Appraising the Causal Association between Systemic Iron Status and Heart Failure Risk: A Mendelian Randomisation Study
Abstract
:1. Introduction
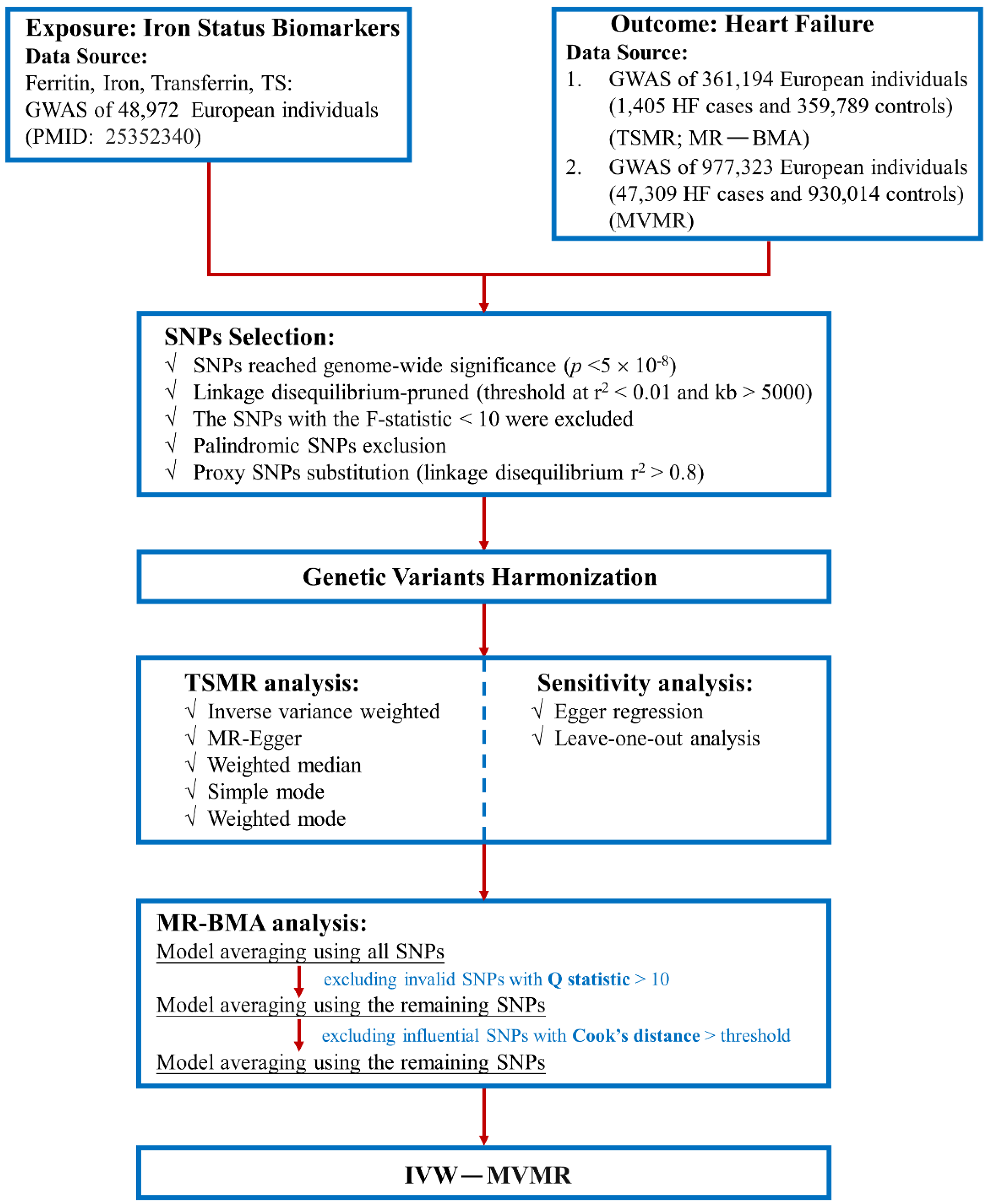
2. Materials and Methods
2.1. Study Design and Data Source
2.2. SNP Selection and Validation
2.3. MR Estimates
2.4. Sensitivity Analysis
2.5. MR-BMA Estimates
2.6. MVMR Analysis
2.7. MR Analysis of Diseases with Abnormal Iron Status
3. Results
3.1. SNP Selection and Validation
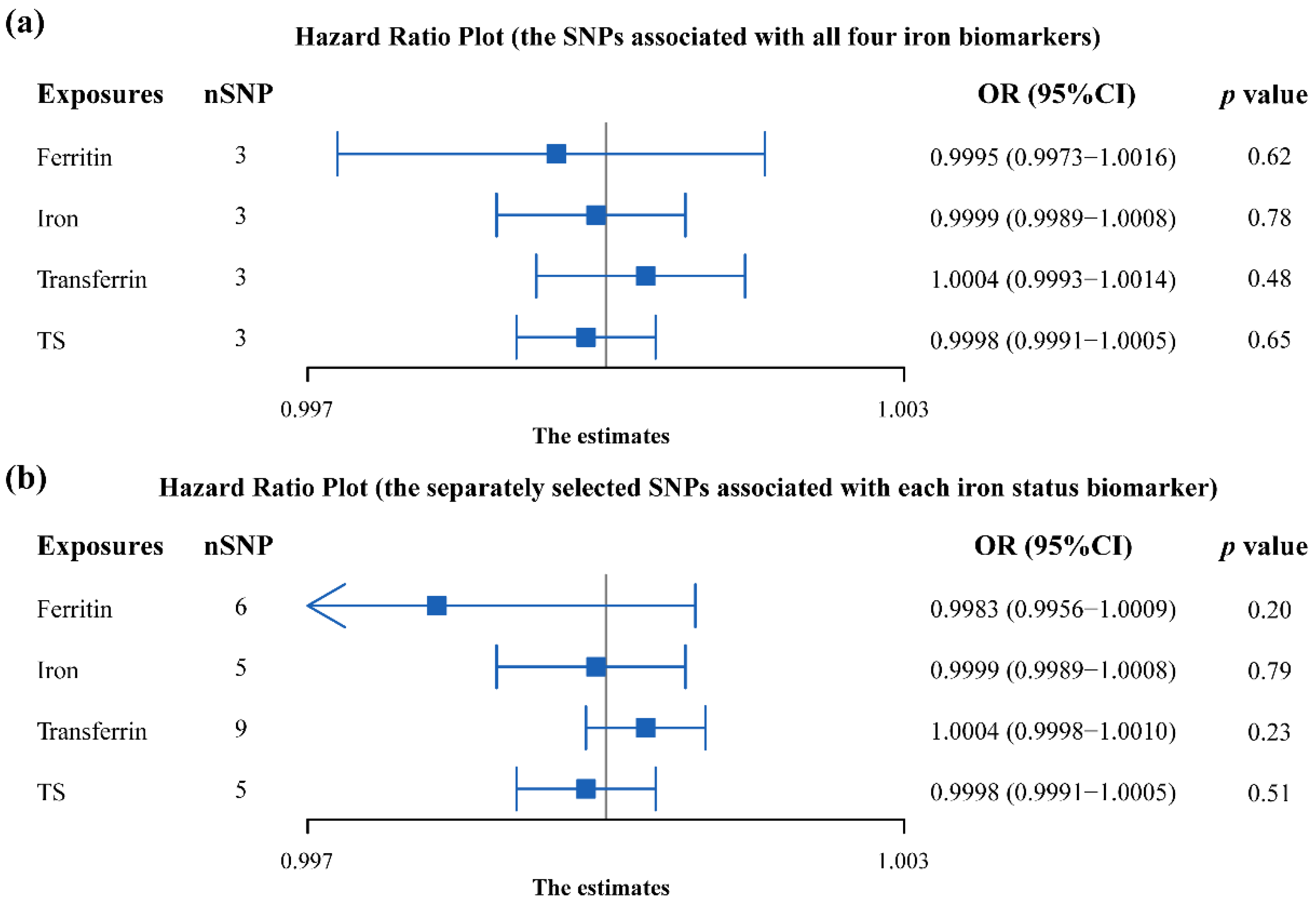
3.2. Analysis Using the Two-Sample MR
3.3. Sensitivity Analysis
3.4. Analysis Using the MR-BMA
3.5. Analysis Using the MVMR
3.6. MR Analysis of Diseases with Abnormal Iron Status
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Crespo-Leiro, M.G.; Metra, M.; Lund, L.H.; Milicic, D.; Costanzo, M.R.; Filippatos, G.; Gustafsson, F.; Tsui, S.; Barge-Caballero, E.; De Jonge, N.; et al. Advanced heart failure: A position statement of the Heart Failure Association of the European Society of Cardiology. Eur. J. Heart Fail. 2018, 20, 1505–1535. [Google Scholar] [CrossRef]
- Bauersachs, J.; de Boer, R.A.; Lindenfeld, J.; Bozkurt, B. The year in cardiovascular medicine 2021: Heart failure and cardiomyopathies. Eur. Heart J. 2022, 17, 27–43. [Google Scholar] [CrossRef]
- Ziaeian, B.; Fonarow, G.C. Epidemiology and aetiology of heart failure. Nat. Rev. Cardiol. 2016, 13, 368–378. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zhang, Y.; Yuan, M.; Gong, M.; Li, G.; Liu, T.; Tse, G. Associations Between Prefrailty or Frailty Components and Clinical Outcomes in Heart Failure: A Follow-up Meta-analysis. J. Am. Med. Dir. Assoc. 2019, 20, 509–510. [Google Scholar] [CrossRef] [PubMed]
- De Boer, R.A.; Nayor, M.; de Filippi, C.R.; Enserro, D.; Bhambhani, V.; Kizer, J.R.; Blaha, M.J.; Brouwers, F.P.; Cushman, M.; Lima, J.A.C.; et al. Association of Cardiovascular Biomarkers With Incident Heart Failure With Preserved and Reduced Ejection Fraction. JAMA Cardiol. 2018, 3, 215–224. [Google Scholar] [CrossRef] [Green Version]
- Nazanin Abbaspour, R.H.; Kelishadi, R. Review on iron and its importance for human health. J. Res. Med. Sci. 2014, 19, 164–174. [Google Scholar]
- Zimmermann, M.B.; Hurrell, R.F. Nutritional iron deficiency. Lancet 2007, 370, 511–520. [Google Scholar] [CrossRef]
- Jacob, C.; Altevers, J.; Barck, I.; Hardt, T.; Braun, S.; Greiner, W. Retrospective analysis into differences in heart failure patients with and without iron deficiency or anaemia. ESC Heart Fail. 2019, 6, 840–855. [Google Scholar] [CrossRef]
- Cappellini, M.D.; Comin-Colet, J.; de Francisco, A.; Dignass, A.; Doehner, W.; Lam, C.S.; Macdougall, I.C.; Rogler, G.; Camaschella, C.; Kadir, R.; et al. Iron deficiency across chronic inflammatory conditions: International expert opinion on definition, diagnosis, and management. Am. J. Hematol. 2017, 92, 1068–1078. [Google Scholar] [CrossRef] [Green Version]
- Ponikowski, P.; Jankowska, E.A. Targeting Iron Deficiency in Heart Failure: Existing Evidence and Future Expectations. Circ. Heart Fail. 2021, 14, e008299. [Google Scholar] [CrossRef]
- Kurz, K.; Lanser, L.; Seifert, M.; Kocher, F.; Polzl, G.; Weiss, G. Anaemia, iron status, and gender predict the outcome in patients with chronic heart failure. ESC Heart Fail. 2020, 7, 1880–1890. [Google Scholar] [CrossRef]
- Anand, I.S.; Gupta, P. Anemia and Iron Deficiency in Heart Failure: Current Concepts and Emerging Therapies. Circulation 2018, 138, 80–98. [Google Scholar] [CrossRef]
- Lin, F.; Huang, Y.; An, D.; Zhan, Q.; Wang, P.; Lai, W.; Zeng, Q.; Dong, S.; Ren, H.; Xu, D. Iron deficiency is an independent risk factor of increased myocardial energy expenditure in chronic heart failure patients. Ann. Palliat. Med. 2021, 10, 12061–12071. [Google Scholar] [CrossRef]
- Silvestre, O.M.; Goncalves, A.; Nadruz, W., Jr.; Claggett, B.; Couper, D.; Eckfeldt, J.H.; Pankow, J.S.; Anker, S.D.; Solomon, S.D. Ferritin levels and risk of heart failure-the Atherosclerosis Risk in Communities Study. Eur. J. Heart Fail. 2017, 19, 340–347. [Google Scholar] [CrossRef] [Green Version]
- Klip, I.T.; Voors, A.A.; Swinkels, D.W.; Bakker, S.J.; Kootstra-Ros, J.E.; Lam, C.S.; van der Harst, P.; van Veldhuisen, D.J.; van der Meer, P. Serum ferritin and risk for new-onset heart failure and cardiovascular events in the community. Eur. J. Heart Fail. 2017, 19, 348–356. [Google Scholar] [CrossRef]
- Dong, F.; Zhang, X.; Culver, B.; Chew, H.G., Jr.; Kelley, R.O.; Ren, J. Dietary iron deficiency induces ventricular dilation, mitochondrial ultrastructural aberrations and cytochrome c release: Involvement of nitric oxide synthase and protein tyrosine nitration. Clin. Sci. 2005, 109, 277–286. [Google Scholar] [CrossRef] [Green Version]
- Das, S.K.; Wang, W.; Zhabyeyev, P.; Basu, R.; McLean, B.; Fan, D.; Parajuli, N.; DesAulniers, J.; Patel, V.B.; Hajjar, R.J.; et al. Iron-overload injury and cardiomyopathy in acquired and genetic models is attenuated by resveratrol therapy. Sci. Rep. 2015, 5, 18132. [Google Scholar] [CrossRef] [Green Version]
- Davey Smith, G.; Hemani, G. Mendelian randomization: Genetic anchors for causal inference in epidemiological studies. Hum. Mol. Genet. 2014, 23, R89–R98. [Google Scholar] [CrossRef] [Green Version]
- Davies, N.M.; Holmes, M.V.; Davey Smith, G. Reading Mendelian randomisation studies: A guide, glossary, and checklist for clinicians. BMJ 2018, 362, k601. [Google Scholar] [CrossRef] [Green Version]
- Richmond, R.C.; Davey Smith, G. Mendelian Randomization: Concepts and Scope. Cold Spring Harb. Perspect. Med. 2022, 12, a040501. [Google Scholar] [CrossRef]
- Benyamin, B.; Esko, T.; Ried, J.S.; Radhakrishnan, A.; Vermeulen, S.H.; Traglia, M.; Gogele, M.; Anderson, D.; Broer, L.; Podmore, C.; et al. Novel loci affecting iron homeostasis and their effects in individuals at risk for hemochromatosis. Nat. Commun. 2014, 5, 4926. [Google Scholar] [CrossRef] [Green Version]
- Staley, J.R.; Blackshaw, J.; Kamat, M.A.; Ellis, S.; Surendran, P.; Sun, B.B.; Paul, D.S.; Freitag, D.; Burgess, S.; Danesh, J.; et al. PhenoScanner: A database of human genotype-phenotype associations. Bioinformatics 2016, 32, 3207–3209. [Google Scholar] [CrossRef] [Green Version]
- Machiela, M.J.; Chanock, S.J. LDlink: A web-based application for exploring population-specific haplotype structure and linking correlated alleles of possible functional variants. Bioinformatics 2015, 31, 3555–3557. [Google Scholar] [CrossRef]
- Johnson, A.D.; Handsaker, R.E.; Pulit, S.L.; Nizzari, M.M.; O’Donnell, C.J.; de Bakker, P.I. SNAP: A web-based tool for identification and annotation of proxy SNPs using HapMap. Bioinformatics 2008, 24, 2938–2939. [Google Scholar] [CrossRef] [Green Version]
- Burgess, S.; Thompson, S.G. Use of allele scores as instrumental variables for Mendelian randomization. Int. J. Epidemiol. 2013, 42, 1134–1144. [Google Scholar] [CrossRef] [Green Version]
- Burgess, S.; Butterworth, A.; Thompson, S.G. Mendelian randomization analysis with multiple genetic variants using summarized data. Genet. Epidemiol. 2013, 37, 658–665. [Google Scholar] [CrossRef] [Green Version]
- Bowden, J.; Davey Smith, G.; Burgess, S. Mendelian randomization with invalid instruments: Effect estimation and bias detection through Egger regression. Int. J. Epidemiol. 2015, 44, 512–525. [Google Scholar] [CrossRef] [Green Version]
- Burgess, S.; Thompson, S.G. Interpreting findings from Mendelian randomization using the MR-Egger method. Eur. J. Epidemiol. 2017, 32, 377–389. [Google Scholar] [CrossRef] [Green Version]
- Zuber, V.; Colijn, J.M.; Klaver, C.; Burgess, S. Selecting likely causal risk factors from high-throughput experiments using multivariable Mendelian randomization. Nat. Commun. 2020, 11, 29. [Google Scholar] [CrossRef] [Green Version]
- Efron, B.; Hastie, T.; Johnstone, I.; Tibshirani, R. Least angle regression. Ann. Stat. 2004, 32, 407–499. [Google Scholar] [CrossRef] [Green Version]
- Cook, R.D. Influential Observations in Linear Regression. J. Am. Stat. Assoc. 1979, 74, 169–174. [Google Scholar] [CrossRef]
- Burgess, S.; Thompson, S.G. Multivariable Mendelian randomization: The use of pleiotropic genetic variants to estimate causal effects. Am. J. Epidemiol. 2015, 181, 251–260. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shah, S.; Henry, A.; Roselli, C.; Lin, H.; Sveinbjornsson, G.; Fatemifar, G.; Hedman, A.K.; Wilk, J.B.; Morley, M.P.; Chaffin, M.D.; et al. Genome-wide association and Mendelian randomisation analysis provide insights into the pathogenesis of heart failure. Nat. Commun. 2020, 11, 163. [Google Scholar] [CrossRef] [PubMed]
- Soranzo, N.; Sanna, S.; Wheeler, E.; Gieger, C.; Radke, D.; Dupuis, J.; Bouatia-Naji, N.; Langenberg, C.; Prokopenko, I.; Stolerman, E.; et al. Common variants at 10 genomic loci influence hemoglobin A(1)(C) levels via glycemic and nonglycemic pathways. Diabetes 2010, 59, 3229–3239. [Google Scholar] [CrossRef] [Green Version]
- Wheeler, E.; Leong, A.; Liu, C.T.; Hivert, M.F.; Strawbridge, R.J.; Podmore, C.; Li, M.; Yao, J.; Sim, X.; Hong, J.; et al. Impact of common genetic determinants of Hemoglobin A1c on type 2 diabetes risk and diagnosis in ancestrally diverse populations: A transethnic genome-wide meta-analysis. PLoS Med. 2017, 14, e1002383. [Google Scholar] [CrossRef] [Green Version]
- Willer, C.J.; Schmidt, E.M.; Sengupta, S.; Peloso, G.M.; Gustafsson, S.; Kanoni, S.; Ganna, A.; Chen, J.; Buchkovich, M.L.; Mora, S.; et al. Discovery and refinement of loci associated with lipid levels. Nat. Genet. 2013, 45, 1274–1283. [Google Scholar] [CrossRef] [Green Version]
- Wain, L.V.; Vaez, A.; Jansen, R.; Joehanes, R.; van der Most, P.J.; Erzurumluoglu, A.M.; O’Reilly, P.F.; Cabrera, C.P.; Warren, H.R.; Rose, L.M.; et al. Novel Blood Pressure Locus and Gene Discovery Using Genome-Wide Association Study and Expression Data Sets From Blood and the Kidney. Hypertension 2017, 70, e4–e19. [Google Scholar] [CrossRef] [Green Version]
- Surendran, P.; Drenos, F.; Young, R.; Warren, H.; Cook, J.P.; Manning, A.K.; Grarup, N.; Sim, X.; Barnes, D.R.; Witkowska, K.; et al. Trans-ancestry meta-analyses identify rare and common variants associated with blood pressure and hypertension. Nat. Genet. 2016, 48, 1151–1161. [Google Scholar] [CrossRef]
- Gill, D.; Del Greco, M.F.; Walker, A.P.; Srai, S.K.S.; Laffan, M.A.; Minelli, C. The Effect of Iron Status on Risk of Coronary Artery Disease: A Mendelian Randomization Study-Brief Report. Arterioscler. Thromb. Vasc. Biol. 2017, 37, 1788–1792. [Google Scholar] [CrossRef] [Green Version]
- Zhu, Y.; Chen, G.; Bo, Y.; Liu, Y. Markers of iron status, blood pressure and incident hypertension among Chinese adults. Nutr. Metab. Cardiovasc. Dis. 2019, 29, 830–836. [Google Scholar] [CrossRef]
- Lee, D.H.; Kang, S.K.; Choi, W.J.; Kwak, K.M.; Kang, D.; Lee, S.H.; Lee, J.H. Association between serum ferritin and hypertension according to the working type in Korean men: The fifth Korean National Health and nutrition examination survey 2010–2012. Ann. Occup. Environ. Med. 2018, 30, 40. [Google Scholar] [CrossRef] [PubMed]
- Wang, X.; Fang, X.; Zheng, W.; Zhou, J.; Song, Z.; Xu, M.; Min, J.; Wang, F. Genetic Support of A Causal Relationship Between Iron Status and Type 2 Diabetes: A Mendelian Randomization Study. J. Clin. Endocrinol. Metab. 2021, 106, e4641–e4651. [Google Scholar] [CrossRef] [PubMed]
- Lawlor, D.A.; Harbord, R.M.; Sterne, J.A.; Timpson, N.; Davey Smith, G. Mendelian randomization: Using genes as instruments for making causal inferences in epidemiology. Stat. Med. 2008, 27, 1133–1163. [Google Scholar] [CrossRef] [PubMed]
- Evans, D.M.; Davey Smith, G. Mendelian Randomization: New Applications in the Coming Age of Hypothesis-Free Causality. Annu. Rev. Genom. Hum. Genet. 2015, 16, 327–350. [Google Scholar] [CrossRef]
- Gupta, V.; Walia, G.K.; Sachdeva, M.P. ‘Mendelian randomization’: An approach for exploring causal relations in epidemiology. Public Health 2017, 145, 113–119. [Google Scholar] [CrossRef]
- Holmes, M.V.; Ala-Korpela, M.; Smith, G.D. Mendelian randomization in cardiometabolic disease: Challenges in evaluating causality. Nat. Rev. Cardiol. 2017, 14, 577–590. [Google Scholar] [CrossRef] [Green Version]
- Girelli, D.; Busti, F.; Brissot, P.; Cabantchik, I.; Muckenthaler, M.U.; Porto, G. Hemochromatosis classification: Update and recommendations by the BIOIRON Society. Blood 2022, 139, 3018–3029. [Google Scholar] [CrossRef]
- Hanson, E.H.; Imperatore, G.; Burke, W. HFE gene and hereditary hemochromatosis: A HuGE review. Human Genome Epidemiology. Am. J. Epidemiol. 2001, 154, 193–206. [Google Scholar] [CrossRef] [Green Version]
- Udani, K.; Chris-Olaiya, A.; Ohadugha, C.; Malik, A.; Sansbury, J.; Paari, D. Cardiovascular manifestations in hospitalized patients with hemochromatosis in the United States. Int. J. Cardiol. 2021, 342, 117–124. [Google Scholar] [CrossRef]
- Ponikowski, P.; Voors, A.A.; Anker, S.D.; Bueno, H.; Cleland, J.G.; Coats, A.J.; Falk, V.; Gonzalez-Juanatey, J.R.; Harjola, V.P.; Jankowska, E.A.; et al. 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: The Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC). Developed with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur. J. Heart Fail. 2016, 18, 891–975. [Google Scholar] [CrossRef]
- Ponikowski, P.; Kirwan, B.-A.; Anker, S.D.; McDonagh, T.; Dorobantu, M.; Drozdz, J.; Fabien, V.; Filippatos, G.; Göhring, U.M.; Keren, A.; et al. Ferric carboxymaltose for iron deficiency at discharge after acute heart failure: A multicentre, double-blind, randomised, controlled trial. Lancet 2020, 396, 1895–1904. [Google Scholar] [CrossRef]
- Martens, P.; Dupont, M.; Dauw, J.; Nijst, P.; Herbots, L.; Dendale, P.; Vandervoort, P.; Bruckers, L.; Tang, W.H.W.; Mullens, W. The effect of intravenous ferric carboxymaltose on cardiac reverse remodelling following cardiac resynchronization therapy-the IRON-CRT trial. Eur. Heart J. 2021, 42, 4905–4914. [Google Scholar] [CrossRef]
- Jankowska, E.A.; Kirwan, B.A.; Kosiborod, M.; Butler, J.; Anker, S.D.; McDonagh, T.; Dorobantu, M.; Drozdz, J.; Filippatos, G.; Keren, A.; et al. The effect of intravenous ferric carboxymaltose on health-related quality of life in iron-deficient patients with acute heart failure: The results of the AFFIRM-AHF study. Eur. Heart J. 2021, 42, 3011–3020. [Google Scholar] [CrossRef]
- Kremastinos, D.T.; Farmakis, D. Iron overload cardiomyopathy in clinical practice. Circulation 2011, 124, 2253–2263. [Google Scholar] [CrossRef] [Green Version]
- Paterek, A.; Okninska, M.; Chajduk, E.; Polkowska-Motrenko, H.; Maczewski, M.; Mackiewicz, U. Systemic iron deficiency does not affect the cardiac iron content and progression of heart failure. J. Mol. Cell. Cardiol. 2021, 159, 16–27. [Google Scholar] [CrossRef]
- Hirsch, V.G.; Tongers, J.; Bode, J.; Berliner, D.; Widder, J.D.; Escher, F.; Mutsenko, V.; Chung, B.; Rostami, F.; Guba-Quint, A.; et al. Cardiac iron concentration in relation to systemic iron status and disease severity in non-ischaemic heart failure with reduced ejection fraction. Eur. J. Heart Fail. 2020, 22, 2038–2046. [Google Scholar] [CrossRef]
- Paterek, A.; Kepska, M.; Sochanowicz, B.; Chajduk, E.; Kolodziejczyk, J.; Polkowska-Motrenko, H.; Kruszewski, M.; Leszek, P.; Mackiewicz, U.; Maczewski, M. Beneficial effects of intravenous iron therapy in a rat model of heart failure with preserved systemic iron status but depleted intracellular cardiac stores. Sci. Rep. 2018, 8, 15758. [Google Scholar] [CrossRef]
- Tang, D.; Kang, R.; Berghe, T.V.; Vandenabeele, P.; Kroemer, G. The molecular machinery of regulated cell death. Cell Res. 2019, 29, 347–364. [Google Scholar] [CrossRef] [Green Version]
- Wu, X.; Li, Y.; Zhang, S.; Zhou, X. Ferroptosis as a novel therapeutic target for cardiovascular disease. Theranostics 2021, 11, 3052–3059. [Google Scholar] [CrossRef]
- Stockwell, B.R.; Friedmann Angeli, J.P.; Bayir, H.; Bush, A.I.; Conrad, M.; Dixon, S.J.; Fulda, S.; Gascon, S.; Hatzios, S.K.; Kagan, V.E.; et al. Ferroptosis: A Regulated Cell Death Nexus Linking Metabolism, Redox Biology, and Disease. Cell 2017, 171, 273–285. [Google Scholar] [CrossRef] [Green Version]
- Fang, X.; Cai, Z.; Wang, H.; Han, D.; Cheng, Q.; Zhang, P.; Gao, F.; Yu, Y.; Song, Z.; Wu, Q.; et al. Loss of Cardiac Ferritin H Facilitates Cardiomyopathy via Slc7a11-Mediated Ferroptosis. Circ. Res. 2020, 127, 486–501. [Google Scholar] [CrossRef]


| SNP | Nearest Gene | Chr | Position | EA | EAF | F | SNP-Exposures Association | SNP-HF Association | ||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Beta | SE | p | Beta | SE | p | |||||||
| Ferritin | ||||||||||||
| rs1800562 | HFE (C282Y) | 6 | 26,093,141 | A | 0.067 | 256 | 0.204 | 0.016 | 1.54 × 10−38 | −1.74 × 10−04 | 0.00027 | 0.515 |
| rs1799945 | HFE (H63D) | 6 | 26,091,179 | C | 0.85 | 53 | −0.065 | 0.01 | 1.71 × 10−10 | 1.32 × 10−04 | 0.0002 | 0.511 |
| rs855791 | TMPRSS6 (V736A) | 22 | 37,462,936 | A | 0.446 | 73 | −0.055 | 0.007 | 1.38 × 10−14 | −1.02 × 10−04 | 0.00015 | 0.486 |
| rs744653 | WDR75–SLC40A1 | 2 | 1.90 × 1008 | T | 0.854 | 97 | −0.089 | 0.01 | 8.37 × 10−19 | 1.35 × 10−04 | 0.00021 | 0.516 |
| rs651007 | ABO | 9 | 1.36 × 1008 | T | 0.202 | 40 | −0.05 | 0.009 | 1.31 × 10−08 | 5.88 × 10−04 | 0.00018 | 0.001 |
| rs411988 | TEX14 | 17 | 56,709,034 | A | 0.564 | 47 | −0.044 | 0.007 | 1.59 × 10−10 | 1.95 × 10−04 | 0.00015 | 0.178 |
| Iron | ||||||||||||
| rs1800562 | HFE (C282Y) | 6 | 26,093,141 | A | 0.067 | 668 | 0.328 | 0.016 | 2.72 × 10−97 | −1.74 × 10−04 | 0.00027 | 0.515 |
| rs1799945 | HFE (H63D) | 6 | 26,091,179 | C | 0.85 | 450 | −0.189 | 0.01 | 1.10 × 10−81 | 1.32 × 10−04 | 0.0002 | 0.511 |
| rs855791 | TMPRSS6 (V736A) | 22 | 37,462,936 | A | 0.446 | 806 | −0.181 | 0.007 | 1.32 × 10−139 | −1.02 × 10−04 | 0.00015 | 0.486 |
| rs8177240 | TF | 3 | 1.33 × 1008 | T | 0.669 | 95 | −0.066 | 0.007 | 6.65 × 10−20 | −9.63 × 10−05 | 0.00015 | 0.526 |
| rs7385804 | TFR2 | 7 | 1 × 1008 | A | 0.621 | 95 | 0.064 | 0.007 | 1.36 × 10−18 | −9.27 × 10−05 | 0.00015 | 0.533 |
| Transferrin | ||||||||||||
| rs1800562 | HFE (C282Y) | 6 | 26,093,141 | A | 0.067 | 1446 | −0.479 | 0.016 | 8.90 × 10−196 | −1.74 × 10−04 | 0.00027 | 0.515 |
| rs1799945 | HFE (H63D) | 6 | 26,091,179 | C | 0.85 | 163 | 0.114 | 0.01 | 9.36 × 10−30 | 1.32 × 10−04 | 0.0002 | 0.511 |
| rs855791 | TMPRSS6 (V736A) | 22 | 37,462,936 | A | 0.446 | 47 | 0.044 | 0.007 | 1.98 × 10−09 | −1.02 × 10−04 | 0.00015 | 0.486 |
| rs744653 | WDR75–SLC40A1 | 2 | 1.9 × 1008 | T | 0.854 | 57 | 0.068 | 0.01 | 1.35 × 10−11 | 1.35 × 10−04 | 0.00021 | 0.516 |
| rs8177240 | TF | 3 | 1.33 × 1008 | T | 0.669 | 3346 | −0.38 | 0.007 | 8.43 × 10−610 | −9.63 × 10−05 | 0.00015 | 0.526 |
| rs9990333 | TFRC | 3 | 1.96 × 1008 | T | 0.46 | 63 | −0.051 | 0.007 | 1.95 × 10−13 | −6.56 × 10−05 | 0.00014 | 0.651 |
| rs4921915 | NAT2 | 8 | 18,272,466 | A | 0.782 | 104 | 0.079 | 0.009 | 7.05 × 10−19 | −8.05 × 10−05 | 0.00017 | 0.643 |
| rs6486121 | ARNTL | 11 | 13,355,770 | T | 0.631 | 48 | −0.046 | 0.007 | 3.89 × 10−10 | −2.03 × 10−04 | 0.00015 | 0.176 |
| rs174577 | FADS2 | 11 | 61,604,814 | A | 0.33 | 83 | 0.062 | 0.007 | 2.28 × 10−17 | 1.45 × 10−04 | 0.00015 | 0.338 |
| TS | ||||||||||||
| rs1800562 | HFE (C282Y) | 6 | 26,093,141 | A | 0.067 | 2127 | 0.577 | 0.016 | 2.19 × 10−270 | −1.74 × 10−04 | 0.00027 | 0.515 |
| rs1799945 | HFE (H63D) | 6 | 26,091,179 | C | 0.85 | 676 | −0.231 | 0.01 | 5.13 × 10−109 | 1.32 × 10−04 | 0.0002 | 0.511 |
| rs855791 | TMPRSS6 (V736A) | 22 | 37,462,936 | A | 0.446 | 889 | −0.19 | 0.008 | 6.41 × 10−137 | −1.02 × 10−04 | 0.00015 | 0.486 |
| rs8177240 | TF | 3 | 1.33 × 1008 | T | 0.669 | 218 | 0.1 | 0.008 | 7.24 × 10−38 | −9.63 × 10−05 | 0.00015 | 0.526 |
| rs7385804 | TFR2 | 7 | 1 × 1008 | A | 0.621 | 67 | 0.054 | 0.008 | 6.07 × 10−12 | −9.27 × 10−05 | 0.00015 | 0.533 |
| Risk Factor for Model | Ranking by MIP | MIP | ˆθMACE | Ranking by PP | PP | ˆθλ | p |
|---|---|---|---|---|---|---|---|
| Model averaging employing 12 SNPs | |||||||
| Ferritin | 1 | 0.771 | −0.001 | 1 | 0.769 | −0.002 | 0.059 |
| Iron | 3 | 0.079 | 0 | 3 | 0.078 | 0 | 0.881 |
| Transferrin | 2 | 0.081 | 0 | 2 | 0.081 | 0 | 0.832 |
| TS | 4 | 0.071 | 0 | 4 | 0.07 | 0 | 0.941 |
| Model averaging employing 11 SNPs (excluding invalid instrument rs651007 with Q-statistic exceed 10) | |||||||
| Ferritin | 1 | 0.652 | −0.001 | 1 | 0.651 | −0.001 | 0.079 |
| Iron | 4 | 0.081 | 0 | 4 | 0.081 | 0 | 0.921 |
| Transferrin | 2 | 0.172 | 0 | 2 | 0.172 | 0 | 0.337 |
| TS | 3 | 0.096 | 0 | 3 | 0.095 | 0 | 0.941 |
| Model averaging employing 10 SNPs (excluding influential instrument rs1800562 with Cook’s distance exceeding the threshold) | |||||||
| Ferritin | 1 | 0.680 | −0.001 | 1 | 0.679 | −0.002 | 0.099 |
| Iron | 4 | 0.093 | 0 | 4 | 0.093 | 0 | 0.891 |
| Transferrin | 2 | 0.131 | 0 | 2 | 0.131 | 0 | 0.475 |
| TS | 3 | 0.097 | 0 | 3 | 0.097 | 0 | 0.921 |
| Exposures | nSNP | Beta | SE | p Value |
|---|---|---|---|---|
| Iron status biomarkers | ||||
| Ferritin | 3 | 0.050 | 0.134 | 0.709 |
| Iron | 3 | 2.320 | 1.429 | 0.104 |
| Transferrin | 8 | −0.947 | 0.587 | 0.107 |
| Transferrin saturation | 3 | −2.442 | 1.493 | 0.102 |
| Iron status biomarkers and risk factors | ||||
| Ferritin | 2 | −0.080 | 0.063 | 0.199 |
| Iron | 3 | 0.312 | 0.242 | 0.198 |
| Transferrin | 6 | −0.134 | 0.102 | 0.190 |
| Transferrin saturation | 3 | −0.310 | 0.255 | 0.224 |
| Coronary heart disease | 12 | 0.280 | 0.027 | 2.420 × 10−24 |
| Diastolic pressure | 199 | 0.022 | 0.005 | 1.310 × 10−05 |
| Low density lipoprotein | 45 | 0.104 | 0.064 | 0.106 |
| HbA1c | 6 | 0.021 | 0.121 | 0.864 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wang, X.; Wang, X.; Gong, Y.; Chen, X.; Zhong, D.; Zhu, J.; Zhuang, L.; Gao, J.; Fu, G.; Lu, X.; et al. Appraising the Causal Association between Systemic Iron Status and Heart Failure Risk: A Mendelian Randomisation Study. Nutrients 2022, 14, 3258. https://doi.org/10.3390/nu14163258
Wang X, Wang X, Gong Y, Chen X, Zhong D, Zhu J, Zhuang L, Gao J, Fu G, Lu X, et al. Appraising the Causal Association between Systemic Iron Status and Heart Failure Risk: A Mendelian Randomisation Study. Nutrients. 2022; 14(16):3258. https://doi.org/10.3390/nu14163258
Chicago/Turabian StyleWang, Xingchen, Xizhi Wang, Yingchao Gong, Xiaoou Chen, Danfeng Zhong, Jun Zhu, Lenan Zhuang, Jing Gao, Guosheng Fu, Xue Lu, and et al. 2022. "Appraising the Causal Association between Systemic Iron Status and Heart Failure Risk: A Mendelian Randomisation Study" Nutrients 14, no. 16: 3258. https://doi.org/10.3390/nu14163258
APA StyleWang, X., Wang, X., Gong, Y., Chen, X., Zhong, D., Zhu, J., Zhuang, L., Gao, J., Fu, G., Lu, X., & Lai, D. (2022). Appraising the Causal Association between Systemic Iron Status and Heart Failure Risk: A Mendelian Randomisation Study. Nutrients, 14(16), 3258. https://doi.org/10.3390/nu14163258







