Microbial Metabolism of Naringin and the Impact on Antioxidant Capacity
Abstract
:1. Introduction
2. Materials and Methods
2.1. Chemicals and Reagents
2.2. Animals
2.3. In Vitro Fermentation of Naringin with Rat Gut Microbiota
2.4. Identification of the Microbial Metabolites of Naringin by UHPLC-Q-TOF-MS/MS
2.5. Quantification of the Microbial Metabolites of Naringin by UHPLC-Q-Trap-MS/MS
2.6. Measurement of Total Antioxidant Capacity of Naringin and Its Primary Metabolites
2.7. Data Analysis
3. Results and Discussion
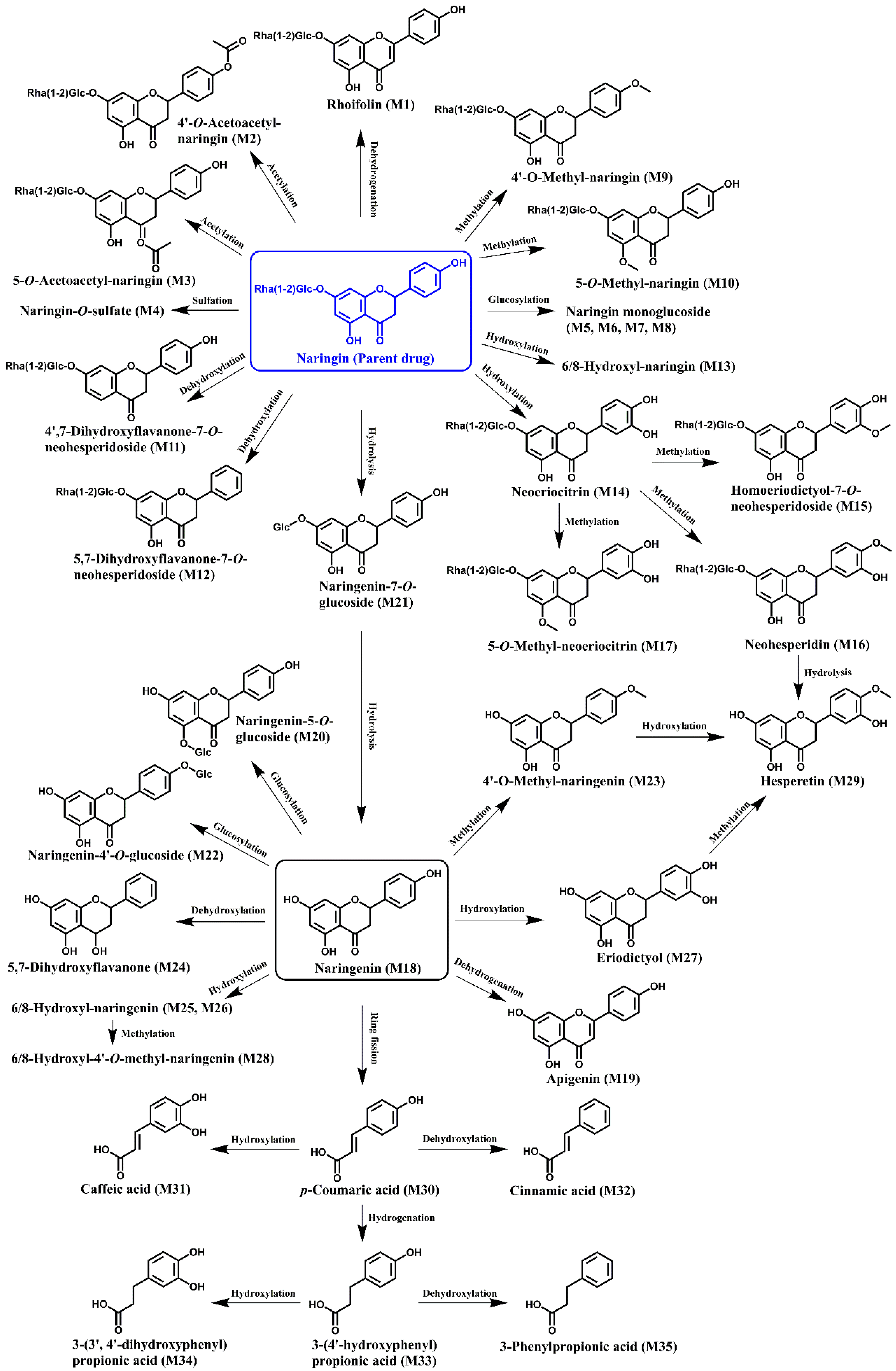
3.1. Identification of the Microbial Metabolites of Naringin after In Vitro Fecal Fermentation
3.2. Biotransformation of Naringin during In Vitro Fecal Fermentation
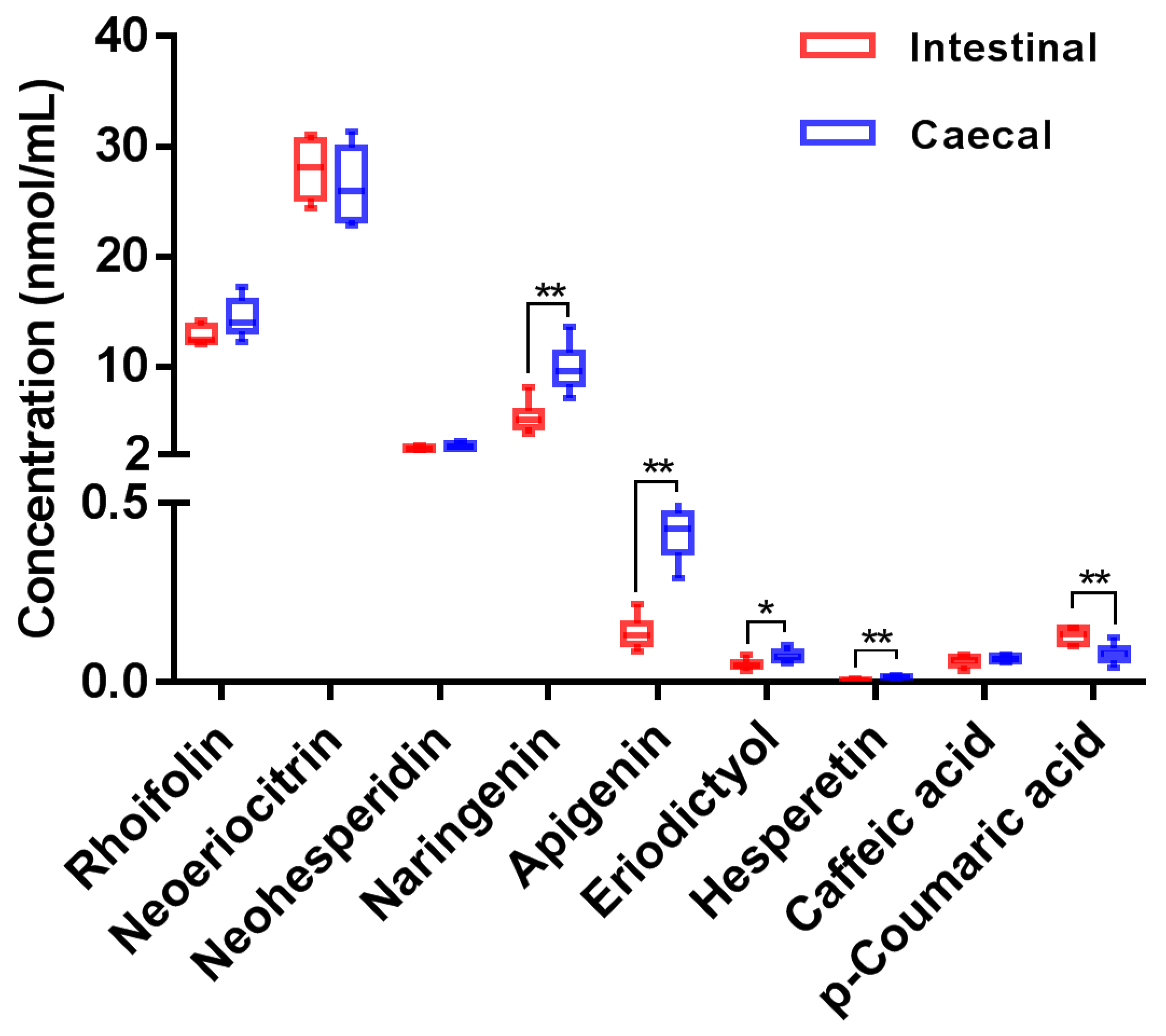
3.3. Quantification of the Microbial Metabolites of Naringin by UHPLC-Q-Trap-MS/MS
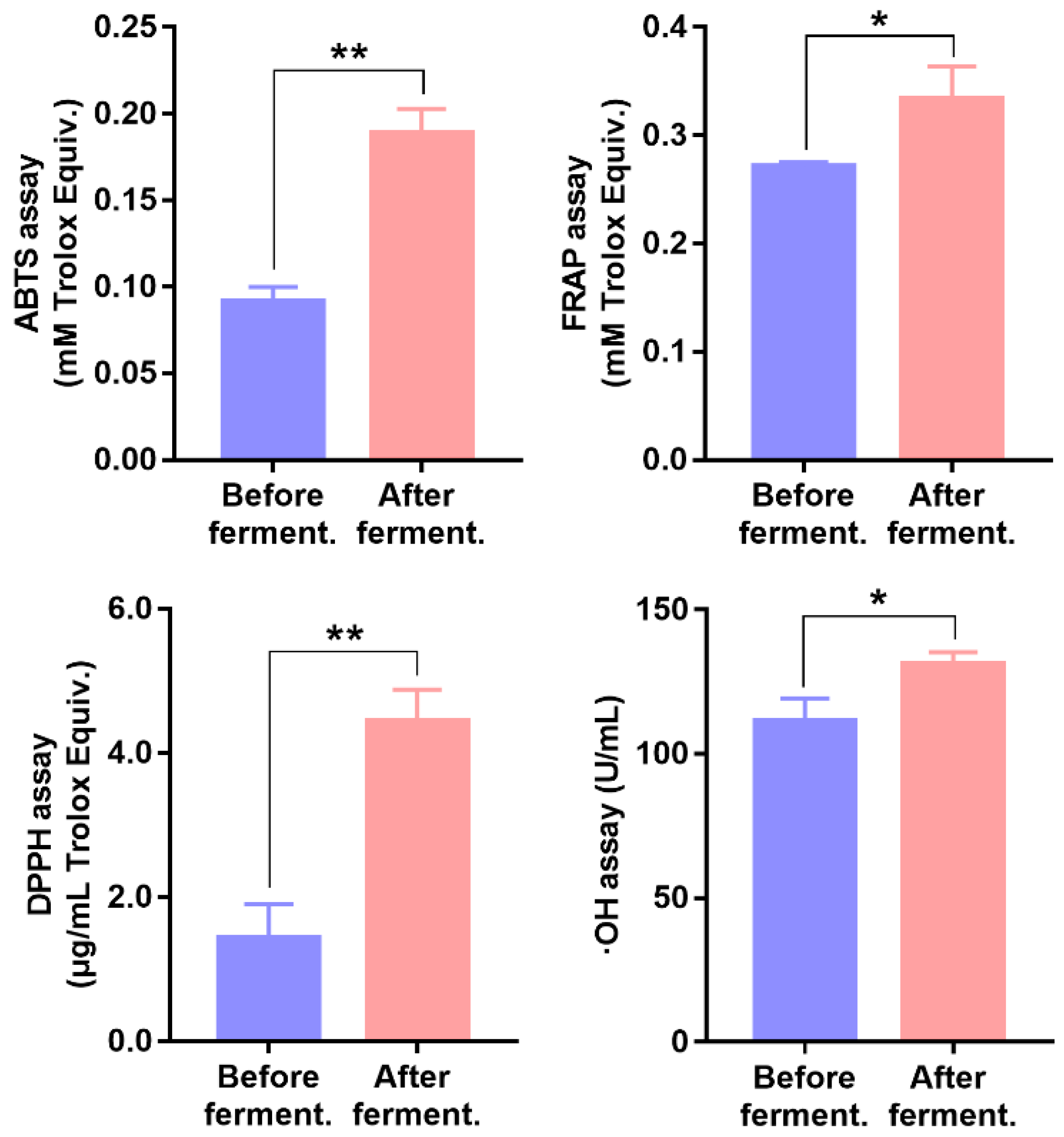
3.4. Effect of Fecal Fermentation on the Antioxidant Capacity
4. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Alam, M.A.; Subhan, N.; Rahman, M.M.; Uddin, S.J.; Reza, H.M.; Sarker, S.D. Effect of citrus flavonoids, naringin and naringenin, on metabolic syndrome and their mechanisms of action. Adv. Nutr. 2014, 5, 404–417. [Google Scholar] [CrossRef] [PubMed]
- Neveu, V.; Perez-Jiménez, J.; Vos, F.; Crespy, V.; du Chaffaut, L.; Mennen, L.; Knox, C.; Eisner, R.; Cruz, J.; Wishart, D.; et al. Phenol-Explorer: An online comprehensive database on polyphenol contents in foods. Database J. Biol. Databases Curation 2010, 2010, bap024. [Google Scholar] [CrossRef] [PubMed]
- Rothwell, J.A.; Urpi-Sarda, M.; Boto-Ordoñez, M.; Knox, C.; Llorach, R.; Eisner, R.; Cruz, J.; Neveu, V.; Wishart, D.; Manach, C.; et al. Phenol-Explorer 2.0: A major update of the Phenol-Explorer database integrating data on polyphenol metabolism and pharmacokinetics in humans and experimental animals. Database J. Biol. Databases Curation 2012, 2012, bas031. [Google Scholar] [CrossRef] [PubMed]
- Viswanatha, G.L.; Shylaja, H.; Moolemath, Y. The beneficial role of Naringin-a citrus bioflavonoid, against oxidative stress-induced neurobehavioral disorders and cognitive dysfunction in rodents: A systematic review and meta-analysis. Biomed. Pharmacother. 2017, 94, 909–929. [Google Scholar] [CrossRef]
- Miles, E.A.; Calder, P.C. Effects of citrus fruit juices and their bioactive components on inflammation and immunity: A narrative review. Front. Immunol. 2021, 12, 712608. [Google Scholar] [CrossRef]
- Ahmed, S.; Khan, H.; Aschner, M.; Hasan, M.M.; Hassan, S.T.S. Therapeutic potential of naringin in neurological disorders. Food Chem. Toxicol. 2019, 132, 110646. [Google Scholar] [CrossRef]
- Heidary Moghaddam, R.; Samimi, Z.; Moradi, S.Z.; Little, P.J.; Xu, S.; Farzaei, M.H. Naringenin and naringin in cardiovascular disease prevention: A preclinical review. Eur. J. Pharmacol. 2020, 887, 173535. [Google Scholar] [CrossRef]
- Raja Kumar, S.; Mohd Ramli, E.S.; Abdul Nasir, N.A.; Ismail, N.H.M.; Mohd Fahami, N.A. Preventive effect of naringin on metabolic syndrome and its mechanism of action: A systematic review. Evid. Based Complement. Alternat. Med. 2019, 2019, 9752826. [Google Scholar] [CrossRef]
- Zeng, X.; Su, W.; Liu, B.; Chai, L.; Shi, R.; Yao, H. A review on the pharmacokinetic properties of naringin and its therapeutic efficacies in respiratory diseases. Mini Rev. Med. Chem. 2020, 20, 286–293. [Google Scholar] [CrossRef]
- Rivoira, M.A.; Rodriguez, V.; Talamoni, G.; Tolosa de Talamoni, N. New perspectives in the pharmacological potential of naringin in medicine. Curr. Med. Chem. 2021, 28, 1987–2007. [Google Scholar] [CrossRef]
- Sánchez-Patán, F.; Barroso, E.; van de Wiele, T.; Jiménez-Girón, A.; Martín-Alvarez, P.J.; Moreno-Arribas, M.V.; Martínez-Cuesta, M.C.; Peláez, C.; Requena, T.; Bartolomé, B. Comparative in vitro fermentations of cranberry and grape seed polyphenols with colonic microbiota. Food Chem. 2015, 183, 273–282. [Google Scholar] [CrossRef]
- Lingua, M.S.; Wunderlin, D.A.; Baroni, M.V. Effect of simulated digestion on the phenolic components of red grapes and their corresponding wines. J. Funct. Foods 2018, 44, 86–94. [Google Scholar] [CrossRef]
- Caponio, G.R.; Noviello, M.; Calabrese, F.M.; Gambacorta, G.; Giannelli, G.; De Angelis, M. Effects of grape pomace polyphenols and in vitro gastrointestinal digestion on antimicrobial activity: Recovery of bioactive compounds. Antioxidants 2022, 11, 567. [Google Scholar] [CrossRef]
- Kawabata, K.; Yoshioka, Y.; Terao, J. Role of intestinal microbiota in the bioavailability and physiological functions of dietary polyphenols. Molecules 2019, 24, 370. [Google Scholar] [CrossRef]
- Joshi, R.; Kulkarni, Y.A.; Wairkar, S. Pharmacokinetic, pharmacodynamic and formulations aspects of Naringenin: An update. Life Sci. 2018, 215, 43–56. [Google Scholar] [CrossRef]
- Stevens, Y.; Rymenant, E.V.; Grootaert, C.; Camp, J.V.; Possemiers, S.; Masclee, A.; Jonkers, D. The intestinal fate of citrus flavanones and their effects on gastrointestinal health. Nutrients 2019, 11, 1464. [Google Scholar] [CrossRef]
- Zhang, M.; Zhu, S.; Yang, W.; Huang, Q.; Ho, C.T. The biological fate and bioefficacy of citrus flavonoids: Bioavailability, biotransformation, and delivery systems. Food Funct. 2021, 12, 3307–3323. [Google Scholar] [CrossRef]
- Zeng, X.; Su, W.; Zheng, Y.; He, Y.; He, Y.; Rao, H.; Peng, W.; Yao, H. Pharmacokinetics, tissue distribution, metabolism, and excretion of naringin in aged rats. Front. Pharmacol. 2019, 10, 34. [Google Scholar] [CrossRef]
- Jeon, S.M.; Kim, H.K.; Kim, H.J.; Do, G.M.; Jeong, T.S.; Park, Y.B.; Choi, M.S. Hypocholesterolemic and antioxidative effects of naringenin and its two metabolites in high-cholesterol fed rats. Transl. Res. 2007, 149, 15–21. [Google Scholar] [CrossRef]
- Steed, A.L.; Christophi, G.P.; Kaiko, G.E.; Sun, L.; Goodwin, V.M.; Jain, U.; Esaulova, E.; Artyomov, M.N.; Morales, D.J.; Holtzman, M.J.; et al. The microbial metabolite desaminotyrosine protects from influenza through type I interferon. Science 2017, 357, 498–502. [Google Scholar] [CrossRef] [Green Version]
- Wei, Y.; Gao, J.; Kou, Y.; Liu, M.; Meng, L.; Zheng, X.; Xu, S.; Liang, M.; Sun, H.; Liu, Z.; et al. The intestinal microbial metabolite desaminotyrosine is an anti-inflammatory molecule that modulates local and systemic immune homeostasis. FASEB J. 2020, 34, 16117–16128. [Google Scholar] [CrossRef] [PubMed]
- Dey, P. Gut microbiota in phytopharmacology: A comprehensive overview of concepts, reciprocal interactions, biotransformations and mode of actions. Pharmacol. Res. 2019, 147, 104367. [Google Scholar] [CrossRef] [PubMed]
- Feng, X.; Li, Y.; Brobbey Oppong, M.; Qiu, F. Insights into the intestinal bacterial metabolism of flavonoids and the bioactivities of their microbe-derived ring cleavage metabolites. Drug Metab. Rev. 2018, 50, 343–356. [Google Scholar] [CrossRef] [PubMed]
- Chen, Z.; Zhang, Z.; Liu, J.; Qi, H.; Li, J.; Chen, J.; Huang, Q.; Liu, Q.; Mi, J.; Li, X. Gut microbiota: Therapeutic targets of ginseng against multiple disorders and ginsenoside transformation. Front. Cell Infect. Microbiol. 2022, 12, 853981. [Google Scholar] [CrossRef]
- Liu, Z.; de Bruijn, W.J.C.; Bruins, M.E.; Vincken, J.P. Microbial metabolism of theaflavin-3,3′-digallate and its gut microbiota composition modulatory effects. J. Agric. Food Chem. 2021, 69, 232–245. [Google Scholar] [CrossRef]
- Xiong, W.; Huang, M.; Liang, J.; Liao, C.; Liu, X.; Liu, X.; Huang, H. In vitro metabolism of naringin by human intestinal microflora. Chin. J. Exp. Tradit. Med. Formulae 2015, 21, 69–71. [Google Scholar]
- Zou, W.; Luo, Y.; Liu, M.; Chen, S.; Wang, S.; Nie, Y.; Cheng, G.; Su, W.; Zhang, K. Human intestinal microbial metabolism of naringin. Eur. J. Drug Metab. Pharmacokinet. 2015, 40, 363–367. [Google Scholar] [CrossRef]
- Chen, T.; Su, W.; Yan, Z.; Wu, H.; Zeng, X.; Peng, W.; Gan, L.; Zhang, Y.; Yao, H. Identification of naringin metabolites mediated by human intestinal microbes with stable isotope-labeling method and UFLC-Q-TOF-MS/MS. J. Pharm. Biomed. Anal. 2018, 161, 262–272. [Google Scholar] [CrossRef]
- Lee, S.M.; Kim, N.; Park, J.H.; Nam, R.H.; Yoon, K.; Lee, D.H. Comparative analysis of ileal and cecal microbiota in aged rats. J. Cancer Prev. 2018, 23, 70–76. [Google Scholar] [CrossRef]
- Qian, H.; Yang, Z.; Liu, D.; Zhang, Y.; Yu, F.; Ma, Z. Study on the metabolism of echinacoside by human intestinal bacteria in vitro. West China J. Pharm. Sci. 2017, 32, 641–643. [Google Scholar]
- Zeng, X.; Yao, H.; Zheng, Y.; Chen, T.; Peng, W.; Wu, H.; Su, W. Metabolite profiling of naringin in rat urine and feces using stable isotope labeling based liquid chromatography-mass spectrometry. J. Agric. Food Chem. 2020, 68, 409–417. [Google Scholar] [CrossRef]
- Pharmacopoeia of the People’s Republic of China. Guidelines for validation of quantitative analytical method of biological samples. In Pharmacopoeia of the People’s Republic of China; China Medical Science Press: Beijing, China, 2020; pp. 466–472. [Google Scholar]
- Zeng, X.; Su, W.; Liu, H.; Zheng, Y.; Chen, T.; Zhang, W.; Yan, Z.; Bai, Y.; Yao, H. Simultaneous determination of rosuvastatin, naringin and naringenin in rat plasma by RRLC-MS/MS and its application to a pharmacokinetic drug interaction study. J. Chromatogr. Sci. 2018, 56, 611–618. [Google Scholar] [CrossRef] [Green Version]
- Zeng, X.; Zheng, Y.; He, Y.; Peng, W.; Su, W. A rapid LC-MS/MS method for simultaneous determination of ten flavonoid metabolites of naringin in rat urine and its application to an excretion study. Foods 2022, 11, 316. [Google Scholar] [CrossRef]
- Corradini, E.; Foglia, P.; Giansanti, P.; Gubbiotti, R.; Samperi, R.; Lagana, A. Flavonoids: Chemical properties and analytical methodologies of identification and quantitation in foods and plants. Nat. Prod. Res. 2011, 25, 469–495. [Google Scholar] [CrossRef]
- Yang, M.; Li, J.; Zhao, C.; Xiao, H.; Fang, X.; Zheng, J. LC-Q-TOF-MS/MS detection of food flavonoids: Principle, methodology, and applications. Crit. Rev. Food Sci. Nutr. 2021, 62, 1–21. [Google Scholar] [CrossRef]
- Miyake, Y.; Minato, K.; Fukumoto, S.; Yamamoto, K.; Oya-Ito, T.; Kawakishi, S.; Osawa, T. New potent antioxidative hydroxyflavanones produced with Aspergillus saitoi from flavanone glycoside in citrus fruit. Biosci. Biotechnol. Biochem. 2003, 67, 1443–1450. [Google Scholar] [CrossRef]
- Kometani, T.; Nishimura, T.; Nakae, T.; Takii, H.; Okada, S. Synthesis of neohesperidin glycosides and naringin glycosides by cyclodextrin glucanotransferase from an alkalophilic Bacillus species. Biosci. Biotechnol. Biochem. 1996, 60, 645–649. [Google Scholar] [CrossRef]
- Lee, S.J.; Kim, J.C.; Kim, M.J.; Kitaoka, M.; Park, C.S.; Lee, S.Y.; Ra, M.J.; Moon, T.W.; Robyt, J.F.; Park, K.H. Transglycosylation of naringin by Bacillus stearothermophilusMaltogenic amylase to give glycosylated naringin. J. Agric. Food. Chem. 1999, 47, 3669–3674. [Google Scholar] [CrossRef]
- Krauze-Baranowska, M.; Pobłocka-Olech, L.; Głód, D.; Wiwart, M.; Zieliński, J.; Migas, P. HPLC of flavanones and chalcones in different species and clones of Salix. Acta Pol. Pharm. 2013, 70, 27–34. [Google Scholar]
- Werner, S.R.; Morgan, J.A. Expression of a Dianthus flavonoid glucosyltransferase in Saccharomyces cerevisiae for whole-cell biocatalysis. J. Biotechnol. 2009, 142, 233–241. [Google Scholar] [CrossRef]
- Murota, K.; Nakamura, Y.; Uehara, M. Flavonoid metabolism: The interaction of metabolites and gut microbiota. Biosci. Biotechnol. Biochem. 2018, 82, 600–610. [Google Scholar] [CrossRef]
- Donaldson, G.P.; Lee, S.M.; Mazmanian, S.K. Gut biogeography of the bacterial microbiota. Nat. Rev. Microbiol. 2016, 14, 20–32. [Google Scholar] [CrossRef]
- Tropini, C.; Earle, K.A.; Huang, K.C.; Sonnenburg, J.L. The gut microbiome: Connecting spatial organization to function. Cell Host Microbe 2017, 21, 433–442. [Google Scholar] [CrossRef] [Green Version]
- Li, D.; Chen, H.; Mao, B.; Yang, Q.; Zhao, J.; Gu, Z.; Zhang, H.; Chen, Y.Q.; Chen, W. Microbial biogeography and core microbiota of the rat digestive tract. Sci. Rep. 2017, 8, 45840. [Google Scholar] [CrossRef]
- Chen, T.; Wu, H.; He, Y.; Pan, W.; Yan, Z.; Liao, Y.; Peng, W.; Gan, L.; Zhang, Y.; Su, W.; et al. Simultaneously quantitative analysis of naringin and its major human gut microbial metabolites Naringenin and 3-(4′-Hydroxyphenyl) propanoic acid via stable isotope deuterium-labeling coupled with RRLC-MS/MS Method. Molecules 2019, 24, 4287. [Google Scholar] [CrossRef]
- Bhattacharyya, A.; Chattopadhyay, R.; Mitra, S.; Crowe, S.E. Oxidative stress: An essential factor in the pathogenesis of gastrointestinal mucosal diseases. Physiol. Rev. 2014, 94, 329–354. [Google Scholar] [CrossRef]
- Pérez, S.; Taléns-Visconti, R.; Rius-Pérez, S.; Finamor, I.; Sastre, J. Redox signaling in the gastrointestinal tract. Free Radic. Biol. Med. 2017, 104, 75–103. [Google Scholar] [CrossRef]
- Yu, Q.Q.; Zhang, H.; Guo, Y.; Han, B.; Jiang, P. The intestinal redox system and its significance in chemotherapy-induced intestinal mucositis. Oxid. Med. Cell Longev. 2022, 2022, 7255497. [Google Scholar] [CrossRef] [PubMed]
| No. | Analytes | Q1 Mass (Da) | Q3 Mass (Da) | DP (eV) | CE (eV) |
|---|---|---|---|---|---|
| 1 | Naringin | 579.1 | 271.1 | −45 | −120 |
| 2 | Rhoifolin | 577.1 | 269.0 | −49 | −46 |
| 3 | Neoeriocitrin | 595.1 | 459.1 | −36 | −98 |
| 4 | Neohesperidin | 609.1 | 301.1 | −39 | −131 |
| 5 | Naringenin | 270.9 | 150.9 | −24 | −44 |
| 6 | Apigenin | 269.0 | 151.0 | −33 | −48 |
| 7 | Eriodictyol | 286.9 | 135.0 | −38 | −56 |
| 8 | Hesperetin | 301.0 | 163.9 | −32 | −134 |
| 9 | p-Coumaric acid | 163.0 | 119.1 | −15 | −83 |
| 10 | Caffeic acid | 179.0 | 135.0 | −35 | −80 |
| 11 | Isoquercitrin (IS) | 463.1 | 299.9 | −36 | −32 |
| No. | Identified Compounds | Formula | RT (min) | [M-H]− (Error, ppm) | Fragment Ions a |
|---|---|---|---|---|---|
| Parent drug | Naringin b | C27H32O14 | 11.5 | 579.1723 (0.6) | 459.1120[M-H-C8H8O]−, 339.0710[M-H-C8H8O-C4H8O4]−, 313.0708[M-H-C8H8O-Rha]−, 271.0590[M-H-Rha-Glc]−, 177.0186[M-H-Rha-Glc-C6H6O]−, 151.0023[M-H-Rha-Glc-C8H8O]−, 119.0493[M-H-Rha-Glc-C7H4O4]− |
| M1 | Rhoifolin b | C27H30O14 | 12.1 | 577.1571 (1.4) | 431.0987[M-H-Rha]−, 413.0871[M-H-Rha-H2O]−, 311.0550[M-H-Rha-C4H8O4]−, 269.0447[M-H-Rha-Glc]− |
| M2 | 4′-O-Acetyl-naringin | C29H34O15 | 12.4 | 621.1808 (−2.7) | 579.1741[M-H-C2H2O]−, 501.1221[M-H-C4H8O4]−, 459.1327[M-H-C4H8O4-C2H2O]−, 339.0740[M-H-C4H8O4-C2H2O-C8H8O]−, 271.0594[M-H-C2H2O-Rha-Glc]−, 151.0041[M-H-C2H2O-Rha-Glc-C8H8O]− |
| M3 | 5-O-Acetyl-naringin | C29H34O15 | 13.4 | 621.1816 (−1.5) | 579.1533[M-H-C2H2O]−, 577.3041, 501.1253[M-H-C4H8O4]−, 459.1389[M-H-C4H8O4-C2H2O]−, 408.2170[M-H-C4H8O4-C6H5O]−, 339.0658[M-H-C4H8O4-C2H2O-C8H8O]−, 271.0593[M-H-C2H2O-Rha-Glc]−, 151.0030[M-H-C2H2O-Rha-Glc-C8H8O]−, 119.0434[M-H-C2H2O-Rha-Glc-C7H4O4]− |
| M4 | Naringin-O-sulfate | C27H32O17S | 10.8 | 659.1339 (4.8) | 596.1722, 579.1683[M-H-SO3]−, 459.1150[M-H-SO3-C8H8O]−, 387.0670, 351.0199[M-H-Rha-Glc]−, 271.0629[M-H-SO3-Rha-Glc]−, 151.0046[M-H-SO3-Rha-Glc-C8H8O]− |
| M5 | Naringin monoglucoside | C33H42O19 | 9.7 | 741.2266 (2.4) | 579.1736[M-H-Glc]−, 459.1147[M-H-Glc-C8H8O]−, 433.1197[M-H-Glc-Rha]−, 339.0582[M-H-Glc-C8H8O-C4H8O4]−, 313.0691[M-H-Glc-Rha-C8H8O]−, 271.0646[M-H-Glc-Rha-Glc]−, 151.0080[M-H-Glc-Rha-Glc-C8H8O]− |
| M6 | Naringin monoglucoside | C33H42O19 | 10.1 | 741.2266 (2.4) | 723.3698[M-H-H2O]−, 621.1735[M-H-C4H8O4]−, 459.1375[M-H-C4H8O4-Glc]−, 339.0673[M-H-C4H8O4-Glc-C8H8O]−, 271.0598[M-H-Glc-Rha-Glc]−, 151.0053[M-H-Glc-Rha-Glc-C8H8O]− |
| M7 | Naringin monoglucoside | C33H42O19 | 10.3 | 741.2250 (0.4) | 621.1645[M-H-C4H8O4]−, 579.1766[M-H-Glc]−, 459.1364[M-H-C4H8O4-Glc]−, 339.0701[M-H-C4H8O4-Glc-C8H8O]−, 271.0609[M-H-Glc-Rha-Glc]−, 151.0057[M-H-Glc-Rha-Glc-C8H8O]− |
| M8 | Naringin monoglucoside | C33H42O19 | 11.3 | 741.2253 (0.8) | 621.1674[M-H-C4H8O4]−, 595.1883[M-H-Rha]−, 579.1776[M-H-Glc]−, 271.0615[M-H-Glc-Rha-Glc]−, 227.0710, 151.0056[M-H-Glc-Rha-Glc-C8H8O]− |
| M9 | 4′-O-Methyl-naringin | C28H34O14 | 13.3 | 593.1866 (−1.6) | 473.1440[M-H-C4H8O4]−, 459.1134[M-H-C9H10O]−, 447.1294[M-H-Rha]−, 431.1334[M-H-C9H10O-CO]−, 387.1080[M-H-Rha-C2H4O2]−, 327.0868[M-H-C4H8O4-Rha]−, 285.0756[M-H-Rha-Glc]−, 270.0534[M-H-Rha-Glc-CH3]−, 241.0868, 164.0120, 151.0039[M-H-Rha-Glc-C9H10O]− |
| M10 | 5-O-Methyl-naringin | C28H34O14 | 14.3 | 593.1857 (−3.2) | 513.2740, 473.1496[M-H-C4H8O4]−, 327.0802[M-H-C4H8O4-Rha]−, 285.0746[M-H-Rha-Glc]−, 241.0898 |
| M11 | 4′,7-Dihydroxyflavanone-7-O-neohesperidoside | C27H32O13 | 13.3 | 563.1774 (0.7) | 443.1395[M-H-C8H8O]−, 297.0875[M-H-C8H8O-Rha]−, 255.0680[M-H-Rha-Glc]−, 211.0774 |
| M12 | 5,7-Dihydroxyflavanone-7-O-neohesperidoside | C27H32O13 | 13.5 | 563.1780 (1.8) | 459.1256[M-H-C8H8]−, 443.1233[M-H-C4H8O4]−, 339.0747[M-H-C8H8-C4H8O4]−, 271.0623, 151.0023[M-H-C8H8-Rha-Glc]−, 119.0526 |
| M13 | 6/8-Hydroxyl-naringin | C27H32O15 | 10.3 | 595.1671 (0.4) | 475.1084[M-H-C8H8O]−, 431.0978[M-H-C8H8O-CO2]−, 287.0580[M-H-Rha-Glc]−, 269.0453, 166.9985[M-H-Rha-Glc-C8H8O]−, 153.0195, 139.0039[M-H-Rha-Glc-C8H8O-CO]−, 119.04895[M-H-Rha-Glc-C7H4O5]− |
| M14 | Neoeriocitrin b | C27H32O15 | 10.7 | 595.1671 (0.5) | 475.1102[M-H-C4H8O4]−, 459.1135[M-H-C8H8O2]−, 339.0718[M-H-C8H8O2-C4H8O4]−, 287.0572[M-H-Rha-Glc]−, 235.0254, 193.0152, 151.0039[M-H-Rha-Glc-C8H8O2]−, 135.0448[M-H-Rha-Glc-C7H4O4]− |
| M15 | Homoeriodictyol-7-O-neohesperidoside | C28H34O15 | 11.6 | 609.1794 (−4.5) | 563.1417[M-H-CO-H2O]−, 489.1238[M-H-C4H8O4]−, 459.1091[M-H-C9H10O2]−, 343.0874[M-H -C4H8O4-Rha]−, 301.0742[M-H-Rha-Glc]−, 235.0208, 151.0023[M-H-Rha-Glc-C9H10O2]−, 125.0272 |
| M16 | Neohesperidin b | C28H34O15 | 11.8 | 609.1830 (0.8) | 489.1373[M-H-C4H8O4]−, 403.1013, 343.0823[M-H -C4H8O4-Rha]−, 325.0736[M-H-Rha-C4H8O4-H2O]−, 301.0718[M-H-Rha-Glc]−, 286.0494[M-H-Rha-Glc-CH3]−, 257.0820[M-H-Rha-Glc-CH3-HCO]−, 242.0581[M-H-Rha-Glc-OCH2-HCO]−, 164.0127[M-H-Rha-Glc-C8H9O2]−, 151.0051[M-H-Rha-Glc-C9H10O2]−, 125.0260 |
| M17 | 5-O-Methyl-neoeriocitrin | C28H34O15 | 12.4 | 609.1824 (−0.2) | 591.2831[M-H-H2O]−, 445.1171[M-H-H2O-Rha]−, 364.1490, 301.0718[M-H-Rha-Glc]−, 273.0760[M-H-Rha-Glc-CO]−, 226.1194, 165.9897[M-H-Rha-Glc-C8H7O2]− |
| M18 | Naringenin b | C15H12O5 | 13.7 | 271.0615 (1.0) | 227.0697, 177.0190[M-H-C6H6O]−, 151.0028[M-H-C8H8O]−, 119.0495[M-H-C7H4O4]−, 107.0134[M-H-C8H8O-CO2]−, 93.0339[M-H-C9H6O4]−, 83.0127 |
| M19 | Apigenin b | C15H10O5 | 15.0 | 269.0454 (−0.6) | 225.0552, 201.0555, 151.0031[M-H-C8H6O]−, 117.0342[M-H-C7H4O4]−, 107.0132[M-H-C8H6O-CO2]− |
| M20 | Naringenin-5-O-glucoside | C21H22O10 | 11.8 | 433.1145 (1.2) | 415.1077[M-H-H2O]−, 373.0961[M-H-C2H4O2]−, 343.0830[M-H-C3H6O3]−, 313.0707[M-H-C4H8O4]−, 271.0613[M-H-Glc]−, 223.0271[M-H-C3H6O3-C8H8O]−, 205.0153[M-H-C3H6O3-C8H8O-H2O]−, 151.0029[M-H-Glc-C8H8O]−, 119.0494[M-H-Glc-C7H4O4]−, 93.0357[M-H-Glc-C9H6O4]− |
| M21 | Naringenin-7-O-glucoside | C21H22O10 | 12.2 | 433.1140 (−0.1) | 415.1071[M-H-H2O]−, 397.0795[M-H-2H2O]−, 373.0938[M-H-C2H4O2]−, 343.0812[M-H-C3H6O3]−, 313.0700[M-H-C4H8O4]−, 271.0618[M-H-Glc]−, 223.0243[M-H-C3H6O3-C8H8O]−, 151.0026[M-H-Glc-C8H8O]−, 119.0492[M-H-Glc-C7H4O4]−, 107.0116[M-H-Glc-C8H8O-CO2]− |
| M22 | Naringenin-4′-O-glucoside | C21H22O10 | 12.9 | 433.1140 (0.1) | 313.0765[M-H-C4H8O4]−, 271.0606[M-H-Glc]−, 151.0050[M-H-Glc-C8H8O]−, 119.0511[M-H-Glc-C7H4O4]−, 93.0322[M-H-Glc-C9H6O4]− |
| M23 | 4′-O-Methyl-naringenin | C16H14O5 | 16.5 | 285.0771 (0.9) | 270.0542[M-H-CH3]−, 243.0665[M-H-C2H2O]−, 227.0348, 215.0727, 201.0563, 175.0774, 164.0121, 151.0034[M-H-C9H10O]−, 136.0159, 108.0214 |
| M24 | 5,7-Dihydroxyflavanone | C15H12O4 | 16.7 | 255.0665 (0.9) | 213.0523[M-H-C2H2O]−, 171.0408, 151.0029[M-H-C8H8]−, 145.0664, 107.0127[M-H-C8H8-CO2]−, 83.0114 |
| M25 | 6-Hydroxyl-naringenin | C15H12O6 | 11.9 | 287.0565 (1.4) | 259.0613[M-H-CO]−, 243.0673, 181.0136[M-H-C7H6O]−, 166.9989[M-H-C8H8O]−, 153.0189[M-H-C7H6O-CO]−, 139.0025[M-H-C8H8O-CO]−, 119.0494[M-H-C7H4O5]−, 111.0085, 95.0139 |
| M26 | 8-Hydroxyl-naringenin | C15H12O6 | 12.2 | 287.0564 (1.0) | 259.0616[M-H-CO]−, 193.0131[M-H-C6H6O]−, 181.0152[M-H-C7H6O]−, 166.9982[M-H-C8H8O]−, 153.0195[M-H-C7H6O-CO]−, 139.0032[M-H-C8H8O-CO]−, 123.0055[M-H-C8H8O-CO2]−, 119.0497[M-H-C7H4O5]−, 111.0071, 95.0135 |
| M27 | Eriodictyol b | C15H12O6 | 12.8 | 287.0565 (1.3) | 151.0027[M-H-C8H8O2]−, 135.0445[M-H-C7H4O4]−, 125.0231, 107.0136[M-H-C8H8O2-CO2]−, 83.0138 |
| M28 | 6/8-Hydroxyl-4′-O-methyl-naringenin | C16H14O6 | 11.2 | 301.0713 (−1.5) | 257.0785[M-H-CH3-HCO]−, 213.0930, 195.0816[M-H-C7H6O]−, 107.0501[M-H-C9H6O5]−, 93.0351[M-H-C9H6O5-CH2]− |
| M29 | Hesperetin b | C16H14O6 | 14.0 | 301.0712 (−1.9) | 286.0525[M-H-CH3]−, 257.0766[M-H-CH3-HCO]−, 242.0533[M-H-OCH2-HCO]−, 224.0465, 199.0381, 164.0103[M-H-C8H9O2]−, 151.0021[M-H-C9H10O2]−, 135.0405, 108.0206 |
| M30 | p-Coumaric acid b | C9H8O3 | 10.9 | 163.0407 (3.8) | 119.0495[M-H-CO2]−, 93.0344[M-H-CO2-C2H2]− |
| M31 | Caffeic acid b | C9H8O4 | 9.5 | 179.0351 (0.9) | 135.0448[M-H-CO2]−, 107.0493, 89.0399 |
| M32 | Cinnamic acid | C9H8O2 | 11.2 | 147.0451 (−0.1) | 103.0562[M-H-CO2]− |
| M33 | 3-(4′-Hydroxyphenyl)propionic acid b | C9H10O3 | 10.9 | 165.0558 (0.6) | 121.0657[M-H-CO2]−, 119.0491[M-H-HCOOH]−, 106.0412[M-H-CO2-CH3]−, 96.9628 |
| M34 | 3-(3′, 4′-Dihydroxyphenyl)propionic acid | C9H10O4 | 7.9 | 181.0506 (−0.1) | 163.0400[M-H-H2O]−, 135.0475[M-H-H2O-CO]−, 119.0469[M-H-H2O-CO2]−, 107.0490[M-H-H2O-2CO]− |
| M35 | 3-Phenylpropionic acid | C9H10O2 | 13.6 | 149.0609 (0.4) | 131.0104[M-H-H2O]−, 105.0679[M-H-CO2]− |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zeng, X.; Zheng, Y.; He, Y.; Zhang, J.; Peng, W.; Su, W. Microbial Metabolism of Naringin and the Impact on Antioxidant Capacity. Nutrients 2022, 14, 3765. https://doi.org/10.3390/nu14183765
Zeng X, Zheng Y, He Y, Zhang J, Peng W, Su W. Microbial Metabolism of Naringin and the Impact on Antioxidant Capacity. Nutrients. 2022; 14(18):3765. https://doi.org/10.3390/nu14183765
Chicago/Turabian StyleZeng, Xuan, Yuying Zheng, Yan He, Jiashuo Zhang, Wei Peng, and Weiwei Su. 2022. "Microbial Metabolism of Naringin and the Impact on Antioxidant Capacity" Nutrients 14, no. 18: 3765. https://doi.org/10.3390/nu14183765
APA StyleZeng, X., Zheng, Y., He, Y., Zhang, J., Peng, W., & Su, W. (2022). Microbial Metabolism of Naringin and the Impact on Antioxidant Capacity. Nutrients, 14(18), 3765. https://doi.org/10.3390/nu14183765







