External Validation with Accuracy Confounders of VCO2-Derived Predicted Energy Expenditure Compared to Resting Energy Expenditure Measured by Indirect Calorimetry in Mechanically Ventilated Children
Abstract
1. Introduction
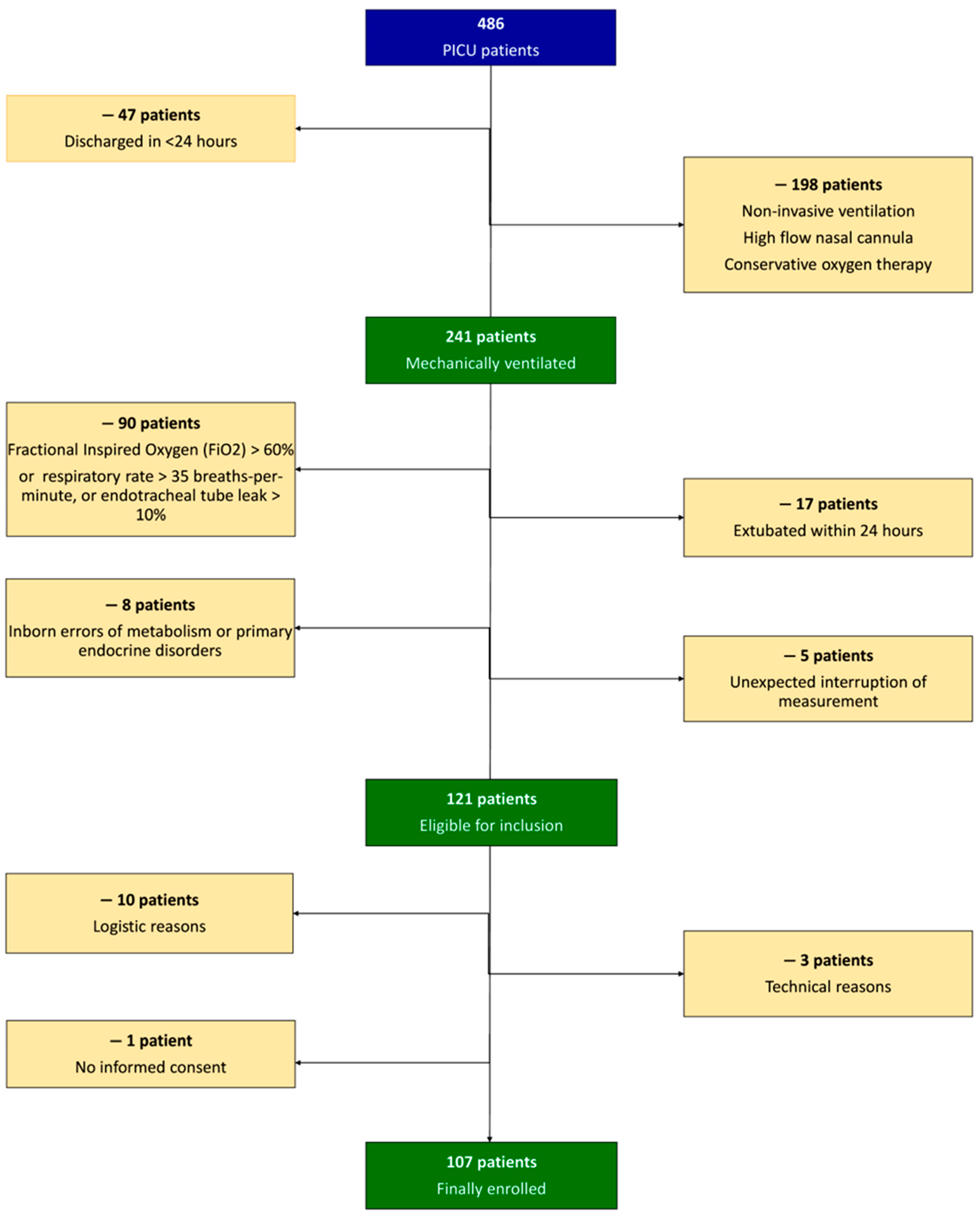
2. Materials and Methods
2.1. Study Design
2.2. Clinical Data
2.3. Anthropometry
2.4. Indirect Calorimetry
2.5. VCO2-Derived REE
2.6. Statistical Analysis
3. Results
3.1. Study Population
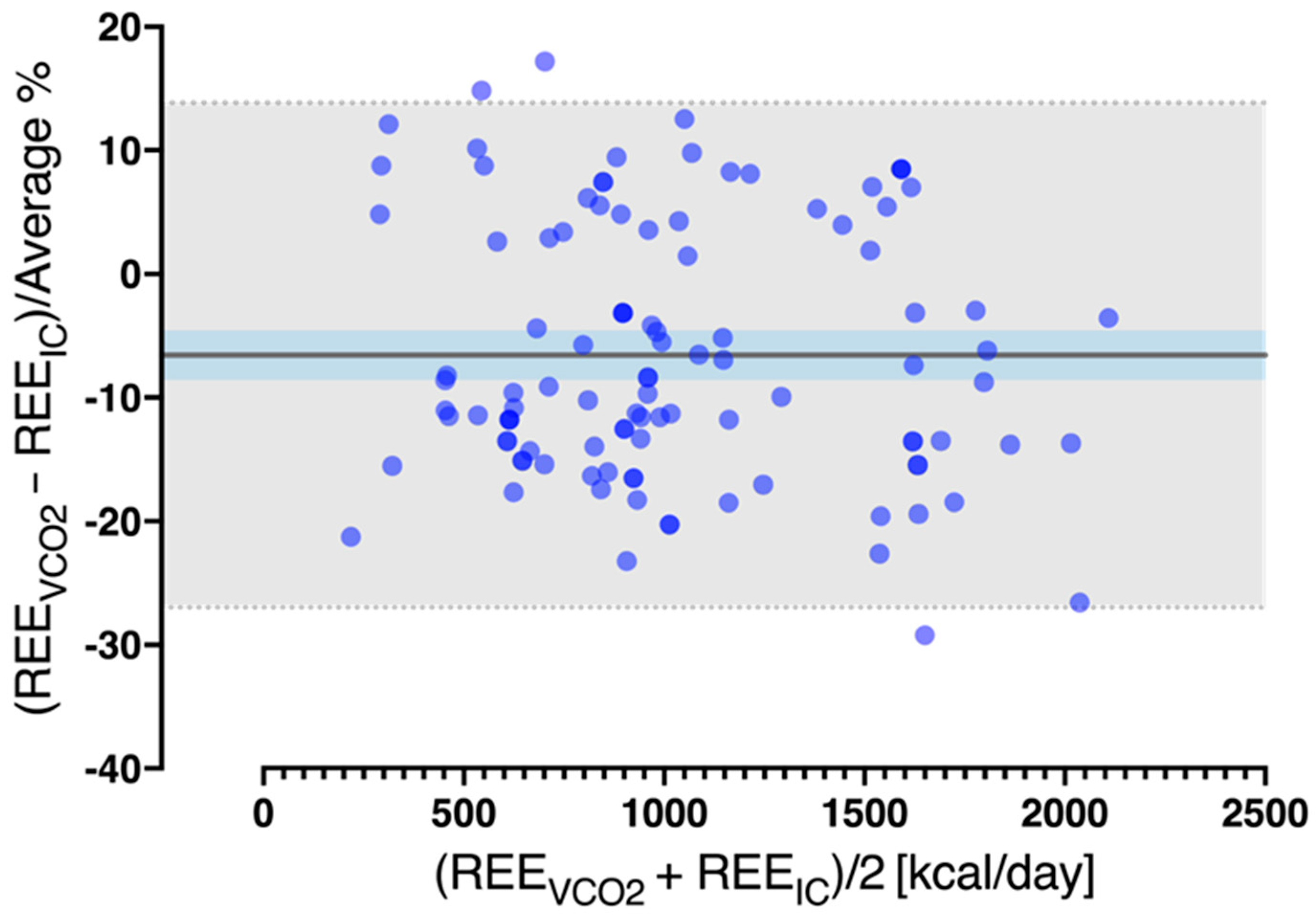
3.2. Performance of the REEVCO2 Equation
3.3. REEVCO2 Using Different RQ Values
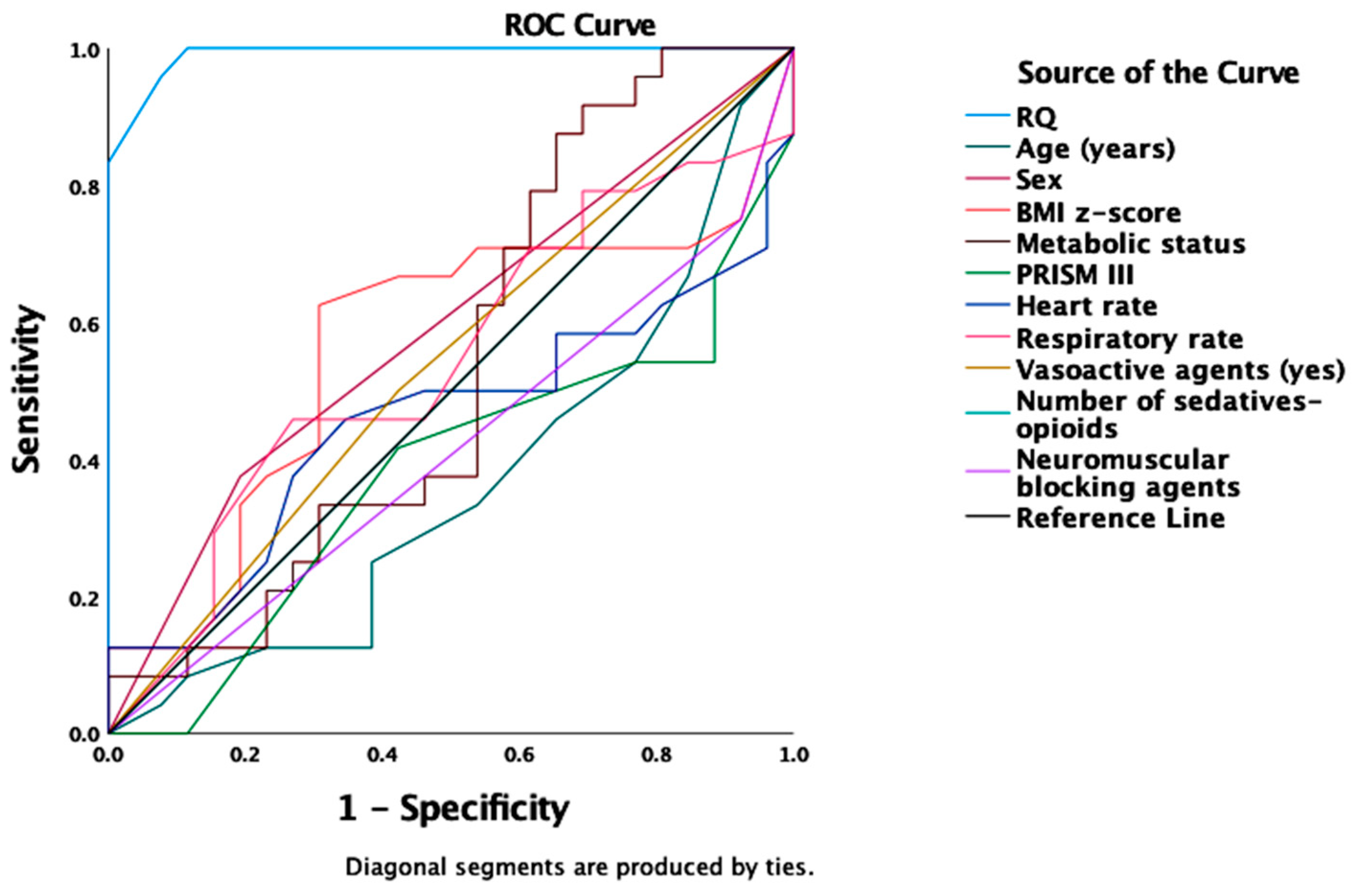
3.4. Factors Affecting the REEVCO2 Accuracy
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Compher, C.; Bingham, A.L.; McCall, M.; Patel, J.; Rice, T.W.; Braunschweig, C.; McKeever, L. Guidelines for the Provision of Nutrition Support Therapy in the Adult Critically Ill Patient: The American Society for Parenteral and Enteral Nutrition. JPEN J. Parenter. Enter. Nutr. 2022, 46, 12–41. [Google Scholar] [CrossRef] [PubMed]
- Tume, L.N.; Valla, F.V.; Joosten, K.; Jotterand Chaparro, C.; Latten, L.; Marino, L.V.; Macleod, I.; Moullet, C.; Pathan, N.; Rooze, S.; et al. Nutritional Support for Children during Critical Illness: European Society of Pediatric and Neonatal Intensive Care (ESPNIC) Metabolism, Endocrine and Nutrition Section Position Statement and Clinical Recommendations. Intensive Care Med. 2020, 46, 411–425. [Google Scholar] [CrossRef] [PubMed]
- Weir, J.B. New Methods for Calculating Metabolic Rate with Special Reference to Protein Metabolism. 1949. Nutrition 1990, 6, 213–221. [Google Scholar] [PubMed]
- Briassoulis, G.; Briassoulis, P.; Michaeloudi, E.; Fitrolaki, D.-M.; Spanaki, A.-M.; Briassouli, E. The Effects of Endotracheal Suctioning on the Accuracy of Oxygen Consumption and Carbon Dioxide Production Measurements and Pulmonary Mechanics Calculated by a Compact Metabolic Monitor. Anesth. Analg. 2009, 109, 873–879. [Google Scholar] [CrossRef] [PubMed]
- Briassoulis, G.; Michaeloudi, E.; Fitrolaki, D.-M.; Spanaki, A.-M.; Briassouli, E. Influence of Different Ventilator Modes on Vo(2) and Vco(2) Measurements Using a Compact Metabolic Monitor. Nutrition 2009, 25, 1106–1114. [Google Scholar] [CrossRef]
- Meyer, R.; Kulinskaya, E.; Briassoulis, G.; Taylor, R.M.; Cooper, M.; Pathan, N.; Habibi, P. The Challenge of Developing a New Predictive Formula to Estimate Energy Requirements in Ventilated Critically Ill Children. Nutr. Clin. Pract. 2012, 27, 669–676. [Google Scholar] [CrossRef]
- Briassoulis, G.; Venkataraman, S.; Thompson, A.E. Energy Expenditure in Critically Ill Children. Crit. Care Med. 2000, 28, 1166–1172. [Google Scholar] [CrossRef] [PubMed]
- Mehta, N.M.; Bechard, L.J.; Cahill, N.; Wang, M.; Day, A.; Duggan, C.P.; Heyland, D.K. Nutritional Practices and Their Relationship to Clinical Outcomes in Critically Ill Children—An International Multicenter Cohort Study. Crit. Care Med. 2012, 40, 2204–2211. [Google Scholar] [CrossRef]
- Stapel, S.N.; de Grooth, H.-J.S.; Alimohamad, H.; Elbers, P.W.G.; Girbes, A.R.J.; Weijs, P.J.M.; Oudemans-van Straaten, H.M. Ventilator-Derived Carbon Dioxide Production to Assess Energy Expenditure in Critically Ill Patients: Proof of Concept. Crit. Care 2015, 19, 370. [Google Scholar] [CrossRef] [PubMed]
- Mehta, N.M.; Smallwood, C.D.; Joosten, K.F.M.; Hulst, J.M.; Tasker, R.C.; Duggan, C.P. Accuracy of a Simplified Equation for Energy Expenditure Based on Bedside Volumetric Carbon Dioxide Elimination Measurement—A Two-Center Study. Clin. Nutr. 2015, 34, 151–155. [Google Scholar] [CrossRef] [PubMed]
- Rousing, M.L.; Hahn-Pedersen, M.H.; Andreassen, S.; Pielmeier, U.; Preiser, J.-C. Energy Expenditure in Critically Ill Patients Estimated by Population-Based Equations, Indirect Calorimetry and CO2-Based Indirect Calorimetry. Ann. Intensive Care 2016, 6, 16. [Google Scholar] [CrossRef] [PubMed]
- Oshima, T.; Graf, S.; Heidegger, C.-P.; Genton, L.; Pugin, J.; Pichard, C. Can Calculation of Energy Expenditure Based on CO2 Measurements Replace Indirect Calorimetry? Crit. Care 2017, 21, 13. [Google Scholar] [CrossRef]
- World Medical Association World Medical Association Declaration of Helsinki: Ethical Principles for Medical Research Involving Human Subjects. JAMA 2013, 310, 2191–2194. [CrossRef] [PubMed]
- Ferreruela, M.; Raurich, J.M.; Llompart-Pou, J.A.; Colomar, A.; Ayestarán, I. Effect of FiO2 in the Measurement of VO2 and VCO2 Using the E-COXV Metabolic Monitor. Med. Intensive 2017, 41, 461–467. [Google Scholar] [CrossRef] [PubMed]
- Shen, Y.; Jiang, J. Meta-Analysis for the Prediction of Mortality Rates in a Pediatric Intensive Care Unit Using Different Scores: PRISM-III/IV, PIM-3, and PELOD-2. Front. Pediatr. 2021, 9, 712276. [Google Scholar] [CrossRef] [PubMed]
- Trope, R.; Vaz, S.; Zinger, M.; Sagy, M. An Updated Therapeutic Intervention Scoring System for Critically Ill Children Enables Nursing Workload Assessment With Insight Into Potential Untoward Events. J. Intensive Care Med. 2015, 30, 344–350. [Google Scholar] [CrossRef]
- CDC BMI Calculator for Child and Teen. Available online: https://www.cdc.gov/healthyweight/bmi/calculator.html (accessed on 3 August 2022).
- Mouzaki, M.; Schwartz, S.M.; Mtaweh, H.; La Rotta, G.; Mah, K.; Herridge, J.; Van Arsdell, G.; Parshuram, C.S.; Floh, A.A. Can Vco2-Based Estimates of Resting Energy Expenditure Replace the Need for Indirect Calorimetry in Critically Ill Children? JPEN J. Parenter. Enter. Nutr. 2017, 41, 619–624. [Google Scholar] [CrossRef]
- Kagan, I.; Zusman, O.; Bendavid, I.; Theilla, M.; Cohen, J.; Singer, P. Validation of Carbon Dioxide Production (VCO2) as a Tool to Calculate Resting Energy Expenditure (REE) in Mechanically Ventilated Critically Ill Patients: A Retrospective Observational Study. Crit. Care 2018, 22, 186. [Google Scholar] [CrossRef]
- Schofield, W.N. Predicting Basal Metabolic Rate, New Standards and Review of Previous Work. Hum. Nutr. Clin. Nutr. 1985, 39 (Suppl. 1), 5–41. [Google Scholar]
- Koo, T.K.; Li, M.Y. A Guideline of Selecting and Reporting Intraclass Correlation Coefficients for Reliability Research. J. Chiropr. Med 2016, 15, 155–163. [Google Scholar] [CrossRef]
- Spanaki, A.M.; Tavladaki, T.; Dimitriou, H.; Kozlov, A.V.; Duvigneau, J.C.; Meleti, E.; Weidinger, A.; Papakonstantinou, E.; Briassoulis, G. Longitudinal Profiles of Metabolism and Bioenergetics Associated with Innate Immune Hormonal Inflammatory Responses and Amino-Acid Kinetics in Severe Sepsis and Systemic Inflammatory Response Syndrome in Children. JPEN J. Parenter. Enter. Nutr. 2018, 42, 1061–1074. [Google Scholar] [CrossRef] [PubMed]
- Oshima, T.; Berger, M.M.; De Waele, E.; Guttormsen, A.B.; Heidegger, C.-P.; Hiesmayr, M.; Singer, P.; Wernerman, J.; Pichard, C. Indirect Calorimetry in Nutritional Therapy. A Position Paper by the ICALIC Study Group. Clin. Nutr. 2017, 36, 651–662. [Google Scholar] [CrossRef]
- Chiumello, D.; Coppola, S.; Froio, S.; Mietto, C.; Brazzi, L.; Carlesso, E.; Gattinoni, L. Time to Reach a New Steady State after Changes of Positive End Expiratory Pressure. Intensive Care Med. 2013, 39, 1377–1385. [Google Scholar] [CrossRef] [PubMed]
- Frankenfield, D.C. Impact of Feeding on Resting Metabolic Rate and Gas Exchange in Critically Ill Patients. JPEN J. Parenter. Enter. Nutr. 2019, 43, 226–233. [Google Scholar] [CrossRef] [PubMed]
- McClave, S.A.; Lowen, C.C.; Kleber, M.J.; McConnell, J.W.; Jung, L.Y.; Goldsmith, L.J. Clinical Use of the Respiratory Quotient Obtained from Indirect Calorimetry. JPEN J. Parenter. Enter. Nutr. 2003, 27, 21–26. [Google Scholar] [CrossRef]
- Hirayama, I.; Asada, T.; Yamamoto, M.; Hayase, N.; Hiruma, T.; Doi, K. Changes in Carbon Dioxide Production and Oxygen Uptake Evaluated Using Indirect Calorimetry in Mechanically Ventilated Patients with Sepsis. Crit. Care 2021, 25, 416. [Google Scholar] [CrossRef]
- Hoeyer-Nielsen, A.K.; Holmberg, M.J.; Grossestreuer, A.V.; Yankama, T.; Branton, J.-P.; Donnino, M.W.; Berg, K.M. Association Between the Oxygen Consumption: Lactate Ratio and Survival in Critically Ill Patients With Sepsis. Shock 2021, 55, 775–781. [Google Scholar] [CrossRef]
- Ilia, S.; Briassoulis, G. Sepsis Is Change and Flows Ever Onwards. Expert Rev. Anti-Infect. Ther. 2017, 15, 515–517. [Google Scholar] [CrossRef][Green Version]
- Tavladaki, T.; Spanaki, A.M.; Dimitriou, H.; Kondili, E.; Choulaki, C.; Georgopoulos, D.; Briassoulis, G. Similar Metabolic, Innate Immunity, and Adipokine Profiles in Adult and Pediatric Sepsis Versus Systemic Inflammatory Response Syndrome-A Pilot Study. Pediatr. Crit. Care Med. 2017, 18, e494–e505. [Google Scholar] [CrossRef]
- Briassoulis, G.; Briassouli, E.; Tavladaki, T.; Ilia, S.; Fitrolaki, D.M.; Spanaki, A.M. Unpredictable Combination of Metabolic and Feeding Patterns in Malnourished Critically Ill Children: The Malnutrition-Energy Assessment Question. Intensive Care Med. 2014, 40, 120–122. [Google Scholar] [CrossRef]
- Mehta, N.M.; Bechard, L.J.; Leavitt, K.; Duggan, C. Cumulative Energy Imbalance in the Pediatric Intensive Care Unit: Role of Targeted Indirect Calorimetry. JPEN J. Parenter. Enter. Nutr. 2009, 33, 336–344. [Google Scholar] [CrossRef] [PubMed]
- Moonen, H.P.F.X.; Beckers, K.J.H.; van Zanten, A.R.H. Energy Expenditure and Indirect Calorimetry in Critical Illness and Convalescence: Current Evidence and Practical Considerations. J. Intensive Care 2021, 9, 8. [Google Scholar] [CrossRef] [PubMed]
- Poulsen, M.K.; Thomsen, L.P.; Kjaergaard, S.; Rees, S.E.; Karbing, D.S. Reliability of, and Agreement Between, Two Breath-by-Breath Indirect Calorimeters at Varying Levels of Inspiratory Oxygen. Nutr. Clin. Pract. 2019, 34, 767–774. [Google Scholar] [CrossRef] [PubMed]


| Characteristic | Variable | N = 107 |
|---|---|---|
| Demographic | Age (years) | 9.2 ± 5.3 |
| Sex (boy/girl) | 75/32 (70.1%/29.9%) | |
| Body weight (kg) | 35.9 ± 26 | |
| Height (cm) | 129 ± 29 | |
| BMI (kg/m2) | 18.7 ± 6 | |
| z-score weight for age | 0.33 (−1.5; 1.6) | |
| z-score height for age | −0.02 (−0.48; 0.66) | |
| z-score BMI for age | 0.22 (−1.26; 1.68) | |
| Underweight | 23 (21.5%) | |
| Normal BMI | 47 (43.9%) | |
| Overweight | 10 (9.3%) | |
| Obese | 27 (25.2%) | |
| Reasons for PICU admission | Respiratory failure | 25 (23.4%) |
| Sepsis | 20 (18.7%) | |
| Surgical | 9 (8.4%) | |
| Organ failure | 2 (1.9%) | |
| Trauma | 28 (26.2%) | |
| Neurologic | 23 (21.5%) | |
| Clinical data | PRISM score | 11 (8; 15) |
| TISS score | 43 (36; 47) | |
| PELOD score | 7 (3; 19) | |
| FiO2 (%) | 35 (30; 50) | |
| pH | 7.38 (7.34; 7.42) | |
| pO2 (mmHg) | 112 (94; 121) | |
| pCO2 (mmHg) | 35 (33.9; 39.3) | |
| HCO3 (mEq/L) | 22.2 (19.0; 23.9) | |
| Heart Rate (bpm) | 98 (78; 117) | |
| Respiratory rate (bpm) | 20 (16; 28) | |
| Systolic Blood Pressure (mmHg) | 94 (75; 110) | |
| Body Temperature (° Celsius) | 37.4 (36.7; 38.1) | |
| Lactate (mg/dL) | 14.1 (6.9; 31) | |
| Glucose (mg/dL) | 105 (94; 121) | |
| Albumin (mg/dL) | 3.2 (2.6; 3.6) | |
| C-Reactive Protein (mg/dL) | 9.7 (2.2; 18) | |
| Vasoactive agents (yes) (%) | 58 (54.24%) | |
| Sedatives and/or opioids > 2 (%) | 91 (85%) | |
| Neuromuscular blocking agents (yes) (%) | 23 (21.5%) | |
| Length of Stay (days) | 14 (7; 24) | |
| Mechanical Ventilation (days) | 12 (7; 18) | |
| Hospital Mortality | 4 (3.7%) | |
| Nutrition | Energy intake (kcal/day) | 720 (480; 1000) |
| Energy intake/IBW (kcal/kg/day) | 24 (13.2; 42.8) | |
| Adequate feeding | 38 (35.5%) | |
| Underfeeding | 50 (46.7%) | |
| Overfeeding | 19 (17.8%) |
| Variables | N = 107 |
|---|---|
| VO2 (mL/min) | 144.8 (105; 207.5) |
| VCO2 (mL/min) | 115 (84.2; 175.4) |
| Respiratory Quotient | 0.81 (0.75; 0.91) |
| REEIC (kcal/day) | 999 (703; 1416) |
| REEVCO2 (kcal/day) | 910.8 (667; 1389) |
| REEIC/IBW (kcal/kg/day) | 32.8 (24; 48.6) |
| REEVCO2/IBW (kcal/kg/day) | 29.3 (29.3; 44) |
| Mean Bias ± SD (kcal/day) * | −72.73 ± 127 |
| Limits of Agreement (kcal/day) * | −321.7 to 176.3 |
| 95% CI Lower-Upper (kcal/day) * | −92.8 to −49.9 |
| Coefficient of Variation (%) * | 174.7 |
| Median of Differences (95%CI) (kcal/day) # | −71.01 (−92.9; −49.9) |
| p value # | <0.001 |
| Cronbach’s alpha (kcal/day) ^ | 0.979 (0.970; 0.986) |
| p value ^ | <0.001 |
| REEVCO2 ± 10% of REEIC ** | 52 (48.6%) |
| REEVCO2 > 10% of REEIC ** | 6 (5.6%) |
| REEVCO2 < 10% of REEIC ** | 49 (45.8%) |
| Normometabolic + | 20 (18.7%) |
| Hypometabolic + | 63 (58.9%) |
| Hypermetabolic + | 24 (22.4%) |
| REE Estimation | REE (kcal/day) | Agreement—Precision * | Paired Differences—Variability # | Accuracy ^ | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Calculated REE (Reference) | Equation | Median | IQR (25th; 75th) | Mean Bias | SD | Limits of Agreement | Median of Differences | 95% CI of Differences Lower-Upper | CV (%) | p Value | REEVCO2 < 10% of REEIC | REEVCO2 ± 10% of REEIC | REEVCO2 > 10% of REEIC |
| N = 107 | |||||||||||||
| REEIC [3] | [3.941 × VO2 + 1.106 × VCO2] × 1440 | 999.0 | (703; 1416) | ||||||||||
| REEVCO2 [10] | 5.5 × VCO2 (L/min) × 1440 [10] | 910.8 | (667; 1389) | −72.73 | 127.0 | −321.7; 176.3 | −71.01 | −92.8; −49.9 | 174.7 | <0.001 | 49 (45.8) | 52 (48.6) | 6 (5.6) |
| REEVCO2 [18] | 5.534 × VCO2 (L/min) × 1440 [10] | 916.4 | (671; 1398) | −66.56 | 126.5 | −314.4; 181.3 | −64.02 | −87.2; −41.8 | 190 | <0.001 | 47 (43.9) | 53 (49.5) | 7 (6.5) |
| REEVCO2 fixed RQ 0.89 [19] | ((5.5 × (VCO2/0.89)) + (1.76 × VCO2) − 26) | 887.1 | (642.5; 1367) | −96.24 | 126.8 | −344.8; 152.3 | −94.38 | −116.6; −73.17 | 131.8 | <0.001 | 58 (54.2) | 46 (43) | 3 (2.8) |
| REEVCO2 fixed RQ 0.85 [19] | ((5.5 × (VCO2/0.85)) + (1.76 × VCO2) − 26) | 920.5 | (667; 1418) | −59.62 | 124.3 | −303.3; 184 | −64.73 | −84.62; −41.49 | 208.5 | <0.001 | 46 (43) | 51 (47.7) | 10 (9.3) |
| REEVCO2 fixed RQ 0.80 [19] | ((5.5 × (VCO2/0.80)) + (1.76 × VCO2) − 26) | 967 | (701.1; 1489) | −8.70 | 124.0 | −251; 234.4 | −29.66 | −46.21; 6.47 | 1427 | 0.332 | 21 (19.6) | 61 (57) | 25 (23.4) |
| REEVCO2 measured RQ by IC | ((5.5 × (VCO2/RQIC)) + (1.76 × VCO2) − 26) | 973.5 | (686.6; 1442) | −38.48 | 102.4 | −239.1; 162.2 | −24.15 | −26.61; −13.48 | 266 | <0.001 | 9 (8.4) | 96 (89.7) | 2 (1.9) |
| Asymptotic 95% Confidence Interval | |||||
|---|---|---|---|---|---|
| Test Result Variable(s) | Area | Std. Error * | Asymptotic Sig. ** | Lower Bound | Upper Bound |
| RQ | 0.991 | 0.008 | 0.000 | 0.975 | 1.00 |
| Age (years) | 0.365 | 0.079 | 0.101 | 0.209 | 0.52 |
| Sex | 0.591 | 0.081 | 0.268 | 0.432 | 0.751 |
| BMI z-score | 0.565 | 0.086 | 0.432 | 0.396 | 0.734 |
| Metabolic status | 0.537 | 0.084 | 0.655 | 0.372 | 0.701 |
| PRISM III | 0.381 | 0.081 | 0.151 | 0.222 | 0.541 |
| Heart rate | 0.458 | 0.086 | 0.607 | 0.289 | 0.626 |
| Number of sedatives-opiods | 0.5 | 0.083 | 0.996 | 0.338 | 0.662 |
| Vasoactive agents (yes) | 0.538 | 0.082 | 0.641 | 0.377 | 0.700 |
| Respiratory rate | 0.542 | 0.084 | 0.607 | 0.378 | 0.707 |
| Neuromuscular blocking agents (yes) | 0.413 | 0.082 | 0.294 | 0.253 | 0.574 |
| Asymptotic 95% Confidence Interval | |||||
|---|---|---|---|---|---|
| Test Result Variable(s) | Area | Std. Error * | Asymptotic Sig. ** | Lower Bound | Upper Bound |
| RQ | 0.804 | 0.082 | 0.013 | 0.643 | 0.966 |
| PRISM III | 0.819 | 0.088 | 0.009 | 0.646 | 0.992 |
| Neuromuscular blocking agents (yes) | 0.569 | 0.128 | 0.573 | 0.319 | 0.819 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Briassoulis, P.; Ilia, S.; Briassouli, E.; Briassoulis, G. External Validation with Accuracy Confounders of VCO2-Derived Predicted Energy Expenditure Compared to Resting Energy Expenditure Measured by Indirect Calorimetry in Mechanically Ventilated Children. Nutrients 2022, 14, 4211. https://doi.org/10.3390/nu14194211
Briassoulis P, Ilia S, Briassouli E, Briassoulis G. External Validation with Accuracy Confounders of VCO2-Derived Predicted Energy Expenditure Compared to Resting Energy Expenditure Measured by Indirect Calorimetry in Mechanically Ventilated Children. Nutrients. 2022; 14(19):4211. https://doi.org/10.3390/nu14194211
Chicago/Turabian StyleBriassoulis, Panagiotis, Stavroula Ilia, Efrossini Briassouli, and George Briassoulis. 2022. "External Validation with Accuracy Confounders of VCO2-Derived Predicted Energy Expenditure Compared to Resting Energy Expenditure Measured by Indirect Calorimetry in Mechanically Ventilated Children" Nutrients 14, no. 19: 4211. https://doi.org/10.3390/nu14194211
APA StyleBriassoulis, P., Ilia, S., Briassouli, E., & Briassoulis, G. (2022). External Validation with Accuracy Confounders of VCO2-Derived Predicted Energy Expenditure Compared to Resting Energy Expenditure Measured by Indirect Calorimetry in Mechanically Ventilated Children. Nutrients, 14(19), 4211. https://doi.org/10.3390/nu14194211







