Low Dietary Diversity for Recommended Food Groups Increases the Risk of Obesity among Children: Evidence from a Chinese Longitudinal Study
Abstract
:1. Introduction
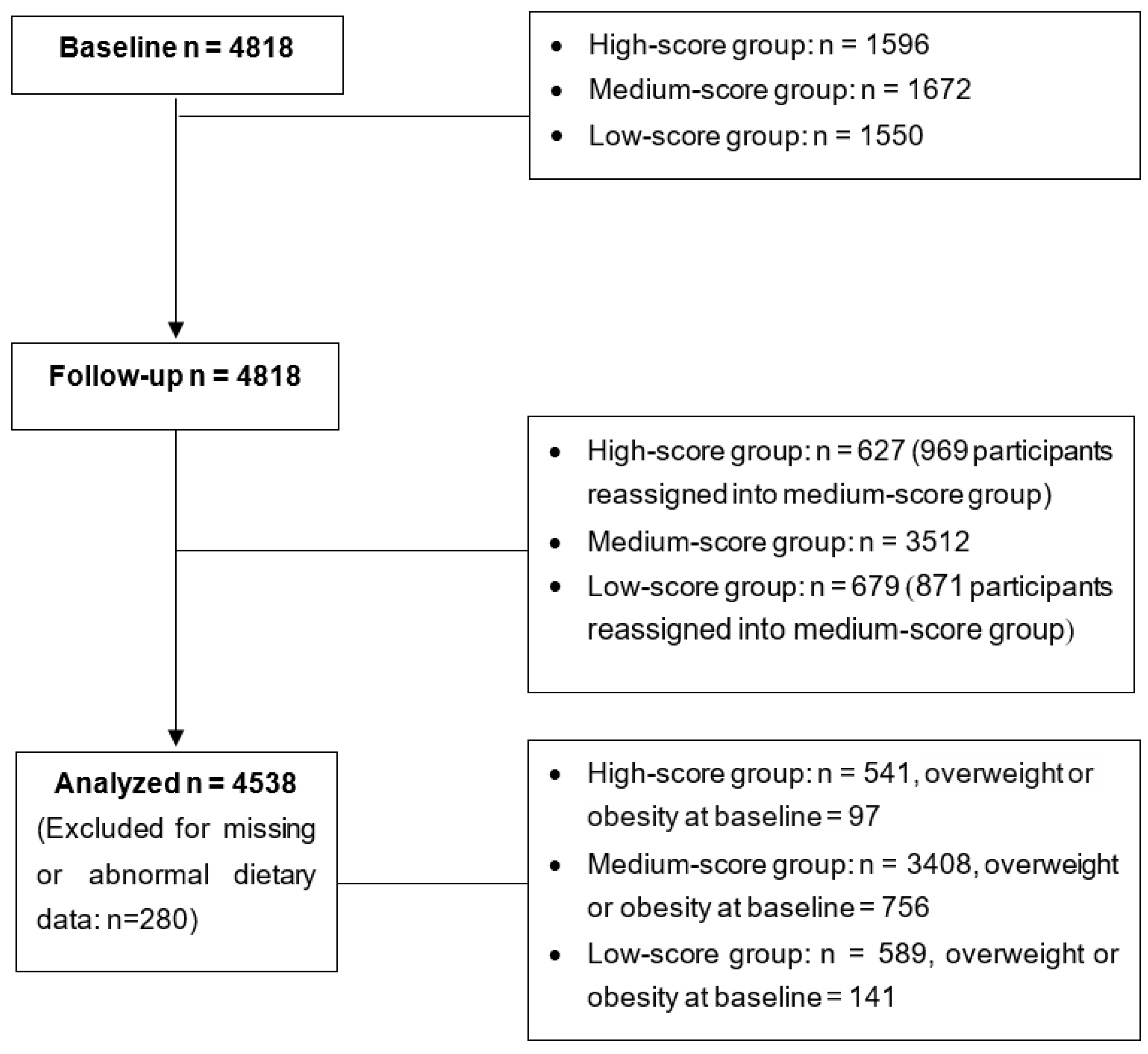
2. Materials and Methods
2.1. Study Design
2.2. Anthropometric Measurements
2.3. Sociodemographic Information
2.4. Dietary Diversity Measurements
2.5. Statistical Analysis
3. Results
3.1. General Characteristics
3.2. Effect of Dietary Diversity on Weight, BMI, WC and BF
3.3. Association between Dietary Diversity and Obesity
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Guh, D.P.; Zhang, W.; Bansback, N.; Amarsi, Z.; Birmingham, C.L.; Anis, A.H. The incidence of co-morbidities related to obesity and overweight: A systematic review and meta-analysis. BMC Public Health 2009, 9, 88. [Google Scholar] [CrossRef] [PubMed]
- Wilson, P.W.; D’Agostino, R.B.; Sullivan, L.; Parise, H.; Kannel, W.B. Overweight and obesity as determinants of cardiovascular risk: The Framingham experience. Arch. Intern. Med. 2002, 162, 1867–1872. [Google Scholar] [CrossRef] [PubMed]
- Finkelstein, E.A.; Trogdon, J.G.; Cohen, J.W.; Dietz, W. Annual medical spending attributable to obesity: Payer-and service-specific estimates. Health Aff. 2009, 28, 822–831. [Google Scholar] [CrossRef]
- Piernas, C.; Wang, D.T.; Du, S.F.; Zhang, B.; Wang, Z.H.; Su, C.; Popkin, B.M. The double burden of under- and overnutrition and nutrient adequacy among Chinese preschool and school-aged children in 2009-2011. Eur. J. Clin. Nutr. 2015, 69, 1323–1329. [Google Scholar] [CrossRef]
- Bureau of Disease Prevention and Control of National Health Commission of the People’s Republic of China. Chinese Residents’ Nutrition and Chronic Disease Report (2020), 1st ed.; People’s Medical Publishing House: Beijing, China, 2021. [Google Scholar]
- Ma, G. Report on Childhood Obesity in China, 1st ed.; People’s Medical Publishing House: Beijing, China, 2017. [Google Scholar]
- Pereira-Santos, M.; Costa, P.R.; Assis, A.M.; Santos, C.A.; Santos, D.B. Obesity and vitamin D deficiency: A systematic review and meta-analysis. Obes. Rev. 2015, 16, 341–349. [Google Scholar] [CrossRef] [PubMed]
- Jacobs, D.R., Jr.; Steffen, L.M. Nutrients, foods, and dietary patterns as exposures in research: A framework for food synergy. Am. J. Clin. Nutr. 2003, 78, 508S–513S. [Google Scholar] [CrossRef]
- Hu, F.B. Dietary pattern analysis: A new direction in nutritional epidemiology. Curr. Opin. Lipidol. 2002, 13, 3–9. [Google Scholar] [CrossRef]
- Azadbakht, L.; Mirmiran, P.; Azizi, F. Variety scores of food groups contribute to the specific nutrient adequacy in Tehranian men. Eur. J. Clin. Nutr. 2005, 59, 1233–1240. [Google Scholar] [CrossRef]
- Mirmiran, P.; Azadbakht, L.; Azizi, F. Dietary diversity within food groups: An indicator of specific nutrient adequacy in Tehranian women. J. Am. Coll. Nutr. 2006, 25, 354–361. [Google Scholar] [CrossRef]
- Drewnowski, A.; Henderson, S.A.; Driscoll, A.; Rolls, B.J. The Dietary Variety Score: Assessing diet quality in healthy young and older adults. J. Am. Diet. Assoc. 1997, 97, 266–271. [Google Scholar] [CrossRef]
- Salehi-Abargouei, A.; Akbari, F.; Bellissimo, N.; Azadbakht, L. Dietary diversity score and obesity: A systematic review and meta-analysis of observational studies. Eur. J. Clin. Nutr. 2016, 70, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Steyn, N.P.; Nel, J.H.; Nantel, G.; Kennedy, G.; Labadarios, D. Food variety and dietary diversity scores in children: Are they good indicators of dietary adequacy? Public Health Nutr. 2006, 9, 644–650. [Google Scholar] [CrossRef]
- Herforth, A.; Arimond, M.; Álvarez-Sánchez, C.; Coates, J.; Christianson, K.; Muehlhoff, E. A Global Review of Food-Based Dietary Guidelines. Adv. Nutr. 2019, 10, 590–605. [Google Scholar] [CrossRef]
- Chinese Nutrition Society. The Chinese Dietary Guidelines (2022), 1st ed.; People’s Medical Publishing House: Beijing, China, 2022. [Google Scholar]
- Fernandez, C.; Kasper, N.M.; Miller, A.L.; Lumeng, J.C.; Peterson, K.E. Association of Dietary Variety and Diversity with Body Mass Index in US Preschool Children. Pediatrics 2016, 137, e20152307. [Google Scholar] [CrossRef]
- Morris, M.A.; Hulme, C.; Clarke, G.P.; Edwards, K.L.; Cade, J.E. What is the cost of a healthy diet? Using diet data from the UK Women’s Cohort Study. J. Epidemiol. Community Health 2014, 68, 1043–1049. [Google Scholar] [CrossRef] [PubMed]
- Oldewage-Theron, W.H.; Egal, A.A. A cross-sectional baseline survey investigating the relationship between dietary diversity and cardiovascular risk factors in women from the Vaal Region, South Africa. J. Nurs. Educ. Pract. 2014, 4, 50–61. [Google Scholar] [CrossRef]
- Azadbakht, L.; Mirmiran, P.; Azizi, F. Dietary diversity score is favorably associated with the metabolic syndrome in Tehranian adults. Int. J. Obes. (Lond.) 2005, 29, 1361–1367. [Google Scholar] [CrossRef]
- Golpour-Hamedani, S.; Rafie, N.; Pourmasoumi, M.; Saneei, P.; Safavi, S.M. The association between dietary diversity score and general and abdominal obesity in Iranian children and adolescents. BMC Endocr. Disord. 2020, 20, 181. [Google Scholar] [CrossRef]
- Li, Y.P.; Hu, X.Q.; Zhang, Q.; Liu, A.L.; Fang, H.Y.; Hao, L.A.; Duan, Y.F.; Xu, H.Q.; Shang, X.W.; Ma, J.; et al. The nutrition-based comprehensive intervention study on childhood obesity in China (NISCOC): A randomised cluster controlled trial. BMC Public Health 2010, 10, 229. [Google Scholar] [CrossRef]
- WS/T 456-2014; Screening of Malnutrition in Children and Adolescents, 1st ed. China Standard Press: Beijing, China, 2014.
- Deurenberg, P.; van der Kooy, K.; Leenen, R.; Weststrate, J.A.; Seidell, J.C. Sex and age specific prediction formulas for estimating body composition from bioelectrical impedance: A cross-validation study. Int. J. Obes. 1991, 15, 17–25. [Google Scholar]
- Guidelines for Measuring Household and Individual Dietary Diversity. Available online: http://www.fao.org/3/i1983e/i1983e00.htm (accessed on 30 April 2022).
- US Department of Agriculture; Dietary Guidelines for Americans. Available online: https://www.nal.usda.gov/human-nutrition-and-food-safety/dietary-guidance. (accessed on 28 September 2022).
- Ruel, M.T. Operationalizing dietary diversity: A review of measurement issues and research priorities. J. Nutr. 2003, 133, 3911S–3926S. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- McCrory, M.A.; Fuss, P.J.; McCallum, J.E.; Yao, M.J.; Vinken, A.G.; Hays, N.P.; Roberts, S.B. Dietary variety within food groups: Association with energy intake and body fatness in men and women. Am. J. Clin. Nutr. 1999, 69, 440–447. [Google Scholar] [CrossRef] [PubMed]
- Otto, M.C.; Padhye, N.S.; Bertoni, A.G.; Jacobs, D.R., Jr.; Mozaffarian, D. Everything in Moderation-Dietary Diversity and Quality, Central Obesity and Risk of Diabetes. PLoS ONE 2015, 10, e0141341. [Google Scholar]
- Masset, G.; Scarborough, P.; Rayner, M.; Mishra, G.; Brunner, E.J. Can nutrient profiling help to identify foods which diet variety should be encouraged? Results from the Whitehall II cohort. Br. J. Nutr. 2015, 113, 1800–1809. [Google Scholar] [CrossRef]
- Zhao, W.Z.; Yu, K.; Tan, S.J.; Zheng, Y.D.; Zhao, A.; Wang, P.Y.; Zhang, Y.M. Dietary diversity scores: An indicator of micronutrient inadequacy instead of obesity for Chinese children. BMC Public Health 2017, 17, 440. [Google Scholar] [CrossRef]
- Karimbeiki, R.; Pourmasoumi, M.; Feizi, A.; Abbasi, B.; Hadi, A.; Rafie, N.; Safavi, S.M. Higher dietary diversity score is associated with obesity: A case-control study. Public Health 2018, 157, 127–134. [Google Scholar] [CrossRef]
- Kelly, T.; Yang, W.; Chen, C.S.; Reynolds, K.; He, J. Global burden of obesity in 2005 and projections to 2030. Int. J. Obes. 2008, 32, 1431–1437. [Google Scholar] [CrossRef]
- Azadbakht, L.; Mirmiran, P.; Esmaillzadeh, A.; Azizi, F. Dietary diversity score and cardiovascular risk factors in Tehranian adults. Public Health Nutr. 2006, 9, 728–736. [Google Scholar] [CrossRef]
- McCrory, M.A.; Burke, A.; Roberts, S.B. Dietary (sensory) variety and energy balance. Physiol. Behav. 2012, 107, 576–583. [Google Scholar] [CrossRef]
- Stubbs, R.J.; Johnstone, A.M.; Mazlan, N.; Mbaiwa, S.E.; Ferris, S. Effect of altering the variety of sensorially distinct foods, of the same macronutrient content, on food intake and body weight in men. Eur. J. Clin. Nutr. 2001, 55, 19–28. [Google Scholar] [CrossRef]
- Bezerra, I.N.; Sichieri, R. Household food diversity and nutritional status among adults in Brazil. Int. J. Behav. Nutr. Phys. Act. 2011, 8, 22. [Google Scholar] [CrossRef] [PubMed]
- Bertoia, M.L.; Mukamal, K.J.; Cahill, L.E.; Hou, T.; Ludwig, D.S.; Mozaffarian, D.; Willett, W.C.; Hu, F.B.; Rimm, E.B. Changes in Intake of Fruits and Vegetables and Weight Change in United States Men and Women Followed for Up to 24 Years: Analysis from Three Prospective Cohort Studies. PLoS Med. 2015, 12, e1001878. [Google Scholar] [CrossRef] [PubMed]
- Tao, C.; Zhao, Q.; Glauben, T.; Ren, Y. Does Dietary Diversity Reduce the Risk of Obesity? Empirical Evidence from Rural School Children in China. Int. J. Environ. Res. Public Health 2020, 17, 8122. [Google Scholar] [CrossRef] [PubMed]
- Azadbakht, L.; Esmaillzadeh, A. Dietary diversity score is related to obesity and abdominal adiposity among Iranian female youth. Public Health Nutr. 2011, 14, 62–69. [Google Scholar] [CrossRef] [PubMed]
- Kant, A.K.; Graubard, B.I. A comparison of three dietary pattern indexes for predicting biomarkers of diet and disease. J. Am. Coll. Nutr. 2005, 24, 294–303. [Google Scholar] [CrossRef]
- de Oliveira Otto, M.C.; Anderson, C.A.M.; Dearborn, J.L.; Ferranti, E.P.; Mozaffaiian, D.; Rao, G.; Wylie-Rosett, J.; Lichtenstein, A.H.; On behalf of the American Heart Association Behavioral Change for Improving Health Factors Committee of the Council on Lifestyle; Cardiometabolic Health and Council on Epidemiology and Prevention; et al. Dietary Diversity: Implications for Obesity Prevention in Adult Populations. Circulation 2018, 138, e160–e168. [Google Scholar] [CrossRef]
- Xu, H.; Ecker, O.; Zhang, Q.; Du, S.; Liu, A.; Li, Y.; Hu, X.; Li, T.; Guo, H.; Li, Y.; et al. The effect of comprehensive intervention for childhood obesity on dietary diversity among younger children: Evidence from a school-based randomized controlled trial in China. PLoS ONE 2020, 15, e0235951. [Google Scholar] [CrossRef]
| High-Score | Medium-Score | Low-Score | p | |
|---|---|---|---|---|
| Sex (N (%)) | ||||
| Boy | 209 (38.6) | 1610 (47.2) | 352 (59.8) | <0.001 |
| Girl | 332 (61.4) | 1798 (52.8) | 237 (40.2) | |
| Group (N (%)) | ||||
| Control | 229 (42.4) | 1455 (42.7) | 267 (45.3) | 0.494 |
| Intervention | 312 (57.6) | 1953 (57.3) | 322 (54.6) | |
| Education (N (%)) | ||||
| Low | 204 (39.2) | 1491 (46.4) | 295 (53.9) | <0.001 |
| High | 316 (60.8) | 1725 (53.6) | 252 (46.1) | |
| Income (N (%)) | ||||
| Low | 215 (41.3) | 1374 (42.7) | 298 (54.5) | <0.001 |
| High | 305 (58.6) | 1842 (57.3) | 249 (45.5) | |
| Age (year, Mean ± SD) | 8.9 ± 1.2 | 9.0 ± 1.2 | 8.9 ± 1.2 | 0.004 |
| DDS (Mean ± SD) | ||||
| Baseline (Mean ± SD) | 5.6 ± 0.6 | 4.4 ± 1.0 | 3.0 ± 0.6 | <0.001 |
| Follow-up (Mean ± SD) | 5.5 ± 0.5 | 4.2 ± 0.9 | 2.8 ± 0.5 | <0.001 |
| High-Score | Medium-Score | Low-Score | p | |
|---|---|---|---|---|
| Baseline | ||||
| Weight (kg, Mean ± SD) | 31.49 ± 8.27 | 32.49 ± 8.85 * | 32.79 ± 8.87 * | 0.032 |
| BMI (kg/m2, Mean ± SD) | 16.74 ± 2.84 | 17.08 ± 3.13 * | 17.45 ± 3.66 * | 0.001 |
| WC (cm, Mean ± SD) | 57.00 ± 8.24 | 58.17 ± 8.69 * | 58.96 ± 8.84 * | <0.001 |
| BF (%, Mean ± SD) | 27.73 ± 6.38 | 27.45 ± 6.66 | 27.02 ± 6.82 | 0.197 |
| Follow-up (changes) | ||||
| Weight (kg, Mean ± SD) | 4.06 ± 3.12 | 4.31 ± 3.78 | 4.62 ± 4.92 * | 0.066 |
| BMI (kg/m2, Mean ± SD) | 0.51 ± 1.34 | 0.61 ± 1.69 | 0.76 ± 2.66 * | 0.079 |
| WC (cm, Mean ± SD) | 3.12 ± 3.23 | 3.14 ± 3.54 | 3.13 ± 4.08 | 0.991 |
| BF (%, Mean ± SD) | 1.13 ± 3.23 | 1.35 ± 3.65 | 1.99 ± 3.88 * | 0.001 |
| High-Score | Medium-Score | Low-Score | p | |
|---|---|---|---|---|
| Prevalence | ||||
| Sample size | 541 | 3408 | 589 | |
| Overweight | 40 (7.39) | 404 (11.85) | 75 (12.73) | 0.005 |
| Obese | 57 (10.54) | 352 (10.38) | 66 (11.21) | 0.812 |
| Overweight and obese | 97 (17.93) | 756 (22.23) | 141 (23.94) | 0.037 |
| Incidence rate | ||||
| Sample size without overweight or obesity at baseline | 444 | 2652 | 448 | |
| Overweight | 20 (4.50) | 161 (6.07) | 39 (8.71) | 0.028 |
| Obese | 5 (1.13) | 28 (1.06) | 14 (3.13) | 0.001 |
| Overweight and obese | 25 (5.63) | 189 (7.13) | 53 (11.84) | <0.001 |
| High-Score | Medium-Score | Low-Score | |
|---|---|---|---|
| ORs | |||
| Model 1 | |||
| Overweight | 1.00 | 1.68 (1.20, 2.36) | 1.83 (1.22, 2.74) |
| Obese | 1.00 | 0.98 (0.73, 1.32) | 1.07 (0.74, 1.56) |
| Overweight and obese | 1.00 | 1.31 (1.03, 1.65) | 1.44 (1.08, 1.93) |
| Model 2 | |||
| Overweight | 1.00 | 1.63 (1.16, 2.29) | 1.68 (1.12, 2.52) |
| Obese | 1.00 | 0.94 (0.7, 1.26) | 0.97 (0.66, 1.41) |
| Overweight and obese | 1.00 | 1.25 (0.99, 1.58) | 1.30 (0.97, 1.74) |
| Model 3 | |||
| Overweight | 1.00 | 1.73 (1.23, 2.44) | 1.91 (1.27, 2.89) |
| Obese | 1.00 | 0.99 (0.73, 1.33) | 1.09 (0.75, 1.6) |
| Overweight and obese | 1.00 | 1.33 (1.05, 1.69) | 1.50 (1.11, 2.01) |
| Model 4 | |||
| Overweight | 1.00 | 1.67 (1.19, 2.35) | 1.84 (1.22, 2.76) |
| Obese | 1.00 | 0.98 (0.72, 1.32) | 1.08 (0.74, 1.58) |
| Overweight and obese | 1.00 | 1.30 (1.03, 1.65) | 1.46 (1.08, 1.96) |
| Model 5 | |||
| Overweight | 1.00 | 1.66 (1.17, 2.34) | 1.76 (1.17, 2.65) |
| Obese | 1.00 | 0.94 (0.70, 1.28) | 0.99 (0.67, 1.46) |
| Overweight and obese | 1.00 | 1.27 (1.01, 1.61) | 1.35 (1.01, 1.81) |
| RRs | |||
| Model 6 | |||
| Overweight | 1.00 | 1.35 (0.86, 2.12) | 1.93 (1.15, 3.26) |
| Obese | 1.00 | 0.94 (0.36, 2.42) | 2.78 (1.01, 7.64) |
| Overweight and obese | 1.00 | 1.27 (0.84, 1.90) | 2.10 (1.33, 3.32) |
| Model 7 | 1.00 | ||
| Overweight | 1.00 | 1.34 (0.85, 2.11) | 1.94 (1.15, 3.27) |
| Obese | 1.00 | 0.94 (0.36, 2.42) | 2.82 (1.03, 7.77) |
| Overweight and obese | 1.00 | 1.26 (0.84, 1.89) | 2.12 (1.34, 3.34) |
| Model 8 | 1.00 | ||
| Overweight | 1.00 | 1.30 (0.83, 2.06) | 1.74 (1.01, 3.00) |
| Obese | 1.00 | 0.89 (0.35, 2.32) | 2.42 (0.81, 7.24) |
| Overweight and obese | 1.00 | 1.22 (0.82, 1.83) | 1.88 (1.16, 3.03) |
| Model 9 | 1.00 | ||
| Overweight | 1.00 | 1.35 (0.86, 2.13) | 1.75 (1.04, 2.95) |
| Obese | 1.00 | 0.97 (0.37, 2.51) | 2.94 (1.00, 8.69) |
| Overweight and obese | 1.00 | 1.28 (0.85, 1.91) | 1.97 (1.24, 3.12) |
| Model 10 | 1.00 | ||
| Overweight | 1.00 | 1.35 (0.86, 2.12) | 1.83 (1.10, 3.07) |
| Obese | 1.00 | 0.93 (0.36, 2.40) | 2.88 (1.00, 8.60) |
| Overweight and obese | 1.00 | 1.26 (0.84, 1.89) | 2.02 (1.28, 3.20) |
| Model 11 | 1.00 | ||
| Overweight | 1.00 | 1.33 (0.82, 2.14) | 1.81 (1.03, 3.19) |
| Obese | 1.00 | 0.91 (0.35,2.39) | 2.31 (0.81,6.59) |
| Overweight and obese | 1.00 | 1.25 (0.81, 1.92) | 1.98 (1.20, 3.28) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Xu, H.; Du, S.; Liu, A.; Zhang, Q.; Ma, G. Low Dietary Diversity for Recommended Food Groups Increases the Risk of Obesity among Children: Evidence from a Chinese Longitudinal Study. Nutrients 2022, 14, 4068. https://doi.org/10.3390/nu14194068
Xu H, Du S, Liu A, Zhang Q, Ma G. Low Dietary Diversity for Recommended Food Groups Increases the Risk of Obesity among Children: Evidence from a Chinese Longitudinal Study. Nutrients. 2022; 14(19):4068. https://doi.org/10.3390/nu14194068
Chicago/Turabian StyleXu, Haiquan, Songming Du, Ailing Liu, Qian Zhang, and Guansheng Ma. 2022. "Low Dietary Diversity for Recommended Food Groups Increases the Risk of Obesity among Children: Evidence from a Chinese Longitudinal Study" Nutrients 14, no. 19: 4068. https://doi.org/10.3390/nu14194068
APA StyleXu, H., Du, S., Liu, A., Zhang, Q., & Ma, G. (2022). Low Dietary Diversity for Recommended Food Groups Increases the Risk of Obesity among Children: Evidence from a Chinese Longitudinal Study. Nutrients, 14(19), 4068. https://doi.org/10.3390/nu14194068








