Infection in Living Donor Liver Transplantation Leads to Increased Risk of Adverse Renal Outcomes
Abstract
:1. Introduction
2. Materials and Methods
2.1. Participants and Measurements
2.2. Exposures of Interest
2.3. Outcomes of Interest
2.4. Statistical Analysis
3. Results
3.1. Baseline Characteristics
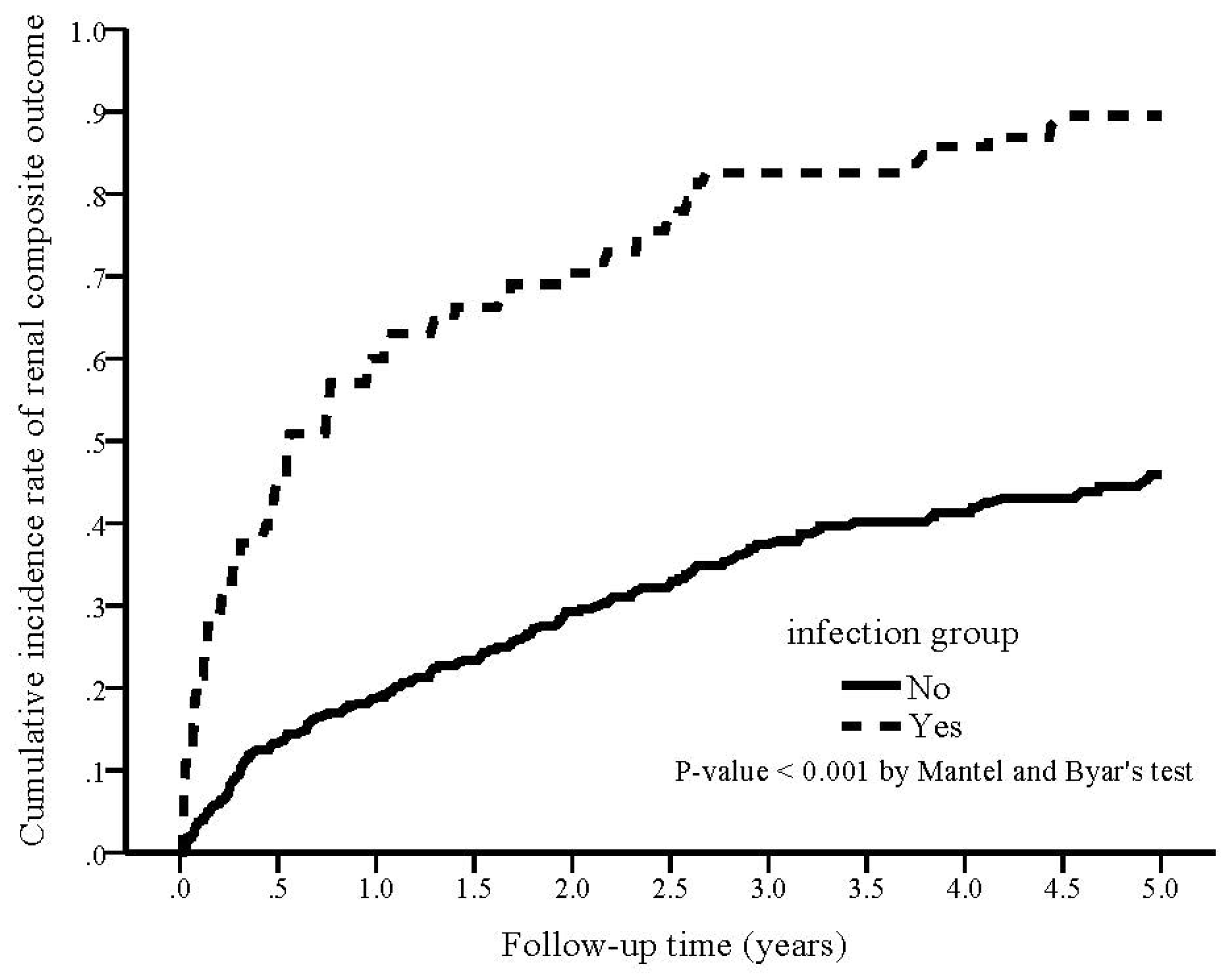
3.2. Association of Infection with Renal Outcomes during the Follow-Up Period
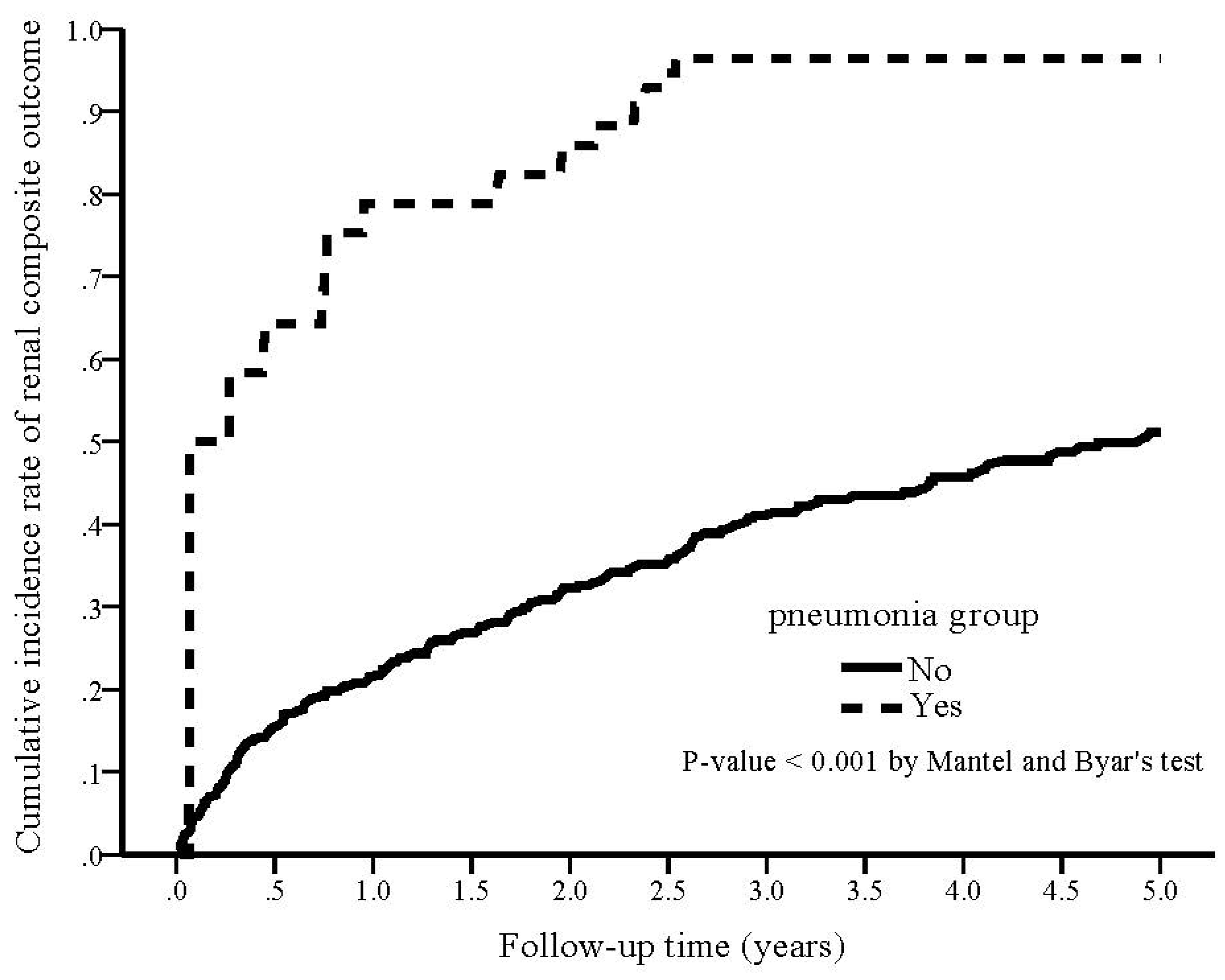
3.3. Association of Pneumonia with Renal Outcomes during the Follow-Up Period
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Ojo, A.O.; Held, P.J.; Port, F.K.; Wolfe, R.A.; Leichtman, A.B.; Young, E.W.; Arndorfer, J.; Christensen, L.; Merion, R.M. Chronic renal failure after transplantation of a nonrenal organ. N. Engl. J. Med. 2003, 349, 931. [Google Scholar] [CrossRef] [PubMed]
- Allen, A.M.; Kim, W.R.; Therneau, T.M.; Larson, J.J.; Heimbach, J.K.; Rule, A.D. Chronic kidney disease and associated mortality after liver transplantation—A time-dependent analysis using measured glomerular filtration rate. J. Hepatol. 2014, 61, 286. [Google Scholar] [CrossRef] [PubMed]
- Nishi, H.; Shibagaki, Y.; Kido, R.; Tamura, S.; Nangaku, M.; Sugawara, Y.; Fujita, T. Chronic renal outcome after living donor liver transplantation. Clin. Transpl. 2013, 27, 90. [Google Scholar] [CrossRef] [PubMed]
- Lim, S.Y.; Wang, R.; Tan, D.J.H.; Ng, C.H.; Lim, W.H.; Quek, J.; Syn, N.; Nah, B.K.Y.; Wong, E.T.; Huang, D.Q.; et al. A meta-analysis of the cumulative incidence, risk factors, and clinical outcomes associated with chronic kidney disease after liver transplantation. Transpl. Int. 2021, 34, 2524–2533. [Google Scholar] [CrossRef] [PubMed]
- Paterno, F.; Wilson, G.C.; Wima, K.; Quillin, R.C.; Abbott, D.E., 3rd; Cuffy, M.C.; Diwan, T.S.; Kaiser, T.; Woodle, E.S.; Shah, S.A. Hospital utilization and consequences of readmissions after liver transplantation. Surgery 2014, 156, 871–878. [Google Scholar] [CrossRef]
- Lee, S.B.; Kalluri, R. Mechanistic connection between inflammation and fibrosis. Kidney Int. Suppl. 2010, 119, S22–S26. [Google Scholar] [CrossRef]
- Kinsey, G.R.; Li, L.; Okusa, M.D. Inflammation in acute kidney injury. Nephron. Exp. Nephrol. 2008, 109, e102–e107. [Google Scholar] [CrossRef]
- Akcay, A.; Nguyen, Q.; Edelstein, C.L. Mediators of inflammation in acute kidney injury. Mediat. Inflamm. 2009, 2009, 137072. [Google Scholar] [CrossRef]
- Naghavi, M.; Wyde, P.; Litovsky, S.; Madjid, M.; Akhtar, A.; Naguib, S.; Siadaty, M.S.; Sanati, S.; Casscells, W. Influenza infection exerts prominent inflammatory and thrombotic effects on the atherosclerotic plaques of apolipoprotein E-deficient mice. Circulation 2003, 107, 762–768. [Google Scholar] [CrossRef]
- Couser, W.G.; Johnson, R.J. The etiology of glomerulonephritis: Roles of infection and autoimmunity. Kidney Int. 2014, 86, 905–914. [Google Scholar] [CrossRef] [Green Version]
- Sundin, P.O.; Udumyan, R.; Fall, K.; Montgomery, S. Hospital admission with pneumonia and subsequent persistent risk of chronic kidney disease: National cohort study. Clin. Epidemiol. 2018, 10, 971–979. [Google Scholar] [CrossRef] [PubMed]
- Cheikh Hassan, H.I.; Tang, M.; Djurdjev, O.; Langsford, D.; Sood, M.M.; Levin, A. Infection in advanced chronic kidney disease leads to increased risk of cardiovascular events, end-stage kidney disease and mortality. Kidney Int. 2016, 90, 897–904. [Google Scholar] [CrossRef]
- Huang, S.T.; Lin, C.L.; Chang, Y.J.; Sher, Y.P.; Wu, M.J.; Shu, K.H.; Sung, F.C.; Kao, C.H. Pneumococcal pneumonia infection is associated with end-stage renal disease in adult hospitalized patients. Kidney Int. 2014, 86, 1023–1030. [Google Scholar] [CrossRef] [PubMed]
- Ishigami, J.; Cowan, L.T.; Demmer, R.T.; Grams, M.E.; Lutsey, P.L.; Coresh, J.; Matsushita, K. Hospitalization With Major Infection and Incidence of End-Stage Renal Disease: The Atherosclerosis Risk in Communities (ARIC) Study. Mayo Clin. Proc. 2020, 95, 1928–1939. [Google Scholar] [CrossRef] [PubMed]
- Su, G.; Trevisan, M.; Ishigami, J.; Matsushita, K.; Stålsby Lundborg, C.; Carrero, J.J. Short- and long-term outcomes after incident pneumonia in adults with chronic kidney disease: A time-dependent analysis from the Stockholm CREAtinine Measurement project. Nephrol. Dial. Transpl. 2020, 35, 1894–1900. [Google Scholar] [CrossRef]
- Angarita, S.A.K.; Russell, T.A.; Kaldas, F.M. Pneumonia after liver transplantation. Curr. Opin. Organ Transpl. 2017, 22, 328–335. [Google Scholar] [CrossRef]
- Kidney Disease: Improving Global Outcomes (KDIGO) AKI Work Group. KDIGO clinical practice guideline for acute kidney injury. Kidney Int. Suppl. 2012, 2, 1–138. [Google Scholar]
- Ikegami, T.; Shirabe, K.; Matono, R.; Yoshizumi, T.; Soejima, Y.; Uchiyama, H.; Kayashima, H.; Morita, K.; Maehara, Y. Etiologies, risk factors, and outcomes of bacterial pneumonia after living donor liver transplantation. Liver Transpl. 2012, 18, 1060–1068. [Google Scholar] [CrossRef]
- Kakihana, Y.; Ito, T.; Nakahara, M.; Yamaguchi, K.; Yasuda, T. Sepsis-induced myocardial dysfunction: Pathophysiology and management. J. Intensive Care 2016, 4, 22. [Google Scholar] [CrossRef]
- Gnanara, J.F.; von Haehling, S.; Anker, S.D.; Raj, D.S.; Radhakrishnan, J. The relevance of congestion in the cardio-renal syndrome. Kidney Int. 2013, 83, 384–391. [Google Scholar] [CrossRef]
- Markowitz, G.S.; Perazella, M.A. Drug-induced renal failure: A focus on tubulointerstitial disease. Clin. Chim. Acta 2005, 351, 31–47. [Google Scholar] [CrossRef]
- Coca, S.G.; Singanamala, S.; Parikh, C.R. Chronic kidney disease after acute kidney injury: A systematic review and meta-analysis. Kidney Int. 2012, 81, 442–448. [Google Scholar] [CrossRef]
- Kellum, J.A.; Kong, L.; Fink, M.P.; Weissfeld, L.A.; Yealy, D.M.; Pinsky, M.R.; Fine, J.; Krichevsky, A.; Delude, R.L.; Angus, D.C. Understanding the inflammatory cytokine response in pneumonia and sepsis: Results of the Genetic and Inflammatory Markers of Sepsis (GenIMS) Study. Arch. Intern. Med. 2007, 167, 1655–1663. [Google Scholar] [CrossRef] [PubMed]
- Hiramoto, J.S.; Katz, R.; Peralta, C.A.; Ix, J.H.; Fried, L.; Cushman, M.; Siscovick, D.; Palmas, W.; Sarnak, M.; Shlipak, M.G. Inflammation and coagulation markers and kidney function decline: The Multi-Ethnic Study of Atherosclerosis (MESA). Am. J. Kidney Dis. 2012, 60, 225–232. [Google Scholar] [CrossRef] [PubMed]
- Shankar, A.; Sun, L.; Klein, B.E.; Lee, K.E.; Muntner, P.; Javier, F.N.; Tsai, M.Y.; Cruickshanks, K.J.; Schubert, C.R.; Brazy, P.C.; et al. Markers of inflammation predict the long-term risk of developing chronic kidney disease: A population-based cohort study. Kidney Int. 2011, 80, 123. [Google Scholar] [CrossRef] [PubMed]
- Zeisberg, M.; Neilson, E.G. Mechanisms of tubulointerstitial fibrosis. J. Am. Soc. Nephrol. 2010, 21, 1819–1834. [Google Scholar] [CrossRef] [PubMed]
- Fried, L.; Solomon, C.; Shlipak, M.; Seliger, S.; Stehman-Breen, C.; Bleyer, A.J.; Chaves, P.; Furberg, C.; Kuller, L.; Newman, A. Inflammatory and prothrombotic markers and the progression of renal disease in elderly individuals. J. Am. Soc. Nephrol. 2004, 15, 3184–3191. [Google Scholar] [CrossRef] [PubMed]
- Cangemi, R.; Pignatelli, P.; Carnevale, R.; Bartimoccia, S.; Nocella, C.; Falcone, M.; Taliani, G.; Violi, F.; Battaglia, S.; Bertazzoni, G.; et al. Low-grade endotoxemia, gut permeability and platelet activation in community-acquired pneumonia. J. Infect. 2016, 73, 107–114. [Google Scholar] [CrossRef]
- Tunjungputri, R.N.; De Jonge, M.I.; De Greeff, A.; Van Selm, S.; Buys, H.; Harders-Westerveen, J.F.; Stockhofe-Zurwieden, N.; Urbanus, R.T.; De Groot, P.G.; Smith, H.E.; et al. Invasive pneumococcal disease leads to activation and hyperreactivity of platelets. Thromb. Res. 2016, 144, 123–126. [Google Scholar] [CrossRef]
- Kim, D.K.; Hunter, P. Advisory Committee on Immunization Practices recommended immunization schedule for adults aged 19 years or older—United States, 2019. MMWR Morbid Mortal Wkly. Rep. 2019, 68, 115–118. [Google Scholar] [CrossRef]
- Gong, N.; Jia, C.; Huang, H.; Liu, J.; Huang, X.; Wan, Q. Predictors of Mortality During Initial Liver Transplant Hospitalization and Investigation of Causes of Death. Ann. Transpl. 2020, 25, e926020. [Google Scholar] [CrossRef] [PubMed]


| With Infection | Without Infection | p-Value | |
|---|---|---|---|
| Sample size | 102 | 333 | |
| Age (years) | 55.1 ± 8.6 | 54.4 ± 8.3 | 0.456 |
| Gender, male | 68 (66.7%) | 264 (79.3%) | 0.009 * |
| Comorbidity | |||
| CCI | 4.6 ± 4.2 | 3.3 ± 3.3 | 0.001 * |
| DM | 20 (19.6%) | 47 (14.1%) | 0.179 |
| Hypertension | 11 (10.8%) | 33 (9.9%) | 0.798 |
| Hepatitis B | 36 (35.3%) | 119 (35.7%) | 0.935 |
| Hepatitis C | 26 (25.5%) | 74 (22.2%) | 0.493 |
| Cirrhosis | 52 (51%) | 161 (48.3%) | 0.642 |
| CHF | 9 (8.8%) | 21 (6.3%) | 0.380 |
| CAD | 0 (0%) | 5 (1.5%) | 0.213 |
| Lab data at baseline | |||
| BUN (mg/dL) | 19.6 ± 15.6 | 17.2 ± 12.3 | 0.118 |
| Creatinine (mg/dL) | 1.15 ± 0.62 | 1.12 ± 0.74 | 0.733 |
| eGFR (mL/min/1.73 m2) | 76.1 ± 38.6 | 74.9 ± 29.9 | 0.748 |
| Albumin (g/dL) | 2.9 ± 0.8 | 2.9 ± 0.7 | 0.975 |
| AST (U/L) | 177 ± 94.5 | 167.2 ± 95.9 | 0.366 |
| ALT (U/L) | 110 ± 53.3 | 112.1 ± 68.2 | 0.774 |
| PT (second) | 18.4 ± 4.5 | 17.9 ± 4 | 0.287 |
| aPTT (second) | 38.2 ± 8.4 | 38.2 ± 10.2 | 0.953 |
| Platelet (103/μL) | 89.1 ± 39.4 | 82.9 ± 38.9 | 0.167 |
| CRP (mg/dL) | 2.7 ± 4.5 | 0.7 ± 1.9 | <0.001 * |
| Anti-HBs (mIU/mL) | 85 (83.3%) | 266 (79.9%) | 0.439 |
| Average tacrolmius concentration (ng/mL) | 6.32 ± 2.5 | 6.34 ± 2.1 | 0.931 |
| eGFR Decline > 40% | Renal Composite Outcome | |
|---|---|---|
| (A) infection | ||
| Yes | 74 (72.5%) | 80 (78.4%) |
| No | 97 (29.1%) | 111 (33.3%) |
| p value | <0.001 | <0.001 |
| (B) pneumonia | ||
| Yes | 29 (74.4%) | 34 (87.2%) |
| No | 142 (35.9%) | 157 (39.6%) |
| p value | <0.001 | <0.001 |
| eGFR Decline > 40% | Composite Renal Outcomes | |||
|---|---|---|---|---|
| Hazard Ratio (95% CI) | p-Value | Hazard Ratio (95% CI) | p-Value | |
| (A) Infection vs. non-infection | ||||
| Model 1 | 3.51 (2.38–5.17) | <0.001 | 3.69 (2.66–5.13) | <0.001 |
| Model 2 | 3.44 (2.31–5.11) | <0.001 | 3.68 (2.63–5.13) | <0.001 |
| Model 3 | 3.20 (2.13–4.81) | <0.001 | 3.48 (2.48–4.88) | <0.001 |
| Model 4 | 3.32 (2.13–5.16) | <0.001 | 3.41 (2.40–4.86) | <0.001 |
| (B) pneumonia vs. non-pneumonia | ||||
| Model 1 | 2.73 (1.28–5.82) | 0.009 | 5.07 (2.94–8.77) | <0.001 |
| Model 2 | 2.67 (1.25–5.73) | 0.012 | 4.86 (2.80–8.45) | <0.001 |
| Model 3 | 2.24 (1.01–4.97) | 0.047 | 4.17 (2.36–7.38) | <0.001 |
| Model 4 | 2.47 (1.10–5.56) | 0.029 | 4.37 (2.39–8.02) | <0.001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hsu, K.-M.; Lin, P.-R.; Chiu, P.-F.; Hsieh, Y.-P. Infection in Living Donor Liver Transplantation Leads to Increased Risk of Adverse Renal Outcomes. Nutrients 2022, 14, 3660. https://doi.org/10.3390/nu14173660
Hsu K-M, Lin P-R, Chiu P-F, Hsieh Y-P. Infection in Living Donor Liver Transplantation Leads to Increased Risk of Adverse Renal Outcomes. Nutrients. 2022; 14(17):3660. https://doi.org/10.3390/nu14173660
Chicago/Turabian StyleHsu, Kao-Ming, Pei-Ru Lin, Ping-Fang Chiu, and Yao-Peng Hsieh. 2022. "Infection in Living Donor Liver Transplantation Leads to Increased Risk of Adverse Renal Outcomes" Nutrients 14, no. 17: 3660. https://doi.org/10.3390/nu14173660
APA StyleHsu, K.-M., Lin, P.-R., Chiu, P.-F., & Hsieh, Y.-P. (2022). Infection in Living Donor Liver Transplantation Leads to Increased Risk of Adverse Renal Outcomes. Nutrients, 14(17), 3660. https://doi.org/10.3390/nu14173660




