Iron Deficiency in Adolescent and Young Adult German Athletes—A Retrospective Study
Abstract
1. Introduction
2. Material and Methods
2.1. Study Design and Participants
2.2. Blood Collection and Preparation
2.3. Anthropometric Data
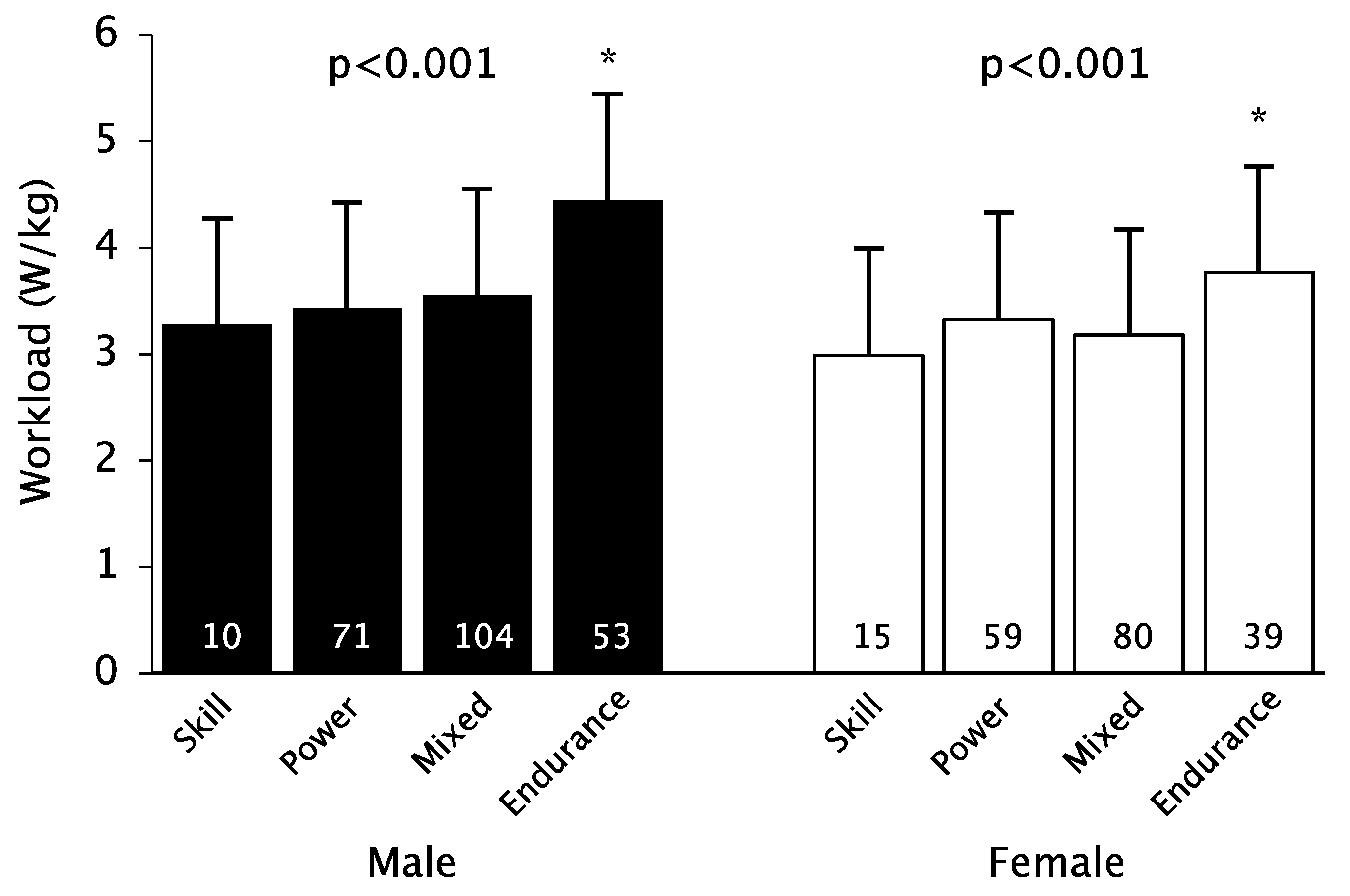
2.4. Ergometry
2.5. Statistical Analysis
3. Results
4. Discussion
5. Limitations
- Athletes should eat an iron-rich diet taking into account vegetarian and vegan diets.
- Athletes should be monitored for iron levels at least once a year, and adolescent competitive athletes and women, in particular, should be monitored and treated more intensively.
- In case of insufficient dietary iron intake and iron deficiency, drug therapy should be taken into account (for points 2 and 3 age, type of sport, and performance status must be considered; for example, the indication of iron supplementation in a female middle-distance runner prior to international competition would be much more generous).
- An uncontrolled iron substitution should not take place.
6. Future Research
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Lieu, P.T.; Heiskala, M.; Peterson, P.A.; Yang, Y. The roles of iron in health and disease. Mol. Asp. Med. 2001, 22, 1–87. [Google Scholar] [CrossRef]
- Mettler, S. Ferrum—Ein Mineralstoff im Sport. Schweiz. Z. Für Sportmed. Und Sport. 2004, 52, 105–114. [Google Scholar]
- Burden, R.J.; Morton, K.; Richards, T.; Whyte, G.P.; Pedlar, C.R. Is iron treatment beneficial in, iron-deficient but non-anaemic (IDNA) endurance athletes? A systematic review and meta-analysis. Br. J. Sports Med. 2015, 49, 1389–1397. [Google Scholar] [CrossRef] [PubMed]
- Conrad, M.E.; Umbreit, J.N. Pathways of iron absorption. Blood.Cells Mol. Dis. 2002, 29, 336–355. [Google Scholar] [CrossRef] [PubMed]
- Peters, H.P.F.; De Vries, W.R.; Vanberge-Henegouwen, G.P.; Akkermans, L.M.A. Potential benefits and hazards of physical activity and exercise on the gastrointestinal tract. Gut 2001, 48, 435–439. [Google Scholar] [CrossRef]
- Warner, D.C.; Schnepf, G.; Barrett, M.S.; Dian, D.; Swigonski, N.L. Prevalence, attitudes, and behaviors related to the use of nonsteroidal anti-inflammatory drugs (NSAIDs) in student athletes. J. Adolesc. Health 2002, 30, 150–153. [Google Scholar] [CrossRef]
- Friedmann, B. Sportleranämie. Dtsch. Z. Sportmed. 2001, 52, 262–263. [Google Scholar]
- Hallberg, L.; Hulthen, L. High serum ferritin is not identical to high iron stores. Am. J. Clin. Nutr. 2003, 78, 1225–1226. [Google Scholar] [CrossRef][Green Version]
- Zoller, H.; Vogel, W. Iron supplementation in athletes-first do no harm. Nutrition 2004, 20, 615–619. [Google Scholar] [CrossRef]
- Stupnicki, R.; Malczewska, J.; Milde, K.; Hackney, A.C. Day to day variability in the transferring receptor/ferritin index in female athletes. Br. J. Sports Med. 2003, 37, 267–269. [Google Scholar] [CrossRef]
- Robinson, Y.; Cristancho, E.; Böning, D. Die Hypoferritinämie des Sportlers ist kein sicheres Indiz für Eisenmangel. Dtsch. Z. Sport. 2010, 61, 141–145. [Google Scholar]
- Malczewska, J.; Blach, W.; Stupnicki, R. The effects of physical exer-cise on the concentrations of ferritin and transferrin receptor in plas-ma of female judoists. Int. J. Sports. Med. 2000, 21, 175–179. [Google Scholar] [CrossRef] [PubMed]
- Murray-Kolb, L.E.; Beard, J.L.; Joseph, L.J.; Davey, S.L.; Evans, W.J.; Campbell, W.W. Resistance training affects iron status in older men and women. Int. J. Sport. Nutr. Exerc. Metab. 2001, 11, 287–298. [Google Scholar] [CrossRef] [PubMed]
- Birkeland, K.I.; Stray-Gundersen, J.; Hemmersbach, P.; Hallen, J.; Haug, E.; Bahr, R. Effect of rhEPO administration on serum levels of sTfRand cycling performance. Med. Sci. Sports. Exerc. 2000, 32, 1238–1243. [Google Scholar] [CrossRef]
- Clénin, G.; Cordes, M.; Huber, A.; Schumacher, Y.O.; Noack, P.; Scales, J.; Kriemler, S. Iron deficiency in sports—Definition, influence on performance and therapy. Swiss Med. Wkly. 2015, 145, w14196. [Google Scholar] [CrossRef] [PubMed]
- WHO. Guideline: Daily Iron Supplementation in Infants and Children; Committee GR; World Health Organization (WHO): Switzerland, Geneva, 2016. [Google Scholar]
- Sekhar, D.L.; Murray-Kolb, L.E.; Kunselman, A.R.; Weisman, C.S.; Paul, I.M. Association between menarche and iron deficiency in non-anemic young women. PLoS ONE 2017, 12, e0177183. [Google Scholar] [CrossRef]
- Schleiffenbaum, B.; Viollier, E.; Wegmller, E.; Viollier, A.; Stettler, E. Unexpected high prevalence of metabolic disorders and chronic disease among young male draftees—The Swiss Army XXI experience. Swiss Med. Wkly. 2006, 18, 136, 175–184. [Google Scholar] [CrossRef]
- Sim, M.; Garvican-Lewis, L.A.; Cox, G.R.; Govus, A.; McKay, A.K.A.; Stellingwerff, T.; Peeling, P. Iron considerations for the athlete: A narrative review. Eur. J Appl. Physiol. 2019, 119, 1463–1478. [Google Scholar] [CrossRef]
- Koehler, K.; Braun, H.; Achtzehn, S.; Hildebrand, U.; Predel, H.G.; Mester, J.; Schänzer, W. Iron status in elite young athletes: Gender-dependent influences of diet and exercise. Eur. J. Appl. Physiol. 2012, 112, 513–523. [Google Scholar] [CrossRef]
- Castell, L.M.; Nieman, D.C.; Bermon, S.; Peeling, P. Exercise-Induced Illness and Inflammation: Can Immunonutrition and Iron Help? Int. J. Sport Nutr. Exerc. Metab. 2019, 29, 181–188. [Google Scholar] [CrossRef]
- Pelliccia, A.; Adami, P.E.; Quattrini, F.; Squeo, M.R.; Caselli, S.; Verdile, L.; Maestrini, V.; Di Paolo, F.; Pisicchio, C.; Ciardo, R.; et al. Are Olympic athletes free from cardiovascular diseases? Systematic investigation in 2352 participants from Athens 2004 to Sochi 2014. Br. J. Sports Med. 2017, 51, 238–243. [Google Scholar] [CrossRef] [PubMed]
- Kuwabara, A.M.; Tenforde, A.S.; Do, J.T.F.; Fredericson, M. Iron deficiency in athletes: A narrative review. PM&R 2022, 14, 620–642. [Google Scholar] [CrossRef]
- Hunt, J.R. Moving toward a plant-based diet: Are iron and zinc at risk? Nutr. Rev. 2002, 60, 127–134. [Google Scholar] [CrossRef] [PubMed]
- Rogerson, D. Vegan diets: Practical advice for athletes and exercisers. J. Int. Soc. Sports Nutr. 2017, 14, 36. [Google Scholar] [CrossRef]
- Beard, J.L. Iron Requirements in Adolescent Females. J. Nutr. 2000, 130, 440S–442S. [Google Scholar] [CrossRef]
- Daily, J.P.; Stumbo, J.R. Female Athlete Triad. Prim. Care Clin. Off. Pract. 2018, 45, 615–624. [Google Scholar] [CrossRef]
- Beard, J.; Tobin, B. Iron status and exercise. Am. J. Clin. Nutr. 2000, 72, 594S–597S. [Google Scholar] [CrossRef]
- Phillips, F. Vegetarian nutrition. Nutr. Bull. 2005, 30, 132–167. [Google Scholar] [CrossRef]
- Stoffel, N.U.; Cercamondi, C.I.; Brittenham, G.; Zeder, C.; Geurts-Moespot, A.J.; Swinkels, D.W.; Moretti, D.; Zimmermann, M.B. Iron absorption from oral iron supplements given on consecutive versus alternate days and as single morning doses versus twice-daily split dosing in iron-depleted women: Two open-label, randomised controlled trials. Lancet Haematol. 2017, 4, e524–e533. [Google Scholar] [CrossRef]
- Schaap, C.; Hendriks, J.C.; Kortman, G.A.; Klaver, S.M.; Kroot, J.J.; Laarakkers, C.M.; Wiegerinck, E.T.; Tjalsma, H.; Janssen, M.C.; Swinkels, D.W. Diurnal Rhythm rather than Dietary Iron Mediates Daily Hepcidin Variations. Clin. Chem. 2013, 59, 527–535. [Google Scholar] [CrossRef]
- Harris, S.S. The Effect of Calcium Consumption on Iron Absorption and Iron Status. Nutr. Clin. Care 2002, 5, 231–235. [Google Scholar] [CrossRef] [PubMed]
- Vadhan-Raj, S.; Strauss, W.; Ford, D.; Bernard, K.; Boccia, R.; Li, J.; Allen, L.F. Efficacy and safety of IV ferumoxytol for adults with iron deficiency anemia previously unresponsive to or unable to tolerate oral iron. Am. J. Hematol. 2014, 89, 7–12. [Google Scholar] [CrossRef] [PubMed]
- MacDougall, I.C. Evolution of IV iron compounds over the last century. J. Ren. Care 2009, 35, 8–13. [Google Scholar] [CrossRef]
- The Prohibited List|World Anti-Doping Agency. Available online: https://www.wada-ama.org/en/prohibited-list?q=intravenous%20infusions (accessed on 9 September 2022).
- Klingshirn, L.A.; Pate, R.R.; Bourque, S.P.; Davis, J.M.; Sargent, R.G. Effect of iron supplementation on endurance capacity in iron-depleted female runners. Med. Sci. Sports Exerc. 1992, 24, 819–824. [Google Scholar] [CrossRef] [PubMed]
- Fogelholm, M.; Jaakkola, L.; Lampisjärvi, T. Effects of Iron Supplementation in Female Athletes with Low Serum Ferritin Concentration. Endoscopy 1992, 13, 158–162. [Google Scholar] [CrossRef]
- Garvican, L.A.; Saunders, P.U.; Cardoso, T.; Macdougall, I.C.; Lobigs, L.M.; Fazakerley, R.; Fallon, K.E.; Anderson, B.; Anson, J.M.; Thompson, K.G.; et al. Intravenous Iron Supplementation in Distance Runners with Low or Suboptimal Ferritin. Med. Sci. Sports Exerc. 2014, 46, 376–385. [Google Scholar] [CrossRef]
- Brutsaert, T.D.; Hernandez-Cordero, S.; Rivera, J.; Viola, T.; Hughes, G.; Haas, J.D. Iron supplementation improves progressive fatigue resistance during dynamic knee extensor exercise in iron-depleted, nonanemic women. Am. J. Clin. Nutr. 2003, 77, 441–448. [Google Scholar] [CrossRef]
- Rubeor, A.; Goojha, C.; Manning, J.; White, J. Does Iron Supplementation Improve Performance in Iron-Deficient Nonanemic Athletes? Sports Health A Multidiscip. Approach 2018, 10, 400–405. [Google Scholar] [CrossRef]
| Age | n | Normal Ferritin Levels | Prelalent | Latent | Anemia | |
|---|---|---|---|---|---|---|
| up to 14 | male | 33 | 27 (81.8%) | 4 (12.1%) | 2 (6.1%) | 0 |
| female | 37 | 28 (75.7%) | 3 (8.1%) | 5 (13.5%) | 1 (2.7%) | |
| 14–18 | male | 198 | 169 (85.4%) | 14 (7.1%) | 14 (7.1%) | 1 (0.5%) |
| female | 159 | 97 (61.0%) | 30 (18.9%) | 31 (19.5%) | 1 (0.6%) | |
| over 18 | male | 108 | 106 (98.1%) | 0 | 1 (0.9%) | 1 (0.9%) |
| female | 94 | 61 (64.9%) | 18 (19.1%) | 11 (11.7%) | 4 (4.3%) | |
| overall | male | 339 | 302 (89.1%) | 18 (5.3%) | 17 (5.0%) | 2 (0.6%) |
| female | 290 | 186 (64.1%) | 51 (17.6%) | 47 (16.2%) | 6 (2.1%) |
| Sport Types | n | Normal Ferritin Levels | Prelalent | Latent | Anemia | |
|---|---|---|---|---|---|---|
| Skill | male | 13 | 12 (92.3%) | 1 (7.7%) | 0 | 0 |
| female | 17 | 10 (58.8%) | 1 (5.9%) | 5 (29.4%) | 1 (5.9%) | |
| Power | male | 108 | 93 (86.1%) | 6 (5.6%) | 9 (8.3%) | 0 |
| female | 106 | 75 (70.8%) | 14 (13.2%) | 16 (15.1%) | 1 (0.9%) | |
| Mixed | male | 144 | 128 (88.9%) | 8 (5.6%) | 6 (4.2%) | 2 (1.4%) |
| female | 111 | 69 (62.2%) | 26 (23.4%) | 13 (11.7%) | 3 (2.7%) | |
| Endurance | male | 74 | 69 (93.2%) | 3 (4.1%) | 2 (2.7%) | 0 |
| female | 56 | 32 (57.1%) | 10 (17.9%) | 13 (23.2%) | 1 (1.8%) |
| Normal Ferritin Levels | Iron Deficiency | ||||||
|---|---|---|---|---|---|---|---|
| n | n | p | g | ||||
| Age (years) | male | 15.6 ± 1.4 | 196 | 15.1 ± 1.3 | 35 | 0.028 | 0.41 |
| female | 15.5 ± 1.6 | 125 | 15.6 ± 1.4 | 71 | 0.620 | - | |
| Height (cm) | male | 178.6 ± 10.8 | 166 | 174.0 ± 11.0 | 33 | 0.038 | 0.43 |
| female | 168.8 ± 7.0 | 99 | 169.9 ± 8.8 | 65 | 0.382 | - | |
| Weight (kg) | male | 67.7 ± 13.6 | 166 | 63.6 ± 13.8 | 33 | 0.044 | 0.37 |
| female | 61.1 ± 10.2 | 99 | 59.9 ± 9.2 | 65 | 0.420 | - | |
| BMI-SDS | male | −0.05 ± 0.77 | 166 | −0.14 ± 0.78 | 33 | 0.564 | - |
| female | 0.01± 0.87 | 99 | −0.25 ± 0.77 | 65 | 0.047 | 0.32 | |
| Body fat (%) | male | 9.6 ± 5.3 | 160 | 9.2 ± 4.7 | 30 | 0.769 | - |
| female | 18.7 ± 7.0 | 99 | 17.9 ± 5.2 | 64 | 0.860 | - | |
| Workload (W/kg) | male | 3.8 ± 0.8 | 138 | 3.7 ± 0.6 | 27 | 0.741 | - |
| female | 3.3 ± 0.5 | 82 | 3.3 ± 0.7 | 56 | 0.588 | - | |
| Heart rate (bpm) | male | 191.3 ± 11.0 | 138 | 193.2 ± 8.5 | 27 | 0.646 | - |
| female | 189.4 ± 9.5 | 82 | 188.7 ± 8.0 | 56 | 0.643 | - | |
| RRsys (mmHg) | male | 197.1 ± 25.0 | 138 | 191.8 ± 25.4 | 27 | 0.321 | - |
| female | 183.5 ± 20.6 | 82 | 190.1 ± 22.0 | 56 | 0.073 | - | |
| RRdia (mmHg) | male | 79.3 ± 9.8 | 138 | 80.8 ± 8.4 | 27 | 0.467 | - |
| female | 79.1 ± 9.1 | 82 | 79.3 ± 8.3 | 56 | 0.927 | - | |
| Lactate (mmol/L) | male | 8.90 ± 2.67 | 12 | 9.97 | 1 | - | - |
| female | 9.14 ± 2.04 | 7 | 7.14 ± 1.28 | 2 | 0.143 | - | |
| Hämoglobin | male | 14.88 ± 0.94 | 196 | 14.31 ± 0.91 | 35 | 0.001 | 0.61 |
| female | 13.39 ± 0.85 | 125 | 12.97 ± 0.95 | 71 | 0.002 | 0.48 | |
| Hämatokrit | male | 43.2 ± 2.7 | 196 | 42.0 ± 2.9 | 35 | 0.021 | 0.42 |
| female | 39.5 ± 2.5 | 125 | 38.8 ± 2.5 | 71 | 0.044 | 0.30 | |
| MCH | male | 29.4 ± 1.3 | 196 | 28.3 ± 1.1 | 35 | <0.001 | 0.85 |
| female | 29.3 ± 1.4 | 125 | 28.5 ± 1.7 | 71 | 0.002 | 0.49 | |
| MCHC | male | 34.5 ± 0.9 | 196 | 34.2 ± 1.0 | 35 | 0.078 | - |
| female | 34.0 ± 0.9 | 125 | 33.5 ± 1.0 | 71 | 0.002 | 0.52 | |
| MCV | male | 84.9 ± 3.3 | 196 | 83.0 ± 2.6 | 35 | 0.003 | 0.59 |
| female | 86.3 ± 3.1 | 125 | 84.9 ± 3.6 | 71 | 0.011 | 0.40 | |
| Ferritin | male | 64.9 ± 32.2 | 196 | 21.1 ± 6.3 | 35 | <0.001 | 1.47 |
| female | 56.6 ±46.3 | 125 | 17.8 ± 6.6 | 71 | <0.001 | 1.04 | |
| Eisen | male | 106.4 ± 40.1 | 196 | 83.2 ± 29.5 | 35 | 0.002 | 0.57 |
| female | 101.2 ± 38.8 | 125 | 80.8 ± 50.1 | 71 | <0.001 | 0.47 | |
| Transferrin | male | 274.7 ± 32.9 | 196 | 302.0 ± 32.9 | 35 | <0.001 | −0.83 |
| female | 281.3 ± 35.5 | 125 | 320.0 ± 46.5 | 71 | <0.001 | −0.97 | |
| Lösl. Rezeptor | male | 3.40 ± 0.43 | 18 | 3.66 ± 0.82 | 35 | 0.127 | - |
| female | 3.14 ± 0.89 | 32 | 3.52 ± 1.15 | 71 | 0.028 | −0.35 | |
| Trans.Sättigung | male | 28.1 ± 12.2 | 196 | 19.8 ± 7.4 | 35 | <0.001 | 0.71 |
| female | 25.8 ± 9.9 | 125 | 18.1 ± 10.1 | 71 | <0.001 | 0.77 | |
| Normal Ferritin Levels | Iron Deficiency | ||||||
|---|---|---|---|---|---|---|---|
| n | n | p | g | ||||
| Age | male | 21.7 ± 3.0 | 106 | 18.7 ± 0.1 | 2 | - | |
| female | 21.7 ± 3.4 | 61 | 21.6 ± 3.5 | 33 | 0.632 | - | |
| Height | male | 182.7 ± 9.4 | 81 | 164.0 | 1 | - | |
| female | 174.8 ± 9.6 | 42 | 170.0 ± 12.5 | 25 | 0.068 | - | |
| Weight | male | 78.6 ± 14.7 | 81 | 53.4 | 1 | - | |
| female | 66.8 ± 11.0 | 42 | 64.2 ± 11.7 | 25 | 0.364 | - | |
| BMI | male | 23.4 ± 3.0 | 81 | 19.9 | 1 | - | |
| female | 21.8 ± 2.7 | 42 | 22.2 ± 2.8 | 25 | 0.555 | - | |
| Body fat (%) | male | 10.8 ± 5.0 | 69 | 22.5 | 1 | - | |
| female | 16.7 ± 5.2 | 42 | 18.0 ± 4.4 | 22 | 0.331 | - | |
| Workload (W/kg) | male | 3.5 ± 0.8 | 72 | 3.7 | 1 | - | |
| female | 3.5± 0.5 | 34 | 3.2 ± 0.8 | 21 | 0.101 | - | |
| Heart rate (bpm) | male | 182.8 ± 13.4 | 72 | 181.0 | 1 | - | - |
| female | 183.4 ± 11.1 | 34 | 183.6 ± 10.9 | 21 | 0.943 | - | |
| RRsys (mmHg) | male | 203.3 ± 22.4 | 72 | 206 | 1 | - | - |
| female | 199.1 ± 20.9 | 34 | 189.0 ± 30.0 | 21 | 0.135 | - | |
| RRdia (mmHg) | male | 81.7 ± 9.1 | 72 | 91.0 | 1 | - | - |
| female | 83.7 ± 7.4 | 34 | 82.0 ± 8.9 | 21 | 0.470 | - | |
| Lactate (mmol/L) | male | 8.99 ± 2.90 | 37 | - | - | - | |
| female | 9.50 ± 2.40 | 17 | 9.28 ± 2.25 | 8 | 0.835 | - | |
| Hämoglobin | male | 15.25 ± 0.96 | 106 | 12.80 ± 0.42 | 2 | - | - |
| female | 13.72 ± 0.90 | 61 | 12.88 ± 0.88 | 33 | <0.001 | 0.93 | |
| Hämatokrit | male | 44.4 ± 2.5 | 106 | 38.1 ± 0.2 | 2 | - | - |
| female | 40.2 ± 2.4 | 61 | 38.9 ± 2.6 | 33 | 0.016 | 0.52 | |
| MCH | male | 29.6 ± 1.3 | 106 | 30.5 ± 0.7 | 2 | - | - |
| female | 30.0 ± 1.3 | 61 | 28.3 ± 2.1 | 33 | <0.001 | 1.05 | |
| MCHC | male | 34.3 ± 0.9 | 106 | 33.5 ± 0.7 | 2 | - | - |
| female | 34.1 ± 0.9 | 61 | 33.2 ± 0.9 | 33 | <0.001 | 1.04 | |
| MCV | male | 86.3 ± 3.0 | 106 | 89.5 ± 0.7 | 2 | - | - |
| female | 88.1 ± 3.2 | 61 | 85.3 ± 4.4 | 33 | 0.005 | 0.76 | |
| Ferritin | male | 115.8 ± 51.1 | 106 | 29.1 ± 16.6 | 2 | - | - |
| female | 84.5 ± 68.0 | 61 | 19.0 ± 8.9 | 33 | <0.001 | 1.18 | |
| Eisen | male | 110.2 ± 41.9 | 106 | 86.5 ± 50.2 | 2 | - | - |
| female | 117.3 ± 49.0 | 61 | 97.6 ± 55.2 | 33 | 0.078 | - | |
| Transferrin | male | 259.4 ± 32.2 | 106 | 257.0 ± 33.9 | 2 | - | - |
| female | 269.8 ± 40.5 | 61 | 328.3 ± 64.9 | 33 | <0.001 | −1.15 | |
| Lösl. Rezeptor | male | - | 3.30 | 1 | - | - | |
| female | 2.20 ± 0.36 | 7 | 3.24 ± 1.19 | 32 | 0.006 | −0.93 | |
| Trans.Sättigung | male | 30.2 ± 11.2 | 106 | 25.0 ± 17.1 | 2 | - | - |
| female | 31.6 ± 14.3 | 61 | 21.7 ± 12.4 | 33 | 0.001 | 0.72 | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Roy, R.; Kück, M.; Radziwolek, L.; Kerling, A. Iron Deficiency in Adolescent and Young Adult German Athletes—A Retrospective Study. Nutrients 2022, 14, 4511. https://doi.org/10.3390/nu14214511
Roy R, Kück M, Radziwolek L, Kerling A. Iron Deficiency in Adolescent and Young Adult German Athletes—A Retrospective Study. Nutrients. 2022; 14(21):4511. https://doi.org/10.3390/nu14214511
Chicago/Turabian StyleRoy, Rubina, Momme Kück, Lukas Radziwolek, and Arno Kerling. 2022. "Iron Deficiency in Adolescent and Young Adult German Athletes—A Retrospective Study" Nutrients 14, no. 21: 4511. https://doi.org/10.3390/nu14214511
APA StyleRoy, R., Kück, M., Radziwolek, L., & Kerling, A. (2022). Iron Deficiency in Adolescent and Young Adult German Athletes—A Retrospective Study. Nutrients, 14(21), 4511. https://doi.org/10.3390/nu14214511





