Anemia Is a Strong Predictor of Wasting, Disease Severity, and Progression, in Clinical Tuberculosis (TB)
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Patients
2.3. Interventions
2.4. Clinical TB Score and Chest X-ray
2.5. Anthropometric and Laboratory Measurements
2.6. Statistical Analysis
3. Results
3.1. Baseline Characteristics
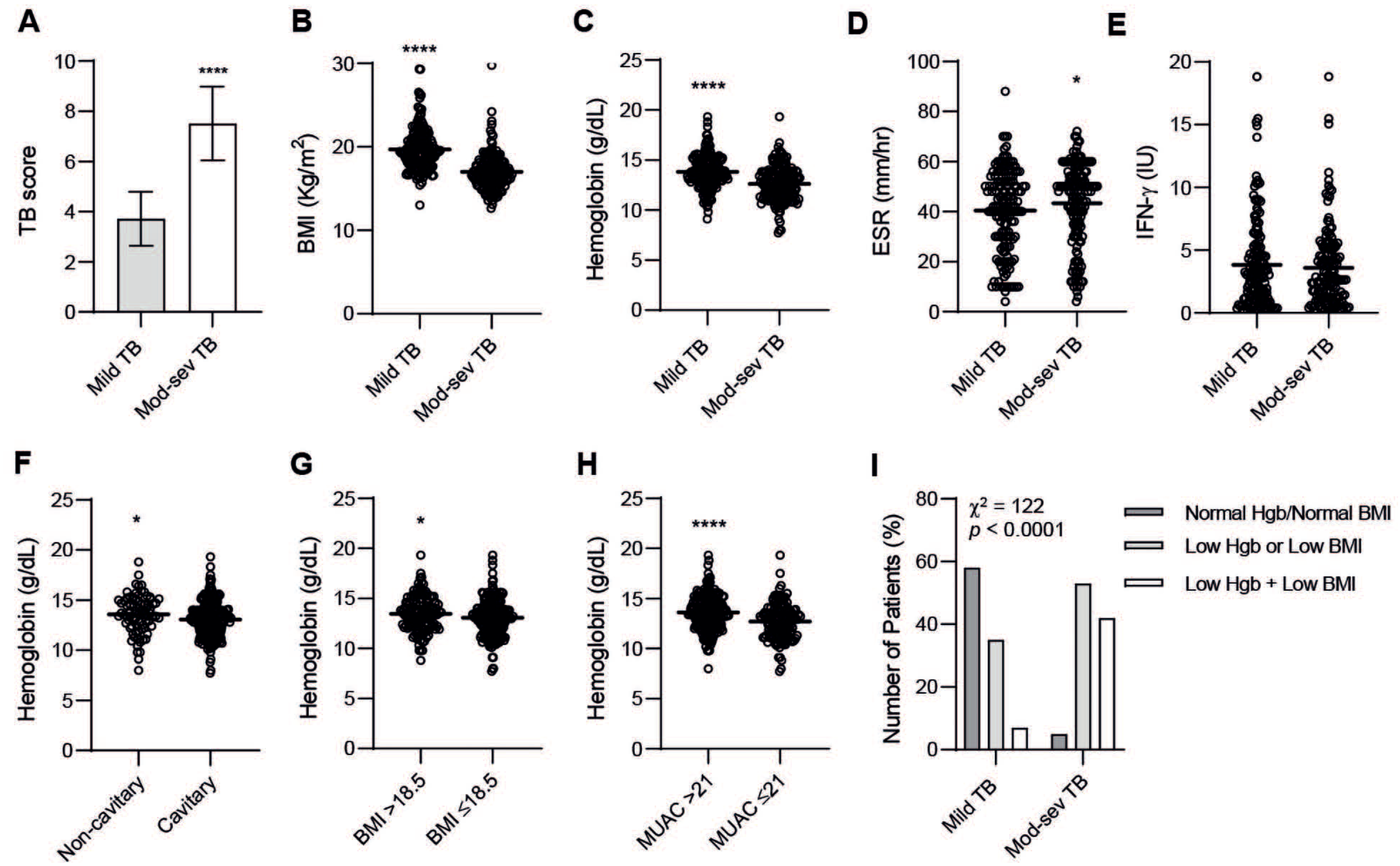
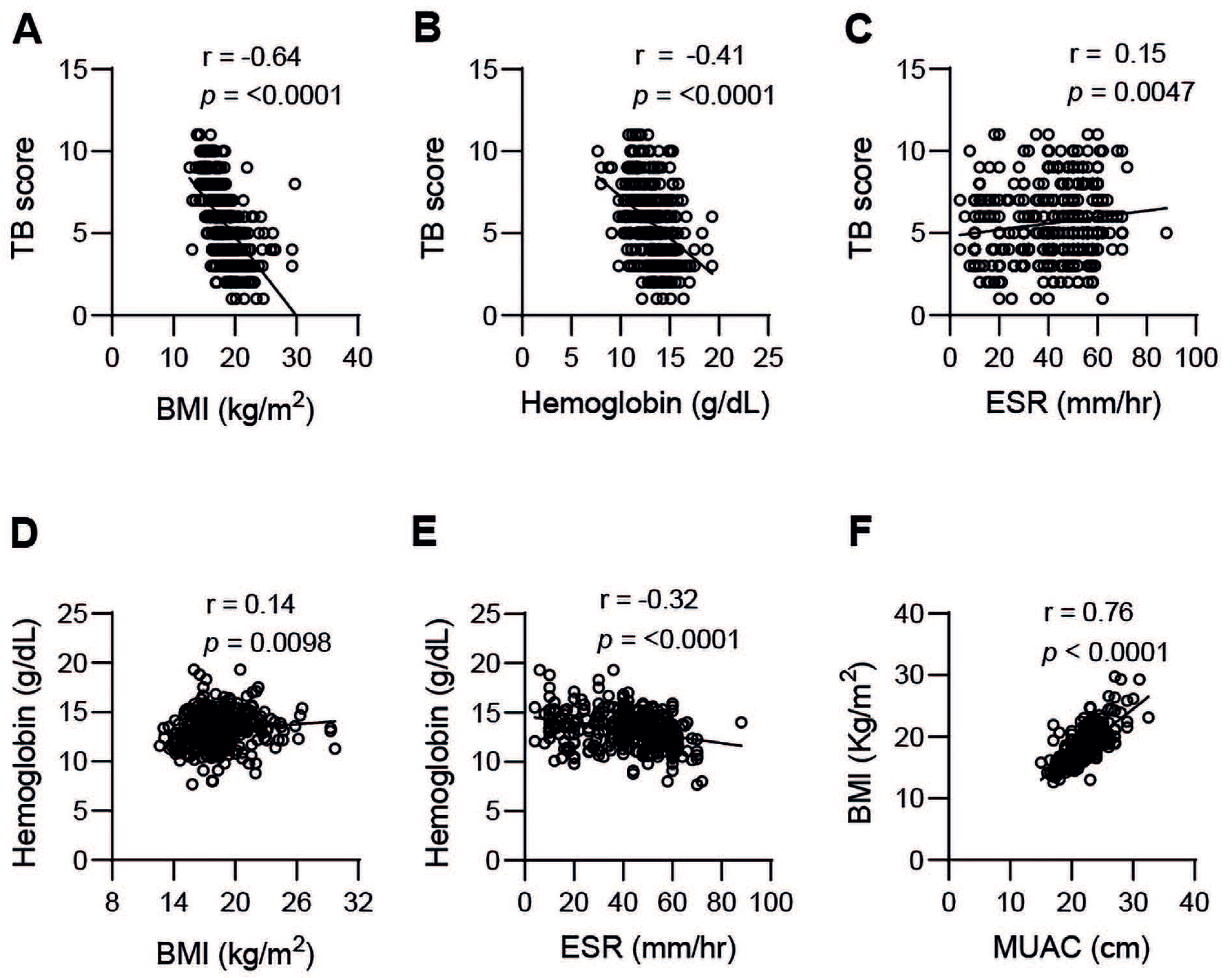
3.2. TB Disease Severity Is Associated with Blood Hb, BMI, and MUAC
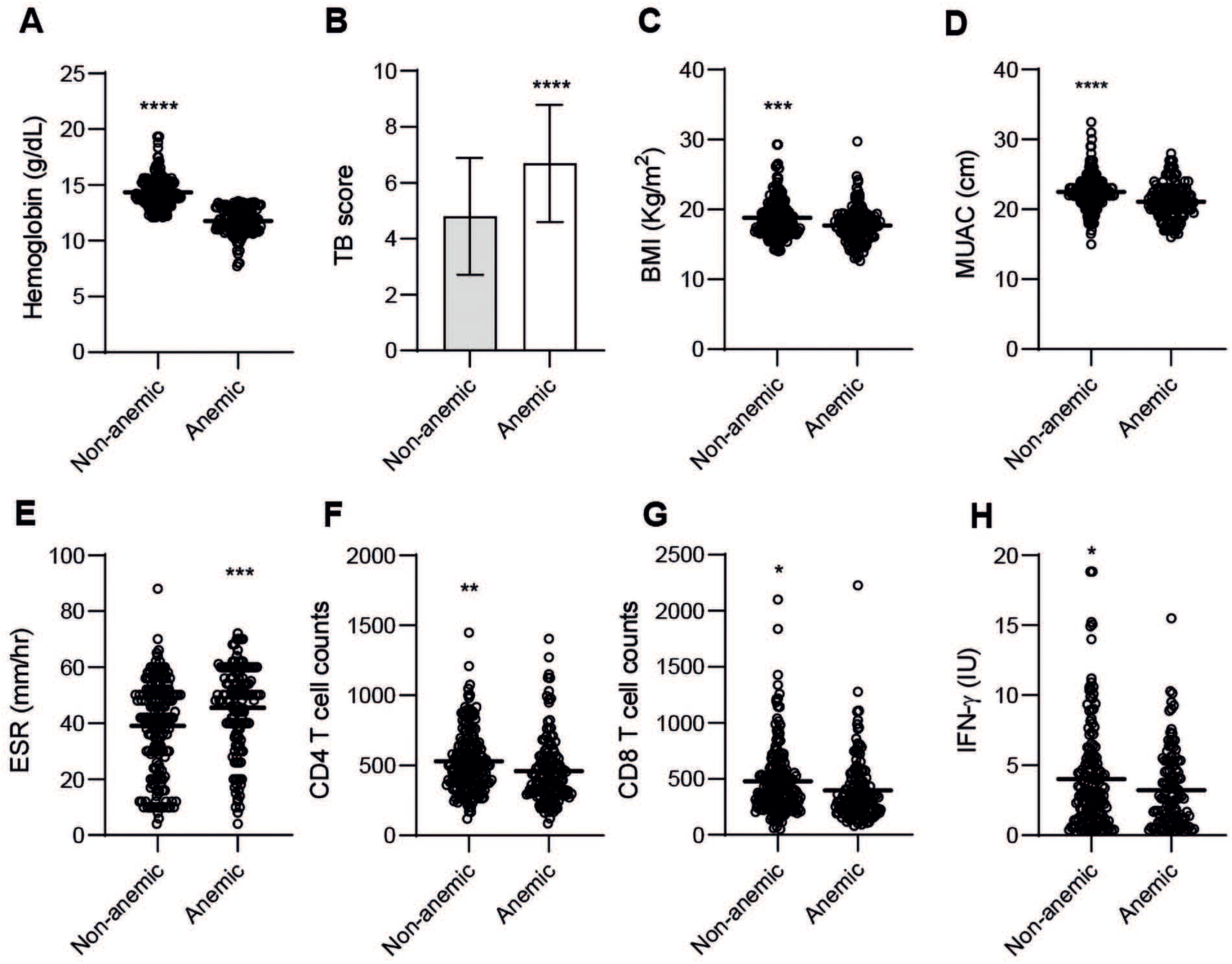
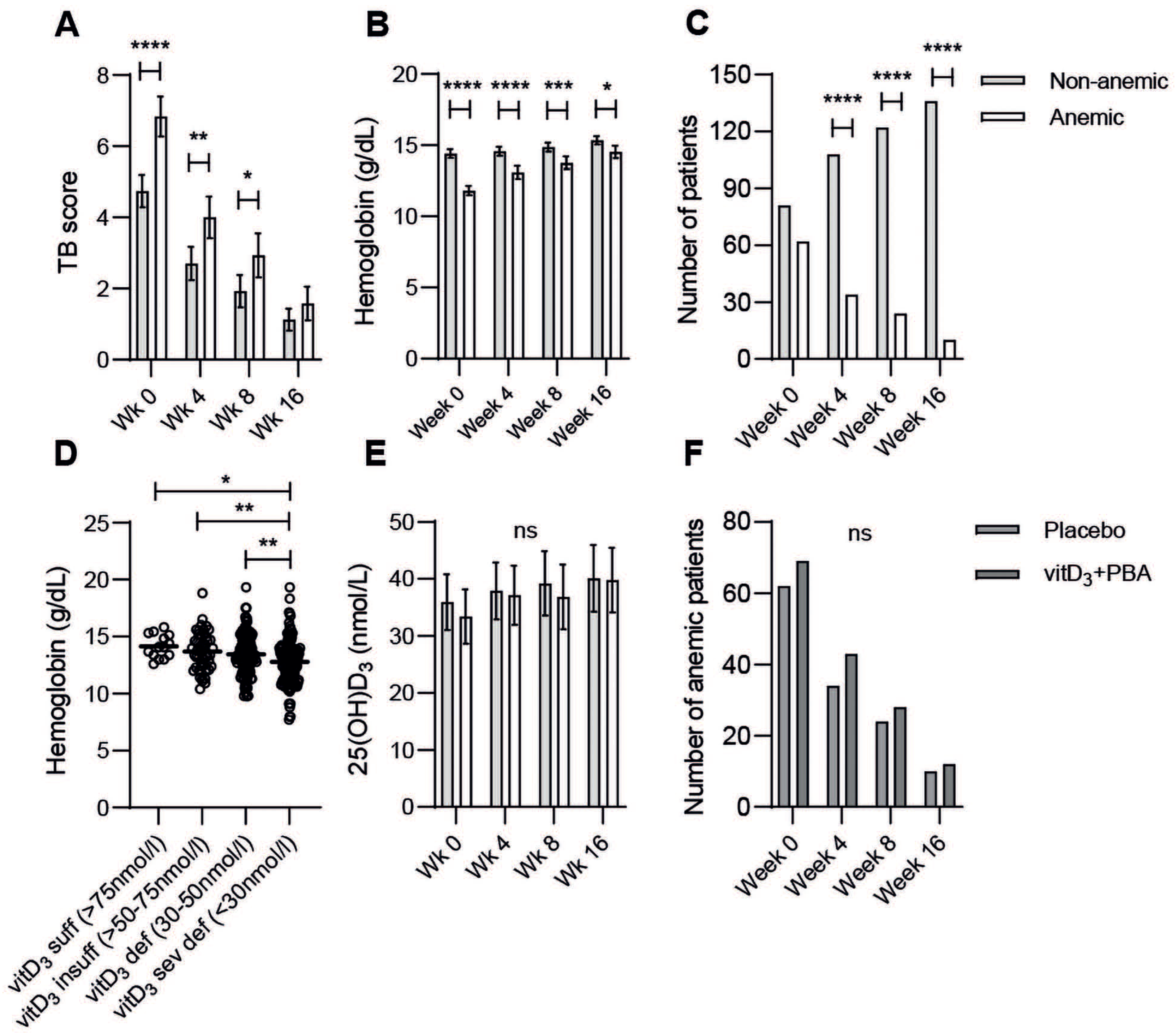
3.3. Anemia Is a Strong Predictor of Moderate-Severe TB Disease
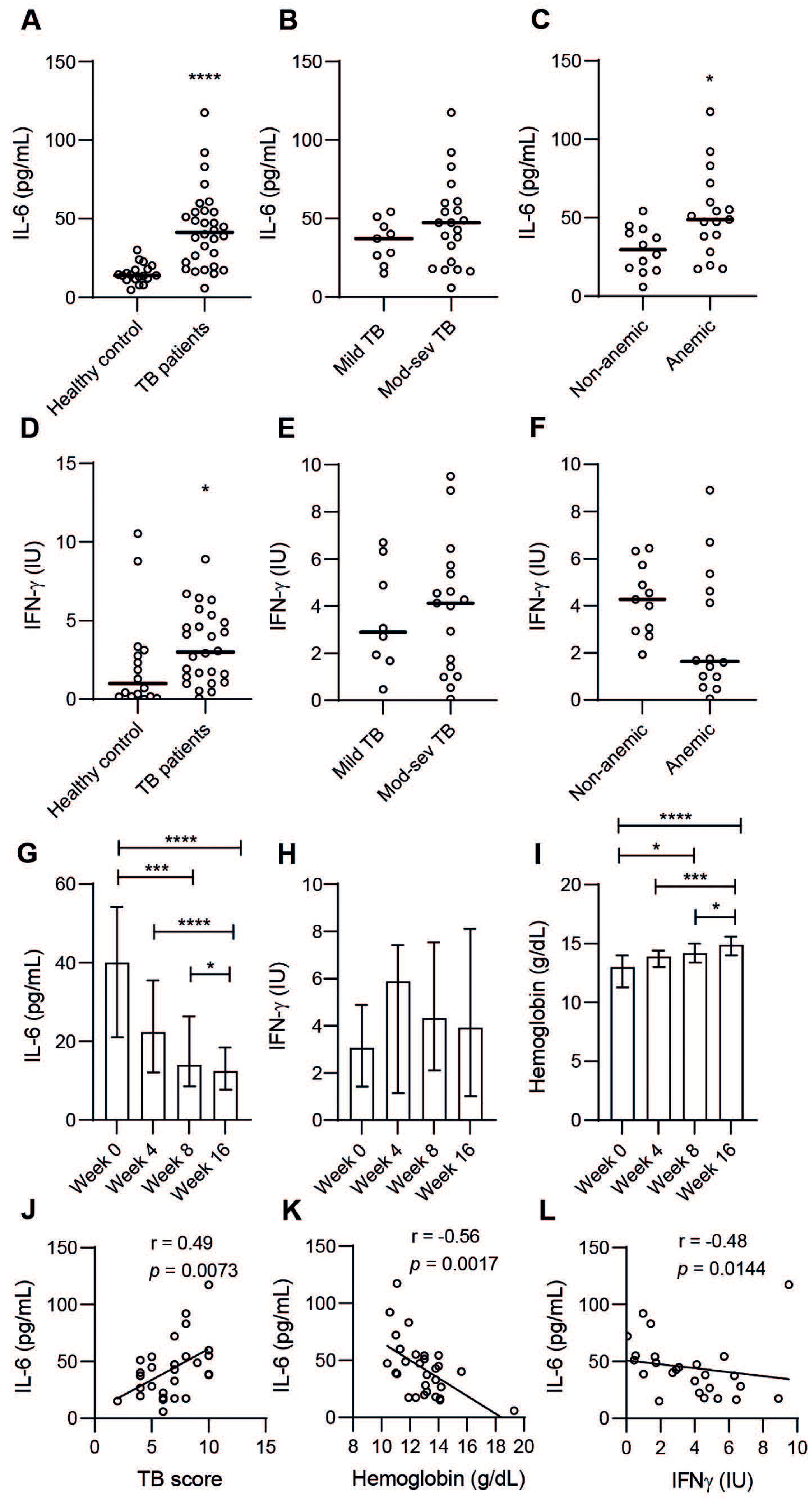
3.4. Plasma IL-6 Is Associated with Active TB Disease, Particularly in Anemic TB Patients
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Gelaw, Y.; Getaneh, Z.; Melku, M. Anemia as a risk factor for tuberculosis: A systematic review and meta-analysis. Environ. Health Prev. Med. 2021, 26, 13. [Google Scholar] [CrossRef] [PubMed]
- Wejse, C.; Gustafson, P.; Nielsen, J.; Gomes, V.F.; Aaby, P.; Andersen, P.L.; Sodemann, M. TBscore: Signs and symptoms from tuberculosis patients in a low-resource setting have predictive value and may be used to assess clinical course. Scand. J. Infect. Dis. 2008, 40, 111–120. [Google Scholar] [CrossRef] [PubMed]
- Raaby, L.; Bendix-Struve, M.; Nielsen, J.; Wejse, C. Inter-observer variation of the Bandim TB-score. Scand. J. Infect. Dis. 2009, 41, 220–223. [Google Scholar] [CrossRef] [PubMed]
- Kalantri, A.; Karambelkar, M.; Joshi, R.; Kalantri, S.; Jajoo, U. Accuracy and reliability of pallor for detecting anaemia: A hospital-based diagnostic accuracy study. PLoS ONE 2010, 5, e8545. [Google Scholar] [CrossRef]
- Ganz, T. Anemia of Inflammation. N. Engl. J. Med. 2019, 381, 1148–1157. [Google Scholar] [CrossRef] [PubMed]
- Weiss, G.; Goodnough, L.T. Anemia of chronic disease. N. Engl. J. Med. 2005, 352, 1011–1023. [Google Scholar] [CrossRef] [PubMed]
- Kamruzzaman, M. Is BMI associated with anemia and hemoglobin level of women and children in Bangladesh: A study with multiple statistical approaches. PLoS ONE 2021, 16, e0259116. [Google Scholar] [CrossRef] [PubMed]
- Van Lettow, M.; Kumwenda, J.J.; Harries, A.D.; Whalen, C.C.; Taha, T.E.; Kumwenda, N.; Kang’ombe, C.; Semba, R.D. Malnutrition and the severity of lung disease in adults with pulmonary tuberculosis in Malawi. Int. J. Tuberc. Lung Dis. 2004, 8, 211–217. [Google Scholar] [PubMed]
- Feleke, B.E.; Feleke, T.E.; Biadglegne, F. Nutritional status of tuberculosis patients, a comparative cross-sectional study. BMC Pulm. Med. 2019, 19, 182. [Google Scholar] [CrossRef] [PubMed]
- Schaible, U.E.; Kaufmann, S.H. Malnutrition and infection: Complex mechanisms and global impacts. PLoS Med. 2007, 4, e115. [Google Scholar] [CrossRef] [PubMed]
- Takele, Y.; Adem, E.; Getahun, M.; Tajebe, F.; Kiflie, A.; Hailu, A.; Raynes, J.; Mengesha, B.; Ayele, T.A.; Shkedy, Z.; et al. Malnutrition in Healthy Individuals Results in Increased Mixed Cytokine Profiles, Altered Neutrophil Subsets and Function. PLoS ONE 2016, 11, e0157919. [Google Scholar] [CrossRef]
- Bourke, C.D.; Berkley, J.A.; Prendergast, A.J. Immune Dysfunction as a Cause and Consequence of Malnutrition. Trends Immunol. 2016, 37, 386–398. [Google Scholar] [CrossRef] [PubMed]
- Chhabra, S.; Kashyap, A.; Bhagat, M.; Mahajan, R.; Sethi, S. Anemia and Nutritional Status in Tuberculosis Patients. Int. J. Appl. Basic Med. Res. 2021, 11, 226–230. [Google Scholar] [CrossRef] [PubMed]
- Bekele, A.; Gebreselassie, N.; Ashenafi, S.; Kassa, E.; Aseffa, G.; Amogne, W.; Getachew, M.; Aseffa, A.; Worku, A.; Raqib, R.; et al. Daily adjunctive therapy with vitamin D3 and phenylbutyrate supports clinical recovery from pulmonary tuberculosis: A randomized controlled trial in Ethiopia. J. Intern. Med. 2018, 284, 292–306. [Google Scholar] [CrossRef] [PubMed]
- Nicoll, D.; Mark, L.C.; McPhee, S.J. (Eds.) Guide to Diagnostic Tests, 7th ed.; McGraw Hill: Columbus, OH, USA, 2017; Available online: https://accessmedicine.mhmedical.com/content.aspx?bookid=2032§ionid=151444058 (accessed on 15 October 2021).
- Amrein, K.; Scherkl, M.; Hoffmann, M.; Neuwersch-Sommeregger, S.; Kostenberger, M.; Berisha, A.T.; Martucci, G.; Pilz, S.; Malle, O. Vitamin D deficiency 2.0: An update on the current status worldwide. Eur. J. Clin. Nutr. 2020, 74, 1498–1513. [Google Scholar] [CrossRef] [PubMed]
- Thorup, L.; Hamann, S.A.; Kallestrup, P.; Hjortdal, V.E.; Tripathee, A.; Neupane, D.; Patsche, C.B. Mid-upper arm circumference as an indicator of underweight in adults: A cross-sectional study from Nepal. BMC Public Health 2020, 20, 1187. [Google Scholar] [CrossRef] [PubMed]
- Minchella, P.A.; Donkor, S.; Owolabi, O.; Sutherland, J.S.; McDermid, J.M. Complex anemia in tuberculosis: The need to consider causes and timing when designing interventions. Clin. Infect. Dis. 2015, 60, 764–772. [Google Scholar] [CrossRef] [PubMed]
- Gil-Santana, L.; Cruz, L.A.B.; Arriaga, M.B.; Miranda, P.F.C.; Fukutani, K.F.; Silveira-Mattos, P.S.; Silva, E.C.; Oliveira, M.G.; Mesquita, E.D.D.; Rauwerdink, A.; et al. Tuberculosis-associated anemia is linked to a distinct inflammatory profile that persists after initiation of antitubercular therapy. Sci. Rep. 2019, 9, 1381. [Google Scholar] [CrossRef] [PubMed]
- Demitto, F.O.; Araujo-Pereira, M.; Schmaltz, C.A.; Sant’Anna, F.M.; Arriaga, M.B.; Andrade, B.B.; Rolla, V.C. Impact of Persistent Anemia on Systemic Inflammation and Tuberculosis Outcomes in Persons Living With HIV. Front. Immunol. 2020, 11, 588405. [Google Scholar] [CrossRef] [PubMed]
- Merker, M.; Amsler, A.; Pereira, R.; Bolliger, R.; Tribolet, P.; Braun, N.; Hoess, C.; Pavlicek, V.; Bilz, S.; Sigrist, S.; et al. Vitamin D deficiency is highly prevalent in malnourished inpatients and associated with higher mortality: A prospective cohort study. Medicine 2019, 98, e18113. [Google Scholar] [CrossRef] [PubMed]
- Song, C.; Sun, H.; Wang, B.; Song, C.; Lu, H. Association Between Vitamin D Status and Undernutrition Indices in Children: A Systematic Review and Meta-Analysis of Observational Studies. Front. Pediatr. 2021, 9, 665749. [Google Scholar] [CrossRef]
- Liu, P.T.; Stenger, S.; Li, H.; Wenzel, L.; Tan, B.H.; Krutzik, S.R.; Ochoa, M.T.; Schauber, J.; Wu, K.; Meinken, C.; et al. Toll-like receptor triggering of a vitamin D-mediated human antimicrobial response. Science 2006, 311, 1770–1773. [Google Scholar] [CrossRef]
- Coussens, A.K.; Wilkinson, R.J.; Hanifa, Y.; Nikolayevskyy, V.; Elkington, P.T.; Islam, K.; Timms, P.M.; Venton, T.R.; Bothamley, G.H.; Packe, G.E.; et al. Vitamin D accelerates resolution of inflammatory responses during tuberculosis treatment. Proc. Natl. Acad. Sci. USA 2012, 109, 15449–15454. [Google Scholar] [CrossRef]
- Grobler, L.; Nagpal, S.; Sudarsanam, T.D.; Sinclair, D. Nutritional supplements for people being treated for active tuberculosis. Cochrane Database Syst. Rev. 2016, 2016, CD006086. [Google Scholar] [CrossRef]
- Brighenti, S.; Bergman, P.; Martineau, A.R. Vitamin D and tuberculosis: Where next? J. Intern. Med. 2018, 284, 145–162. [Google Scholar] [CrossRef] [PubMed]
- Lonnroth, K.; Williams, B.G.; Cegielski, P.; Dye, C. A consistent log-linear relationship between tuberculosis incidence and body mass index. Int. J. Epidemiol. 2010, 39, 149–155. [Google Scholar] [CrossRef] [PubMed]
- Choi, H.; Yoo, J.E.; Han, K.; Choi, W.; Rhee, S.Y.; Lee, H.; Shin, D.W. Body Mass Index, Diabetes, and Risk of Tuberculosis: A Retrospective Cohort Study. Front. Nutr. 2021, 8, 739766. [Google Scholar] [CrossRef] [PubMed]
- Chen, J.; Zha, S.; Hou, J.; Lu, K.; Qiu, Y.; Yang, R.; Li, L.; Yang, Y.; Xu, L. Dose-response relationship between body mass index and tuberculosis in China: A population-based cohort study. BMJ Open 2022, 12, e050928. [Google Scholar] [CrossRef] [PubMed]
- Nemeth, E.; Rivera, S.; Gabayan, V.; Keller, C.; Taudorf, S.; Pedersen, B.K.; Ganz, T. IL-6 mediates hypoferremia of inflammation by inducing the synthesis of the iron regulatory hormone hepcidin. J. Clin. Investig. 2004, 113, 1271–1276. [Google Scholar] [CrossRef] [PubMed]
- De Voss, J.J.; Rutter, K.; Schroeder, B.G.; Barry, C.E., III. Iron acquisition and metabolism by mycobacteria. J. Bacteriol. 1999, 181, 4443–4451. [Google Scholar] [CrossRef]
- Abreu, R.; Essler, L.; Giri, P.; Quinn, F. Interferon-gamma promotes iron export in human macrophages to limit intracellular bacterial replication. PLoS ONE 2020, 15, e0240949. [Google Scholar] [CrossRef] [PubMed]
- van Lettow, M.; West, C.E.; van der Meer, J.W.; Wieringa, F.T.; Semba, R.D. Low plasma selenium concentrations, high plasma human immunodeficiency virus load and high interleukin-6 concentrations are risk factors associated with anemia in adults presenting with pulmonary tuberculosis in Zomba district, Malawi. Eur. J. Clin. Nutr. 2005, 59, 526–532. [Google Scholar] [CrossRef] [PubMed]
- Sonal, V.; Suman, S.; Kapoor, A.; Nema, S.K. Serum hepcidin and interleukin-6 as biochemical markers in differentiation of iron deficiency anemia and anemia of chronic disease. Int. J. Res. Med. Sci. 2018, 6, 1922–1926. [Google Scholar]
- Cercamondi, C.I.; Stoffel, N.U.; Moretti, D.; Zoller, T.; Swinkels, D.W.; Zeder, C.; Mhimibra, F.; Hella, J.; Fenner, L.; Zimmermann, M.B. Iron homeostasis during anemia of inflammation: A prospective study of patients with tuberculosis. Blood 2021, 138, 1293–1303. [Google Scholar] [CrossRef] [PubMed]
- Das, B.S.; Devi, U.; Rao, C.M.; Srivastava, V.K.; Rath, P.K.; Das, B.S. Effect of iron supplementation on mild to moderate anaemia in pulmonary tuberculosis. Br. J. Nutr. 2003, 90, 541–550. [Google Scholar] [CrossRef] [PubMed]
- Bayliss, T.J.; Smith, J.T.; Schuster, M.; Dragnev, K.H.; Rigas, J.R. A humanized anti-IL-6 antibody (ALD518) in non-small cell lung cancer. Expert Opin. Biol. Ther. 2011, 11, 1663–1668. [Google Scholar] [CrossRef]
- Noguchi-Sasaki, M.; Sasaki, Y.; Shimonaka, Y.; Mori, K.; Fujimoto-Ouchi, K. Treatment with anti-IL-6 receptor antibody prevented increase in serum hepcidin levels and improved anemia in mice inoculated with IL-6-producing lung carcinoma cells. BMC Cancer 2016, 16, 270. [Google Scholar] [CrossRef]
- Song, S.N.; Tomosugi, N.; Kawabata, H.; Ishikawa, T.; Nishikawa, T.; Yoshizaki, K. Down-regulation of hepcidin resulting from long-term treatment with an anti-IL-6 receptor antibody (tocilizumab) improves anemia of inflammation in multicentric Castleman disease. Blood 2010, 116, 3627–3634. [Google Scholar] [CrossRef]
- Cobelens, F.; Kerkhoff, A.D. Tuberculosis and anemia-cause or effect? Environ. Health Prev. Med. 2021, 26, 93. [Google Scholar] [CrossRef]
| Variables a | TB Patients (n = 345) | Healthy Controls (n = 102) | p-Value b |
|---|---|---|---|
| Gender (M/F) (no/%) | 200/145 (58/42) | 60/42 (59/41) | 0.880 |
| Age (years) | 30.4 | 36.2 | <0.0001 |
| TB score c | 5.61 | na | |
| Mild TB/Mod-sev TB (no/%) | 173/172 (50/50) | na | |
| Non-cavitary TB/Cavitary TB c (no/%) d | 82/238 (26/74) | na | |
| Hemoglobin (g/dL) (M/F) e | 13.22 (13.64/12.64) | nd | <0.0001 |
| Non-anemic/anemic (no/%) | 193/147 (57/43) | nd | |
| BMI (Kg/m2) | 18.36 | 22.71 | <0.0001 |
| MUAC (mm) | 21.87 | 25.83 | <0.0001 |
| 25(OH)D3 nmol/L | 35.28 | 32.47 | 0.190 |
| ESR (mm/hour) | 41.83 | nd | |
| WBC counts (109 cells/L) | 7.87 | nd | |
| CD4 T cell counts (cells/mm3) | 499 | 668 | < 0.0001 |
| CD8 T cell counts (cells/mm3) | 442 | 538 | < 0.0032 |
| IFN-γ (IU) f | 3.72 | 2.93 | 0.198 |
| TB Score | n | Difference a | 95% CI b | p-Value |
|---|---|---|---|---|
| Age | 346 | 1.15 | (−0.01 to 0.03) | 0.253 |
| Sex | 346 | −0.03 | (−0.47 to 0.39) | 0.868 |
| Hemoglobin | 341 | −6.45 | (−0.50 to −0.27) | <0.0001 |
| BMI | 346 | −13.08 | (−0.56 to −0.42) | <0.0001 |
| ESR | 336 | 1.75 | (−0.00 to 0.02) | 0.081 |
| 25(OH)D3 | 343 | 0.30 | (−0.01 to 0.01) | 0.761 |
| CD4 T cell count | 334 | −0.85 | (−0.00 to 0.00) | 0.396 |
| CD8 T cell count | 332 | 0.74 | (−0.00 to 0.00) | 0.458 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ashenafi, S.; Bekele, A.; Aseffa, G.; Amogne, W.; Kassa, E.; Aderaye, G.; Worku, A.; Bergman, P.; Brighenti, S. Anemia Is a Strong Predictor of Wasting, Disease Severity, and Progression, in Clinical Tuberculosis (TB). Nutrients 2022, 14, 3318. https://doi.org/10.3390/nu14163318
Ashenafi S, Bekele A, Aseffa G, Amogne W, Kassa E, Aderaye G, Worku A, Bergman P, Brighenti S. Anemia Is a Strong Predictor of Wasting, Disease Severity, and Progression, in Clinical Tuberculosis (TB). Nutrients. 2022; 14(16):3318. https://doi.org/10.3390/nu14163318
Chicago/Turabian StyleAshenafi, Senait, Amsalu Bekele, Getachew Aseffa, Wondwossen Amogne, Endale Kassa, Getachew Aderaye, Alemayehu Worku, Peter Bergman, and Susanna Brighenti. 2022. "Anemia Is a Strong Predictor of Wasting, Disease Severity, and Progression, in Clinical Tuberculosis (TB)" Nutrients 14, no. 16: 3318. https://doi.org/10.3390/nu14163318
APA StyleAshenafi, S., Bekele, A., Aseffa, G., Amogne, W., Kassa, E., Aderaye, G., Worku, A., Bergman, P., & Brighenti, S. (2022). Anemia Is a Strong Predictor of Wasting, Disease Severity, and Progression, in Clinical Tuberculosis (TB). Nutrients, 14(16), 3318. https://doi.org/10.3390/nu14163318







