The Australian Feeding Infants and Toddlers Study (OzFITS) 2021: Highlights and Future Directions
Abstract
1. Introduction
2. Summary of Key Findings and Implications
2.1. Breastfeeding, Breast Milk Substitutes, and the Introduction of Complementary Foods
2.2. Introduction to Common Food Allergens
2.3. Foods and Drinks
2.4. Nutrient Intakes
2.5. Iron Intakes
2.6. Sodium Intakes
3. Other Findings
3.1. Pouches
3.2. Juice and Smoothies
3.3. Alternative Diets
3.4. Impact of the COVID-19 Global Pandemic
4. Gaps in Evidence and Areas for Future Research
4.1. Need for National Representative Survey of 0-2-Year-Olds
4.2. Estimating Breastmilk Intake and Nutrient Composition
4.3. Inclusion of Breastmilk in Food-Based Dietary Guidelines
4.4. Improved Nutrient Reference Values for Infants and Young Children
4.5. The Need to Measure Nutrient Biomarkers in Infants and Toddlers
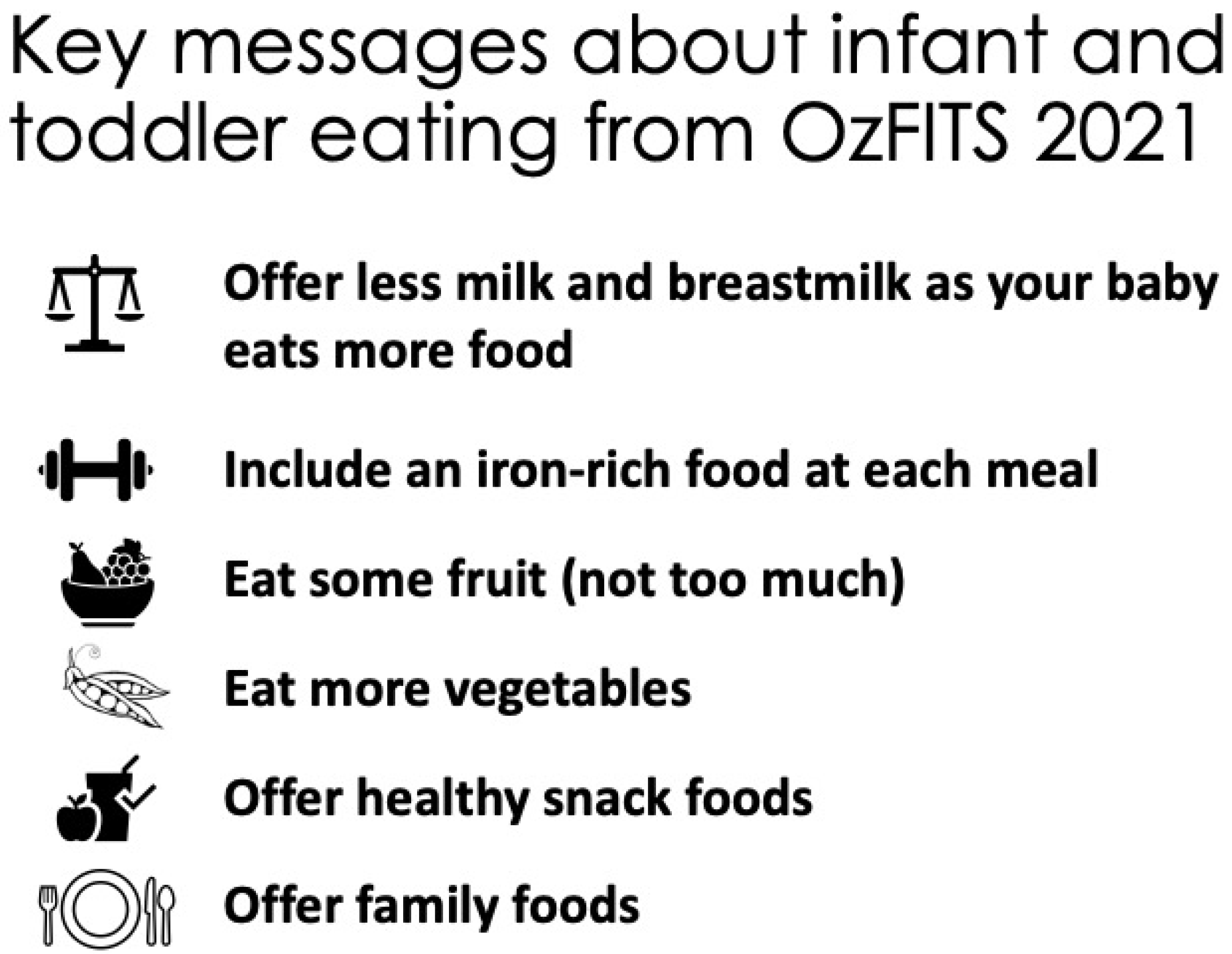
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Black, R.E.; Allen, L.H.; Bhutta, Z.A.; Caulfield, L.E.; de Onis, M.; Ezzati, M.; Mathers, C.; Rivera, J. Maternal and child undernutrition: Global and regional exposures and health consequences. Lancet 2008, 371, 243–260. [Google Scholar] [CrossRef]
- Shrimpton, R.; Victora, C.G.; de Onis, M.; Lima, R.C.; Blössner, M.; Clugston, G. Worldwide timing of growth faltering: Implications for nutritional interventions. Pediatrics 2001, 107, E75. [Google Scholar] [CrossRef] [PubMed]
- Monteiro, P.O.; Victora, C.G. Rapid growth in infancy and childhood and obesity in later life–A systematic review. Obes. Rev. 2005, 6, 143–154. [Google Scholar] [CrossRef] [PubMed]
- Tang, M.; Dewey, K.G.; Krebs, N.F. Nutritional Requirements in the Life Stages. In The Biology of the First 1000 Days; Klaus, K., Tim, J.G., Crysta, D.K., Kyly, C.W., Eds.; CRC Press: Boca Raton, FL, USA, 2018; pp. 75–86. [Google Scholar]
- Australian Institute of Health and Welfare. 2010 Australian National Infant Feeding Survey: Indicator Results; Australian Institute of Health and Welfare: Canberra, Australia, 2011.
- Moumin, N.A.; Golley, R.K.; Mauch, C.E.; Makrides, M.; Green, T.J.; Netting, M.J. The Australian Feeding Infants and Toddlers Study (OzFITS) 2021: Study Design, Methods and Sample Description. Nutrients 2021, 13, 4524. [Google Scholar] [CrossRef] [PubMed]
- National Health and Medical Research Council. Infant Feeding Guidelines Information for Health Workers; National Health and Medical Research Council: Canberra, Australia, 2012.
- Netting, M.J.; Moumin, N.A.; Knight, E.J.; Golley, R.K.; Makrides, M.; Green, T.J. The Australian Feeding Infants and Toddler Study (OzFITS 2021): Breastfeeding and Early Feeding Practices. Nutrients 2022, 14, 206. [Google Scholar] [CrossRef] [PubMed]
- Abrams, E.M.; Sicherer, S.H. Cow’s milk allergy prevention. Ann. Allergy Asthma Immunol. 2021, 127, 36–41. [Google Scholar] [CrossRef] [PubMed]
- Carlo, A.; Tamas, D.; Mary, F.; Olivier, G.; Sanja, K.; Berthold, K.; Fleischer, M.K.; Luis, M.; John, P.; Jacques, R.; et al. Complementary feeding: A commentary by the ESPGHAN Committee on Nutrition. J. Pediatr. Gastroenterol. Nutr. 2008, 46, 99–110. [Google Scholar]
- Du Toit, G.; Roberts, G.; Sayre, P.H.; Bahnson, H.T.; Radulovic, S.; Santos, A.F.; Brough, H.A.; Phippard, D.; Basting, M.; Feeney, M.; et al. Randomized trial of peanut consumption in infants at risk for peanut allergy. N. Engl. J. Med. 2015, 372, 803–813. [Google Scholar] [CrossRef]
- Perkin, M.R.; Logan, K.; Tseng, A.; Raji, B.; Ayis, S.; Peacock, J.; Brough, H.; Marrs, T.; Radulovic, S.; Craven, J.; et al. Randomized Trial of Introduction of Allergenic Foods in Breast-Fed Infants. N. Engl. J. Med. 2016, 374, 1733–1743. [Google Scholar] [CrossRef]
- Guidelines: Infant Feeding and Allergy Prevention. Available online: https://www.allergy.org.au/images/pcc/ASCIA_Guidelines_Infant_Feeding_and_Allergy_Prevention_2020.pdf (accessed on 24 August 2022).
- Netting, M.J.; Gold, M.S.; Quinn, P.; Palmer, S.; Makrides, M.; Green, T.J. Does SMS text messaging promote the early introduction of food allergens? A randomized controlled trial. Pediatr. Allergy Immunol. 2022, 33, e13720. [Google Scholar]
- National Health and Medical Research Council. Eat for Health Educator Guide; National Health and Medical Research Council: Canberra, Australia, 2013.
- Baghurst, K.; Cobiac, L.; Baghurst, P.; Magary, A.; Bryon, A. A Modelling System to Inform the Revision of the Australian Guide to Healthy Eating; Dietitians Association of Australia for Department of Health and Ageing and National Health and Medical Research Council: Canberra, Australia, 2011.
- Moumin, N.A.; Netting, M.J.; Golley, R.K.; Mauch, C.E.; Makrides, M.; Green, T.J. Does Food Intake of Australian Toddlers 12–24 Months Align with Recommendations: Findings from the Australian Feeding Infants and Toddlers Study (OzFITS) 2021. Nutrients 2022, 14, 2890. [Google Scholar] [CrossRef] [PubMed]
- Victora, C.G.; Bahl, R.; Barros, A.J.D.; França, G.V.A.; Horton, S.; Krasevec, J.; Murch, S.; Sankar, M.J.; Walker, N.; Rollins, N.C.; et al. Breastfeeding in the 21st century: Epidemiology, mechanisms, and lifelong effect. Lancet 2016, 387, 475–490. [Google Scholar] [CrossRef]
- Scott, J.; Davey, K.; Ahwong, E.; Devenish, G.; Ha, D.; Do, L. A Comparison by Milk Feeding Method of the Nutrient Intake of a Cohort of Australian Toddlers. Nutrients 2016, 8, 501. [Google Scholar] [CrossRef] [PubMed]
- Moumin, N.A.; Netting, M.J.; Golley, R.K.; Mauch, C.E.; Makrides, M.; Green, T.J. Usual Nutrient Intake Distribution and Prevalence of Inadequacy among Australian Children 0–24 Months: Findings from the Australian Feeding Infants and Toddlers Study (OzFITS) 2021. Nutrients 2022, 14, 1381. [Google Scholar] [CrossRef] [PubMed]
- Bailey, R.L.; Catellier, D.J.; Jun, S.; Dwyer, J.T.; Jacquier, E.F.; Anater, A.S.; Eldridge, A.L. Total Usual Nutrient Intakes of US Children (Under 48 Months): Findings from the Feeding Infants and Toddlers Study (FITS) 2016. J. Nutr. 2018, 148, 1557S–1566S. [Google Scholar] [CrossRef] [PubMed]
- Roess, A.A.; Jacquier, E.F.; Catellier, D.J.; Carvalho, R.; Lutes, A.C.; Anater, A.S.; Dietz, W.H. Food Consumption Patterns of Infants and Toddlers: Findings from the Feeding Infants and Toddlers Study (FITS) 2016. J. Nutr. 2018, 148, 1525S–1535S. [Google Scholar] [CrossRef]
- Leyvraz, M.; Chatelan, A.; da Costa, B.R.; Taffé, P.; Paradis, G.; Bovet, P.; Bochud, M.; Chiolero, A. Sodium intake and blood pressure in children and adolescents: A systematic review and meta-analysis of experimental and observational studies. Int. J. Epidemiol. 2018, 47, 1796–1810. [Google Scholar] [CrossRef]
- Bao, W.; Threefoot, S.A.; Srinivasan, S.R.; Berenson, G.R. Essential hypertension predicted by tracking of elevated blood pressure from childhood to adulthood: The Bogalusa Heart Study. Am. J. Hypertens 1995, 8, 657–665. [Google Scholar] [CrossRef]
- Webster, J.; Trieu, K.; Dunford, E.; Nowson, C.; Jolly, K.-A.; Greenland, G.R.; Reimers, J.; Bolam, B. Salt reduction in Australia: From advocacy to action. Cardiovasc. Diagn. Ther. 2015, 5, 207–218. [Google Scholar]
- Partnership Reformulation Program: Food Categories and Reformulation Targets. Available online: https://www.health.gov.au/sites/default/files/documents/2021/07/partnership-reformulation-program-summary-of-food-categories-and-reformulation-targets-food-reformulation-program-summary-of-food-categories-and-reformulation-targets.pdf (accessed on 23 September 2022).
- Moumin, N.A.; Green, T.J.; Golley, R.K.; Netting, M.J. Are the nutrient and textural properties of Australian commercial infant and toddler foods consistent with infant feeding advice? Br. J.Nutr. 2020, 124, 754–760. [Google Scholar] [CrossRef]
- Koletzko, B.; Bührer, C.; Ensenauer, R.; Jochum, F.; Kalhoff, H.; Lawrenz, B.; Körner, A.; Mihatsch, W.; Rudloff, S.; Zimmer, K.-P. Complementary foods in baby food pouches: Position statement from the Nutrition Commission of the German Society for Pediatrics and Adolescent Medicine (DGKJ, e.V.). Mol. Cell Pediatr. 2019, 6, 2. [Google Scholar] [CrossRef] [PubMed]
- Mills, A.; Tyler, H. Food and Nutrient Intakes of British Infants Aged 6–12 Months; Her Majesty’s Stationary Office: London, UK, 1992. [Google Scholar]
- Paul, A.; Black, A.E.; Evans, J.; Cole, T.J.; Whitehead, R.G. Breastmilk intake and growth in infants from two to ten months. Hum. Nutr. Diet. 1988, 1, 437–450. [Google Scholar] [CrossRef]
- Berube, L.T.; Gross, R.; Messito, M.J.; Deierlein, A.; Katzow, M.; Woolf, K. Concerns About Current Breast Milk Intake Measurement for Population-Based Studies. J. Acad. Nutr. Diet. 2018, 118, 1827–1831. [Google Scholar]
- National Health and Medical Research Council. Nutrient Reference Values for Australia and New Zealand Including Recommended Dietary Intakes; National Health and Medical Research Council: Canberra, Australia, 2006.
- Food Standards Australia New Zealand. Australian Food, Supplement and Nutrient Database; Food Standards Australia New Zealand: Canberra, Australia, 2013.
- Ward, E.; Yang, N.; Muhlhausler, B.S.; Leghi, G.E.; Netting, M.J.; Elmes, M.J.; Langley-Evans, S.C. Acute changes to breast milk composition following consumption of high-fat and high-sugar meals. Matern. Child Nutr. 2021, 17, e13168. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Netting, M.J.; Moumin, N.A.; Makrides, M.; Green, T.J. The Australian Feeding Infants and Toddlers Study (OzFITS) 2021: Highlights and Future Directions. Nutrients 2022, 14, 4343. https://doi.org/10.3390/nu14204343
Netting MJ, Moumin NA, Makrides M, Green TJ. The Australian Feeding Infants and Toddlers Study (OzFITS) 2021: Highlights and Future Directions. Nutrients. 2022; 14(20):4343. https://doi.org/10.3390/nu14204343
Chicago/Turabian StyleNetting, Merryn J., Najma A. Moumin, Maria Makrides, and Tim J. Green. 2022. "The Australian Feeding Infants and Toddlers Study (OzFITS) 2021: Highlights and Future Directions" Nutrients 14, no. 20: 4343. https://doi.org/10.3390/nu14204343
APA StyleNetting, M. J., Moumin, N. A., Makrides, M., & Green, T. J. (2022). The Australian Feeding Infants and Toddlers Study (OzFITS) 2021: Highlights and Future Directions. Nutrients, 14(20), 4343. https://doi.org/10.3390/nu14204343





