Nootropics as Cognitive Enhancers: Types, Dosage and Side Effects of Smart Drugs
Abstract
1. Introduction
2. What Are Nootropics?
2.1. Mechanisms of Action
2.2. Indications
2.3. Nootropic Treatment
2.4. Use by Students
2.5. Advantages and Disadvantages of Natural vs. Synthetic Nootropics
3. Classical Nootropic Compounds
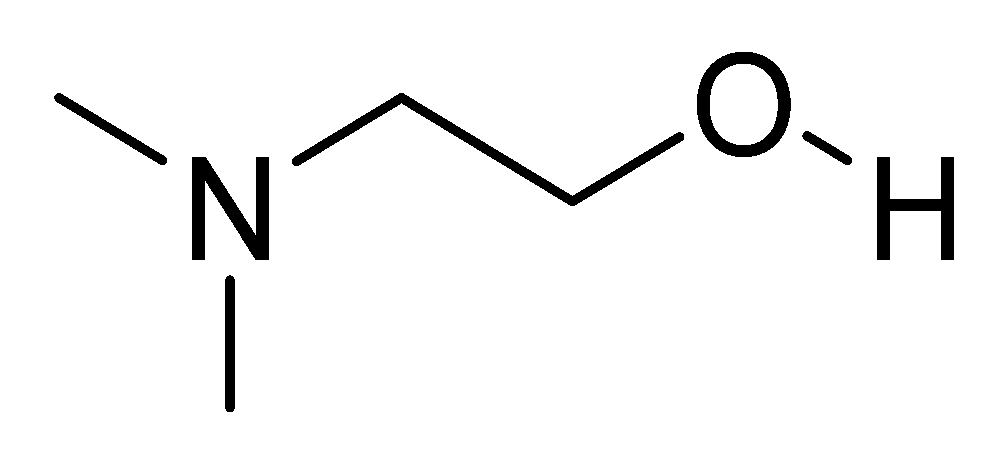
3.1. Deanol (DMAE)
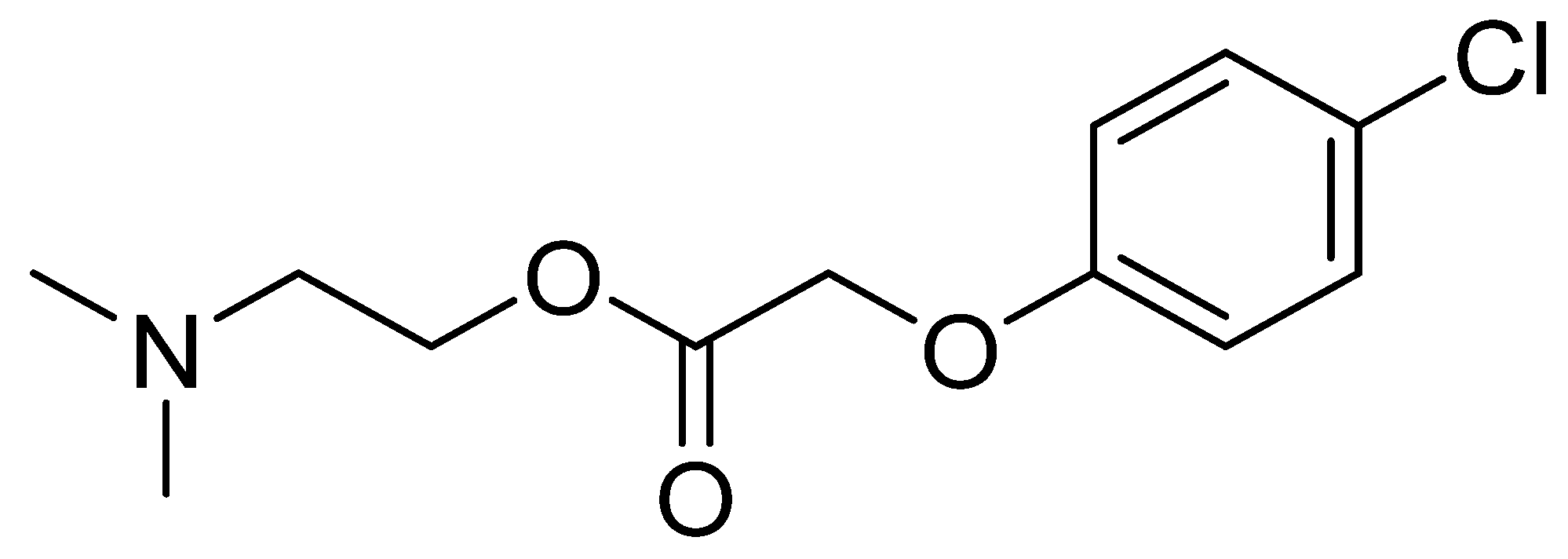
3.2. Meclofenoxate
3.3. Nicergoline
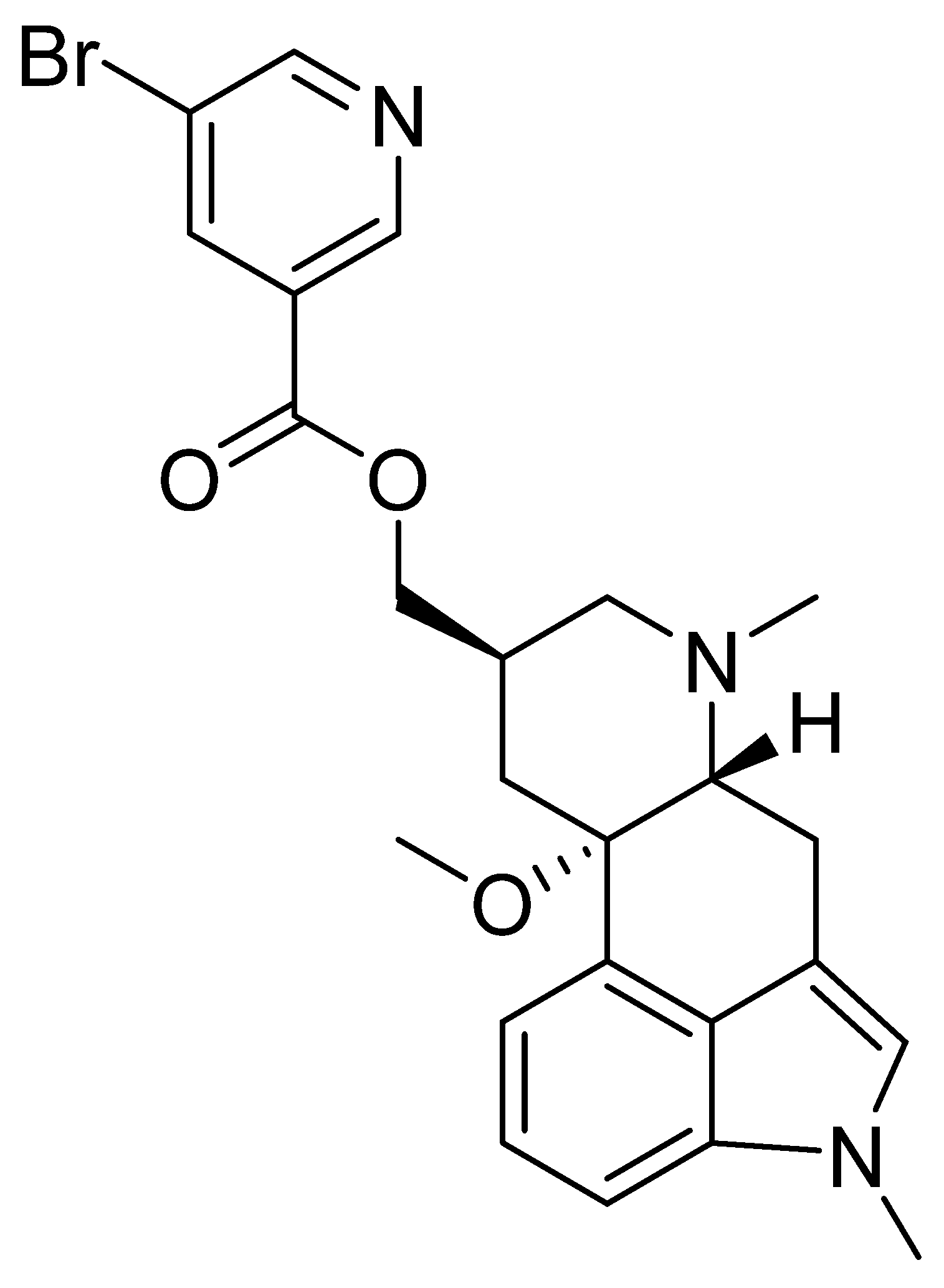
3.4. Piracetam
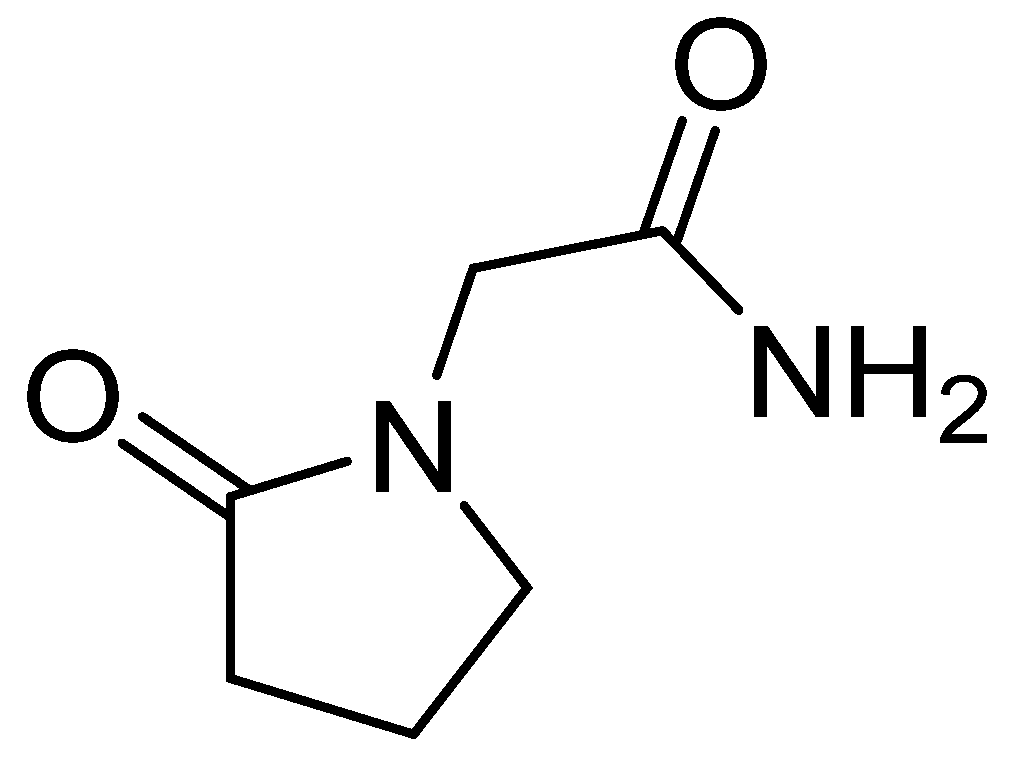
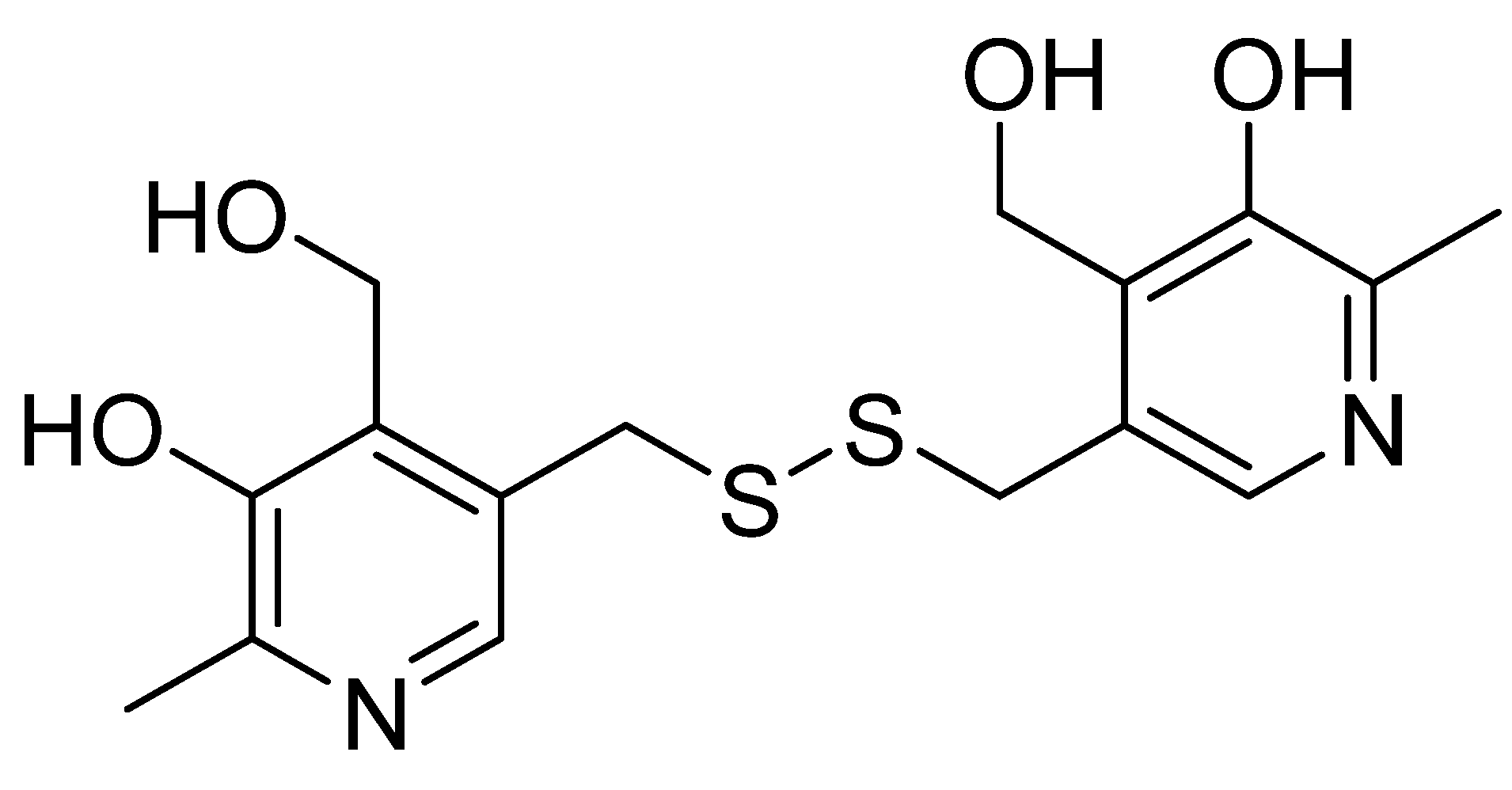
3.5. Pyritinol
4. Substances Increasing Brain Metabolism
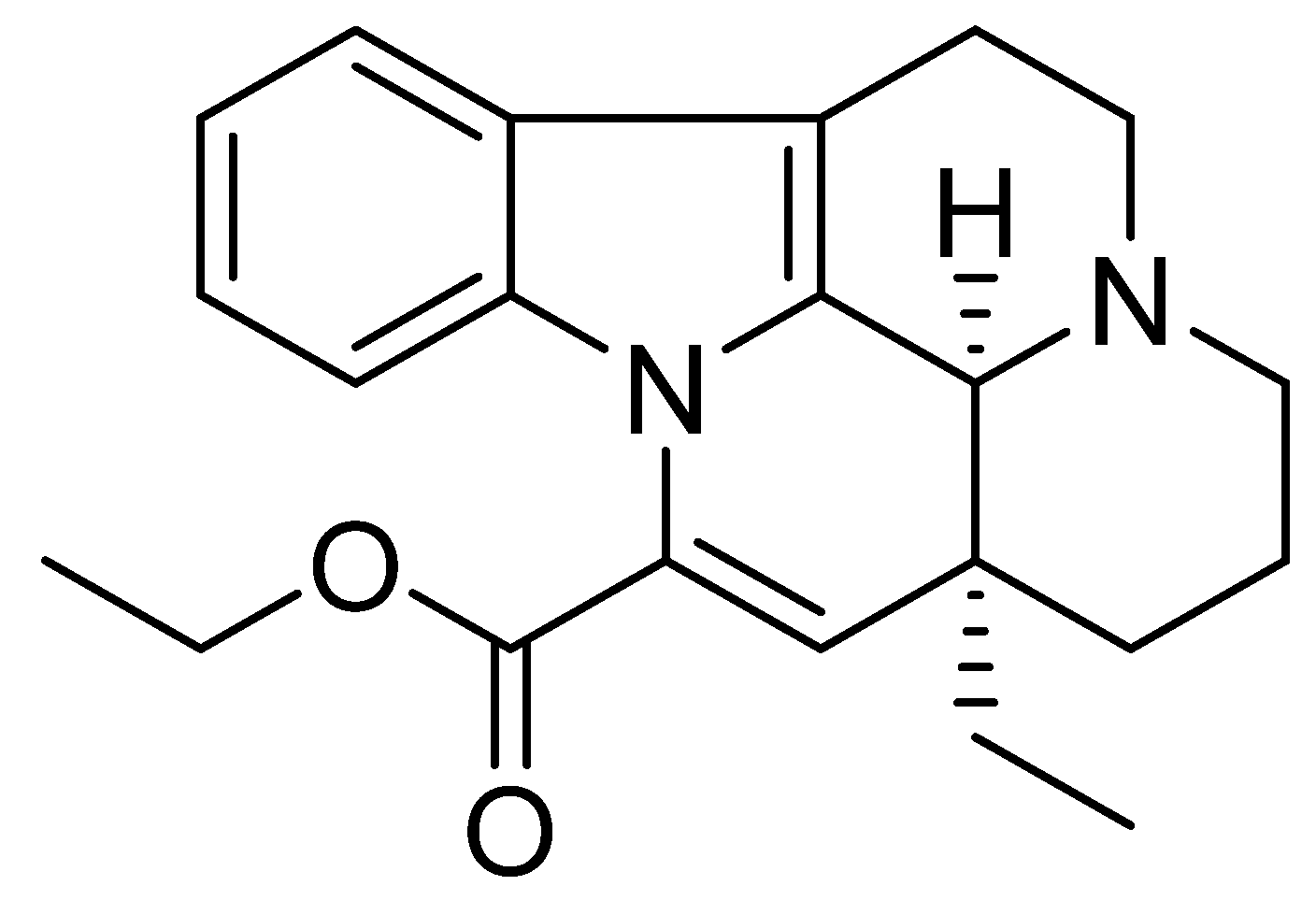
4.1. Vinpocetine
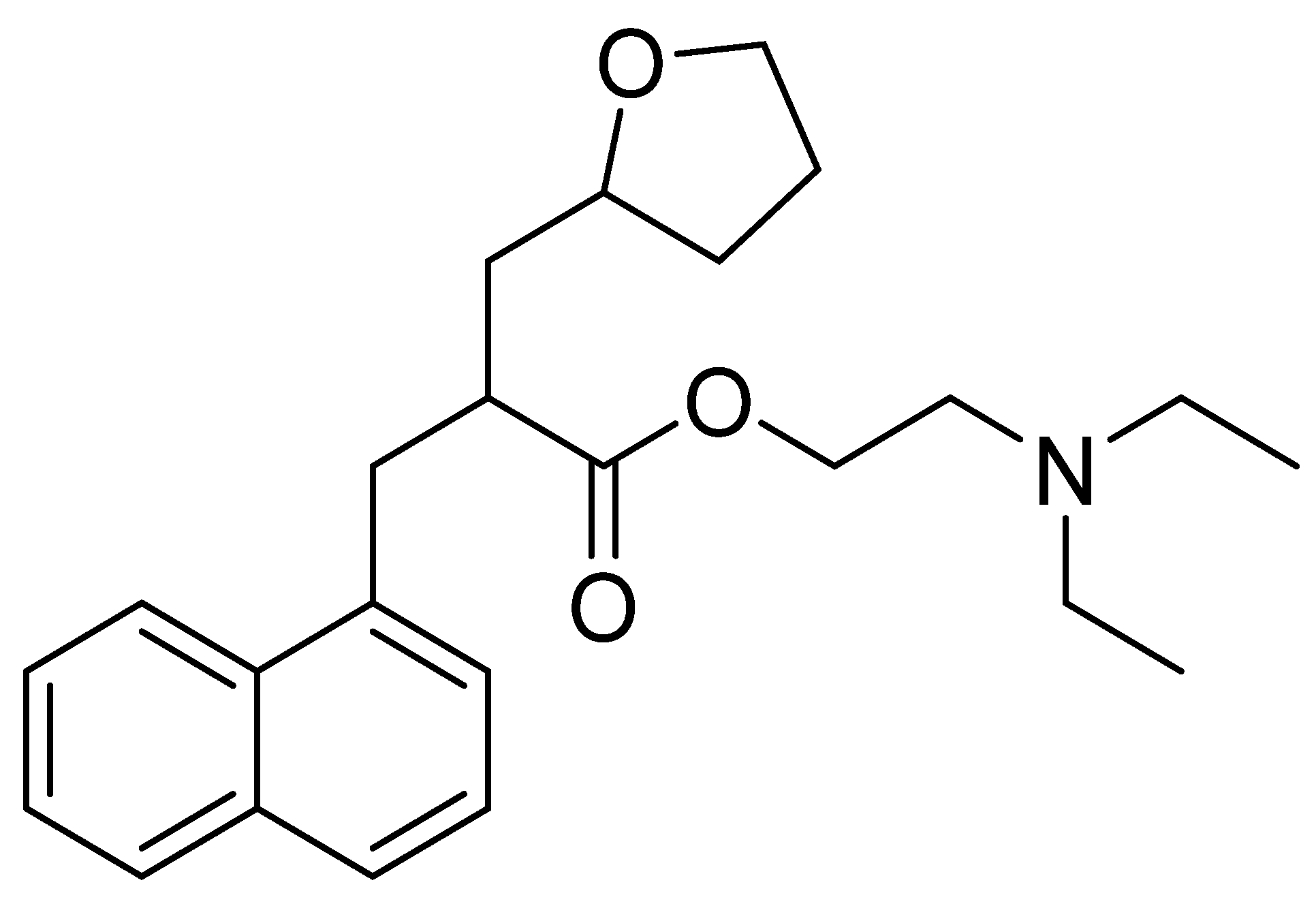
4.2. Naftidrofuryl
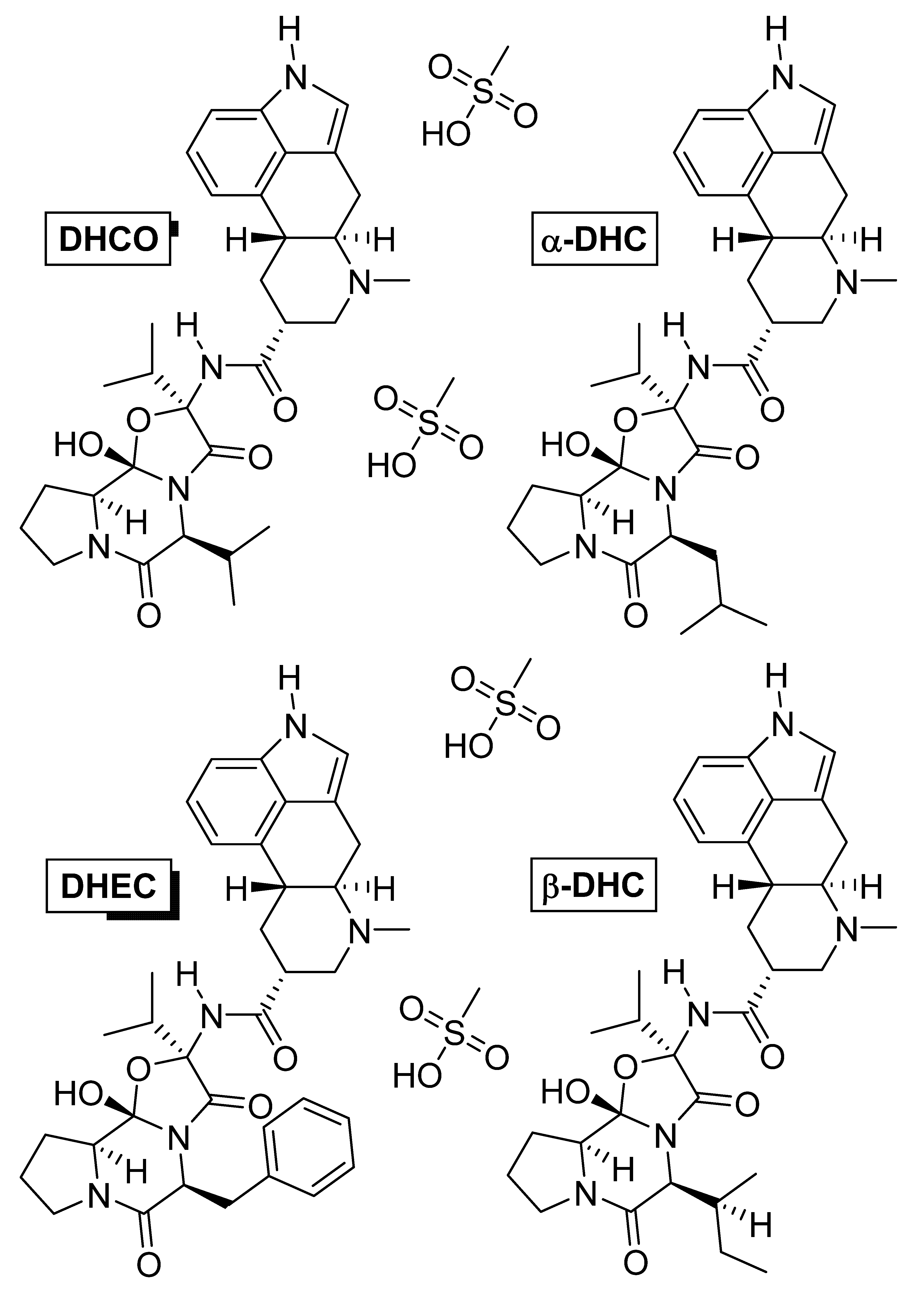
4.3. Dihydroergotoxine
5. Cholinergics
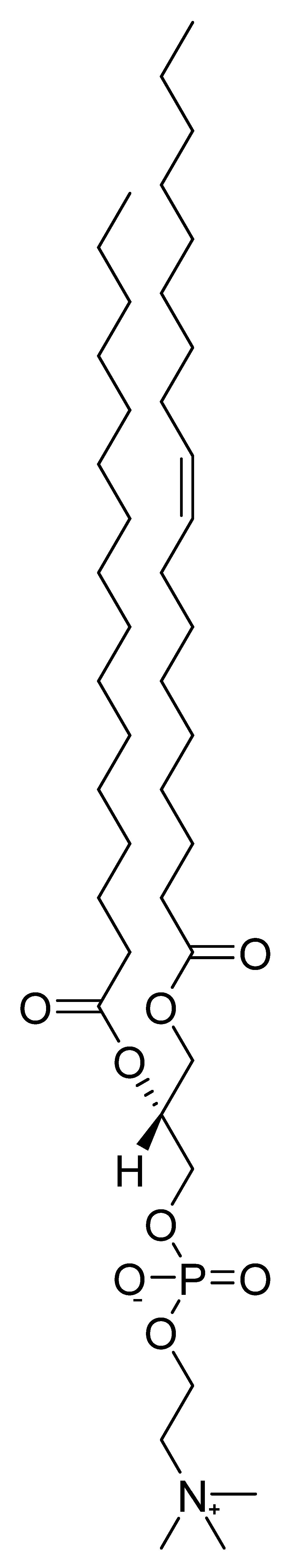
Phosphatidylcholine (Lecithin)
6. Plants and Their Extracts with Nootropic Effects
6.1. Herbal Drug Plant Collection
6.2. Plant Material Processing
| Ref. | Phytochemical Group | Main Active Compounds | Uses and Effects | Botanical Name |
|---|---|---|---|---|
| [178,179,180,181,182] | Terpenoids | Panaxosides (Ginsenosides) | Adaptogen, antioxidant, vasorelaxation | Panax ginseng |
| [183,184,185,186,187] | Ginkgolides | Antioxidant, neuroprotection, vasodilatation | Ginkgo biloba | |
| [188,189,190] | Asiatic acid, centellic acid, madecassic acid, asiaticoside, centelloside, madecassoside, brahmoside | Antioxidant, anxiolytic, nootropic | Centella asiatica | |
| [191,192,193,194] | Withanolides | Antioxidant, increase in red blood cell content, nootropic | Withania somnifera | |
| [195,196,197,198] | Bacosides, bacopasides | Antioxidant, cognitive enhancer, neuroprotectant | Bacopa monnieri | |
| [199,200] | Alkaloids | Methylxanthines | Anxiolytic, nootropic, panicolytic, stimulant | Paullinia cupana |
| [201,202,203] | Polyphenols | Rosavins, salidroside | Adaptogen, antidepressant, antioxidant, anxiolytic, stimulant | Rhodiola rosea |
| [204,205,206] | Schisandra lignans | Antioxidant, neuroprotection | Schisandra chinensis | |
| [207,208,209,210,211] | Diverse 1 | Eleutherosides, ciwujianosides | Antioxidant, memory improvement | Eleutherococcus senticosus |
| [212,213,214] | Macamides, macaenes | Antioxidant, antidepressant, cognitive enhancer | Lepidium meyenii |
6.3. Specific Plant Species
6.3.1. Ginseng (Panax ginseng)
6.3.2. Ginkgo (Ginkgo biloba)
6.3.3. Asiatic Pennywort (Centella asiatica)
6.3.4. Ashwagandha (Withania somnifera)
6.3.5. Water Hyssop (Bacopa monnieri)
6.3.6. Guarana (Paullinia cupana)
6.3.7. Eleuthero (Eleutherococcus senticosus)
6.3.8. Rhodiola (Rhodiola rosea)
6.3.9. Schisandra (Schisandra chinensis)
6.3.10. Maca (Lepidium meyenii)
7. Summary and Recommendations
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Giurgea, C.; Salama, M. Nootropic drugs. Prog. Neuro-Psychopharmacol. 1977, 1, 235–247. [Google Scholar] [CrossRef]
- Schifano, F.; Catalani, V.; Sharif, S.; Napoletano, F.; Corkery, J.M.; Arillotta, D.; Fergus, S.; Vento, A.; Guirguis, A. Benefits and Harms of ‘Smart Drugs’ (Nootropics) in Healthy Individuals. Drugs 2022, 82, 633–647. [Google Scholar] [CrossRef] [PubMed]
- Vyas, S.; Kothari, S.; Kachhwaha, S. Nootropic medicinal plants: Therapeutic alternatives for Alzheimer’s disease. J. Herb. Med. 2019, 17, 100291. [Google Scholar] [CrossRef]
- Ihl, R.; Kretschmar, C. Nootropic drug evaluation for general practice. Nervenarzt 1997, 68, 853–861. [Google Scholar] [CrossRef]
- Chaudhari, K.S.; Tiwari, N.R.; Tiwari, R.R.; Sharma, R.S. Neurocognitive Effect of Nootropic Drug Brahmi (Bacopa monnieri) in Alzheimer’s Disease. Ann. Neurosci. 2017, 24, 111–122. [Google Scholar] [CrossRef]
- Benninghoff, J.; Perneczky, R. Anti-Dementia Medications and Anti-Alzheimer’s Disease Drugs: Side Effects, Contraindications, and Interactions. In NeuroPsychopharmacotherapy; Riederer, P., Laux, G., Nagatsu, T., Le, W., Riederer, C., Eds.; Springer International Publishing: Cham, Switzerland, 2022; pp. 1–10. [Google Scholar] [CrossRef]
- Dormehl, I.C.; Jordaan, B.; Oliver, D.W.; Croft, S. SPECT monitoring of improved cerebral blood flow during long-term treatment of elderly patients with nootropic drugs. Clin. Nucl. Med. 1999, 24, 29–34. [Google Scholar] [CrossRef] [PubMed]
- Napoletano, F.; Schifano, F.; Corkery, J.M.; Guirguis, A.; Arillotta, D.; Zangani, C.; Vento, A. The Psychonauts’ World of Cognitive Enhancers. Front. Psychiatry 2020, 11, 546796. [Google Scholar] [CrossRef]
- Malik, R.; Sangwan, A.; Saihgal, R.; Paul Jindal, D.; Piplani, P. Towards better brain management: Nootropics. Curr. Med. Chem. 2007, 14, 123–131. [Google Scholar] [CrossRef]
- Giurgea, C. The “nootropic” approach to the pharmacology of the integrative activity of the brain 1, 2. Integr. Psychol. Behav. Sci. 1973, 8, 108–115. [Google Scholar] [CrossRef]
- Giurgea, C. Pharmacology of integrative activity of the brain. Attempt at nootropic concept in psychopharmacology. Actual. Pharm. 1972, 25, 115–156. [Google Scholar]
- Zhao, X.; Yeh, J.Z.; Narahashi, T. Post-Stroke Dementia: Nootropic Drug Modulation of Neuronal Nicotinic Acetylcholine Receptors. Ann. N. Y. Acad. Sci. 2001, 939, 179–186. [Google Scholar] [CrossRef] [PubMed]
- Zhao, X.; Kuryatov, A.; Lindstrom, J.M.; Yeh, J.Z.; Narahashi, T. Nootropic Drug Modulation of Neuronal Nicotinic Acetylcholine Receptors in Rat Cortical Neurons. Mol. Pharmacol. 2001, 59, 674–683. [Google Scholar] [CrossRef] [PubMed]
- Suliman, N.A.; Mat Taib, C.N.; Mohd Moklas, M.A.; Adenan, M.I.; Hidayat Baharuldin, M.T.; Basir, R. Establishing Natural Nootropics: Recent Molecular Enhancement Influenced by Natural Nootropic. Evid.-Based Complement. Altern. Med. 2016, 2016, 4391375. [Google Scholar] [CrossRef] [PubMed]
- Froestl, W.; Muhs, A.; Pfeifer, A. Cognitive enhancers (nootropics). Part 1: Drugs interacting with receptors. J. Alzheimer’s Dis. 2012, 32, 793–887. [Google Scholar] [CrossRef]
- Mali, A.; Shenoy, P.; Bandawane, D.; Nipate, S.; Chaudhari, P. Screening of nootropics: An overview on preclinical evaluation techniques. Int. J. Pharm. 2012, 2, 159–180. [Google Scholar]
- Joshi Pranav, C. A review on natural memory enhancers (Nootropics). Unique J. Eng. Adv. Sci. 2013, 1, 8–18. [Google Scholar]
- Chekman, I.; Belenichev, I.; Demchenko, A.; Bobrova, V.; Kucherenko, L.; Gorchakova, N.; Bukhtiyarova, N. Nootropics in comlex therapy of chronic cerebral ischemia. Sci. Innov. 2014, 10, 56–68. [Google Scholar] [CrossRef]
- McDaniel, M.A.; Maier, S.F.; Einstein, G.O. “Brain-specific” nutrients: A memory cure? Nutrition 2003, 19, 957–975. [Google Scholar] [CrossRef]
- Ishchenko, M.M.; Ostrovskaia, O.S. The effect of combined drug treatment on rheologic properties of the blood in patients with disordered circulatory encephalopathy. Vrachebnoe Delo 1990, 3, 58–60. [Google Scholar]
- Nicholson, C.D. Pharmacology of nootropics and metabolically active compounds in relation to their use in dementia. Psychopharmacology 1990, 101, 147–159. [Google Scholar] [CrossRef]
- Pepeu, G.; Spignoli, G. Nootropic drugs and brain cholinergic mechanisms. Prog. Neuropsychopharmacol. Biol. Psychiatry 1989, 13, S77–S88. [Google Scholar] [CrossRef]
- Rainer, M.; Mucke, H.A.; Chwatal, K.; Havelec, L. Alcohol-induced organic cerebral psychosyndromes: Partial reversal of cognitive impairments assisted by dihydroergocristine. Psychopharmacology 1996, 127, 365–369. [Google Scholar] [CrossRef]
- Benešová, O. Neuropathobiology of senile dementia and mechanism of action of nootropic drugs. Drugs Aging 1994, 4, 285–303. [Google Scholar] [CrossRef] [PubMed]
- Wu, C.-Y.; Hu, H.-Y.; Chow, L.-H.; Chou, Y.-J.; Huang, N.; Wang, P.-N.; Li, C.-P. The effects of anti-dementia and nootropic treatments on the mortality of patients with dementia: A population-based cohort study in Taiwan. PLoS ONE 2015, 10, e0130993. [Google Scholar] [CrossRef] [PubMed]
- Finney-Brown, T. Schisandra, Rhodiola and Eleuthrococcus as nootropic agents. Aust. J. Herb. Med. 2010, 22, 64–65. [Google Scholar]
- Panossian, A.; Wikman, G. Effects of Adaptogens on the Central Nervous System and the Molecular Mechanisms Associated with Their Stress—Protective Activity. Pharmaceuticals 2010, 3, 188–224. [Google Scholar] [CrossRef]
- Zavadenko, N.; NIu, S.; Rumiantseva, M.; Ovchinnikova, A. The use of instenon in children with minimal brain dysfunction. Zhurnal Nevrol. Psikhiatrii Im. SS Korsakova 2002, 102, 29–35. [Google Scholar]
- Colucci, L.; Bosco, M.; Ziello, A.R.; Rea, R.; Amenta, F.; Fasanaro, A.M. Effectiveness of nootropic drugs with cholinergic activity in treatment of cognitive deficit: A review. J. Exp. Pharmacol. 2012, 4, 163–172. [Google Scholar] [CrossRef]
- Zokiriv, M. Correction of cognitive impairments in patients with HIV-associated encephalopathy. J. Theor. Appl. Sci. 2021, 7, 62–66. [Google Scholar] [CrossRef]
- Kupats, E.; Vrublevska, J.; Zvejniece, B.; Vavers, E.; Stelfa, G.; Zvejniece, L.; Dambrova, M. Safety and tolerability of the anxiolytic and nootropic drug phenibut: A systematic review of clinical trials and case reports. Pharmacopsychiatry 2020, 53, 201–208. [Google Scholar] [CrossRef]
- Voronina, T.A. Nootropic drugs in Alzheimer disease treatment. New pharmacological strategies. In Alzheimer Disease; Springer: Berlin/Heidelberg, Germany, 1994; pp. 265–269. [Google Scholar]
- Noorbala, A.; Akhondzadeh, S.; Davari-Ashtiani, R.; Amini-Nooshabadi, H. Piracetam in the treatment of schizophrenia: Implications for the glutamate hypothesis of schizophrenia. J. Clin. Pharm. Ther. 1999, 24, 369–374. [Google Scholar] [CrossRef] [PubMed]
- Sukhotina, N.; Konovalova, V.; Kryzhanovskaia, I.; Kupriianova, T. Efficacy of pantogam in the treatment of hyperkinetic disorders in children. Zhurnal Nevrol. Psikhiatrii Im. SS Korsakova 2010, 110, 24–28. [Google Scholar]
- Sarris, J.; Kean, J.; Schweitzer, I.; Lake, J. Complementary medicines (herbal and nutritional products) in the treatment of Attention Deficit Hyperactivity Disorder (ADHD): A systematic review of the evidence. Complement. Ther. Med. 2011, 19, 216–227. [Google Scholar] [CrossRef] [PubMed]
- Teasdale, G.; Jennett, B. Assessment of Coma and Impaired Consciousness: A Practical Scale. Lancet 1974, 304, 81–84. [Google Scholar] [CrossRef]
- Canterbury, R.J.; Lloyd, E. Smart drugs: Implications of student use. J. Prim. Prev. 1994, 14, 197–207. [Google Scholar] [CrossRef] [PubMed]
- Wagner, H.; Ulrich-Merzenich, G. Synergy research: Approaching a new generation of phytopharmaceuticals. Phytomedicine 2009, 16, 97–110. [Google Scholar] [CrossRef]
- Caesar, L.K.; Cech, N.B. Synergy and antagonism in natural product extracts: When 1 + 1 does not equal 2. Nat. Prod. Rep. 2019, 36, 869–888. [Google Scholar] [CrossRef]
- Balunas, M.J.; Kinghorn, A.D. Drug discovery from medicinal plants. Life Sci. 2005, 78, 431–441. [Google Scholar] [CrossRef]
- Petrovska, B.B. Historical review of medicinal plants’ usage. Pharmacogn. Rev. 2012, 6, 1–5. [Google Scholar] [CrossRef]
- Malykh, A.G.; Sadaie, M.R. Piracetam and Piracetam-Like Drugs. Drugs 2010, 70, 287–312. [Google Scholar] [CrossRef]
- Chary, M.; Yi, D.; Manini, A.F. Candyflipping and Other Combinations: Identifying Drug–Drug Combinations from an Online Forum. Front. Psychiatry 2018, 9, 135. [Google Scholar] [CrossRef] [PubMed]
- Elks, J. The Dictionary of Drugs: Chemical Data: Chemical Data, Structures and Bibliographies; Springer: Berlin/Heidelberg, Germany, 2014. [Google Scholar]
- Malanga, G.; Aguiar, M.B.; Martinez, H.D.; Puntarulo, S. New insights on dimethylaminoethanol (DMAE) features as a free radical scavenger. Drug Metab. Lett. 2012, 6, 54–59. [Google Scholar] [CrossRef]
- Blin, O.; Audebert, C.; Pitel, S.; Kaladjian, A.; Casse-Perrot, C.; Zaim, M.; Micallef, J.; Tisne-Versailles, J.; Sokoloff, P.; Chopin, P.; et al. Effects of dimethylaminoethanol pyroglutamate (DMAE p-Glu) against memory deficits induced by scopolamine: Evidence from preclinical and clinical studies. Psychopharmacology 2009, 207, 201–212. [Google Scholar] [CrossRef] [PubMed]
- Levin, E.D.; Rose, J.E.; Abood, L. Effects of nicotinic dimethylaminoethyl esters on working memory performance of rats in the radial-arm maze. Pharmacol. Biochem. Behav. 1995, 51, 369–373. [Google Scholar] [CrossRef]
- Dimpfel, W.; Wedekind, W.; Keplinger, I. Efficacy of dimethylaminoethanol (DMAE) containing vitamin-mineral drug combination on EEG patterns in the presence of different emotional states. Eur. J. Med. Res. 2003, 8, 183–191. [Google Scholar]
- Sergio, W. Use of DMAE (2-dimethylaminoethanol) in the induction of lucid dreams. Med. Hypotheses 1988, 26, 255–257. [Google Scholar] [CrossRef]
- Baumgaertel, A. Alternative and Controversial Treatments for Attention-Deficit/Hyperactivity Disorder. Pediatr. Clin. N. Am. 1999, 46, 977–992. [Google Scholar] [CrossRef]
- Lewis, J.A.; Young, R. Deanol and methylphenidate in minimal brain dysfunction. Clin. Pharm. Therap. 1975, 17, 534–540. [Google Scholar] [CrossRef]
- Casey, D.E. Mood alterations during deanol therapy. Psychopharmacology 1979, 62, 187–191. [Google Scholar] [CrossRef]
- Ferris, S.H.; Sathananthan, G.; Gershon, S.; Clark, C. Senile Dementia: Treatment with Deanol. J. Am. Geriatr. Soc. 1977, 25, 241–244. [Google Scholar] [CrossRef]
- Wood, P.L.; Péloquin, A. Increases in choline levels in rat brain elicited by meclofenoxate. Neuropharmacology 1982, 21, 349–354. [Google Scholar] [CrossRef]
- Liao, Y.; Wang, R.; Tang, X.-C. Centrophenoxine improves chronic cerebral ischemia induced cognitive deficit and neuronal degeneration in rats. Acta Pharmacol. Sin. 2004, 25, 1590–1596. [Google Scholar] [PubMed]
- Bakhtogarimov, I.R.; Kudryavtseva, A.V.; Krasnov, G.S.; Gladysh, N.S.; Volodin, V.V.; Kudryavtsev, A.A.; Bulavkina, E.V.; Goncharova, M.A.; Ledyaeva, V.S.; Pastukhov, I.S.; et al. The Effect of Meclofenoxate on the Transcriptome of Aging Brain of Nothobranchius guentheri Annual Killifish. Int. J. Mol. Sci. 2022, 23, 2491. [Google Scholar] [CrossRef] [PubMed]
- Marcer, D.; Hopkins, S.M. The Differential Effects of Meclofenoxate on Memory Loss in the Elderly. Age Ageing 1977, 6, 123–131. [Google Scholar] [CrossRef]
- Izumi, K.; Tominaga, H.; Koja, T.; Nomoto, M.; Shimizu, T.; Sonoda, H.; Imamura, K.; Igata, A.; Fukuda, T. Meclofenoxate therapy in tardive dyskinesia: A preliminary report. Biol. Psychiatry 1986, 21, 151–160. [Google Scholar] [CrossRef]
- Popa, R.; Schneider, F.; Mihalas, G.; Stefaniga, P.; Mihalas, I.G.; Maties, R.; Mateescu, R. Antagonic-stress superiority versus meclofenoxate in gerontopsychiatry (alzheimer type dementia). Arch. Gerontol. Geriatr. 1994, 19, 197–206. [Google Scholar] [CrossRef]
- Oliver, J.E.; Restell, M. Serial Testing in Assessing the Effect of Meclofenoxate on Patients with Memory Defects. Br. J. Psychiatry 1967, 113, 219–222. [Google Scholar] [CrossRef]
- Winblad, B.; Fioravanti, M.; Dolezal, T.; Logina, I.; Milanov, I.G.; Popescu, D.C.; Solomon, A. Therapeutic Use of Nicergoline. Clin. Drug Investig. 2008, 28, 533–552. [Google Scholar] [CrossRef]
- Winblad, B.; Carfagna, N.; Bonura, L.; Rossini, B.M.; Wong, E.H.F.; Battaglia, A. Nicergoline in Dementia. CNS Drugs 2000, 14, 267–287. [Google Scholar] [CrossRef]
- Caraci, F.; Chisari, M.; Frasca, G.; Canonico, P.L.; Battaglia, A.; Calafiore, M.; Battaglia, G.; Bosco, P.; Nicoletti, F.; Copani, A.; et al. Nicergoline, a drug used for age-dependent cognitive impairment, protects cultured neurons against β-amyloid toxicity. Brain Res. 2005, 1047, 30–37. [Google Scholar] [CrossRef]
- Giardino, L.; Giuliani, A.; Battaglia, A.; Carfagna, N.; Aloe, L.; Calzà, L. Neuroprotection and aging of the cholinergic system: A role for the ergoline derivative nicergoline (Sermion®). Neuroscience 2002, 109, 487–497. [Google Scholar] [CrossRef]
- Heitz, C.; Descombes, J.-J.; Miller, R.C.; Stoclet, J.-C. α-adrenoceptor antagonistic and calcium antagonistic effects of nicergoline in the rat isolated aorta. Eur. J. Pharmacol. 1986, 123, 279–285. [Google Scholar] [CrossRef]
- Molteni, A.; Nickerson, P.A.; Brownie, A.C.; Liu, K. Effect on an ergoline derivate-nicergoline (Sermion) on methylandrostenediol-induced hypertension in the rat. Arch. Int. Pharmacodyn. Ther. 1980, 247, 119–134. [Google Scholar] [PubMed]
- Tanaka, M.; Yoshida, T.; Okamoto, K.; Hirai, S. Antioxidant properties of nicergoline; inhibition of brain auto-oxidation and superoxide production of neutrophils in rats. Neurosci. Lett. 1998, 248, 68–72. [Google Scholar] [CrossRef]
- Zang, G.; Fang, L.; Chen, L.; Wang, C. Ameliorative effect of nicergoline on cognitive function through the PI3K/AKT signaling pathway in mouse models of Alzheimer’s disease. Mol. Med. Rep. 2018, 17, 7293–7300. [Google Scholar] [CrossRef] [PubMed]
- Iliff, L.D.; Boulay, G.H.D.; Marshall, J.; Russell, R.W.R.; Symon, L. Effect of nicergoline on cerebral blood flow. J. Neurol. Neurosurg. Psychiatry 1977, 40, 746–747. [Google Scholar] [CrossRef][Green Version]
- Baskys, A.; Hou, A.C. Vascular dementia: Pharmacological treatment approaches and perspectives. Clin. Interv. Aging 2007, 2, 327–335. [Google Scholar] [CrossRef]
- Kuznetsov, V. The influence of nicergoline on cerebral, systemic and cardiac hemodynamics in patients who have had an ischemic stroke. Ageing Long 2021, 2, 32–41. [Google Scholar] [CrossRef]
- Saletu, B.; Paulus, E.; Linzmayer, L.; Anderer, P.; Semlitsch, H.V.; Grünberger, J.; Wicke, L.; Neuhold, A.; Podreka, I. Nicergoline in senile dementia of alzheimer type and multi-infarct dementia: A double-blind, placebo-controlled, clinical and EEG/ERP mapping study. Psychopharmacology 1995, 117, 385–395. [Google Scholar] [CrossRef]
- Fioravanti, M.; Nakashima, T.; Xu, J.; Garg, A. A systematic review and meta-analysis assessing adverse event profile and tolerability of nicergoline. BMJ Open 2014, 4, e005090. [Google Scholar] [CrossRef]
- Klamkam, P.; Pagcharoenpol, R.; Treesaranuwattana, T.; Silpsrikul, P.; Jaruchinda, P.; Wasuwat, P.; Suwannahitatorn, P. A clinical trial of nicergoline to prevent temporary threshold shift. Laryngoscope Investig. Otolaryngol. 2022, 7, 515–522. [Google Scholar] [CrossRef] [PubMed]
- Gouliaev, A.H.; Senning, A. Piracetam and other structurally related nootropics. Brain Res. Rev. 1994, 19, 180–222. [Google Scholar] [CrossRef]
- Stoll, L.; Schubert, T.; Müller, W.E. Age-related deficits of central muscarinic cholinergic receptor function in the mouse: Partial restoration by chronic piracetam treatment. Neurobiol. Aging 1992, 13, 39–44. [Google Scholar] [CrossRef]
- Scheuer, K.; Rostock, A.; Bartsch, R.; Müller, W. Piracetam improves cognitive performance by restoring neurochemical deficits of the aged rat brain. Pharmacopsychiatry 1999, 32, 10–16. [Google Scholar] [CrossRef] [PubMed]
- Nickolson, V.J.; Wolthuis, O.L. Effect of the acquisition-enhancing drug ptracetam on rat cerebral energy metabolism. Comparison with naftidrofuryl and methamphetamine. Biochem. Pharmacol. 1976, 25, 2241–2244. [Google Scholar] [CrossRef]
- Tacconi, M.T.; Wurtman, R.J. Piracetam: Physiological disposition and mechanism of action. Adv. Neurol. 1986, 43, 675–685. [Google Scholar]
- Grau, M.; Montero, J.L.; Balasch, J. Effect of piracetam on electrocorticogram and local cerebral glucose utilization in the rat. Vasc. Pharmacol. 1987, 18, 205–211. [Google Scholar] [CrossRef]
- Brandao, F.; Paula-Barbosa, M.M.; Cadete-Leite, A. Piracetam impedes hippocampal neuronal loss during withdrawal after chronic alcohol intake. Alcohol 1995, 12, 279–288. [Google Scholar] [CrossRef]
- Brandão, F.; Cadete-Leite, A.; Andrade, J.P.; Madeira, M.D.; Paula-Barbosa, M.M. Piracetam promotes mossy fiber synaptic reorganization in rats withdrawn from alcohol. Alcohol 1996, 13, 239–249. [Google Scholar] [CrossRef]
- Winnicka, K.; Tomasiak, M.; Bielawska, A. Piracetam-an old drug with novel properties. Acta Pol. Pharm. 2005, 62, 405–409. [Google Scholar]
- Müller, W.; Eckert, G.; Eckert, A. Piracetam: Novelty in a unique mode of action. Pharmacopsychiatry 1999, 32, 2–9. [Google Scholar] [CrossRef] [PubMed]
- Wilsher, C.R.; Bennett, D.; Chase, C.H.; Conners, C.K.; Diianni, M.; Feagans, L.; Hanvik, L.J.; Helfgott, E.; Koplewicz, H.; Overby, P. Piracetam and dyslexia: Effects on reading tests. J. Clin. Psychopharmacol. 1987, 7, 230–237. [Google Scholar] [CrossRef] [PubMed]
- Croisile, B.; Trillet, M.; Fondarai, J.; Laurent, B.; Mauguière, F.; Billardon, M. Long-term and high-dose piracetam treatment of Alzheimer’s disease. Neurology 1993, 43, 301. [Google Scholar] [CrossRef] [PubMed]
- Growdon, J.H.; Corkin, S.; Huff, F.J.; Rosen, T.J. Piracetam combined with lecithin in the treatment of Alzheimer’s disease. Neurobiol. Aging 1986, 7, 269–276. [Google Scholar] [CrossRef]
- Tanaka, H.; Yamazaki, K.; Hirata, K. Effects of nootropic drugs for demented patients—A study using LORETA. Int. Congr. Ser. 2002, 1232, 605–611. [Google Scholar] [CrossRef]
- Winblad, B. Piracetam: A Review of Pharmacological Properties and Clinical Uses. CNS Drug Rev. 2005, 11, 169–182. [Google Scholar] [CrossRef]
- Singh, A.; Purohit, V. A critical review of pyritinol. Drugs Ther. Perspect. 2019, 35, 278–282. [Google Scholar] [CrossRef]
- Wojszel, Z.B. Nootropics (Piracetam, Pyritinol, Co-dergocrine, Meclophenoxat, Pentoxifylline, Nimodipine). In NeuroPsychopharmacotherapy; Riederer, P., Laux, G., Nagatsu, T., Le, W., Riederer, C., Eds.; Springer International Publishing: Cham, Switzerland, 2020; pp. 1–45. [Google Scholar] [CrossRef]
- Toledano, A.; Bentura, M.L. Pyritinol facilitates the recovery of cortical cholinergic deficits caused by nucleus basalis lesions. J. Neural Transm. Gen. Sect. 1994, 7, 195–209. [Google Scholar] [CrossRef]
- Martin, K.J.; Vyas, S. Increase in acetylcholine concentrations in the brain of ‘old’ rats following treatment with pyrithioxin (Encephabol). Br. J. Pharmacol. 1987, 90, 561–565. [Google Scholar] [CrossRef]
- Jiménez-Andrade, G.Y.; Reyes-García, G.; Sereno, G.; Ceballos-Reyes, G.; Vidal-Cantú, G.C.; Granados-Soto, V. Pyritinol reduces nociception and oxidative stress in diabetic rats. Eur. J. Pharmacol. 2008, 590, 170–176. [Google Scholar] [CrossRef]
- Magnusson, K.; Brim, B.; Das, S. Selective vulnerabilities of N-methyl-D-aspartate (NMDA) receptors during brain aging. Front. Aging Neurosci. 2010, 2, 11. [Google Scholar] [CrossRef] [PubMed]
- Jaiswal, A.K.; Upadhyay, S.N.; Bhattacharya, S.K. Effect of pyritinol, a cerebral protector, on learning and memory deficits induced by prenatal undernutrition and environmental impoverishment in young rats. Indian J. Exp. Biol. 1990, 28, 609–615. [Google Scholar] [PubMed]
- Hindmarch, I.; Coleston, D.M.; Kerr, J.S. Psychopharmacological Effects of Pyritinol in Normal Volunteers. Neuropsychobiology 1990, 24, 159–164. [Google Scholar] [CrossRef] [PubMed]
- Alkuraishy, H.M.; Al-Gareeb, A.I.; Albuhadilly, A.K. Vinpocetine and Pyritinol: A New Model for Blood Rheological Modulation in Cerebrovascular Disorders—A Randomized Controlled Clinical Study. Biomed. Res. Int. 2014, 2014, 324307. [Google Scholar] [CrossRef]
- Nachbar, F.; Korting, H.C.; Vogl, T. Erythema multiforme-like Eruption in Association with Severe Headache following Pyritinol. Dermatology 1993, 187, 42–46. [Google Scholar] [CrossRef]
- Straumann, A.; Bauer, M.; Pichler, W.J.; Pirovino, M. Acute pancreatitis due to pyritinol: An immune-mediated phenomenon. Gastroenterology 1998, 115, 452–454. [Google Scholar] [CrossRef]
- Leopold, M. Pyritinol. In Meyler’s Side Effects of Drugs, 16th ed.; Aronson, J.K., Ed.; Elsevier: Oxford, UK, 2016; pp. 1067–1068. [Google Scholar] [CrossRef]
- Barradell, L.B.; Brogden, R.N. Oral Naftidrofuryl. Drugs Aging 1996, 8, 299–322. [Google Scholar] [CrossRef]
- Goldsmith, D.R.; Wellington, K. Naftidrofuryl. Drugs Aging 2005, 22, 967–977. [Google Scholar] [CrossRef]
- Kiss, B.; Kárpáti, E. Mechanism of action of vinpocetine. Acta Pharm. Hung. 1996, 66, 213–224. [Google Scholar]
- Dubey, A.; Kumar, N.; Mishra, A.; Singh, Y.; Tiwari, M. Review on Vinpocetine. Int. J. Pharm. Life Sci. 2020, 11, 6590–6597. [Google Scholar]
- Sharma, N.; Sharma, V.K.; Manikyam, H.K.; Krishna, A.B. Ergot alkaloids: A review on therapeutic applications. Eur. J. Med. Plants 2016, 14, 1–17. [Google Scholar] [CrossRef]
- Lörincz, C.; Szász, K.; Kisfaludy, L. The synthesis of ethyl apovincaminate. Arzneimittelforschung 1976, 26, 1907. [Google Scholar]
- Hagiwara, M.; Endo, T.; Hidaka, H. Effects of vinpocetine on cyclic nucleotide metabolism in vascular smooth muscle. Biochem. Pharmacol. 1984, 33, 453–457. [Google Scholar] [CrossRef]
- Molnár, P.; Erdő, S.L. Vinpocetine is as potent as phenytoin to block voltage-gated Na+ channels in rat cortical neurons. Eur. J. Pharmacol. 1995, 273, 303–306. [Google Scholar] [CrossRef]
- Erdõ, S.L.; Molnár, P.; Lakics, V.; Bence, J.Z.; Tömösközi, Z. Vincamine and vincanol are potent blockers of voltage-gated Na+ channels. Eur. J. Pharmacol. 1996, 314, 69–73. [Google Scholar] [CrossRef]
- Chiu, P.J.S.; Tetzloff, G.; Ahn, H.-S.; Sybertz, E.J. Comparative Effects of Vinpocetine and 8-Br-Cyclic GMP on the Contraction and 45Ca-Fluxes in the Rabbit Aorta. Am. J. Hypertens. 1988, 1, 262–268. [Google Scholar] [CrossRef]
- Milusheva, E.; Sperlágh, B.; Kiss, B.; Szporny, L.; Pásztor, E.; Papasova, M.; Vizi, E.S. Inhibitory effect of hypoxic condition on acetylcholine release is partly due to the effect of adenosine released from the tissue. Brain Res. Bull. 1990, 24, 369–373. [Google Scholar] [CrossRef]
- Miyamoto, M.; Murphy, T.H.; Schnaar, R.L.; Coyle, J.T. Antioxidants protect against glutamate-induced cytotoxicity in a neuronal cell line. J. Pharmacol. Exp. Ther. 1989, 250, 1132–1140. [Google Scholar]
- Krieglstein, J.; Rischke, R. Vinpocetine increases the neuroprotective effect of adenosine in vitro. Eur. J. Pharmacol. 1991, 205, 7–10. [Google Scholar] [CrossRef]
- Patyar, S.; Prakash, A.; Modi, M.; Medhi, B. Role of vinpocetine in cerebrovascular diseases. Pharmacol. Rep. 2011, 63, 618–628. [Google Scholar] [CrossRef]
- Li, J.; Chen, F.; Hu, C.; He, L.; Yan, K.; Zhou, L.; Pan, W. Optimized Preparation of in Situ Forming Microparticles for the Parenteral Delivery of Vinpocetine. Chem. Pharm. Bull. 2008, 56, 796–801. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Vas, Á.; Gulyás, B. Eburnamine derivatives and the brain. Med. Res. Rev. 2005, 25, 737–757. [Google Scholar] [CrossRef] [PubMed]
- Willson, C. Vinpocetine. In Reference Module in Biomedical Sciences; Elsevier: Amsterdam, The Netherlands, 2015. [Google Scholar] [CrossRef]
- Avula, B.; Chittiboyina, A.G.; Sagi, S.; Wang, Y.-H.; Wang, M.; Khan, I.A.; Cohen, P.A. Identification and quantification of vinpocetine and picamilon in dietary supplements sold in the United States. Drug Test. Anal. 2016, 8, 334–343. [Google Scholar] [CrossRef] [PubMed]
- Cohen, P.A. Vinpocetine: An Unapproved Drug Sold as a Dietary Supplement. Mayo Clin. Proc. 2015, 90, 1455. [Google Scholar] [CrossRef]
- Waidyanatha, S.; Toy, H.; South, N.; Gibbs, S.; Mutlu, E.; Burback, B.; McIntyre, B.S.; Catlin, N. Systemic exposure of vinpocetine in pregnant Sprague Dawley rats following repeated oral exposure: An investigation of fetal transfer. Toxicol. Appl. Pharmacol. 2018, 338, 83–92. [Google Scholar] [CrossRef]
- Louis, J.-C. Effect of naftidrofuryl on metabolism and survival of cultured neurons. Neurochem. Res. 1989, 14, 1195–1201. [Google Scholar] [CrossRef]
- Meynaud, A.; Grand, M.; Fontaine, L. Effect of naftidrofuryl upon energy metabolism of the brain. Arzneimittelforschung 1973, 23, 1431–1436. [Google Scholar]
- Toussaint, O.; Houbion, A.; Remacle, J. Effects of modulations of the energetic metabolism on the mortality of cultured cells. Biochim. Biophys. Acta Bioenerg. 1994, 1186, 209–220. [Google Scholar] [CrossRef]
- Barradas, M.A.; Stansby, G.; Hamilton, G.; Mikhailidis, D.P. Effect of naftidrofuryl and aspirin on platelet aggregation in peripheral vascular disease. In Vivo 1993, 7, 543–548. [Google Scholar]
- Kirsten, R.; Erdeg, B.; Moxter, D.; Hesse, K.; Breidert, M.; Nelson, K. Platelet aggregation after naftidrofuryl application in vitro and ex vivo. Int. J. Clin. Pharmacol. Ther. 1995, 33, 81–84. [Google Scholar]
- Nabeshima, T.; Hiramatsu, M.; Niwa, K.; Fuji, K.; Kameyama, T. Effect of naftidrofuryl oxalate on 5-HT2 receptors in mouse brain: Evaluation based on quantitative autoradiography and head-twitch response. Eur. J. Pharmacol. 1992, 223, 109–115. [Google Scholar] [CrossRef]
- Hoyer, D.; Clarke, D.E.; Fozard, J.R.; Hartig, P.R.; Martin, G.R.; Mylecharane, E.J.; Saxena, P.R.; Humphrey, P.P. International Union of Pharmacology classification of receptors for 5-hydroxytryptamine (Serotonin). Pharmacol. Rev. 1994, 46, 157–203. [Google Scholar] [PubMed]
- Plotkine, M.; Massad, L.; Allix, M.; Boulu, R.G. A new arterial thrombosis model to study antithrombotic agents: Efficacy of naftidrofuryl. Clin. Hemorheol. Microcirc. 1989, 9, 339–349. [Google Scholar] [CrossRef]
- Kienbaum, P.; Braun, M.; Hohlfeld, T.; Weber, A.A.; Sarbia, M.; Schrör, K. Antiatherosclerotic effects of oral naftidrofuryl in cholesterol-fed rabbits involve inhibition of neutrophil function. J. Cardiovasc. Pharmacol. 1995, 25, 774–781. [Google Scholar] [CrossRef]
- Ogawa, S.-i.; Kameyama, T.; Nabeshima, T. Naftidrofuryl oxalate, nootropic effects on the scopolamine- and the basal forebrain lesion-induced amnesia in rats. Pharmacol. Biochem. Behav. 1991, 39, 997–1002. [Google Scholar] [CrossRef]
- Jung, F.; Kiesewetter, H.; Mrowietz, C.; Leipnitz, G.; Braun, B.; Wappler, M.; Scheffler, P.; Wenzel, E. Hemorrheological, micro- and macrocirculatory effects of naftidrofuryl in an acute study: A randomized, placebo-controlled, double-blind individual comparison. Int. J. Clin. Pharmacol. Ther. Toxicol. 1987, 25, 507–514. [Google Scholar]
- Shaw, S.W.J.; Johnson, R.H. The Effect of Naftidrofuryl on the Metabolic Response to Exercise in Man. Acta Neurol. Scand. 1975, 52, 231–237. [Google Scholar] [CrossRef]
- De Backer, T.; Vander Stichele, R.; Lehert, P.; Van Bortel, L. Naftidrofuryl for intermittent claudication: Meta-analysis based on individual patient data. BMJ 2009, 338, b603. [Google Scholar] [CrossRef][Green Version]
- Yaman, A.; Yaman, H. Complementary Medications (Statins, Nicergoline, Naftidrofuryl) in Dementia. In NeuroPsychopharmacotherapy; Riederer, P., Laux, G., Nagatsu, T., Le, W., Riederer, C., Eds.; Springer International Publishing: Cham, Switzerland, 2020; pp. 1–14. [Google Scholar] [CrossRef]
- Möller, H.J.; Hartmann, A.; Kessler, C.; Rainer, M.; Brown, T.; Gamand, S.; Lehert, P. Naftidrofuryl in the treatment of vascular dementia. Eur. Arch. Psychiatry Clin. Neurosci. 2001, 251, 247–254. [Google Scholar] [CrossRef]
- Cholongitas, E.; Papatheodoridis, G.V.; Mavrogiannaki, A.; Manesis, E. Naftidrofuryl-induced liver injury. Am. J. Gastroenterol. 2003, 98, 1448–1450. [Google Scholar] [CrossRef]
- Stoll, A.; Hofmann, A. Die Alkaloide der Ergotoxingruppe: Ergocristin, Ergokryptin und Ergocornin. (7. Mitteilung über Mutterkornalkaloide). Helv. Chim. Acta 1943, 26, 1570–1601. [Google Scholar] [CrossRef]
- Wilbrandt, R. Treatment of Hypertension With Hydergine: A Review of 200 Cases. Angiology 1953, 4, 183–194. [Google Scholar] [CrossRef] [PubMed]
- Ammon, R.; Sharma, R.; Gambert, S.R.; Lal Gupta, K. Hydergine revisited: A statistical analysis of studies showing efficacy in the treatment of cognitively impaired elderly. AGE 1995, 18, 5–9. [Google Scholar] [CrossRef]
- Sticher, O.; Hamburger, M. Albert Hofmann (1906–2008)–an Obituary. Planta Med. 2008, 74, 791–793. [Google Scholar] [CrossRef]
- Walovitch, R.C.; Ingram, D.K.; Spangler, E.L.; London, E.D. Co-dergocrine, cerebral glucose utilization and maze performance in middle-aged rats. Pharmacol. Biochem. Behav. 1987, 26, 95–101. [Google Scholar] [CrossRef]
- Nagasawa, H.; Kogure, K.; Kawashima, K.; Ido, T.; Itoh, M.; Hatazawa, J.U.N. Effects of Co-Dergocrine Mesylate (Hydergine®) in Multi-Infarct Dementia as Evaluated by Positron Emission Tomography. Tohoku J. Exp. Med. 1990, 162, 225–233. [Google Scholar] [CrossRef][Green Version]
- Büyüköztürk, A.l.; Kanıt, L.; Ersöz, B.; Menteş, G.; Hariri, N.İ. The effects of hydergine on the MAO activity of the aged and adult rat brain. Eur. Neuropsychopharmacol. 1995, 5, 527–529. [Google Scholar] [CrossRef]
- Sözmen, E.Y.; Kanit, L.; Kutay, F.Z.; Hariri, N.İ. Possible supportive effects of co-dergocrine mesylate on antioxidant enzyme systems in aged rat brain. Eur. Neuropsychopharmacol. 1998, 8, 13–16. [Google Scholar] [CrossRef]
- Imperato, A.; Obinu, M.C.; Dazzi, L.; Carta, G.; Mascia, M.S.; Casu, M.A.; Gessa, G.L. Co-dergocrine (hydergine) regulates striatal and hippocampal acetylcholine release through D2; receptors. Neuroreport 1994, 5, 674–676. [Google Scholar] [CrossRef]
- Amenta, F.; Cavallotti, C.; Franch, F.; Ricci, A. Muscarinic cholinergic receptors in the hippocampus of the aged rat: Effects of long-term hydergine administration. Arch. Int. Pharmacodyn. Ther. 1989, 297, 225–234. [Google Scholar]
- Amenta, D.; Ferrante, F.; Franch, F.; Amenta, F. Effects of Long-Term Hydergine® Administration on Lipofuscin Accumulation in Senescent Rat Brain. Gerontology 1988, 34, 250–256. [Google Scholar] [CrossRef] [PubMed]
- Szewczykowski, J.; Meyer, J.S.; Kondo, A.; Nomura, F.; Teraura, T. Effects of ergot alkaloids (Hydergine) on cerebral hemodynamics and oxygen consumption in monkeys. J. Neurol. Sci. 1970, 10, 25–31. [Google Scholar] [CrossRef]
- Saletu, B.; Grünberger, J.; Anderer, R. On brain protection of co-dergocrine mesylate (Hydergine) against hypoxic hypoxidosis of different severity: Double-blind placebo-controlled quantitative EEG and psychometric studies. Int. J. Clin. Pharmacol. Ther. Toxicol. 1990, 28, 510–524. [Google Scholar] [PubMed]
- Schneider, L.S.; Olin, J.T. Overview of Clinical Trials of Hydergine in Dementia. Arch. Neurol. 1994, 51, 787–798. [Google Scholar] [CrossRef]
- Flynn, B.L.; Ranno, A.E. Pharmacologic Management of Alzheimer Disease Part II: Antioxidants, Antihypertensives, and Ergoloid Derivatives. Ann. Pharmacother. 1999, 33, 188–197. [Google Scholar] [CrossRef]
- Thompson, T.L.; Filley, C.M.; Mitchell, W.D.; Culig, K.M.; LoVerde, M.; Byyny, R.L. Lack of Efficacy of Hydergine in Patients with Alzheimer’s Disease. N. Engl. J. Med. 1990, 323, 445–448. [Google Scholar] [CrossRef]
- Olpe, H.R.; Steinmann, M.W. The effect of vincamine, hydergine and piracetam on the firing rate of locus coeruleus neurons. J. Neural Transm. 1982, 55, 101–109. [Google Scholar] [CrossRef]
- Zoglio, M.A.; Maulding, H.V. Complexes of Ergot Alkaloids and Derivatives II: Interaction of Dihydroergotoxine with Certain Xanthines. J. Pharm. Sci. 1970, 59, 215–219. [Google Scholar] [CrossRef]
- Cannon, J.G. Cholinergics. In Burger’s Medicinal Chemistry and Drug Discovery; Spring: Berlin/Heidelberg, Germany, 1984; pp. 39–108. [Google Scholar] [CrossRef]
- White, H.L.; Scates, P.W. Acetyl-L-carnitine as a precursor of acetylcholine. Neurochem. Res. 1990, 15, 597–601. [Google Scholar] [CrossRef]
- Heise, G.A. Facilitation of memory and cognition by drugs. Trends Pharmacol. Sci. 1987, 8, 65–68. [Google Scholar] [CrossRef]
- Fernandes, G.D.; Alberici, R.M.; Pereira, G.G.; Cabral, E.C.; Eberlin, M.N.; Barrera-Arellano, D. Direct characterization of commercial lecithins by easy ambient sonic-spray ionization mass spectrometry. Food Chem. 2012, 135, 1855–1860. [Google Scholar] [CrossRef] [PubMed]
- Wendel, A. Lecithin. In Kirk-Othmer Encyclopedia of Chemical Technology; Wiley: New York, NY, USA, 2000. [Google Scholar] [CrossRef]
- Canty, D.J.; Zeisel, S.H. Lecithin and Choline in Human Health and Disease. Nutr. Rev. 1994, 52, 327–339. [Google Scholar] [CrossRef] [PubMed]
- Chung, S.-Y.; Moriyama, T.; Uezu, E.; Uezu, K.; Hirata, R.; Yohena, N.; Masuda, Y.; Kokubu, Y.; Yamamoto, S. Administration of Phosphatidylcholine Increases Brain Acetylcholine Concentration and Improves Memory in Mice with Dementia. J. Nutr. 1995, 125, 1484–1489. [Google Scholar] [CrossRef] [PubMed]
- Higgins, J.P.T.; Flicker, L. Lecithin for dementia and cognitive impairment. Cochrane Database Syst. Rev. 2000. [Google Scholar] [CrossRef]
- Ladd, S.L.; Sommer, S.A.; LaBerge, S.; Toscano, W. Effect of phosphatidylcholine on explicit memory. Clin. Neuropharmacol. 1993, 16, 540–549. [Google Scholar] [CrossRef] [PubMed]
- Kulkarni, R.; Girish, K.J.; Kumar, A. Nootropic herbs (Medhya Rasayana) in Ayurveda: An update. Pharmacogn. Rev. 2012, 6, 147–153. [Google Scholar] [CrossRef] [PubMed]
- Dwivedi, P.; Singh, R.; Malik, M.T.; Jawaid, T. A traditional approach to herbal nootropic agents: An overview. Int. J. Pharm. Sci. 2012, 3, 630–636. [Google Scholar]
- Zuin, V.G.; Vilegas, J.H.Y. Pesticide residues in medicinal plants and phytomedicines. Phytother. Res. 2000, 14, 73–88. [Google Scholar] [CrossRef]
- Pandey, A.; Savita, R. Harvesting and post-harvest processing of medicinal plants: Problems and prospects. J. Pharm. Innov. 2017, 6, 229–235. [Google Scholar]
- Mishra, M.; Kotwal, P.; Prasad, C. Harvesting of medicinal plants in the forest of Central India and its impact on quality of raw materials: A case of Nagpur District, India. Ecoprint Int. J. Ecol. 2009, 16, 35–42. [Google Scholar] [CrossRef]
- Harnischfeger, G. Proposed Guidelines for Commercial Collection of Medicinal Plant Material. J. Herbs Spices Med. Plants 2000, 7, 43–50. [Google Scholar] [CrossRef]
- Tanko, H.; Carrier, D.J.; Duan, L.; Clausen, E. Pre- and post-harvest processing of medicinal plants. Plant Genet. Res. 2005, 3, 304–313. [Google Scholar] [CrossRef]
- Belwal, T.; Cravotto, C.; Prieto, M.A.; Venskutonis, P.R.; Daglia, M.; Devkota, H.P.; Baldi, A.; Ezzat, S.M.; Gómez-Gómez, L.; Salama, M.M.; et al. Effects of different drying techniques on the quality and bioactive compounds of plant-based products: A critical review on current trends. Dry 2022, 40, 1539–1561. [Google Scholar] [CrossRef]
- Lewicki, P.P. Effect of pre-drying treatment, drying and rehydration on plant tissue properties: A review. Int. J. Food Prop. 1998, 1, 1–22. [Google Scholar] [CrossRef]
- Abascal, K.; Ganora, L.; Yarnell, E. The effect of freeze-drying and its implications for botanical medicine: A review. Phytother. Res. 2005, 19, 655–660. [Google Scholar] [CrossRef]
- Liapis, A.I.; Bruttini, R. Freeze drying. In Handbook of Industrial Drying; Mujumdar, A.S., Ed.; CRC Press: Boca Raton, FL, USA, 2020; pp. 309–343. [Google Scholar]
- Wijesekera, R. The Medicinal Plant Industry; Routledge: London, UK, 2017. [Google Scholar]
- Fonmboh, D.J.; Abah, E.R.; Fokunang, T.E.; Herve, B.; Teke, G.N.; Rose, N.M.; Borgia, N.N.; Fokunang, L.B.; Andrew, B.N.; Kaba, N. An overview of methods of extraction, isolation and characterization of natural medicinal plant products in improved traditional medicine research. Asian J. Res. Med. Pharm. Sci. 2020, 9, 31–57. [Google Scholar] [CrossRef]
- Fu, Y.; Ji, L.L. Chronic Ginseng Consumption Attenuates Age-Associated Oxidative Stress in Rats. J. Nutr. 2003, 133, 3603–3609. [Google Scholar] [CrossRef]
- Churchill, J.D.; Gerson, J.L.; Hinton, K.A.; Mifek, J.L.; Walter, M.J.; Winslow, C.L.; Deyo, R.A. The nootropic properties of ginseng saponin Rb1 are linked to effects on anxiety. Integr. Physiol. Behav. Sci. 2002, 37, 178–187. [Google Scholar] [CrossRef]
- Wang, Y.; Liu, J.; Zhang, Z.; Bi, P.; Qi, Z.; Zhang, C. Anti-neuroinflammation effect of ginsenoside Rbl in a rat model of Alzheimer disease. Neurosci. Lett. 2011, 487, 70–72. [Google Scholar] [CrossRef]
- Yang, L.; Zhang, J.; Zheng, K.; Shen, H.; Chen, X. Long-term Ginsenoside Rg1 Supplementation Improves Age-Related Cognitive Decline by Promoting Synaptic Plasticity Associated Protein Expression in C57BL/6J Mice. J. Gerontol. A 2013, 69A, 282–294. [Google Scholar] [CrossRef]
- Yu, J.; Eto, M.; Akishita, M.; Kaneko, A.; Ouchi, Y.; Okabe, T. Signaling pathway of nitric oxide production induced by ginsenoside Rb1 in human aortic endothelial cells: A possible involvement of androgen receptor. Biochem. Biophys. Res. Commun. 2007, 353, 764–769. [Google Scholar] [CrossRef] [PubMed]
- Diamond, B.J.; Shiflett, S.C.; Feiwel, N.; Matheis, R.J.; Noskin, O.; Richards, J.A.; Schoenberger, N.E. Ginkgo biloba extract: Mechanisms and clinical indications. Arch. Phys. Med. Rehabil. 2000, 81, 668–678. [Google Scholar] [CrossRef]
- Kim, M.-S.; Bang, J.H.; Lee, J.; Han, J.-S.; Baik, T.G.; Jeon, W.K. Ginkgo biloba L. extract protects against chronic cerebral hypoperfusion by modulating neuroinflammation and the cholinergic system. Phytomedicine 2016, 23, 1356–1364. [Google Scholar] [CrossRef] [PubMed]
- Nishimon, S.; Yamaguchi, M.; Muraki, H.; Sakai, N.; Nishino, S. Intraperitoneal injection of ginkgolide B, a major active compound of Ginkgo biloba, dose-dependently increases the amount of wake and decreases non-rapid eye movement sleep in C57BL/6 mice. Neurosci. Lett. 2020, 722, 134832. [Google Scholar] [CrossRef]
- Stough, C.; Clarke, J.; Lloyd, J.; Nathan, P.J. Neuropsychological changes after 30-day Ginkgo biloba administration in healthy participants. Int. J. Neuropsychopharmacol. 2001, 4, 131–134. [Google Scholar] [CrossRef]
- Valli, G.; Giardina, E.-G.V. Benefits, adverse effects and drug interactionsof herbal therapies with cardiovascular effects. J. Am. Coll. Cardiol. 2002, 39, 1083–1095. [Google Scholar] [CrossRef]
- Chanana, P.; Kumar, A. Possible Involvement of Nitric Oxide Modulatory Mechanisms in the Neuroprotective Effect of Centella asiatica Against Sleep Deprivation Induced Anxiety Like Behaviour, Oxidative Damage and Neuroinflammation. Phytother. Res. 2016, 30, 671–680. [Google Scholar] [CrossRef]
- Chen, C.-L.; Tsai, W.-H.; Chen, C.-J.; Pan, T.-M. Centella asiatica extract protects against amyloid β1–40-induced neurotoxicity in neuronal cells by activating the antioxidative defence system. J. Tradit. Complement. Med. 2016, 6, 362–369. [Google Scholar] [CrossRef]
- Rao, S.B.; Chetana, M.; Uma Devi, P. Centella asiatica treatment during postnatal period enhances learning and memory in mice. Physiol. Behav. 2005, 86, 449–457. [Google Scholar] [CrossRef]
- Bhattacharya, S.K.; Kumar, A.; Ghosal, S. Effects of glycowithanolides from Withania somnifera on an animal model of Alzheimer’s disease and perturbed central cholinergic markers of cognition in rats. Phytother. Res. 1995, 9, 110–113. [Google Scholar] [CrossRef]
- Naidu, P.S.; Singh, A.; Kulkarni, S.K. Effect of Withania somnifera root extract on reserpine-induced orofacial dyskinesia and cognitive dysfunction. Phytother. Res. 2006, 20, 140–146. [Google Scholar] [CrossRef] [PubMed]
- Schliebs, R.; Liebmann, A.; Bhattacharya, S.K.; Kumar, A.; Ghosal, S.; Bigl, V. Systemic administration of defined extracts from Withania somnifera (Indian ginseng) and Shilajit differentially affects cholinergic but not glutamatergic and GABAergic markers in rat brain. Neurochem. Int. 1997, 30, 181–190. [Google Scholar] [CrossRef]
- Ziauddin, M.; Phansalkar, N.; Patki, P.; Diwanay, S.; Patwardhan, B. Studies on the immunomodulatory effects of Ashwagandha. J. Ethnopharmacol. 1996, 50, 69–76. [Google Scholar] [CrossRef]
- Le, X.T.; Pham, H.T.N.; Do, P.T.; Fujiwara, H.; Tanaka, K.; Li, F.; Van Nguyen, T.; Nguyen, K.M.; Matsumoto, K. Bacopa monnieri Ameliorates Memory Deficits in Olfactory Bulbectomized Mice: Possible Involvement of Glutamatergic and Cholinergic Systems. Neurochem. Res. 2013, 38, 2201–2215. [Google Scholar] [CrossRef] [PubMed]
- Russo, A.; Borrelli, F.; Campisi, A.; Acquaviva, R.; Raciti, G.; Vanella, A. Nitric oxide-related toxicity in cultured astrocytes: Effect of Bacopa monniera. Life Sci. 2003, 73, 1517–1526. [Google Scholar] [CrossRef]
- Singh, H.; Dhawan, B. Neuropsychopharmacological effects of the Ayurvedic nootropic Bacopa monniera Linn.(Brahmi). Indian J. Pharmacol. 1997, 29, 359. [Google Scholar]
- Uabundit, N.; Wattanathorn, J.; Mucimapura, S.; Ingkaninan, K. Cognitive enhancement and neuroprotective effects of Bacopa monnieri in Alzheimer’s disease model. J. Ethnopharmacol. 2010, 127, 26–31. [Google Scholar] [CrossRef]
- Espinola, E.B.; Dias, R.F.; Mattei, R.; Carlini, E.A. Pharmacological activity of Guarana (Paullinia cupana Mart.) in laboratory animals. J. Ethnopharmacol. 1997, 55, 223–229. [Google Scholar] [CrossRef]
- Otobone, F.J.; Sanches, A.C.; Nagae, R.L.; Martins, J.V.C.; Obici, S.; Mello, J.C.P.d.; Audi, E.A. Effect of crude extract and its semi purified constituents from guaraná seeds [Paullinia cupana var. sorbilis (Mart.) lucke] on cognitive performance in Morris water maze in rats. Braz. Arch. Biol. Technol. 2005, 48, 723–728. [Google Scholar] [CrossRef]
- Cropley, M.; Banks, A.P.; Boyle, J. The Effects of Rhodiola rosea L. Extract on Anxiety, Stress, Cognition and Other Mood Symptoms. Phytother. Res. 2015, 29, 1934–1939. [Google Scholar] [CrossRef]
- Perfumi, M.; Mattioli, L. Adaptogenic and central nervous system effects of single doses of 3% rosavin and 1% salidroside Rhodiola rosea L. extract in mice. Phytother. Res. 2007, 21, 37–43. [Google Scholar] [CrossRef] [PubMed]
- Yu, S.; Liu, M.; Gu, X.; Ding, F. Neuroprotective Effects of Salidroside in the PC12 Cell Model Exposed to Hypoglycemia and Serum Limitation. Cell Mol. Neurobiol. 2008, 28, 1067–1078. [Google Scholar] [CrossRef] [PubMed]
- Sa, F.; Zhang, L.Q.; Chong, C.M.; Guo, B.J.; Li, S.; Zhang, Z.J.; Zheng, Y.; Hoi, P.M.; Lee, S.M.Y. Discovery of novel anti-parkinsonian effect of schisantherin A in in vitro and in vivo. Neurosci. Lett. 2015, 593, 7–12. [Google Scholar] [CrossRef] [PubMed]
- Yan, T.; Shang, L.; Wang, M.; Zhang, C.; Zhao, X.; Bi, K.; Jia, Y. Lignans from Schisandra chinensis ameliorate cognition deficits and attenuate brain oxidative damage induced by D-galactose in rats. Metab. Brain Dis. 2016, 31, 653–661. [Google Scholar] [CrossRef]
- Zhang, L.Q.; Sa, F.; Chong, C.M.; Wang, Y.; Zhou, Z.Y.; Chang, R.C.C.; Chan, S.W.; Hoi, P.M.; Yuen Lee, S.M. Schisantherin A protects against 6-OHDA-induced dopaminergic neuron damage in zebrafish and cytotoxicity in SH-SY5Y cells through the ROS/NO and AKT/GSK3β pathways. J. Ethnopharmacol. 2015, 170, 8–15. [Google Scholar] [CrossRef]
- Bajpai, V.K.; Sharma, A.; Kim, S.H.; Kim, Y.; Kim, J.-J.; Baeak, K.-H. Microwave-Assisted seed essential oil of eleutherococcus senticosus and its antioxidant and free radical-scavenging activities. J. Food Biochem. 2013, 37, 119–127. [Google Scholar] [CrossRef]
- Gromovaya, V.F.; Shapoval, G.S.; Mironyuk, I.E.; Nestyuk, N.V. Antioxidant properties of medicinal plants. Pharm. Chem. J. 2008, 42, 25–28. [Google Scholar] [CrossRef]
- Szołomicki, S.; Samochowiec, L.; Wójcicki, J.; Droździk, M. The influence of active components of Eleutherococcus senticosus on cellular defence and physical fitness in man. Phytother. Res. 2000, 14, 30–35. [Google Scholar] [CrossRef]
- Takasugi, N.; Moriguchi, T.; Fuwa, T.; Sanada, S.; Ida, Y.; Shoji, J.; Saito, H. Effect of Eleutherococcus senticosus and its components on rectal temperature, body and grip tones, motor coordination, and exploratory and spontaneous movements in acute stressed mice. Pharmacogn. Mag. 1985, 39, 232–237. [Google Scholar]
- Yamauchi, Y.; Ge, Y.-W.; Yoshimatsu, K.; Komatsu, K.; Kuboyama, T.; Yang, X.; Tohda, C. Memory Enhancement by Oral Administration of Extract of Eleutherococcus senticosus Leaves and Active Compounds Transferred in the Brain. Nutrients 2019, 11, 1142. [Google Scholar] [CrossRef]
- Caicai, K.; Limin, H.; Liming, Z.; Zhiqiang, Z.; Yongwu, Y. Isolation, purification and antioxidant activity of polysaccharides from the leaves of maca (Lepidium Meyenii). Int. J. Biol. Macromol. 2018, 107, 2611–2619. [Google Scholar] [CrossRef] [PubMed]
- Guo, S.-S.; Gao, X.-F.; Gu, Y.-R.; Wan, Z.-X.; Lu, A.M.; Qin, Z.-H.; Luo, L. Preservation of Cognitive Function by Lepidium meyenii (Maca) Is Associated with Improvement of Mitochondrial Activity and Upregulation of Autophagy-Related Proteins in Middle-Aged Mouse Cortex. J. Evid. Based Complement. Altern. Med. 2016, 2016, 4394261. [Google Scholar] [CrossRef]
- Rubio, J.; Caldas, M.; Dávila, S.; Gasco, M.; Gonzales, G.F. Effect of three different cultivars of Lepidium meyenii (Maca) on learning and depression in ovariectomized mice. BMC Complement. Altern. Med. 2006, 6, 23. [Google Scholar] [CrossRef]
- Ha, D.-C.; Ryu, G.-H. Chemical components of red, white and extruded root ginseng. J. Korean Soc. Food Sci. Nutr. 2005, 34, 247–254. [Google Scholar] [CrossRef]
- Petkov, V.D.; Belcheva, S.; Konstantinova, E.; Kehayov, R.; Petkov, V.V.; Hadjiivanova, C. Participation of the serotonergic system in the memory effects of Ginkgo biloba L. and Panax ginseng C. A. Mey. Phytother. Res. 1994, 8, 470–477. [Google Scholar] [CrossRef]
- Nocerino, E.; Amato, M.; Izzo, A.A. The aphrodisiac and adaptogenic properties of ginseng. Fitoterapia 2000, 71, S1–S5. [Google Scholar] [CrossRef]
- Kiefer, D.S.; Pantuso, T. Panax ginseng. Am. Fam. Physician 2003, 68, 1539–1542. [Google Scholar]
- Ekor, M. The growing use of herbal medicines: Issues relating to adverse reactions and challenges in monitoring safety. Front. Pharmacol. 2014, 4, 177. [Google Scholar] [CrossRef]
- Masteikova, R.; Muselik, J.; Bernatonienė, J.; Bernatonienė, R. Antioxidative activity of Ginkgo, Echinacea, and Ginseng tinctures. Medicina 2007, 43, 306. [Google Scholar] [CrossRef]
- Boateng, I.D.; Yang, X.-M. Effect of different drying methods on product quality, bioactive and toxic components of Ginkgo biloba L. seed. J. Sci. Food Agric. 2021, 101, 3290–3297. [Google Scholar] [CrossRef]
- Canter, P.; Ernst, E. Ginkgo biloba is not a smart drug: An updated systematic review of randomised clinical trials testing the nootropic effects of G. biloba extracts in healthy people. Hum. Psychopharmacol. 2007, 22, 265–278. [Google Scholar] [CrossRef] [PubMed]
- Le Bars, P.L.; Kastelan, J. Efficacy and safety of a Ginkgo biloba extract. Public Health Nutr. 2000, 3, 495–499. [Google Scholar] [CrossRef] [PubMed]
- EGb 761. Drugs R & D; Springer: Berlin/Heidelberg, Germany, 2003; Volume 4, pp. 188–193. [Google Scholar] [CrossRef]
- Mahady, G.B. Ginkgo Biloba: A Review of Quality, Safety, and Efficacy. Nutr. Clin. Care 2001, 4, 140–147. [Google Scholar] [CrossRef]
- Jayasinghe, M.; Senadheera, S.; Wijesekara, I.; Ranaweera, K. Determination of macronutrient compositions in selected, frequently consumed leafy vegetables, prepared according to common culinary methods in Sri Lanka. Vidyodaya J. Sci. 2019, 22, 816–820. [Google Scholar] [CrossRef]
- Wijeweera, P.; Arnason, J.T.; Koszycki, D.; Merali, Z. Evaluation of anxiolytic properties of Gotukola—(Centella asiatica) extracts and asiaticoside in rat behavioral models. Phytomedicine 2006, 13, 668–676. [Google Scholar] [CrossRef] [PubMed]
- Gohil, K.J.; Patel, J.A.; Gajjar, A.K. Pharmacological Review on Centella asiatica: A Potential Herbal Cure-all. Indian J. Pharm. Sci. 2010, 72, 546–556. [Google Scholar] [CrossRef]
- Anukunwithaya, T.; Tantisira, M.H.; Tantisira, B.; Khemawoot, P. Pharmacokinetics of a standardized extract of Centella asiatica ECa 233 in rats. Planta Med. 2017, 83, 710–717. [Google Scholar] [CrossRef]
- Brinkhaus, B.; Lindner, M.; Schuppan, D.; Hahn, E.G. Chemical, pharmacological and clinical profile of the East Asian medical plant Centella aslatica. Phytomedicine 2000, 7, 427–448. [Google Scholar] [CrossRef]
- Bamola, N.; Verma, P.; Negi, C. A review on some traditional medicinal plants. Int. J. Life Sci. Res. 2018, 4, 1550–1556. [Google Scholar] [CrossRef]
- Patel, K.; Singh, R.B.; Patel, D.K. Pharmacological and analytical aspects of withaferin A: A concise report of current scientific literature. Asian Pac. J. Reprod. 2013, 2, 238–243. [Google Scholar] [CrossRef]
- Raut, A.A.; Rege, N.N.; Tadvi, F.M.; Solanki, P.V.; Kene, K.R.; Shirolkar, S.G.; Pandey, S.N.; Vaidya, R.A.; Vaidya, A.B. Exploratory study to evaluate tolerability, safety, and activity of Ashwagandha (Withania somnifera) in healthy volunteers. J. Ayurveda Integr. Med. 2012, 3, 111–114. [Google Scholar] [CrossRef] [PubMed]
- Meher, S.K.; Das, B.; Panda, P.; Bhuyan, G.C.; Rao, M.M. Uses of Withania somnifera (Linn) Dunal (Ashwagandha) in Ayurveda and its pharmacological evidences. Res. J. Pharmacol. Pharmacodyn. 2016, 8, 23–29. [Google Scholar] [CrossRef]
- Chadha, M.L. Indigenous vegetables of India with potentials for improving livelihood. Acta Hortic. 2009, 806, 579–586. [Google Scholar] [CrossRef]
- Devendra, P.; Patel, S.S.; Birwal, P.; Basu, S.; Deshmukh, G.; Datir, R. Brahmi (Bacopa monnieri) as functional food ingredient in food processing industry. J. Pharmacogn. Phytochem. 2018, 7, 189–194. [Google Scholar]
- Gohil, K.J.; Patel, J.A. A review on Bacopa monniera: Current research and future prospects. Int. J. Green Pharm. 2010, 4, 1–9. [Google Scholar] [CrossRef]
- Russo, A.; Borrelli, F. Bacopa monniera, a reputed nootropic plant: An overview. Phytomedicine 2005, 12, 305–317. [Google Scholar] [CrossRef]
- Kean, J.D.; Downey, L.A.; Stough, C. A systematic review of the Ayurvedic medicinal herb Bacopa monnieri in child and adolescent populations. Complement. Ther. Med. 2016, 29, 56–62. [Google Scholar] [CrossRef]
- Cavalcanti, V.; Marques, M.; Do Nascimento, W.M.; Rocha, A.W.D.O.; Ferreira, I.D.J.; Leão, D.P.; Félix, P.H.C.; De Oliveira, C.M.C. Bioproducts based on guarana (Paulinia cupana) for practitioners of physical activity. Eur. Acad. Res. 2020, 8, 1746–1759. [Google Scholar]
- Banga, S.; Kumar, V.; Suri, S.; Kaushal, M.; Prasad, R.; Kaur, S. Nutraceutical Potential of Diet Drinks: A Critical Review on Components, Health Effects, and Consumer Safety. J. Am. Coll. Nutr. 2020, 39, 272–286. [Google Scholar] [CrossRef]
- Rangel, M.P.; De Mello, J.C.P.; Audi, E.A. Evaluation of neurotransmitters involved in the anxiolytic and panicolytic effect of the aqueous fraction of Paullinia cupana (guaraná) in elevated T maze. Rev. Bras. Farmacogn. 2013, 23, 358–365. [Google Scholar] [CrossRef]
- Kennedy, D.O.; Haskell, C.F.; Wesnes, K.A.; Scholey, A.B. Improved cognitive performance in human volunteers following administration of guarana (Paullinia cupana) extract: Comparison and interaction with Panax ginseng. Pharmacol. Biochem. Behav. 2004, 79, 401–411. [Google Scholar] [CrossRef] [PubMed]
- Marques, L.L.M.; Klein, T.; De Mello, J.C.P. Chapter 3.24—Guarana. In Nonvitamin and Nonmineral Nutritional Supplements; Nabavi, S.M., Silva, A.S., Eds.; Academic Press: New York, NY, USA, 2019; pp. 283–288. [Google Scholar] [CrossRef]
- Davydov, M.; Krikorian, A.D. Eleutherococcus senticosus (Rupr. & Maxim.) Maxim. (Araliaceae) as an adaptogen: A closer look. J. Ethnopharmacol. 2000, 72, 345–393. [Google Scholar] [CrossRef] [PubMed]
- Gerontakos, S.; Taylor, A.; Avdeeva, A.Y.; Shikova, V.A.; Pozharitskaya, O.N.; Casteleijn, D.; Wardle, J.; Shikov, A.N. Findings of Russian literature on the clinical application of Eleutherococcus senticosus (Rupr. & Maxim.): A narrative review. J. Ethnopharmacol. 2021, 278, 114274. [Google Scholar] [CrossRef]
- Mahady, G.B.; Gyllenhaal, C.; Fong, H.H.; Farnsworth, N.R. Ginsengs: A Review of Safety and Efficacy. Nutr. Clin. Care 2000, 3, 90–101. [Google Scholar] [CrossRef]
- Bleakney, T.L. Deconstructing an Adaptogen: Eleutherococcus senticosus. Holist. Nurs. Pract. 2008, 22, 220–224. [Google Scholar] [CrossRef] [PubMed]
- Schmidt, M.; Thomsen, M.; Kelber, O.; Kraft, K. Myths and facts in herbal medicines: Eleutherococcus senticosus (Siberian ginseng) and its contraindication in hypertensive patients. Botanics 2014, 4, 27–32. [Google Scholar] [CrossRef]
- Kołodziej, B.; Sugier, D. Influence of plants age on the chemical composition of roseroot (Rhodiola rosea L.). Acta Sci. Pol. 2013, 12, 147–160. [Google Scholar]
- Gregory, S.; Kelly, N. Rhodiola rosea: A Possible Plant Adaptogen. Altern. Med. Rev. 2001, 6, 293–302. [Google Scholar]
- Jagtap, P.N.; Mhetre, O.S.; Malavdkar, P.R. A Review Article on Rhodiola Rosea: An Adaptogen Having Multiple Benefits. Int. J. Pharmacogn. 2020, 7, 62–69. [Google Scholar] [CrossRef]
- Panossian, A.; Wikman, G. Pharmacology of Schisandra chinensis Bail.: An overview of Russian research and uses in medicine. J. Ethnopharmacol. 2008, 118, 183–212. [Google Scholar] [CrossRef]
- Liu, X.; Guo, Y.; Cai, G.; Gong, J.; Wang, Y.; Liu, S. Chemical composition analysis of Schisandra chinensis fructus and its three processed products using UHPLC-Q-Orbitrap/MS-based metabolomics approach. Nat. Prod. Res. 2020, 36, 3464–3468. [Google Scholar] [CrossRef] [PubMed]
- Li, N.; Liu, C.; Jing, S.; Wang, M.; Wang, H.; Sun, J.; Wang, C.; Chen, J.; Li, H. Compound Schisandra-Ginseng-Notoginseng-Lycium Extract Ameliorates Scopolamine-Induced Learning and Memory Disorders in Mice. Evid. Based Complement. Altern. Med. 2017, 2017, 8632016. [Google Scholar] [CrossRef] [PubMed]
- Zovko Koncic, M.; Tomczyk, M. New insights into dietary supplements used in sport: Active substances, pharmacological and side effects. Curr. Drug Targets 2013, 14, 1079–1092. [Google Scholar] [CrossRef] [PubMed]
- Brinckmann, J.; Smith, E. Maca Culture of the Junín Plateau. J. Altern. Complement. Med. 2004, 10, 426–430. [Google Scholar] [CrossRef]
- Smith, E. Maca root: Modern Rediscovery of An Ancient Andean Fertility Food. J. Am. Herb. Guild 2004, 4, 15–21. [Google Scholar]
- Gonzales, G.F.; Córdova, A.; Vega, K.; Chung, A.; Villena, A.; Góñez, C.; Castillo, S. Effect of Lepidium meyenii (MACA) on sexual desire and its absent relationship with serum testosterone levels in adult healthy men. Andrologia 2002, 34, 367–372. [Google Scholar] [CrossRef]
- Gonzales-Arimborgo, C.; Yupanqui, I.; Montero, E.; Alarcón-Yaquetto, D.E.; Zevallos-Concha, A.; Caballero, L.; Gasco, M.; Zhao, J.; Khan, I.A.; Gonzales, G.F. Acceptability, Safety, and Efficacy of Oral Administration of Extracts of Black or Red Maca (Lepidium meyenii) in Adult Human Subjects: A Randomized, Double-Blind, Placebo-Controlled Study. Pharmaceuticals 2016, 9, 49. [Google Scholar] [CrossRef]
- West, E.; Krychman, M. Natural Aphrodisiacs—A Review of Selected Sexual Enhancers. Sex. Med. Rev. 2015, 3, 279–288. [Google Scholar] [CrossRef]
- Turnbull, D.; Rodricks, J.V.; Mariano, G.F.; Chowdhury, F. Caffeine and cardiovascular health. Regul. Toxicol. Pharmacol. 2017, 89, 165–185. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Malík, M.; Tlustoš, P. Nootropics as Cognitive Enhancers: Types, Dosage and Side Effects of Smart Drugs. Nutrients 2022, 14, 3367. https://doi.org/10.3390/nu14163367
Malík M, Tlustoš P. Nootropics as Cognitive Enhancers: Types, Dosage and Side Effects of Smart Drugs. Nutrients. 2022; 14(16):3367. https://doi.org/10.3390/nu14163367
Chicago/Turabian StyleMalík, Matěj, and Pavel Tlustoš. 2022. "Nootropics as Cognitive Enhancers: Types, Dosage and Side Effects of Smart Drugs" Nutrients 14, no. 16: 3367. https://doi.org/10.3390/nu14163367
APA StyleMalík, M., & Tlustoš, P. (2022). Nootropics as Cognitive Enhancers: Types, Dosage and Side Effects of Smart Drugs. Nutrients, 14(16), 3367. https://doi.org/10.3390/nu14163367







