p < 0.001). Additionally, the indirect effect of the children’s nutritional knowledge levels, in terms of the children’s unhealthy-food eating behaviors, was also correlated with a decrease in the children’s BMI (model A: −0.0192, p < 0.001; model B: −0.0176, p < 0.001).
4. Discussion
The total prevalence rate of overweight and obesity was 27.23%, which is considerably higher than the national level (19% in 2020) [32] and the international level (20% in 2016) [1], and lower than the prevalence rate among children and adolescents in the Jiangsu province, China (33.2% in 2019–2020) [33]; Shanghai, China (30.31% in 2019) [34]; Maya, Mexico (39%) [35]; and Thrace, NE Greece (48.5% in 2018) [36]. This study examined a conceptual and multi-factorial model and offered an understanding of the intricate relationship between children’s neighborhood food environment and their BMI by applying SEM. The children’s BMI was the primary dependent variable, and the family’s socioeconomic status was the primary independent variable. Two types of models were extracted from our data, based on our hypothesized model, which had a good fit. A direct and positive relationship can be seen between the family’s socioeconomic status and the children’s BMI, as well as between the parental feeding behaviors and the children’s BMI. Conversely, a direct and negative relationship can be seen between the neighborhood food environment and the children’s BMI, as well as between the unhealthy-food eating behaviors and the children’s BMI.
Four latent constructs were extracted, using the exploratory factor analysis, and their validity and reliability were evaluated according to the value of the average variance extracted (AVE), Cronbach’s alpha, and composite reliabilities (CR). The data indicated that, with the exception of the AVE value of the children’s unhealthy-food eating behaviors, the other latent constructs met the acceptable value standards. However, Fornell and D. F. Larcker suggested that if the AVE is between 0.4 to 0.5, and the composite reliabilities of the latent constructs are higher than 0.6, this indicates that the convergent validity of the construct is still adequate [25]. Therefore, the validity and reliability of the four latent variables of this study met the acceptable criteria.
According to the structural models, in model A, the conceptual relationship between the family’s economic status, parental feeding behaviors, the children’s unhealthy-food eating behaviors, the nutritional knowledge level, and the children’s BMI were demonstrated to be statistically significant. Family socioeconomic status was inversely associated with the children’s weight status in this study. This suggested that parents with higher incomes and higher educational levels are more likely to have a positive influence on their children’s weight control. Similar results have been documented in previous research, conducted by Huang H et al. [10], Crouch, P et al. [37], and Sares-Jaske L et al. [38]. Moreover, the data in our study revealed that a high family socioeconomic status has a positive impact on the parents’ nutritional knowledge levels, which are directly associated with the children’s nutritional knowledge levels in both models. It is logical that a parent’s higher educational background may lead to obtaining a higher socioeconomic status and a higher level of nutritional knowledge. Furthermore, the parents with a higher level of nutritional knowledge were more likely to teach their children more regarding nutritional education. Simultaneously, they might also guide their children toward healthy eating and help them to form good eating habits. This finding was in line with the previous literature on childhood obesity [39,40,41], except that parental feeding behaviors were found to significantly increase children’s unhealthy-food intake in both models. This is consistent with the results obtained in the study by Gevers DWM et al., who found that parental feeding behaviors can contribute to the specific food intakes of children by controlling and monitoring children’s eating behaviors [42]. For example, unhealthy parental feeding behaviors, such as a lack of monitoring [43], or over-restricting [44], the children’s unhealthy-food intake, have detrimental impacts on child weight control. Therefore, this is evidence that reasonable parental monitoring is more likely to lead to children having healthier eating habits. Regarding children’s unhealthy-food eating behaviors, such as a high consumption of fast-food, sugar-sweetened beverages, and deep-fried foods (e.g., chips, fried chicken, fried noodles, and so on), are the main risk factor for childhood obesity [44,45,46,47,48]. Similarly, this study demonstrated that children’s unhealthy-food eating behaviors are a crucial mediator between the other three latent constructs and the children’s BMI.
In comparison to model A, the data in model B indicated that the neighborhood food environment may have a positive impact on children’s BMI via two pathways: (1) the direct association between the neighborhood food environment and children’s BMI; (2) indirectly, via mediation of the children’s unhealthy-food eating behaviors. This finding was consistent with the study by Shier V et al., which demonstrated that greater exposure to fast-food restaurants, supermarkets, and convenience stores was correlated with a higher BMI among youth in the USA [49]. Moreover, a systematic review conducted in China reported that the neighborhood food environment had an impact on the diet and obesity of the residents [50]. Similar evidence from South Korea reported that unhealthy behaviors of children were linked to the neighborhood environment, and a greater availability of fast-food restaurants and convenience stores was more likely positively associated with increases in children’s BMI, among the children who had obesity [51]. It is worth mentioning that the integrated impact was positive, but not considered strong. The neighborhood food environment in this study not only included unhealthy-food environments, such Western fast-food restaurants, convenience stores/supermarkets, and bakeries/cafés/milk tea shops, but also included healthy-food environments, such as Chinese-style fast-food restaurants and fruit and vegetable stores. In this model, the family’s socioeconomic status had a positive impact on the neighborhood environment. A possible explanation is that the family’s socioeconomic status plays a key role in the neighborhood’s socioeconomic condition, which was recognized as a vital determinant of obesity prevalence among the Chinese population [22]. Therefore, it can be concluded that the total impact of the neighborhood food environment on the participants was more likely to increase the children’s BMI.
5. Limitations
Due to the cross-sectional nature of this study, it was difficult to determine the temporal relationships. We suggest that the model of the current study could be tested using longitudinal data, which may provide researchers with clearer and more accurate causal relationships. Moreover, there were limitations in the data collection; we did not collect data regarding neighborhood security, physical activity, sleep time, and built environments, which are deemed remarkable factors in causing childhood obesity. Therefore, it is recommended that these factors are studied in future investigations. Additionally, the present study focused only on the proximal environment; however, the macro environment, including socioeconomic conditions, political policies, and the neighborhood environment of schools, was not measured in the research framework used in this study. We also recommend that future studies take these factors into consideration.
6. Conclusions
This study identified the intricate relationship between the neighborhood food environment and children’s BMI. The findings provide a foundation for our follow-up intervention study, which will be conducted next year. The findings of this study suggest that the focus should be placed on the integrated effects of the potential risk factors of childhood obesity, based on considering the neighborhood food environment, which may be related to children’s unhealthy-food eating behaviors and weight status. This study provides some evidence for the childhood obesity model, based on the neighborhood food environment.
Author Contributions
R.Z. designed and managed the research, T.A. interpreted the data, and contributed to subsequent manuscript writing and discussion. D.Z. and R.Z. collected the data; T.A. performed the data analysis. All authors have read and agreed to the published version of the manuscript.
Funding
This research was supported in part by the Intervention Effect of Intensive lifestyle on Overweight and Obesity in Adolescent Children project supported by Health Commission of Zhejiang Province (No. 2022RC123).
Institutional Review Board Statement
The study was approved by the Ethics Committee of the Institute of Nutrition and Health of the Chinese Center for Disease Control and Prevention (No. 2021-018).
Informed Consent Statement
All participants provided written informed consent before participating in this study.
Data Availability Statement
The data supporting the findings of the study are available from the corresponding author on reasonable request.
Acknowledgments
The authors thank the Surveillance of Nutritional Health Status of Rural Students in Compulsory Education project leader Zhang Qian and other coworkers for their instruction. Meanwhile, the authors are also sincerely grateful for the supports of the schools, families and the local Centers for Disease Control and other investigators. The authors also sincerely appreciate the insightful suggestions of Yuan Changzheng and her student Huang Yuhui.
Conflicts of Interest
The authors declare no conflict of interest.
Appendix A

Table A1.
Minimum sample size required for SEM analysis.
Table A1.
Minimum sample size required for SEM analysis.
| Model Characteristics (Number of Latent Constructs and Items) Minimum Sample Required | |
|---|---|
| 1. Five or less latent constructs. Each latent construct has more than three measurement items. | 100 samples |
| 2. Seven or less latent constructs. Each construct has more than three items. | 150 samples |
| 3. Seven or less latent constructs. Some constructs have less than three items (the identified model) | 300 samples |
| 4. More than seven latent constructs. Some constructs have less than three items (the identified model) | 500 samples |

Table A2.
The descriptive statistics of the latent variables characters.
Table A2.
The descriptive statistics of the latent variables characters.
| Variables | Number | Percentage |
|---|---|---|
| The number of fast-food restaurants | ||
| 0 | 2626 | 52.84 |
| 1∼2 | 1806 | 36.34 |
| 3∼5 | 428 | 8.61 |
| >5 | 110 | 2.21 |
| The number of Chinese-style restaurants | ||
| 0 | 1338 | 26.92 |
| 1∼2 | 1694 | 34.08 |
| 3∼5 | 1035 | 20.82 |
| >5 | 903 | 18.17 |
| The number of fruit and vegetable stores | ||
| 0 | 1029 | 20.70 |
| 1∼2 | 2111 | 42.47 |
| 3∼5 | 1248 | 25.11 |
| >5 | 582 | 11.71 |
| The number of supermarket/convenience store | ||
| 0 | 335 | 6.74 |
| 1∼2 | 2336 | 47.00 |
| 3∼5 | 1690 | 34.00 |
| >5 | 609 | 12.25 |
| The number of Milk Tea Shop/Bakery/Dessert Shop | ||
| 0 | 2085 | 41.95 |
| 1∼2 | 1861 | 37.44 |
| 3∼5 | 715 | 14.39 |
| >5 | 309 | 6.22 |
| Mothers’ education | ||
| Less than primary school | 150 | 3.02 |
| Elementary | 483 | 9.72 |
| Secondary school | 2112 | 42.49 |
| High school | 1143 | 23.00 |
| Bachelor | 1064 | 21.41 |
| Master and PhD | 18 | 0.36 |
| Fathers’ education | ||
| Less than primary school | 127 | 2.56 |
| Elementary | 383 | 7.71 |
| Secondary school | 2167 | 43.60 |
| High school | 1275 | 25.65 |
| Bachelor | 982 | 19.76 |
| Master and PhD | 36 | 0.72 |
| Family’s income | ||
| less than 20,000 RMB/year | 443 | 8.91 |
| 20,000–49,000 RMB/year | 1084 | 21.81 |
| 50,000–99,000 RMB/year | 1685 | 33.90 |
| 100,000–199,000 RMB/year | 1543 | 31.05 |
| ≥200,000 RMB/year | 215 | 4.33 |
10,000 RMB = 1389.7768 USD.

Table A3.
Normality analysis.
Table A3.
Normality analysis.
| Indicators | Skew | Kurtosis |
|---|---|---|
| parent’s nutrition knowledge score | −0.98 | 1.749 |
| children’s nutritional knowledge score | −0.554 | 0.095 |
| BMI | 0.745 | 0.326 |
| Deep-fried food | 1.816 | 5.162 |
| Buying sugar-sweetened beverages | 0.503 | −0.729 |
| Buying snacks | 0.283 | −0.653 |
| Fathers’ education | −0.083 | −0.298 |
| Mothers’ education | −0.118 | −0.466 |
| Family income | −0.262 | −0.65 |
| Sugar-sweetened beverages | 1.557 | 2.803 |
| money for buying snack | 0.626 | −0.701 |
| Snacks | 0.686 | −0.261 |
| Milk Tea Shop/Bakery/Dessert Shop/Café | 0.786 | −0.173 |
| Supermarket/convenience store | 0.277 | −0.499 |
| Fruit and vegetable stores | 0.277 | −0.743 |
| Chinese-style restaurants | 0.218 | −1.171 |
| Fast food restaurants | 1.085 | 0.802 |
To increase the validity of the latent constructs, it is worthy to test the multicollinearity in a study. There is demonstrated that correlation among the four latent variables by using double arrows. The value exceeds 0.85 means a high correlation between the two latent constructs [1]. The results from Figure 3 indicated that there is no high correlation exist among the present study variables.

Figure A1.
Multicollinearity Analysis.
Appendix B
- Nutritional knowledge questionary for children
- How many types of food should school-age children eat per day?
[1] 4 types [2] 6 types [3] 10 types [4] 12 types [4] 15 types
- 2.
- Which nutrients are a good source of fresh fruits and vegetables:
[1] carbohydrates [2] fat [3] protein [4] vitamins [5] are not known
- 3.
- Among the following foods, the foods with the richest high-quality protein are:
[1] Milk [2] Cereals and potatoes [3] Vegetables and fruits [4] Meat, eggs [5] I don’t know
- 4.
- Which of the following foods is a good source of calcium?
[1] Milk [2] Cereals and potatoes [3] Vegetables and fruits [4] Meat, eggs [5] I don’t know
- 5.
- How to prevent iron deficiency anemia?
[1] Eat more meat and fresh fruits and vegetables [2] Drink more milk [3] Eat light food [4] Eat more rice steamed buns [5] I don’t know
- 6.
- What diseases are likely to be caused by eating salty food regularly?
[1] Diabetes [2] High blood pressure [3] Hyperlipidemia [4] I don’t know
- 7.
- How long do you think children and adolescents should be moderately vigorously active each day? [1] More than 10 min [2] More than 30 min [3] More than 60 min [4] More than 90 min [5] Don’t know
(Note: “Moderate-to-vigorous physical activity” refers to exercise that requires moderate or heavy effort, resulting in a significant increase in heart rate or shortness of breath. Such as brisk walking, dancing, running, climbing, swimming, skipping rope, football, volleyball, basketball, etc. )
- 8.
- How long do you think children and adolescents should look at electronic screens (including computers, mobile phones, pads, etc.) every day?
[1] 60 min [2] 90 min [3] 120 min [4] 150 min
- 9.
- What are the dangers of drinking sugary drinks to children’s bodies? (Multiple selections possible)
[1] Caries [2] Overweight and obese [3] Hepatitis [4] I don’t know
- 10.
- Which of the following methods can help maintain a healthy weight? (Multiple choices are possible)
[1] Moderate diet [2] Active exercise [3] Only eat what you like to eat [4] I don’t know
- Nutritional knowledge questionary for parents
- Varied food is better for balanced nutrition.
[1] Correct [2] Incorrect [3] I don’t know
- 2.
- You can eat fruits instead of vegetables.
[1] Correct [2] Incorrect [3] I don’t know
- 3.
- Milk and soybeans are rich in calcium and high-quality protein, so they should eat more appropriately.
[1] Correct [2] Incorrect [3] I don’t know
- 4.
- Proper eating of fish, poultry and eggs, lean meat, and fresh vegetables and fruits can prevent iron deficiency anemia
[1] Correct [2] Incorrect [3] I don’t know
- 5.
- Cereals are rich in high-quality protein
[1] Correct [2] Incorrect [3] I don’t know
- 6.
- To drink enough water, it is recommended that adults drink 7-8 glasses of water a day, and it is recommended to drink plain water.
[1] Correct [2] Incorrect [3] I don’t know
- 7.
- How many grams of salt should adults eat per person per day?
[1] Know, no more than g [2] do not know
- 8.
- Your child should do at least 60 min of moderate-intensity or more physical activity each day
Note: Physical activity of moderate intensity and above refers to activities that increase breathing and heartbeat.
[1] Correct [2] Incorrect [3] I don’t know
- 9.
- Children should not spend more than 2 h a day looking at electronic screens (including computers, mobile phones, pads, etc.).
[1] Correct [2] Incorrect [3] I don’t know
- 10.
- Children who are underweight or too high are prone to illness.
[1] Correct [2] Incorrect [3] I don’t know
References
- World Health Organization. Global Health Observatory Online Database Table BMIPLUS1CWBv; WHO: Geneva, Switzerland, 2021. [Google Scholar]
- Report on Nutrition and Chronic Diseases of Chinese Residents (2020). J. Agric. Prod. Mark. 2021, 58–59.
- Ma, G.; Mi, J.; Ma, J. Report on Childhood Obesity in China; People’s Health Publishing House: Beijing, China, 2017. [Google Scholar]
- Jing, Z.; Juan, Z.; Jie, Y.; Yan, W.; Xiyan, Z.; Fengyun, Z. Analysis on the status and influencing factors of overweight and obesity in children and adolescents in Jiangsu Province. Chin. Sch. Health 2019, 40, 778–780. [Google Scholar] [CrossRef]
- Fang, G.; Ronghua, Z.; Dan, L.; Jia, M.; Haifeng, H. Analysis on the influencing factors of simple obesity in children and adolescents in Zhejiang Province. Chin. Sch. Hyg. 2015, 36, 231–235. [Google Scholar]
- Yang, Y.; Wu, Y.; Wang, X.; Peng, N. Study on the influencing factors of overweight and obesity behavior among primary and middle school students in Shanghai. Chin. Sch. Health 2019, 40, 12–19. [Google Scholar] [CrossRef]
- Doub, A.E.; Small, M.; Birch, L.L. A call for research exploring social media influences on mothers’ child feeding practices and childhood obesity risk. Appetite 2016, 99, 298–305. [Google Scholar] [CrossRef]
- Andrews, K.R.; Silk, K.S.; Eneli, I.U. Parents as health promoters: A theory of planned behavior perspective on the prevention of childhood obesity. J. Health Commun. 2010, 15, 95–107. [Google Scholar] [CrossRef]
- Nau, C.; Schwartz, B.S.; Bandeen-Roche, K.; Liu, A.; Pollak, J.; Hirsch, A.; Lisa, B.D.; Glass, T.A. Community socioeconomic deprivation and obesity trajectories in children using electronic health records. Obesity 2015, 23, 207–212. [Google Scholar] [CrossRef]
- Huang, H.; Radzi, C.; Jenatabadi, H.S. Family Environment and Childhood Obesity: A New Framework with Structural Equation Modeling. Int. J. Environ. Res. Public Health 2017, 14, 181. [Google Scholar] [CrossRef]
- Mandal, B.; Powell, L.M. Childcare choices, food intake, and children’s obesity status in the United States. Econ. Hum. Biol. 2014, 14, 50–61. [Google Scholar] [CrossRef]
- Khajeheian, D.; Colabi, A.M.; Shah, N.; Radzi, C.; Jenatabadi, H.S. Effect of social media on Child Obesity: Application of Structural Equation Modeling with the Taguchi Method. Int. J. Environ. Res. Public Health 2018, 15, 1343. [Google Scholar] [CrossRef]
- Meseri, R.; Ergin, I.; Mermer, G.; Hassoy, H.; Yoruk, S.; Catalgol, S. School based multifaceted nutrition intervention decreased obesity in a high school: An intervention study from Turkey. Prog. Nutr. 2017, 19, 373–383. [Google Scholar]
- Meseri, R.; Mermer, G.; Ergin, I.; Hassoy, H. Evaluation of obesity prevalence and nutritional knowledge in adolescents in a semi urban area of Turkey. Prog. Nutr. 2015, 17, 58–67. [Google Scholar]
- Elgaard Jensen, T.; Kleberg Hansen, A.K.; Ulijaszek, S.; Munk, A.K.; Madsen, A.K.; Hillersdal, L.; Jespersen, A.P. Identifying notions of environment in obesity research using a mixed-methods approach. Obes. Rev. 2019, 20, 621–630. [Google Scholar] [CrossRef]
- Kirk, S.F.; Penney, T.L.; McHugh, T.L. Characterizing the obesogenic environment: The state of the evidence with directions for future research. Obes. Rev. 2010, 11, 109–117. [Google Scholar] [CrossRef]
- Jia, P. Obesogenic environment and childhood obesity. Obes. Rev. 2021, 22, 3. [Google Scholar] [CrossRef]
- Sun, B.D.; Yan, H.; Zhang, T.L. Built environmental impacts on individual mode choice and BMI: Evidence from China. J. Transp. Geogr. 2017, 63, 11–21. [Google Scholar] [CrossRef]
- Jia, P.; Luo, M.; Li, Y.; Zheng, J.S.; Xiao, Q.; Luo, J. Fast-food restaurant, unhealthy eating, and childhood obesity: A systematic review and meta-analysis. Obes. Rev. 2021, 22 (Suppl. 1), e12944. [Google Scholar] [CrossRef]
- Xin, J.; Zhao, L.; Wu, T.; Zhang, L.; Li, Y.; Xue, H.; Xiao, Q.; Wang, R.; Xu, P.; Visscher, T.; et al. Association between access to convenience stores and childhood obesity: A systematic review. Obes. Rev. 2021, 22 (Suppl. 1), e12908. [Google Scholar] [CrossRef]
- Zhou, M.; Tan, S.; Tao, Y.; Lu, Y.; Zhang, Z.; Zhang, L.; Yan, D. Neighborhood socioeconomics, food environment and land use determinants of public health: Isolating the relative importance for essential policy insights. Land Use Policy 2017, 68, 246–253. [Google Scholar] [CrossRef]
- Zhang, M.; Guo, W.; Zhang, N.; He, H.; Zhang, Y.; Zhou, M.; Zhang, J.; Li, M.; Ma, G. Association between Neighborhood Food Environment and Body Mass Index among Older Adults in Beijing, China: A Cross-Sectional Study. Int. J. Environ. Res. Public Health 2020, 17, 7658. [Google Scholar] [CrossRef]
- Zhou, P.L.; Li, R.F.; Liu, K. The Neighborhood Food Environment and the Onset of Child-Hood Obesity: A Retrospective Time-Trend Study in a Mid-sized City in China. Front. Public Health 2021, 9, 1066. [Google Scholar] [CrossRef]
- Schreiber, J.B. Update to core reporting practices in structural equation modeling. Res. Soc. Adm. Pharm. 2017, 13, 634–643. [Google Scholar] [CrossRef]
- Fornell, C.; Larcker, D.F. Evaluating structural equation models with unobservable variables and measurement error. J. Mark. Res. 1981, 18, 39–50. [Google Scholar] [CrossRef]
- National Health Commission of PRC. WS/T586-2018 Screening for Overweight and Obesity among School-Age Children and Adolescents; Standards Press of China: Beijing, China, 2018. [Google Scholar]
- Tabachnick, B.; Fidell, L. Using Multivariate Statistics; Allyn & Bacon, Inc.: Needham, MA, USA, 2007. [Google Scholar]
- Snook, S.C.G.; Richard, L. Component analysis versus common factor analysis: A Monte Carlo study. Psychol. Bull. 1989, 106, 148–154. [Google Scholar] [CrossRef]
- Anderson, J.; Gerbing, D. Structural equation mod- eling in practice: A review and recommended two-step approach. Psychol. Bull. 1988, 103, 411–423. [Google Scholar] [CrossRef]
- Keith, T.Z. Multiple Regression and Beyond; Pearson Education: Boston, MA, USA, 2006. [Google Scholar]
- Kline, T.J.; Klammer, J.D. Path model analyzed with ordinary least squares multiple regression versus LISREL. J. Psychol. Interdiscip. Appl. 2001, 135, 213–225. [Google Scholar] [CrossRef]
- Report on Nutrition and Chronic Disease Status of Chinese Residents. J. Nutr. 2020, 42, 52.
- Chen, S.A.; Zhang, X.Y.; Du, W.; Fan, L.J.; Zhang, F.Y. Association of insufficient sleep and skipping breakfast with overweight/obesity in children and adolescents: Findings from a cross-sectional provincial surveillance project in Jiangsu. Pediatr. Obes. 2022, 17, e12950. [Google Scholar] [CrossRef]
- Chen, H.; Wang, L.J.; Xin, F.; Liang, G.; Chen, Y. Associations between sleep duration, sleep quality, and weight status in Chinese children and adolescents. BMC Public Health 2022, 22, 1136. [Google Scholar] [CrossRef]
- May-Kim, S.; Pena-Espinoza, B.I.; Menjivar, M. Malnutrition in Maya children: High prevalence of linear growth deficiency. Am. J. Biol. Anthropol. 2022, 177, 620–629. [Google Scholar] [CrossRef]
- Dampoudani, N.; Giakouvaki, A.; Diamantoudi, D.; Skoufi, G.; Kontogiorgis, C.A.; Constantinidis, T.C.; Nena, E. Physical Activity, Body Mass Index (BMI) and Abdominal Obesity of Pre-Adolescent Children in the Region of Thrace, NE Greece, in Relation to Socio-Demographic Characteristics. Children 2022, 9, 340. [Google Scholar] [CrossRef]
- Crouch, P.; O’dea, J.A.; Battisti, R. Child feeding practices and perceptions of childhood overweight and childhood obesity risk among mothers of preschool children. Nutr. Diet. 2007, 64, 151–158. [Google Scholar] [CrossRef]
- Sares-Jaske, L.; Gronqvist, A.; Maki, P.; Tolonen, H.; Laatikainen, T. Family socioeconomic status and childhood adiposity in Europe—A scoping review. Prev. Med. 2022, 160, 107095. [Google Scholar] [CrossRef]
- Espinosa-Curiel, I.E.; Pozas-Bogarin, E.E.; Lozano-Salas, J.L.; Martinez-Miranda, J.; Delgado-Perez, E.E.; Estrada-Zamarron, L.S. Nutritional Education and Promotion of Healthy Eating Behaviors among Mexican Children through Video Games: Design and Pilot Test of FoodRateMaster. JMIR Serious Games 2020, 8, e16431. [Google Scholar] [CrossRef]
- Gibson, E.L.; Androutsos, O.; Moreno, L.; Flores-Barrantes, P.; Socha, P.; Iotova, V.; Cardon, G.; De Bourdeaudhuij, I.; Koletzko, B.; Skripkauskaite, S.; et al. Influences of Parental Snacking-Related Attitudes, Behaviours and Nutritional Knowledge on Young Children’s Healthy and Unhealthy Snacking: The ToyBox Study. Nutrients 2020, 12, 432. [Google Scholar] [CrossRef]
- Xu, J.L. The Roles of Family and School Members in Influencing Children’s Eating Behaviours in China: A Narrative. Children 2022, 9, 315. [Google Scholar] [CrossRef]
- Gevers, D.W.M.; Kremers, S.P.J.; de Vries, N.K.; van Assema, P. Clarifying concepts of food parenting practices. A Delphi study with an application to snacking behavior. Appetite 2014, 79, 51–57. [Google Scholar] [CrossRef]
- Klesges, R.C.; Stein, R.J.; Eck, L.H.; Isbell, T.R.; Klesges, L.M. Parental influence on food selection in young children and its relationships to childhood obesity. Am. J. Clin. Nutr. 1991, 53, 859–864. [Google Scholar] [CrossRef]
- Clark, H.R.; Goyder, E.; Bissell, P.; Blank, L.; Peters, J. How do parents’ child-feeding behaviours influence child weight? Implications for childhood obesity policy. J. Public Health 2007, 29, 132–141. [Google Scholar] [CrossRef]
- Patterson, R.; Risby, A.; Chan, M.Y. Consumption of takeaway and fast food in a deprived inner London Borough: Are they associated with childhood obesity? BMJ Open 2012, 2, e000402. [Google Scholar] [CrossRef]
- Hamano, T.; Li, X.J.; Sundquist, J.; Sundquist, K. Association between Childhood Obesity and Neighbourhood Accessibility to Fast-Food Outlets: A Nationwide 6-Year follow-up Study of 944,487 Children. Obes. Facts 2017, 10, 559–568. [Google Scholar] [CrossRef] [PubMed]
- Macintyre, A.K.; Marryat, L.; Chambers, S. Exposure to liquid sweetness in early childhood: Artificially sweetened and sugar-sweetened beverage consumption at 4–5 years and risk of overweight and obesity at 7–8 years. Pediatr. Obes. 2018, 13, 755–765. [Google Scholar] [CrossRef] [PubMed]
- Shang, X.W.; Liu, A.L.; Zhang, Q.; Hu, X.Q.; Du, S.M.; Ma, J.; Xu, G.F.; Li, Y.; Guo, H.W.; Du, L.; et al. Report on Childhood Obesity in China (9): Sugar-sweetened Beverages Consumption and Obesity. Biomed. Environ. Sci. 2012, 25, 125–132. [Google Scholar]
- Shier, V.; An, R.; Sturm, R. Is there a robust relationship between neighborhood food environment and childhood obesity in the USA? Public Health 2012, 126, 723–730. [Google Scholar] [CrossRef] [PubMed]
- An, R.P.; He, L.; Shen, J. Impact of neighborhood food environment on diet and obesity in China: A systematic review. Public Health Nutr. 2020, 23, 457–473. [Google Scholar] [CrossRef] [PubMed]
- Choo, J.; Kim, H.J.; Park, S. Neighborhood Environments: Links to Health Behaviors and Obesity Status in Vulnerable Children. West. J. Nurs. Res. 2017, 39, 1169–1191. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).