Maternal Vitamin B12 Deficiency Detected by Newborn Screening—Evaluation of Causes and Characteristics
Abstract
:1. Introduction
1.1. Uptake and Function of Vitamin B12
1.2. Causes and Symptoms of Vitamin B12 Deficiency
1.3. Early Detection through Newborn Screening for Vitamin B12 Deficiency
2. Material and Methods
2.1. Study Population and Study Design
2.2. Data Collection
2.3. Study Objective
2.4. Statistical Analysis
3. Results
3.1. Maternal and Child Characteristics
3.2. Maternal Diagnoses
3.3. Maternal Vitamin B12 Status
3.4. Blood Counts of Mothers and Children
3.5. Neonatal Vitamin B12 Status
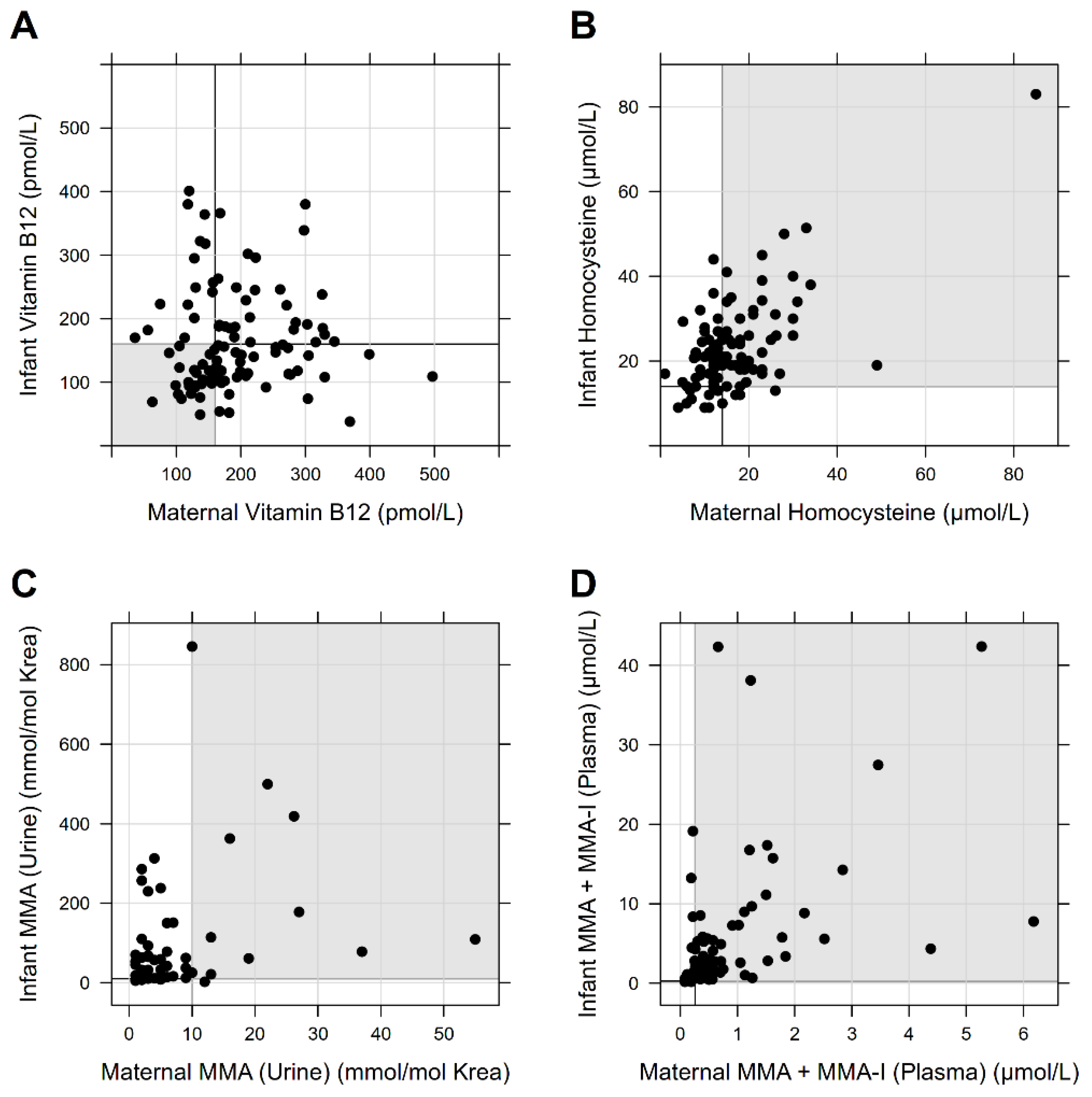
3.6. Effect of Maternal Vitamin B12 Status on Infant Metabolism
3.7. Effect of Neonatal Nutrition on Newborns’ Vitamin B12 Status
3.8. Gestational Age, Birth Weight, and Congenital Heart Defects
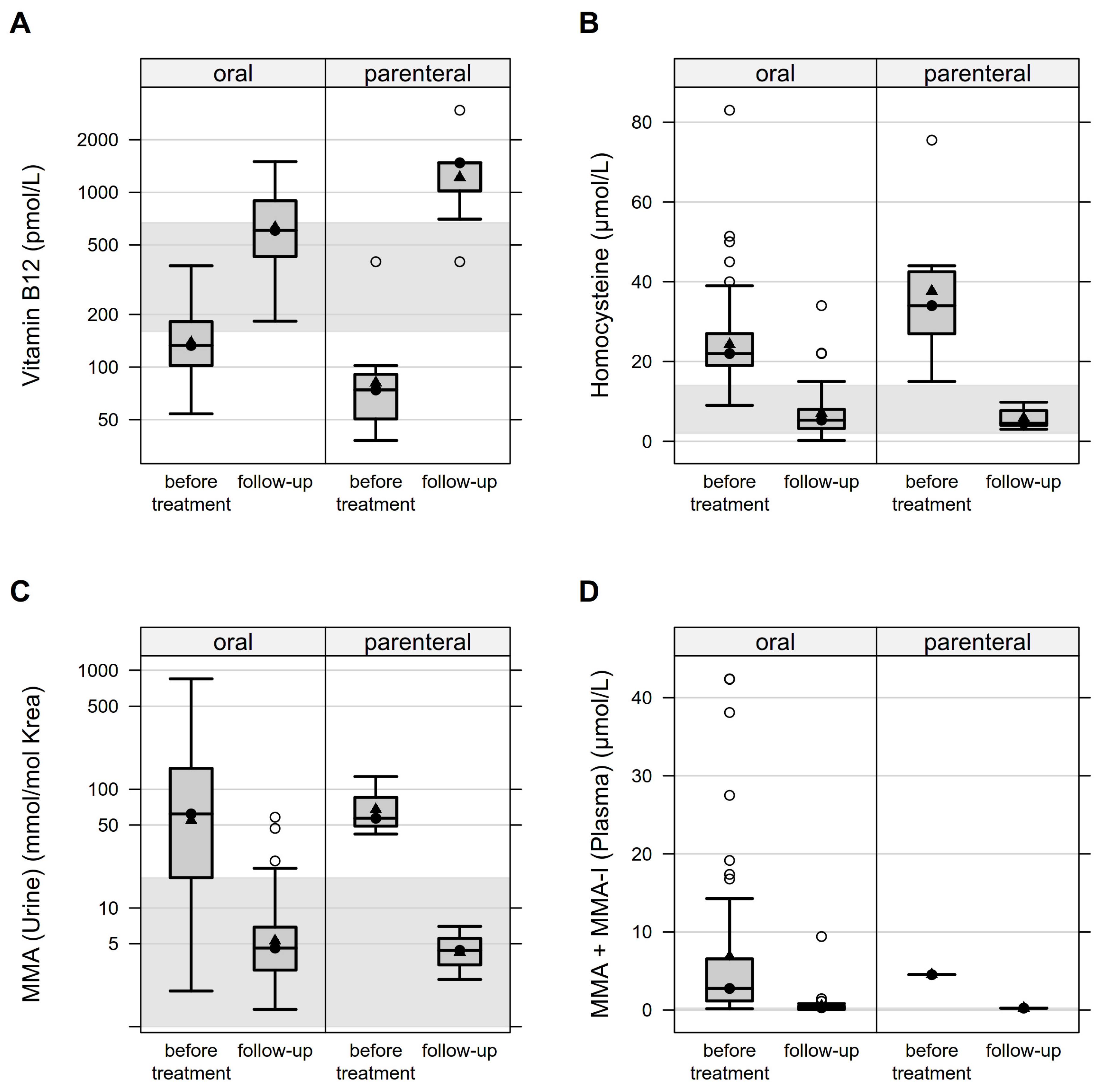
3.9. Infants’ Response to Therapy
4. Discussion
4.1. Maternal Diet and Causes of Vitamin B12 Deficiency
4.2. Maternal and Infants’ Vitamin B12 Status
4.3. Gestational Age, Birth Weight, and Congenital Heart Defects
4.4. Infantiles’ Response to Therapy
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- Lyon, P.; Strippoli, V.; Fang, B.; Cimmino, L. B vitamins and one-carbon metabolism: Implications in human health and disease. Nutrients 2020, 12, 2867. [Google Scholar] [CrossRef] [PubMed]
- Stabler, S.P. Vitamin B12 deficiency. N. Engl. J. Med. 2013, 368, 149–160. [Google Scholar] [CrossRef]
- Nielsen, M.J.; Rasmussen, M.R.; Andersen, C.B.F.; Nexø, E.; Moestrup, S.K. Vitamin B12 transport from food to the body’s cells—A sophisticated, multistep pathway. Nat. Rev. Gastroenterol. Hepatol. 2012, 9, 345–354. [Google Scholar] [CrossRef]
- Stabler, S.P.; Allen, R.H. Vitamin B12 deficiency as a worldwide problem. Annu. Rev. Nutr. 2004, 24, 299–326. [Google Scholar] [CrossRef] [PubMed]
- Green, R.; Allen, L.H.; Bjørke-Monsen, A.-L.; Brito, A.; Guéant, J.-L.; Miller, J.W.; Molloy, A.M.; Nexo, E.; Stabler, S.; Toh, B.-H.; et al. Vitamin B 12 deficiency. Nat. Rev. Dis. Primers 2017, 3, 17040. [Google Scholar] [CrossRef]
- McLean, E.; de Benoist, B.; Allen, L.H. Review of the magnitude of folate and vitamin B12 deficiencies worldwide. Food Nutr. Bull. 2008, 29 (Suppl. 2), S38–S51. [Google Scholar] [CrossRef]
- Allen, L.H. How common is vitamin B-12 deficiency? Am. J. Clin. Nutr. 2009, 89, 693S–696S. [Google Scholar] [CrossRef]
- Sukumar, N.; Adaikalakoteswari, A.; Venkataraman, H.; Maheswaran, H.; Saravanan, P. Vitamin B12 status in women of childbearing age in the UK and its relationship with national nutrient intake guidelines: Results from two National Diet and Nutrition Surveys. BMJ Open 2016, 6, e011247. [Google Scholar] [CrossRef] [PubMed]
- Obeid, R.; Murphy, M.; Solé-Navais, P.; Yajnik, C. Cobalamin status from pregnancy to early childhood: Lessons from global experience. Adv. Nutr. 2017, 8, 971–979. [Google Scholar] [CrossRef]
- Murphy, M.M.; Molloy, A.M.; Ueland, P.M.; Fernandez-Ballart, J.D.; Schneede, J.; Arija, V.; Scott, J.M. Longitudinal study of the effect of pregnancy on maternal and fetal cobalamin status in healthy women and their offspring. J. Nutr. 2007, 137, 1863–1867. [Google Scholar] [CrossRef] [Green Version]
- Gramer, G.; Hoffmann, G.F. Vitamin B12 deficiency in newborns and their mothers. Curr. Med. Sci. 2020, 40, 801–809. [Google Scholar] [CrossRef]
- Scolamiero, E.; Villani, G.R.D.; Ingenito, L.; Pecce, R.; Albano, L.; Caterino, M.; di Girolamo, M.G.; Di Stefano, C.; Franzese, I.; Gallo, G.; et al. Maternal vitamin B12 deficiency detected in expanded newborn screening. Clin. Biochem. 2014, 47, 312–317. [Google Scholar] [CrossRef] [PubMed]
- Sukumar, N.; Rafnsson, S.B.; Kandala, N.-B.; Bhopal, R.; Yajnik, C.S.; Saravanan, P. Prevalence of vitamin B-12 insufficiency during pregnancy and its effect on offspring birth weight: A systematic review and meta-analysis. Am. J. Clin. Nutr. 2016, 103, 1232–1251. [Google Scholar] [CrossRef]
- Schroder, T.H.; Sinclair, G.; Mattman, A.; Jung, B.; Barr, S.I.; Vallance, H.D.; Lamers, Y. Pregnant women of South Asian ethnicity in Canada have substantially lower vitamin B12 status compared with pregnant women of European ethnicity. Br. J. Nutr. 2017, 118, 454–462. [Google Scholar] [CrossRef]
- Finkelstein, J.L.; Layden, A.J.; Stover, P.J. Vitamin B-12 and perinatal health. Adv. Nutr. 2015, 6, 552–563. [Google Scholar] [CrossRef] [PubMed]
- Varsi, K.; Ueland, P.M.; Torsvik, I.K.; Bjørke-Monsen, A.-L. Maternal serum cobalamin at 18 weeks of pregnancy predicts infant cobalamin status at 6 months—A prospective, observational study. J. Nutr. 2018, 148, 738–745. [Google Scholar] [CrossRef] [PubMed]
- Graham, S.M.; Arvela, O.M.; Wise, G.A. Long-term neurologic consequences of nutritional vitamin B12 deficiency in infants. J. Pediatrics 1992, 121, 710–714. [Google Scholar] [CrossRef]
- Jain, R.; Singh, A.; Mittal, M.; Talukdar, B. Vitamin B12 deficiency in children: A treatable cause of neurodevelopmental delay. J. Child Neurol. 2015, 30, 641–643. [Google Scholar] [CrossRef]
- Singh, G.; Le, D.; Schnabl, K.; Leaker, M.T.; Steele, M.; Sparkes, R.L. Vitamin B12 deficiency in infancy: The case for screening. Pediatric Blood Cancer 2016, 63, 740–742. [Google Scholar] [CrossRef]
- Röschinger, W.; Sonnenschein, S.; Schuhmann, E.; Nennstiel-Ratzel, U.; Roscher, A.; Olgemöller, B. Neue zielerkrankungen im neugeborenenscreening. Mon. Kinderheilkd. 2015, 163, 142–149. [Google Scholar] [CrossRef]
- Mütze, U.; Walter, M.; Keller, M.; Gramer, G.; Garbade, S.F.; Gleich, F.; Haas, D.; Posset, R.; Grünert, S.C.; Hennermann, J.B.; et al. Health outcomes of infants with Vitamin B12 deficiency identified by newborn screening and early treated. J. Pediatrics 2021, 235, 42–48. [Google Scholar] [CrossRef] [PubMed]
- Gramer, G.; Fang-Hoffmann, J.; Feyh, P.; Klinke, G.; Monostori, P.; Mütze, U.; Posset, R.; Weiss, K.H.; Hoffmann, G.F.; Okun, J.G.; et al. Newborn screening for Vitamin B(12) deficiency in Germany—Strategies, results, and public health implications. J. Pediatr. 2020, 216, 165–172.e4. [Google Scholar] [CrossRef] [PubMed]
- Reinson, K.; Künnapas, K.; Kriisa, A.; Vals, M.-A.; Muru, K.; Õunap, K. High incidence of low vitamin B12 levels in Estonian newborns. Mol. Genet. Metab. Rep. 2018, 15, 1–5. [Google Scholar] [CrossRef] [PubMed]
- Sarafoglou, K.; Rodgers, J.; Hietala, A.; Matern, D.; Bentler, K. Expanded newborn screening for detection of vitamin B12 deficiency. JAMA 2011, 305, 1198–1200. [Google Scholar] [CrossRef] [PubMed]
- Richtlinie des Gemeinsamen Bundesausschusses über die Früherkennung von Krankheiten bei Kindern (Kinder-Richtlinie); Gemeinsamer Bundesausschuss: Berlin/Heidelberg, Germany, 2022; Volume 18.
- Monostori, P.; Klinke, G.; Richter, S.; Baráth, A.; Fingerhut, R.; Baumgartner, M.R.; Kölker, S.; Hoffmann, G.F.; Gramer, G.; Okun, J.G. Simultaneous determination of 3-hydroxypropionic acid, methylmalonic acid and methylcitric acid in dried blood spots: Second-tier LC-MS/MS assay for newborn screening of propionic acidemia, methylmalonic acidemias and combined remethylation disorders. PLoS ONE 2017, 12, e0184897. [Google Scholar] [CrossRef] [PubMed]
- Gan-Schreier, H.; Kebbewar, M.; Fang-Hoffmann, J.; Wilrich, J.; Abdoh, G.; Ben-Omran, T.; Shahbek, N.; Bener, A.; Al Rifai, H.; Al Khal, A.L.; et al. Newborn population screening for classic homocystinuria by determination of total homocysteine from guthrie cards. J. Pediatr. 2010, 156, 427–432. [Google Scholar] [CrossRef] [PubMed]
- Hannibal, L.; Lysne, V.; Bjørke-Monsen, A.-L.; Behringer, S.; Grünert, S.C.; Spiekerkoetter, U.; Jacobsen, D.W.; Blom, H.J. Biomarkers and algorithms for the diagnosis of vitamin B12 deficiency. Front. Mol. Biosci. 2016, 3, 27. [Google Scholar] [CrossRef]
- Bundesamt, S. Bevölkerung Migration und Integration 2022. Available online: https://www.destatis.de/DE/Themen/Gesellschaft-Umwelt/Bevoelkerung/Migration-Integration/_inhalt.html (accessed on 20 February 2022).
- Honzik, T.; Adamovicova, M.; Smolka, V.; Magner, M.; Hruba, E.; Zeman, J. Clinical presentation and metabolic consequences in 40 breastfed infants with nutritional vitamin B12 deficiency—What have we learned? Eur. J. Paediatr. Neurol. 2010, 14, 488–495. [Google Scholar] [CrossRef]
- Hinton, C.F.; Ojodu, J.A.; Fernhoff, P.M.; Rasmussen, S.A.; Scanlon, K.S.; Hannon, W.H. Maternal and neonatal vitamin B12 deficiency detected through expanded newborn screening—United States, 2003–2007. J. Pediatr. 2010, 157, 162–163. [Google Scholar] [CrossRef]
- Koletzko, B.; Cremer, M.; Flothkötter, M.; Graf, C.; Hauner, H.; Hellmers, C.; Kersting, M.; Krawinkel, M.; Przyrembel, H.; Röbl-Mathieu, M.; et al. Diet and lifestyle before and during pregnancy–practical recommendations of the Germany-wide healthy start–young family network. Geburtshilfe Frauenheilkd. 2018, 78, 1262–1282. [Google Scholar] [CrossRef] [Green Version]
- Schaefer, H.; Bellach, B. Der bundes-gesundheits-survey 1998—Erfahrungen, ergebnisse, perspektiven. Gesundheitswesen 1999, 61, S55–S56. [Google Scholar]
- Masih, S.P.; Plumptre, L.; Ly, A.; Berger, H.; Lausman, A.Y.; Croxford, R.; Kim, Y.-I.; O’Connor, D.L. Pregnant Canadian women achieve recommended intakes of one-carbon nutrients through prenatal supplementation but the supplement composition, including choline, requires reconsideration. J. Nutr. 2015, 145, 1824–1834. [Google Scholar] [CrossRef] [PubMed]
- Karabiber, H.; Sonmezgoz, E.; Ozerol, E.; Yakinci, C.; Otlu, B.; Yologlu, S. Effects of valproate and carbamazepine on serum levels of homocysteine, vitamin B12, and folic acid. Brain Dev. 2003, 25, 113–115. [Google Scholar] [CrossRef]
- Karaoglu, L.; Pehlivan, E.; Egri, M.; Deprem, C.; Gunes, G.; Genc, M.F.; Temel, I. The prevalence of nutritional anemia in pregnancy in an east Anatolian province, Turkey. BMC Public Health 2010, 10, 329. [Google Scholar] [CrossRef] [PubMed]
- Hartong, S.; Steegers, E.; Visser, W. Hemolysis, elevated liver enzymes and low platelets during pregnancy due to vitamin B12 and folate deficiencies. Eur. J. Obstet. Gynecol. Reprod. Biol. 2007, 131, 241–242. [Google Scholar] [CrossRef]
- Solé-Navais, P.; Cavallé-Busquets, P.; Fernandez-Ballart, J.D.; Murphy, M.M. Early pregnancy B vitamin status, one carbon metabolism, pregnancy outcome and child development. Biochimie 2016, 126, 91–96. [Google Scholar] [CrossRef]
- Eidgenossenschaft, S. Gesundheit von Müttern und Kindern mit Migrationshintergrund. 2015. Available online: https://www.bfs.admin.ch/bfs/portal/de/index/news/00/06.html (accessed on 28 November 2014).
- Centers for Disease Control and Prevention. Neurologic impairment in children associated with maternal dietary deficiency of cobalamin—Georgia, 2001. MMWR Morb. Mortal. Wkly. Rep. 2003, 52, 61–64. [Google Scholar]
- Mishra, J.; Tomar, A.; Puri, M.; Jain, A.; Saraswathy, K. Trends of folate, vitamin B12, and homocysteine levels in different trimesters of pregnancy and pregnancy outcomes. Am. J. Hum. Biol. 2020, 32, e23388. [Google Scholar] [CrossRef]
- Rogne, T.; Tielemans, M.J.; Chong, M.F.-F.; Yajnik, C.S.; Krishnaveni, G.V.; Poston, L.; Jaddoe, V.W.V.; Steegers, E.A.P.; Joshi, S.; Chong, Y.-S.; et al. Associations of maternal vitamin B12 concentration in pregnancy with the risks of preterm birth and low birth weight: A systematic review and meta-analysis of individual participant data. Am. J. Epidemiol. 2017, 185, 212–223. [Google Scholar] [CrossRef]
- Özturk, Ö.; Keskin, L.; Tafl, E.E.; Akgün, N.; Avflar, F. The effect of vitamin B12 level on fetal birth weight. Perinat. J. 2015, 23, 73–78. [Google Scholar] [CrossRef]
- Hogeveen, M.; Blom, H.J.; van der Heijden, E.H.; Semmekrot, B.A.; Sporken, J.M.; Ueland, P.M.; Heijer, M.D. Maternal homocysteine and related B vitamins as risk factors for low birthweight. Am. J. Obstet. Gynecol. 2010, 202, 572.e1–572.e6. [Google Scholar] [CrossRef] [PubMed]
- Tan, A.; Sinclair, G.; Mattman, A.; Vallance, H.D.; Lamers, Y. Maternal vitamin B12 status in early pregnancy and its association with birth outcomes in Canadian mother–newborn Dyads. Br. J. Nutr. 2021, 126, 1823–1831. [Google Scholar] [CrossRef]
- Verkleij-Hagoort, A.C.; van Driel, L.M.; Lindemans, J.; Isaacs, A.; Steegers, E.A.; Helbing, W.A.; Uitterlinden, A.G.; Steegers-Theunissen, R.P. Genetic and lifestyle factors related to the periconception vitamin B12 status and congenital heart defects: A Dutch case-control study. Mol. Genet. Metab. 2008, 94, 112–119. [Google Scholar] [CrossRef]
- Van Der Linde, D.; Konings, E.E.; Slager, M.A.; Witsenburg, M.; Helbing, W.A.; Takkenberg, J.J. Birth prevalence of congenital heart disease worldwide: A systematic review and meta-analysis. J. Am. Coll. Cardiol. 2011, 58, 2241–2247. [Google Scholar] [CrossRef]
- Pfitzer, C.; Helm, P.C.; Ferentzi, H.; Rosenthal, L.-M.; Bauer, U.M.M.; Berger, F.; Schmitt, K.R.L. Changing prevalence of severe congenital heart disease: Results from the National Register for Congenital Heart Defects in Germany. Congenit. Heart Dis. 2017, 12, 787–793. [Google Scholar] [CrossRef] [PubMed]
- Bahadir, A.; Reis, P.G.; Erduran, E. Oral vitamin B 12 treatment is effective for children with nutritional vitamin B 12 deficiency. J. Paediatr. Child Health 2014, 50, 721–725. [Google Scholar] [CrossRef] [PubMed]
| Normal Range | ||
|---|---|---|
| Vitamin B12 (S) (Valid data: n = 107; missing data n = 14) | 160–679 pmol/L | |
| Mean ± SD | 189 ± 79 | |
| Median (IQR) | 168 (137; 223) | |
| Minimum/maximum | 36/497 | |
| Folic Acid (S) (Valid data: n = 97; missing data n = 24) | 4.5–21 nmol/L | |
| Mean ± SD | 18.1 ± 12.7 | |
| Median (IQR) | 13.0 (8.0; 23.5) | |
| Minimum/maximum | 5.0/45.0 | |
| Total Hcy (P) (Valid data: n = 102; missing data: n = 19) | 2–14 µmol/L | |
| Mean ± SD | 16.6 ± 10.2 | |
| Median (IQR) | 14.0 (11.0; 20.2) | |
| Minimum/maximum | 1.0/85.0 | |
| MMA + MMA-I (P) ** (Valid data: n = 87; missing data: N =34) | <0.26 µmol/L | |
| Mean ± SD | 0.85 ± 1.07 | |
| Median (IQR) | 0.45 (0.25; 1.05) | |
| Minimum/maximum | 0.08/6.18 | |
| MMA (U) (Valid data: n = 63; missing data: n = 58) | <10 mmol/mol Creatinine | |
| Mean ± SD | 7.4 ± 9.5 | |
| Median (IQR) | 4.0 (2.0; 9.0) | |
| Minimum/maximum | 1.0/55.0 | |
| MMA-I (U) ** (Valid data: n = 83; missing data: n = 38) | <18 mmol/mol Creatinine | |
| Mean ± SD | 4.9 ± 9.8 | |
| Median (IQR) | 2.1 (1.5; 4.7) | |
| Minimum/maximum | 0.4/79.8 | |
| Maternal hemoglobin (Valid data: n = 31; missing data: n = 90) | |
| Normal | 20 (64.5%) |
| Anemia | 11 (35.5%) |
| Maternal MCV (Valid data: n = 31; missing data: n = 90) | |
| Normocytosis | 22 (71.0%) |
| Microcytosis | 8 (25.8%) |
| Macrocytosis | 1 (3.2%) |
| Newborn hemoglobin (Valid data: n = 45; missing data: n = 76) | |
| Normal | 35 (77.8%) |
| Anemia | 7 (15.5%) |
| Polyglobuly | 3 (6.7%) |
| Newborn MCV (Valid data: n = 42; missing data: n = 79) | |
| Normocytosis | 37 (88.1%) |
| Microcytosis | 2 (4.8%) |
| Macrocytosis | 3 (7.1%) |
| Confirmation Data | Normal Range | |
|---|---|---|
| Vitamin B12 (S) (Valid data: n = 118; missing data n = 3) | 160–670 pmol/L | |
| Mean ± SD | 161 ± 79 | |
| Median (IQR) | 144 (102; 191) | |
| Minimum/maximum | 38/401 | |
| Folic Acid (S) (Valid data: n = 108; missing data n = 13) | 4.5–21 nmol/L | |
| Mean ± SD | 34.6 ± 9.3 | |
| Median (IQR) | 36.0 (27.0; 45.0) | |
| Minimum/maximum | 14.0/46.0 | |
| Hcy (P) (Valid data: n = 117; missing data: n = 4) | 2–14 µmol/L | |
| Mean ± SD | 23.3 ± 11.3 | |
| Median (IQR) | 21.0 (17.0; 27.0) | |
| Minimum/maximum | 9.0/83.0 | |
| MMA + MMA-I (P) (Valid data: n = 85; missing data n = 36) | <0.26 µmol/L | |
| Mean ± SD | 5.64 ± 8.47 | |
| Median (IQR) | 2.60 (0.91; 5.79) | |
| Minimum/maximum | 0.17/42.37 | |
| MMA (U) (Valid data: n = 86; missing data: n = 35) | <18 mmol/mol Creatinine | |
| Mean ± SD | 105 ± 145 | |
| Median (IQR) | 50 (16; 133) | |
| Minimum/maximum | 2/846 | |
| MMA-I (U) (Valid data: n = 94; missing data: n = 27) | <10 mmol/mol Creatinine | |
| Mean ± SD | 99.9 ± 190.0 | |
| Median (IQR) | 38.5 (14.4; 100.4) | |
| Minimum/maximum | 2.3/1368.8 | |
| Screening Data | Normal Range | |
| Hcy (DBS 1) (n = 116) | <12 (P99.2) µmol/L | |
| Mean ± SD | 17.1 ± 7.3 | |
| Median (IQR) | 15.9 (12.9; 20.4) | |
| Minimum/maximum | 2.9/50.5 | |
| MMA (DBS 1) (n = 80) | 2.14 (P99.9), 2.35 (P99.9) *** µmol/L | |
| Mean ± SD | 5.55 ± 10.47 | |
| Median (IQR) | 2.30 (1.69; 6.15) | |
| Minimum/maximum | 0.06/85.71 | |
| MCA (DBS 1) (n = 90) | 0.08 (P99.9)/0.34 (P99.9) *** µmol/L | |
| Mean ± SD | 0.35 ± 0.58 | |
| Median (IQR) | 0.18 (0.10; 0.37) | |
| Minimum/maximum | 0/4.62 | |
| Hcy (DBS 2) (n = 107) | <12 (P99.2) µmol/L | |
| Mean ± SD | 15.6 ± 6.9 | |
| Median (IQR) | 14.7 (10.0; 20.4) | |
| Minimum/maximum | 4.9/46.0 | |
| MMA (DBS 2) (n = 94) | 2.14 (P99.9), 2.35 (P99.9) *** µmol/L | |
| Mean ± SD | 5.10 ± 6.28 | |
| Median (IQR) | 2,79 (1.94; 5.89) | |
| Minimum/maximum | 0/34.40 | |
| MCA (DBS 2) (n = 102) | 0.08 (P99.9)/0.34 (P99.9) *** µmol/L | |
| Mean ± SD | 0.37 ± 0.46 | |
| Median (IQR) | 0.26 (0.16; 0.42) | |
| Minimum/maximum | 0/2.84 | |
| Maternal Vitamin B12 Status | Infant Vitamin B12 Status | p-Value |
|---|---|---|
| Confirmation Data | ||
| Folic acid | Folic acid | p < 0.001 |
| Increase in maternal folic acid concentration by one unit indicates a 0.2 increase in infant folic acid concentration. | ||
| Homocysteine | Homocysteine | p < 0.001 |
| Increase in maternal Hcy concentration by one unit indicates a 0.7 increase in infant Hcy concentration. | ||
| Homocysteine | MMA (U) | p = 0.002 |
| Increase in maternal Hcy concentration by one unit indicates a 5.1 increase in infant MMA (U) concentration. | ||
| Homocysteine | MMA-I (U) | p < 0.001 |
| Increase in maternal Hcy concentration by one unit indicates a 9.8 increase in infant MMA-I (U) concentration. | ||
| Homocysteine | MMA or MMA-I (P) | p = 0.018 |
| Increase in maternal Hcy concentration by one unit indicates a 0.25 increase in infant MMA or MMA-I in plasma concentration. | ||
| MMA + MMA-I (P) | MMA or MMA-I (P) | p < 0.001 |
| Increase in maternal MMA and MMA-I in plasma concentration by one unit indicates a 3.66 increase in infant MMA and MMA-I in plasma concentration. | ||
| NBS data (DBS 1) | ||
| Homocysteine | Homocysteine | p < 0.001 |
| Increase in maternal Hcy concentration by one unit indicates a 0.2 increase in infant Hcy concentration. | ||
| Vitamin B12 | Homocysteine | p = 0.009 |
| Increase in maternal vitamin B12 concentration by one unit indicates a 0.02 decrease in infant Hcy concentration. | ||
| MMA + MMA-I (P) | Homocysteine | p < 0.001 |
| Increase in maternal MMA and MMA-I in plasma concentration by one unit indicates a 2.78 increase in infant Hcy concentration. | ||
| MMA (U) | Homocysteine | p = 0.025 |
| Increase in maternal MMA concentration in urine by one unit indicates a 0.31 increase in infant Hcy concentration. | ||
| Homocysteine | MMA | p < 0.001 |
| Increase in maternal Hcy concentration by one unit indicates a 0.8 increase in infant MMA concentration. | ||
| Vitamin B12 | MMA | p = 0.015 |
| Increase in maternal Vitamin B12 concentration by one unit indicates a 0.04 decrease in infant MMA concentration. | ||
| MMA + MMA-I (P) | MMA | p < 0.001 |
| Increase in maternal MMA and MMA-I in plasma concentration by one unit indicates a 6.44 increase in infant MMA concentration. | ||
| MMA (U) | MMA | p = 0.034 |
| Increase in maternal MMA concentration in urine by one unit indicates a 0.7 increase in infant MMA concentration. | ||
| Folic acid | MCA | p = 0.014 |
| Increase in maternal folic acid concentration by one unit indicates a 0.1 increase in infant MCA concentration. | ||
| Homocysteine | MCA | p < 0.001 |
| Increase in maternal Hcy concentration by one unit indicates a 0.45 increase in infant MCA concentration. | ||
| MMA + MMA-I (P) | MCA | p < 0.001 |
| Increase in maternal MMA and MMA-I in plasma concentration by one unit indicates a 0.36 increase in infant MCA concentration. | ||
| NBS data (DBS 2) | ||
| Vitamin B12 | MMA | p = 0.02 |
| Increase in maternal vitamin B12 concentration by one unit indicates a 0.21 decrease in infant MMA concentration. | ||
| Homocysteine | Homocysteine | p < 0.001 |
| Increase in maternal Hcy concentration by one unit indicates a 0.2 increase in infant Hcy concentration. | ||
| Homocysteine | MMA | p < 0.001 |
| Increase in maternal Hcy concentration by one unit indicates a 0.32 increase in infant MMA concentration. | ||
| Homocysteine | MCA | p < 0.001 |
| Increase in maternal Hcy concentration by one unit indicates a 0.02 increase in infant MCA concentration. | ||
| MMA + MMA-I (P) | Homocysteine | p < 0.001 |
| Increase in maternal MMA and MMA-I in plasma concentration by one unit indicates a 0.4 increase in infant Hcy concentration. | ||
| MMA + MMA-I (P) | MMA | p < 0.001 |
| Increase in maternal MMA and MMA-I in plasma concentration by one unit indicates a 2.54 increase in infant MMA concentration. | ||
| MMA + MMA-I (P) | MCA | p = 0.005 |
| Increase in maternal MMA and MMA-I in plasma concentration by one unit indicates a 0.14 increase in infant MCA concentration. | ||
| MMA (U) | MMA | p = 0.033 |
| Increase in maternal MMA in urine concentration by one unit indicates a 0.22 increase in infant MMA concentration. | ||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Reischl-Hajiabadi, A.T.; Garbade, S.F.; Feyh, P.; Weiss, K.H.; Mütze, U.; Kölker, S.; Hoffmann, G.F.; Gramer, G. Maternal Vitamin B12 Deficiency Detected by Newborn Screening—Evaluation of Causes and Characteristics. Nutrients 2022, 14, 3767. https://doi.org/10.3390/nu14183767
Reischl-Hajiabadi AT, Garbade SF, Feyh P, Weiss KH, Mütze U, Kölker S, Hoffmann GF, Gramer G. Maternal Vitamin B12 Deficiency Detected by Newborn Screening—Evaluation of Causes and Characteristics. Nutrients. 2022; 14(18):3767. https://doi.org/10.3390/nu14183767
Chicago/Turabian StyleReischl-Hajiabadi, Anna T., Sven F. Garbade, Patrik Feyh, Karl Heinz Weiss, Ulrike Mütze, Stefan Kölker, Georg F. Hoffmann, and Gwendolyn Gramer. 2022. "Maternal Vitamin B12 Deficiency Detected by Newborn Screening—Evaluation of Causes and Characteristics" Nutrients 14, no. 18: 3767. https://doi.org/10.3390/nu14183767
APA StyleReischl-Hajiabadi, A. T., Garbade, S. F., Feyh, P., Weiss, K. H., Mütze, U., Kölker, S., Hoffmann, G. F., & Gramer, G. (2022). Maternal Vitamin B12 Deficiency Detected by Newborn Screening—Evaluation of Causes and Characteristics. Nutrients, 14(18), 3767. https://doi.org/10.3390/nu14183767