Moderate-to-Severe Malnutrition Identified by the Controlling Nutritional Status (CONUT) Score Is Significantly Associated with Treatment Failure of Periprosthetic Joint Infection
Abstract
1. Introduction
2. Materials and Methods
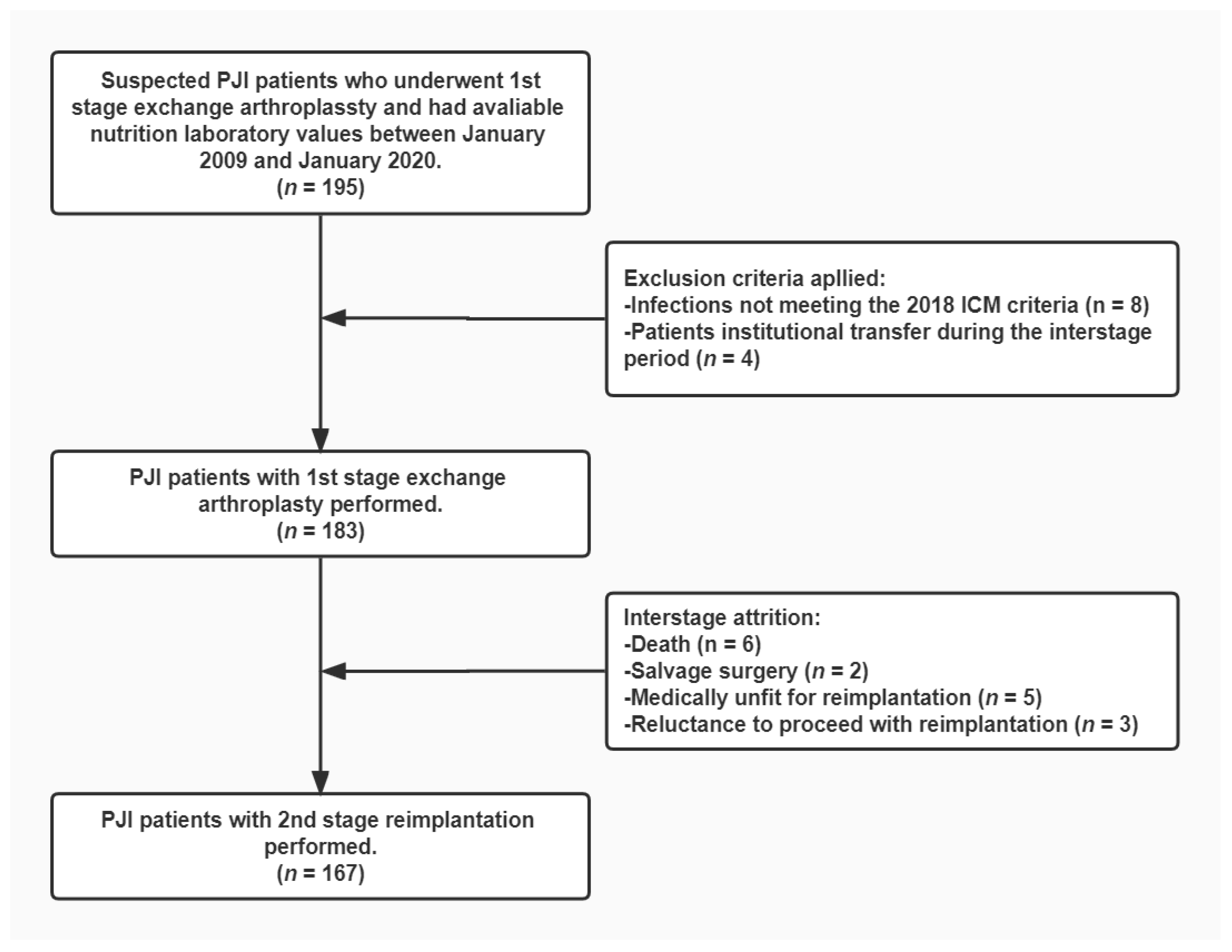
2.1. Study Population
2.2. Two-Stage Exchange Technique
2.3. Clinical Data Extraction and Nutritional Status Assessment
2.4. Clinical Outcome Assessment
2.5. Statistical Analysis
3. Results
3.1. Patient Characteristics
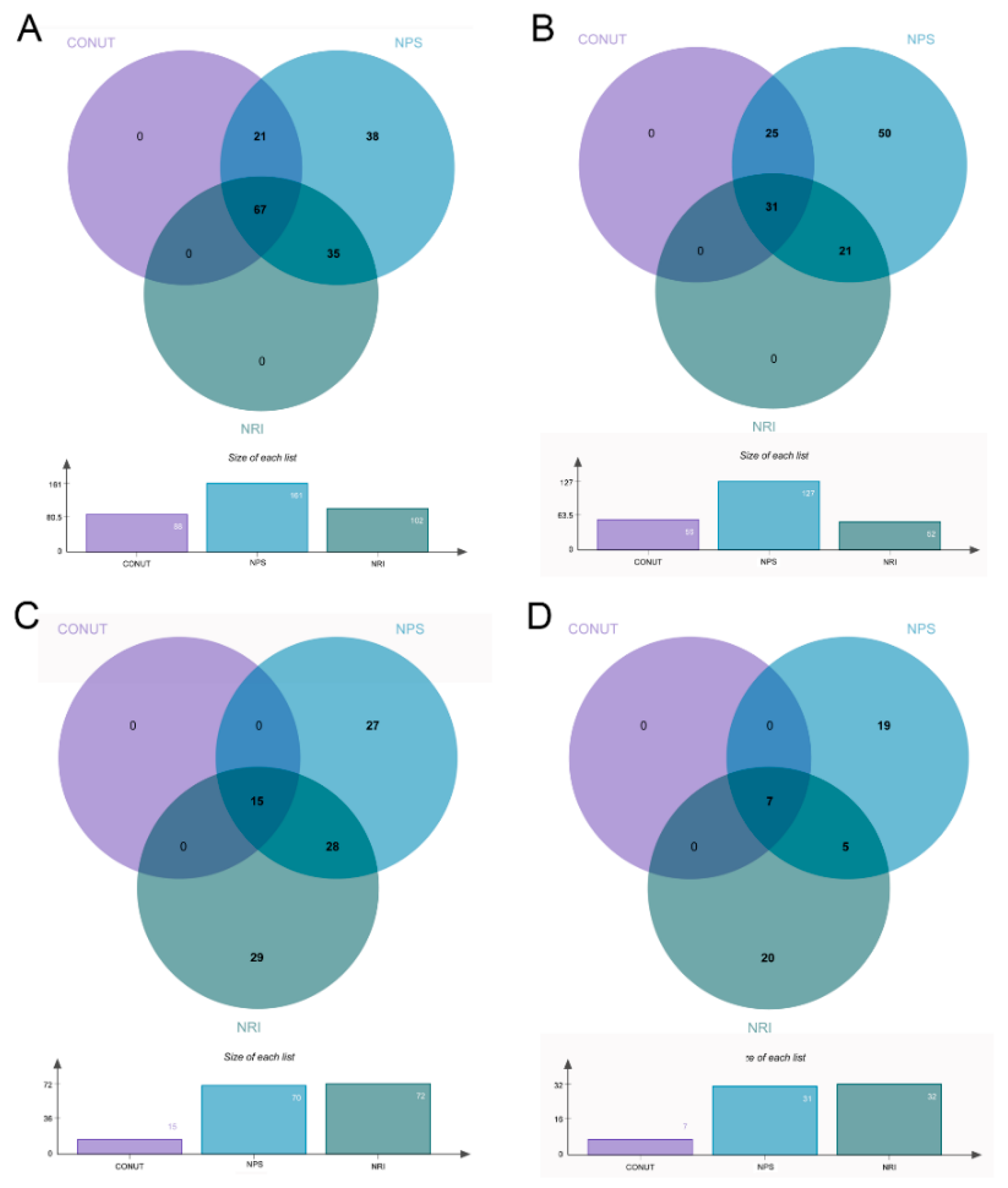
3.2. Prevalent Trends and Clinical Features of Malnutrition
3.3. Association between Malnutrition and Treatment Failure
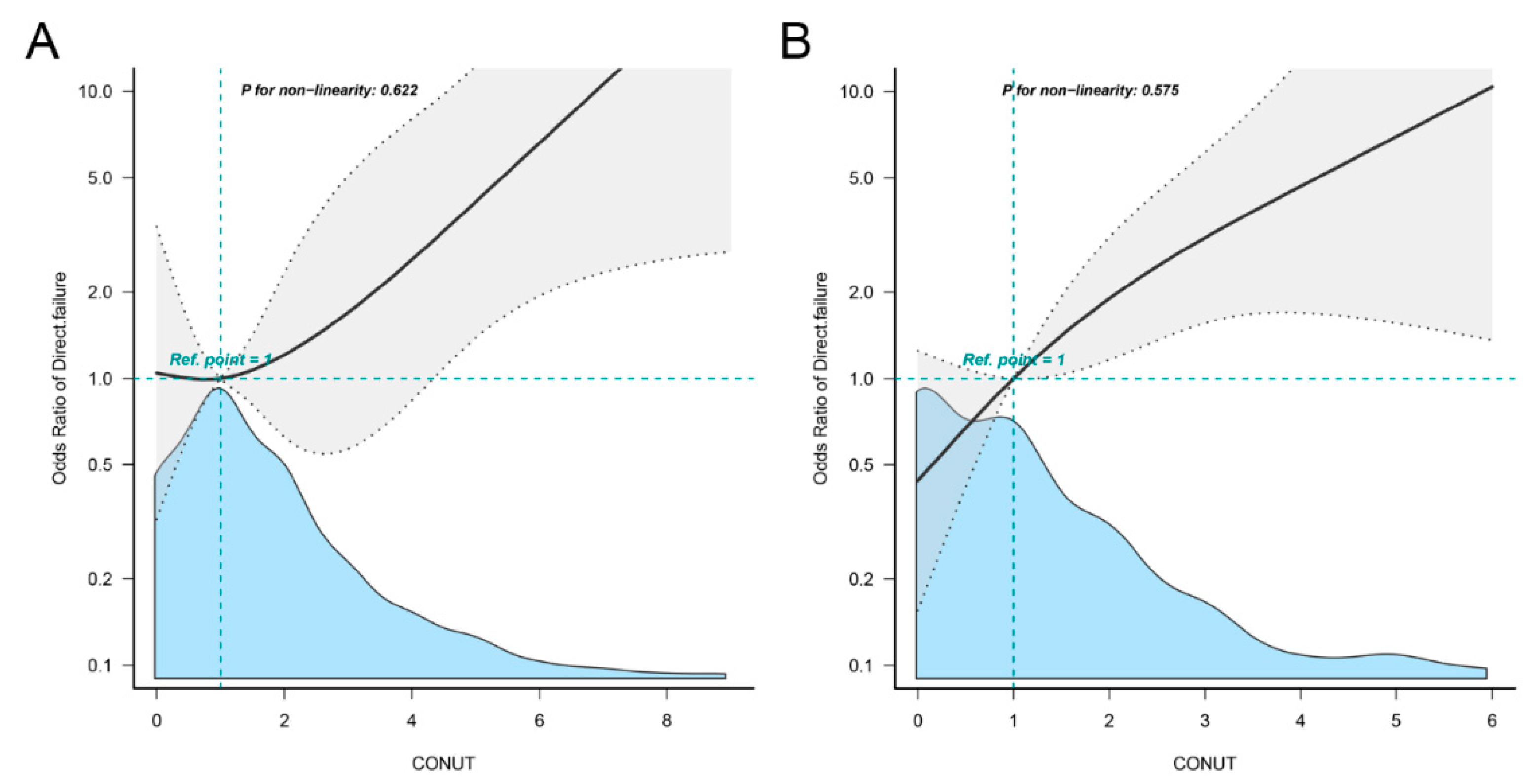
3.4. Risk Factors for Moderate-to-Severe Malnutrition at 1st Stage Exchange
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A
| Definition | 1st Stage Exchange | 2nd Stage Exchange | p |
|---|---|---|---|
| CONUT | 1.8 ± 1.7 | 1.3 ± 1.4 | <0.001 |
| NPS | 2.1 ± 1.3 | 1.4 ± 1.1 | <0.001 |
| NRI | 99.3 ± 6.1 | 102 ± 6.3 | <0.001 |
Appendix B
| Definition | Failure Rate | OR (95% CI) | p | |
|---|---|---|---|---|
| Malnutrition at 1st Stage | ||||
| CONUT | Normal | 28/95 (29.5%) | Reference Category | |
| Mild | 18/73 (24.6%) | 0.72 (0.30−1.76) | 0.472 | |
| Moderate-to-severe | 7/15 (46.7%) | 2.96 (0.75−11.67) | 0.102 | |
| Malnutrition at 2nd Stage | ||||
| CONUT | Normal | 20/111 (17.1%) | Reference Category | |
| Mild | 14/49 (28.6%) | 3.02 (1.10−8.29) | 0.032 | |
| Moderate-to-severe | 3/7 (42.9%) | 10.99 (1.38−87.54) | 0.024 | |
References
- Kurtz, S.; Ong, K.; Lau, E.; Mowat, F.; Halpern, M. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J. Bone Jt. Surg. Am. 2007, 89, 780–785. [Google Scholar] [CrossRef]
- Kurtz, S.M.; Ong, K.L.; Lau, E.; Bozic, K.J.; Berry, D.; Parvizi, J. Prosthetic joint infection risk after TKA in the Medicare population. Clin. Orthop. Relat. Res. 2010, 468, 52–56. [Google Scholar] [CrossRef] [PubMed]
- Ong, K.L.; Kurtz, S.M.; Lau, E.; Bozic, K.J.; Berry, D.J.; Parvizi, J. Prosthetic joint infection risk after total hip arthroplasty in the Medicare population. J. Arthroplast. 2009, 24, 105–109. [Google Scholar] [CrossRef] [PubMed]
- Pangaud, C.; Ollivier, M.; Argenson, J.N. Outcome of single-stage versus two-stage exchange for revision knee arthroplasty for chronic periprosthetic infection. EFORT Open Rev. 2019, 4, 495–502. [Google Scholar] [CrossRef]
- Lazic, I.; Scheele, C.; Pohlig, F.; von Eisenhart-Rothe, R.; Suren, C. Treatment options in PJI-is two-stage still gold standard? J. Orthop. 2021, 23, 180–184. [Google Scholar] [CrossRef] [PubMed]
- Kurtz, S.M.; Higgs, G.B.; Lau, E.; Iorio, R.R.; Courtney, P.M.; Parvizi, J. Hospital Costs for Unsuccessful Two-Stage Revisions for Periprosthetic Joint Infection. J. Arthroplast. 2022, 37, 205–212. [Google Scholar] [CrossRef] [PubMed]
- Drain, N.P.; Bertolini, D.M.; Anthony, A.W.; Feroze, M.W.; Chao, R.; Onyekweli, T.; Longo, S.E.; Hersh, B.L.; Smith, C.N.; Rothenberger, S.D.; et al. High Mortality After Total Knee Arthroplasty Periprosthetic Joint Infection is Related to Preoperative Morbidity and the Disease Process but Not Treatment. J. Arthroplast. 2022, 37, 1383–1389. [Google Scholar] [CrossRef]
- Henderson, R.A.; Austin, M.S. Management of Periprosthetic Joint Infection: The More We Learn, the Less We Know. J. Arthroplast. 2017, 32, 2056–2059. [Google Scholar] [CrossRef]
- Cederholm, T.; Barazzoni, R.; Austin, P.; Ballmer, P.; Biolo, G.; Bischoff, S.C.; Compher, C.; Correia, I.; Higashiguchi, T.; Holst, M.; et al. ESPEN guidelines on definitions and terminology of clinical nutrition. Clin. Nutr. 2017, 36, 49–64. [Google Scholar] [CrossRef] [PubMed]
- Rovesti, G.; Valoriani, F.; Rimini, M.; Bardasi, C.; Ballarin, R.; Benedetto, F.D.; Menozzi, R.; Dominici, M.; Spallanzani, A. Clinical Implications of Malnutrition in the Management of Patients with Pancreatic Cancer: Introducing the Concept of the Nutritional Oncology Board. Nutrients 2021, 13, 3522. [Google Scholar] [CrossRef]
- Viasus, D.; Perez-Vergara, V.; Carratala, J. Effect of Undernutrition and Obesity on Clinical Outcomes in Adults with Community-Acquired Pneumonia. Nutrients 2022, 14, 3235. [Google Scholar] [CrossRef] [PubMed]
- Blevins, K.; Aalirezaie, A.; Shohat, N.; Parvizi, J. Malnutrition and the Development of Periprosthetic Joint Infection in Patients Undergoing Primary Elective Total Joint Arthroplasty. J. Arthroplast. 2018, 33, 2971–2975. [Google Scholar] [CrossRef] [PubMed]
- Font-Vizcarra, L.; Lozano, L.; Rios, J.; Forga, M.T.; Soriano, A. Preoperative nutritional status and post-operative infection in total knee replacements: A prospective study of 213 patients. Int. J. Artif. Organs. 2011, 34, 876–881. [Google Scholar] [CrossRef] [PubMed]
- Gherini, S.; Vaughn, B.K.; Lombardi, A.V., Jr.; Mallory, T.H. Delayed wound healing and nutritional deficiencies after total hip arthroplasty. Clin. Orthop. Relat. Res. 1993, 293, 188–195. [Google Scholar] [CrossRef]
- Huang, R.; Greenky, M.; Kerr, G.J.; Austin, M.S.; Parvizi, J. The effect of malnutrition on patients undergoing elective joint arthroplasty. J. Arthroplast. 2013, 28, 21–24. [Google Scholar] [CrossRef] [PubMed]
- Yi, P.H.; Frank, R.M.; Vann, E.; Sonn, K.A.; Moric, M.; Valle, C.J.D. Is potential malnutrition associated with septic failure and acute infection after revision total joint arthroplasty? Clin. Orthop. Relat. Res. 2015, 473, 175–182. [Google Scholar] [CrossRef]
- Ellsworth, B.; Kamath, A.F. Malnutrition and Total Joint Arthroplasty. J. Nat. Sci. 2016, 2, e179. [Google Scholar] [PubMed]
- Dube, M.D.; Rothfusz, C.A.; Emara, A.K.; Hadad, M.; Surace, P.; Krebs, V.E.; Molloy, R.M.; Piuzzi, N.S. Nutritional Assessment and Interventions in Elective Hip and Knee Arthroplasty: A Detailed Review and Guide to Management. Curr. Rev. Musculoskelet. Med. 2022, 15, 311–322. [Google Scholar] [CrossRef]
- He, Y.; Tang, X.; Ning, N.; Chen, J.; Li, P.; Kang, P. Effects of Preoperative Oral Electrolyte-Carbohydrate Nutrition Supplement on Postoperative Outcomes in Elderly Patients Receiving Total Knee Arthroplasty: A Prospective Randomized Controlled Trial. Orthop. Surg. 2022, 14, 2535–2544. [Google Scholar] [CrossRef] [PubMed]
- Schroer, W.C.; LeMarr, A.R.; Mills, K.; Childress, A.L.; Morton, D.J.; Reedy, M.E. 2019 Chitranjan S. Ranawat Award: Elective joint arthroplasty outcomes improve in malnourished patients with nutritional intervention: A prospective population analysis demonstrates a modifiable risk factor. Bone Jt. J. 2019, 101-B, 17–21. [Google Scholar] [CrossRef] [PubMed]
- Alito, M.A.; de Aguilar-Nascimento, J.E. Multimodal perioperative care plus immunonutrition versus traditional care in total hip arthroplasty: A randomized pilot study. Nutr. J. 2016, 15, 34. [Google Scholar] [CrossRef] [PubMed]
- Ibrahim, M.K.; Zambruni, M.; Melby, C.L.; Melby, P.C. Impact of Childhood Malnutrition on Host Defense and Infection. Clin. Microbiol. Rev. 2017, 30, 919–971. [Google Scholar] [CrossRef] [PubMed]
- Schaible, U.E.; Kaufmann, S.H. Malnutrition and infection: Complex mechanisms and global impacts. PLoS Med. 2007, 4, e115. [Google Scholar] [CrossRef] [PubMed]
- Bachou, H.; Tylleskar, T.; Downing, R.; Tumwine, J.K. Severe malnutrition with and without HIV-1 infection in hospitalised children in Kampala, Uganda: Differences in clinical features, haematological findings and CD4+ cell counts. Nutr. J. 2006, 5, 27. [Google Scholar] [CrossRef][Green Version]
- Pironi, L.; Sasdelli, A.S.; Ravaioli, F.; Baracco, B.; Battaiola, C.; Bocedi, G.; Brodosi, L.; Leoni, L.; Mari, G.A.; Musio, A. Malnutrition and nutritional therapy in patients with SARS-CoV-2 disease. Clin. Nutr. 2021, 40, 1330–1337. [Google Scholar] [CrossRef] [PubMed]
- Bossi, P.; Delrio, P.; Mascheroni, A.; Zanetti, M. The Spectrum of Malnutrition/Cachexia/Sarcopenia in Oncology According to Different Cancer Types and Settings: A Narrative Review. Nutrients 2021, 13, 1980. [Google Scholar] [CrossRef]
- Bullock, A.F.; Greenley, S.L.; McKenzie, G.A.G.; Paton, L.W.; Johnson, M.J. Relationship between markers of malnutrition and clinical outcomes in older adults with cancer: Systematic review, narrative synthesis and meta-analysis. Eur. J. Clin. Nutr. 2020, 74, 1519–1535. [Google Scholar] [CrossRef]
- Zajonz, D.; Daikos, A.; Prager, F.; Edel, M.; Mobius, R.; Fakler, J.K.M.; Roth, A.; Ghanem, M. Significance of nutritional status in the development of periprosthetic infections: A retrospective analysis of 194 patients. Orthopade 2021, 50, 188–197. [Google Scholar] [CrossRef]
- Bohl, D.D.; Shen, M.R.; Kayupov, E.; Cvetanovich, G.L.; Valle, C.J.D. Is Hypoalbuminemia Associated With Septic Failure and Acute Infection After Revision Total Joint Arthroplasty? A Study of 4517 Patients From the National Surgical Quality Improvement Program. J. Arthroplast. 2016, 31, 963–967. [Google Scholar] [CrossRef]
- Choi, J.T.; Yoshida, B.; Jalali, O.; Hatch, G.F., 3rd. Malnutrition in Orthopaedic Sports Medicine: A Review of the Current Literature. Sports Health 2021, 13, 65–70. [Google Scholar] [CrossRef]
- Morey, V.M.; Song, Y.D.; Whang, J.S.; Kang, Y.G.; Kim, T.K. Can Serum Albumin Level and Total Lymphocyte Count be Surrogates for Malnutrition to Predict Wound Complications After Total Knee Arthroplasty? J. Arthroplast. 2016, 31, 1317–1321. [Google Scholar] [CrossRef] [PubMed]
- Wada, H.; Dohi, T.; Miyauchi, K.; Doi, S.; Konishi, H.; Naito, R.; Tsuboi, S.; Ogita, M.; Kasai, T.; Okazaki, S.; et al. Prognostic impact of nutritional status assessed by the Controlling Nutritional Status score in patients with stable coronary artery disease undergoing percutaneous coronary intervention. Clin. Res. Cardiol. 2017, 106, 875–883. [Google Scholar] [CrossRef] [PubMed]
- Bouillanne, O.; Morineau, G.; Dupont, C.; Coulombel, I.; Vincent, J.P.; Nicolis, I.; Benazeth, S.; Cynober, L.; Aussel, C. Geriatric Nutritional Risk Index: A new index for evaluating at-risk elderly medical patients. Am. J. Clin. Nutr. 2005, 82, 777–783. [Google Scholar] [CrossRef] [PubMed]
- Galizia, G.; Lieto, E.; Auricchio, A.; Cardella, F.; Mabilia, A.; Podzemny, V.; Castellano, P.; Orditura, M.; Napolitano, V. Naples Prognostic Score, Based on Nutritional and Inflammatory Status, is an Independent Predictor of Long-term Outcome in Patients Undergoing Surgery for Colorectal Cancer. Dis. Colon. Rectum 2017, 60, 1273–1284. [Google Scholar] [CrossRef]
- Bodolea, C.; Nemes, A.; Avram, L.; Craciun, R.; Coman, M.; Ene-Cocis, M.; Ciobanu, C.; Crisan, D. Nutritional Risk Assessment Scores Effectively Predict Mortality in Critically Ill Patients with Severe COVID-19. Nutrients 2022, 14, 2105. [Google Scholar] [CrossRef]
- Yang, Z.W.; Wei, X.B.; Fu, B.Q.; Chen, J.Y.; Yu, D.Q. Prevalence and Prognostic Significance of Malnutrition in Hypertensive Patients in a Community Setting. Front. Nutr. 2022, 9, 822376. [Google Scholar] [CrossRef]
- Zhang, Q.; Qian, L.; Liu, T.; Ding, J.S.; Zhang, X.; Song, M.M.; Wang, Z.W.; Ge, Y.Z.; Hu, C.L.; Li, X.R.; et al. Prevalence and Prognostic Value of Malnutrition Among Elderly Cancer Patients Using Three Scoring Systems. Front. Nutr. 2021, 8, 738550. [Google Scholar] [CrossRef]
- Shohat, N.; Bauer, T.; Buttaro, M.; Budhiparama, N.; Cashman, J.; Valle, C.J.D.; Drago, L.; Gehrke, T.; Marcelino Gomes, L.S.; Goswami, K.; et al. Hip and Knee Section, What is the Definition of a Periprosthetic Joint Infection (PJI) of the Knee and the Hip? Can the Same Criteria be Used for Both Joints?: Proceedings of International Consensus on Orthopedic Infections. J. Arthroplast. 2019, 34, S325–S327. [Google Scholar] [CrossRef]
- Bingham, J.S.; Hassebrock, J.D.; Christensen, A.L.; Beauchamp, C.P.; Clarke, H.D.; Spangehl, M.J. Screening for Periprosthetic Joint Infections With ESR and CRP: The Ideal Cutoffs. J. Arthroplast. 2020, 35, 1351–1354. [Google Scholar] [CrossRef]
- Stambough, J.B.; Curtin, B.M.; Odum, S.M.; Cross, M.B.; Martin, J.R.; Fehring, T.K. Does Change in ESR and CRP Guide the Timing of Two-stage Arthroplasty Reimplantation? Clin. Orthop. Relat. Res. 2019, 477, 364–371. [Google Scholar] [CrossRef]
- Fillingham, Y.A.; Valle, C.J.D.; Suleiman, L.I.; Springer, B.D.; Gehrke, T.; Bini, S.A.; Segreti, J.; Chen, A.F.; Goswami, K.; Tan, T.L.; et al. Definition of Successful Infection Management and Guidelines for Reporting of Outcomes After Surgical Treatment of Periprosthetic Joint Infection: From the Workgroup of the Musculoskeletal Infection Society (MSIS). J. Bone Jt. Surg. Am. 2019, 101, e69. [Google Scholar] [CrossRef] [PubMed]
- Borsinger, T.M.; Pierce, D.A.; Hanson, T.M.; Werth, P.M.; Orem, A.R.; Moschetti, W.E. Is the Proportion of Patients with "Successful" Outcomes After Two-stage Revision for Prosthetic Joint Infection Different When Applying the Musculoskeletal Infection Society Outcome Reporting Tool Compared with the Delphi-based Consensus Criteria? Clin. Orthop. Relat. Res. 2021, 479, 1589–1597. [Google Scholar] [CrossRef] [PubMed]
- Nanri, Y.; Shibuya, M.; Fukushima, K.; Uchiyama, K.; Takahira, N.; Takaso, M. Preoperative malnutrition is a risk factor for delayed recovery of mobilization after total hip arthroplasty. PM&R 2021, 13, 1331–1339. [Google Scholar] [CrossRef]
- Ahiko, Y.; Shida, D.; Horie, T.; Tanabe, T.; Takamizawa, Y.; Sakamoto, R.; Moritani, K.; Tsukamoto, S.; Kanemitsu, Y. Controlling nutritional status (CONUT) score as a preoperative risk assessment index for older patients with colorectal cancer. BMC Cancer 2019, 19, 946. [Google Scholar] [CrossRef] [PubMed]
- Miura, N.; Shoji, F.; Kozuma, Y.; Toyokawa, G.; Yamazaki, K.; Takeo, S. Preoperative Immune-Nutritional Abnormality Predicts Poor Outcome in Elderly Non-Small-Cell Lung Cancer Patients with Comorbidities. Ann. Thorac. Cardiovasc. Surg. 2020, 26, 240–247. [Google Scholar] [CrossRef] [PubMed]
- Yoshida, N.; Baba, Y.; Shigaki, H.; Harada, K.; Iwatsuki, M.; Kurashige, J.; Sakamoto, Y.; Miyamoto, Y.; Ishimoto, T.; Kosumi, K.; et al. Preoperative Nutritional Assessment by Controlling Nutritional Status (CONUT) is Useful to estimate Postoperative Morbidity After Esophagectomy for Esophageal Cancer. World J. Surg. 2016, 40, 1910–1917. [Google Scholar] [CrossRef] [PubMed]
- Tsantes, A.G.; Papadopoulos, D.V.; Lytras, T.; Tsantes, A.E.; Mavrogenis, A.F.; Korompilias, A.V.; Gelalis, I.D.; Tsantes, C.G.; Bonovas, S. Association of malnutrition with periprosthetic joint and surgical site infections after total joint arthroplasty: A systematic review and meta-analysis. J. Hosp. Infect. 2019, 103, 69–77. [Google Scholar] [CrossRef] [PubMed]
- Gu, A.; Malahias, M.A.; Strigelli, V.; Nocon, A.A.; Sculco, T.P.; Sculco, P.K. Preoperative Malnutrition Negatively Correlates With Postoperative Wound Complications and Infection After Total Joint Arthroplasty: A Systematic Review and Meta-Analysis. J. Arthroplast. 2019, 34, 1013–1024. [Google Scholar] [CrossRef] [PubMed]
- Zhang, D.; Zhang, X. Effect of serologic malnutrition on postoperative wound infection problems after total joint arthroplasty: A meta-analysis. Int. Wound J. 2022. [Google Scholar] [CrossRef] [PubMed]
- Fang, C.J.; Saadat, G.H.; Butler, B.A.; Bokhari, F. The Geriatric Nutritional Risk Index Is an Independent Predictor of Adverse Outcomes for Total Joint Arthroplasty Patients. J. Arthroplast. 2022, 37, S836–S841. [Google Scholar] [CrossRef]
- Heath, M.L.; Sidbury, R. Cutaneous manifestations of nutritional deficiency. Curr. Opin. Pediatr. 2006, 18, 417–422. [Google Scholar] [CrossRef] [PubMed]
- Nassar, M.F.; El-Batrawy, S.R.; Nagy, N.M. CD95 expression in white blood cells of malnourished infants during hospitalization and catch-up growth. East Mediterr. Health J. 2009, 15, 574–583. [Google Scholar] [CrossRef] [PubMed]
- Roubin, S.R.; Assi, E.A.; Fernandez, M.C.; Pardal, C.B.; Castro, A.L.; Parada, J.A.; Perez, D.D.; Prieto, S.B.; Rossello, X.; Ibanez, B.; et al. Prevalence and Prognostic Significance of Malnutrition in Patients With Acute Coronary Syndrome. J. Am. Coll. Cardiol. 2020, 76, 828–840. [Google Scholar] [CrossRef]
- Johnson, N.R.; Rowe, T.M.; Valenzeula, M.M.; Scarola, G.T.; Fehring, T.K. Do Pre-Reimplantation Erythrocyte Sedimentation Rate/C-Reactive Protein Cutoffs Guide Decision-Making in Prosthetic Joint Infection? Are We Flying Blind? J. Arthroplast. 2022, 37, 347–352. [Google Scholar] [CrossRef]
- Chen, Q.; Chen, K.; Wang, S.; Zhang, L.; Shi, Y.; Tao, S.; He, Z.; Wang, C.; Yu, L. Prognostic value of the controlling nutritional status score in patients with myelodysplastic syndromes. Front. Nutr. 2022, 9, 902704. [Google Scholar] [CrossRef] [PubMed]
- Martinez-Escribano, C.; Moreno, F.A.; Perez-Lopez, M.; Cunha-Perez, C.; Belenguer-Varea, A.; Peredo, D.C.; Gonzalez, F.J.B.; Tarazona-Santabalbina, F.J. Malnutrition and Increased Risk of Adverse Outcomes in Elderly Patients Undergoing Elective Colorectal Cancer Surgery: A Case-Control Study Nested in a Cohort. Nutrients 2022, 14, 207. [Google Scholar] [CrossRef] [PubMed]
- Li, J.; Feng, D.; Pang, N.; Zhao, C.; Gao, L.; Liu, S.; Li, L. Controlling nutritional status score as a new indicator of overt hepatic encephalopathy in cirrhotic patients following transjugular intrahepatic portosystemic shunt. Clin. Nutr. 2022, 41, 560–566. [Google Scholar] [CrossRef]
- Norman, K.; Pichard, C.; Lochs, H.; Pirlich, M. Prognostic impact of disease-related malnutrition. Clin. Nutr. 2008, 27, 5–15. [Google Scholar] [CrossRef] [PubMed]
- Hickson, M. Malnutrition and ageing. Postgrad. Med. J. 2006, 82, 2–8. [Google Scholar] [CrossRef] [PubMed]
- Miozzari, H.H.; Barea, C.; Hannouche, D.; Lubbeke, A. History of previous surgery is associated with higher risk of revision after primary total knee arthroplasty: A cohort study from the Geneva Arthroplasty Registry. Acta Orthop. 2021, 92, 709–715. [Google Scholar] [CrossRef]
- Kunutsor, S.K.; Whitehouse, M.R.; Blom, A.W.; Beswick, A.D.; Team, I. Patient-Related Risk Factors for Periprosthetic Joint Infection after Total Joint Arthroplasty: A Systematic Review and Meta-Analysis. PLoS ONE 2016, 11, e0150866. [Google Scholar] [CrossRef] [PubMed]
- Norman, K.; Hass, U.; Pirlich, M. Malnutrition in Older Adults-Recent Advances and Remaining Challenges. Nutrients 2021, 13, 2764. [Google Scholar] [CrossRef] [PubMed]
- Iddrisu, I.; Monteagudo-Mera, A.; Poveda, C.; Pyle, S.; Shahzad, M.; Andrews, S.; Walton, G.E. Malnutrition and Gut Microbiota in Children. Nutrients 2021, 13, 2727. [Google Scholar] [CrossRef] [PubMed]
- Ciebiera, M.; Esfandyari, S.; Siblini, H.; Prince, L.; Elkafas, H.; Wojtyla, C.; Al-Hendy, A.; Ali, M. Nutrition in Gynecological Diseases: Current Perspectives. Nutrients 2021, 13, 1178. [Google Scholar] [CrossRef]
- Najera, O.; Gonzalez, C.; Toledo, G.; Lopez, L.; Cortes, E.; Betancourt, M.; Ortiz, R. CD45RA and CD45RO isoforms in infected malnourished and infected well-nourished children. Clin. Exp. Immunol. 2001, 126, 461–465. [Google Scholar] [CrossRef] [PubMed]
- Procaccini, C.; Rosa, V.D.; Galgani, M.; Carbone, F.; Cassano, S.; Greco, D.; Qian, K.; Auvinen, P.; Cali, G.; Stallone, G.; et al. Leptin-induced mTOR activation defines a specific molecular and transcriptional signature controlling CD4+ effector T cell responses. J. Immunol. 2012, 189, 2941–2953. [Google Scholar] [CrossRef]
- Seebach, E.; Kubatzky, K.F. Chronic Implant-Related Bone Infections-Can Immune Modulation be a Therapeutic Strategy? Front. Immunol. 2019, 10, 1724. [Google Scholar] [CrossRef]
| Characteristics | Value |
|---|---|
| Demographic Details | |
| Age, years | 59.6 ± 13.2 |
| Male gender | 87 (47.5) |
| BMI, kg/m2 | 25.0 ± 4.1 |
| Smoking | 11 (6.0) |
| Comorbidities | |
| Cardiovascular disease | 39 (21.3) |
| Diabetes | 24 (13.1) |
| Disease Data | |
| Hip | 104 (56.8) |
| Primary diagnosis | |
| Osteoarthritis | 52 (28.4) |
| ONFH | 44 (24.0) |
| DDH | 3 (1.6) |
| Inflammatory arthropathy | 11 (6.0) |
| Fracture | 47 (25.7) |
| Others | 26 (14.2) |
| Pathogens | |
| Staphylococcus aureus | 17 (9.3) |
| Coagulase-negative Staphylococcus | 52 (28.4) |
| Entoococcus | 3 (1.6) |
| Streptococcus | 5 (2.7) |
| Gram-Negative Bacteria | 9 (4.9) |
| Others | 13 (7.1) |
| Mixed | 30 (16.4) |
| Negative | 50 (29.5) |
| Number of prior procedures | 1.2 ± 1.1 |
| Laboratory Test | |
| Serum albumin, g/L | 38.5 ± 3.7 |
| Lymphocyte count, 109/L | 1.8 ± 0.6 |
| Total cholesterol, mmol/L | 165.9 ± 38.6 |
| C-reactive protein, mg/dL | 2.4 ± 2.6 |
| ESR, mm/h | 40.7 ± 26.8 |
| Indicator | CRP | ESR | CONUT | NPS | NRI |
|---|---|---|---|---|---|
| CONUT | r = 0.34, p < 0.001 | r = 0.16, p = 0.029 | r = 0.63, p < 0.001 | r = −0.52, p < 0.001 | |
| NPS | r = 0.34, p < 0.001 | r = 0.24, p = 0.001 | r = 0.63, p < 0.001 | r = −0.53, p < 0.001 | |
| NRI | r = −0.29, p < 0.001 | r = −0.31, p < 0.001 | r = −0.52, p < 0.001 | r = −0.53, p < 0.001 |
| MSIS Outcome | 1st Stage Exchange (n = 183) | 2nd Stage Exchange (n = 167) |
|---|---|---|
| Tier 1/2 | 130 (71.0) | 130 (77.8) |
| Tier 3 | 31 (16.9) | 18 (10.8) |
| Tier 3A | 4 (2.2) | 4 (2.4) |
| Tier 3B | 2 (1.1) | 2 (1.2) |
| Tier 3C | 3 (1.6) | 3 (1.8) |
| Tier 3D | 6 (3.3) | 6 (3.6) |
| Tier 3E | 3 (1.6) | 3 (1.8) |
| Tier 3F | 13 (7.1) | - |
| Tier 4 | 22 (12.0) | 19 (11.4) |
| Tier 4A | 5 (2.7) | 2 (1.2) |
| Tier 4B | 17 (9.3) | 17 (10.2) |
| Definition | Failure Rate | OR * (95% CI) | p | |
|---|---|---|---|---|
| Malnutrition at 1st Stage | ||||
| CONUT | Normal | 13/95 (13.7%) | Reference Category | |
| Mild | 13/73 (17.8%) | 1.07 (0.38–3.01) | 0.891 | |
| Moderate-to-severe | 6/15 (40.0%) | 5.86 (1.39–24.67) | 0.016 | |
| NPS | Normal | 2/22 (9.1%) | Reference Category | |
| Mild | 12/91 (13.2%) | 1.06 (0.18–6.14) | 0.945 | |
| Moderate-to-severe | 18/70 (25.7%) | 2.32 (0.41–12.96) | 0.239 | |
| NRI | Normal | 13/81 (16.0%) | Reference Category | |
| Mild | 4/30 (13.3%) | 0.55 (0.13–2.30) | 0.415 | |
| Moderate-to-severe | 15/72 (20.8%) | 0.86 (0.27–2.15) | 0.603 | |
| Malnutrition at 2nd Stage | ||||
| CONUT | Normal | 7/111 (6.3%) | Reference Category | |
| Mild | 7/49 (14.3%) | 3.86 (1.03–14.44) | 0.045 | |
| Moderate-to-severe | 2/7 (28.6%) | 12.15 (1.14–129.36) | 0.039 | |
| NPS | Normal | 1/40 (2.5%) | Reference Category | |
| Mild | 10/96 (10.4%) | 11.26 (0.92–138.22) | 0.068 | |
| Moderate-to-severe | 5/31 (16.1%) | 14.39 (1.27–266.22) | 0.033 | |
| NRI | Normal | 8/115 (7.0%) | Reference Category | |
| Mild | 2/20 (10.0%) | 1.94 (0.28–13.41) | 0.501 | |
| Moderate-to-severe | 6/32 (18.8%) | 3.60 (0.84–15.36) | 0.083 | |
| Variables | Odds Ratio | 95% CI | p |
|---|---|---|---|
| Age ≥ 68 | 5.35 | 1.17–24.52 | 0.031 |
| Female gender | 0.31 | 0.07–1.26 | 0.101 |
| Number of previous surgeries | 2.04 | 1.20–3.50 | 0.009 |
| Primary diagnosis | |||
| Osteoarthritis | Reference Category | ||
| ONFH | 0.11 | 0.01–0.87 | 0.037 |
| Inflammatory arthropathy | 7.16 | 0.51–101.45 | 0.146 |
| Fracture | 0.17 | 0.02–1.29 | 0.087 |
| Others | 1.41 | 0.20–9.86 | 0.729 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Li, Z.; Maimaiti, Z.; Li, Z.-Y.; Fu, J.; Hao, L.-B.; Xu, C.; Chen, J.-Y. Moderate-to-Severe Malnutrition Identified by the Controlling Nutritional Status (CONUT) Score Is Significantly Associated with Treatment Failure of Periprosthetic Joint Infection. Nutrients 2022, 14, 4433. https://doi.org/10.3390/nu14204433
Li Z, Maimaiti Z, Li Z-Y, Fu J, Hao L-B, Xu C, Chen J-Y. Moderate-to-Severe Malnutrition Identified by the Controlling Nutritional Status (CONUT) Score Is Significantly Associated with Treatment Failure of Periprosthetic Joint Infection. Nutrients. 2022; 14(20):4433. https://doi.org/10.3390/nu14204433
Chicago/Turabian StyleLi, Zhuo, Zulipikaer Maimaiti, Zhi-Yuan Li, Jun Fu, Li-Bo Hao, Chi Xu, and Ji-Ying Chen. 2022. "Moderate-to-Severe Malnutrition Identified by the Controlling Nutritional Status (CONUT) Score Is Significantly Associated with Treatment Failure of Periprosthetic Joint Infection" Nutrients 14, no. 20: 4433. https://doi.org/10.3390/nu14204433
APA StyleLi, Z., Maimaiti, Z., Li, Z.-Y., Fu, J., Hao, L.-B., Xu, C., & Chen, J.-Y. (2022). Moderate-to-Severe Malnutrition Identified by the Controlling Nutritional Status (CONUT) Score Is Significantly Associated with Treatment Failure of Periprosthetic Joint Infection. Nutrients, 14(20), 4433. https://doi.org/10.3390/nu14204433






