Utilization of Small Dense Low-Density Lipoprotein Cholesterol Testing in Korean Patients Visiting Local Clinics and Hospitals
Abstract
:1. Introduction
2. Materials and Methods
3. Results
3.1. Baseline Characteristics of the Subjects
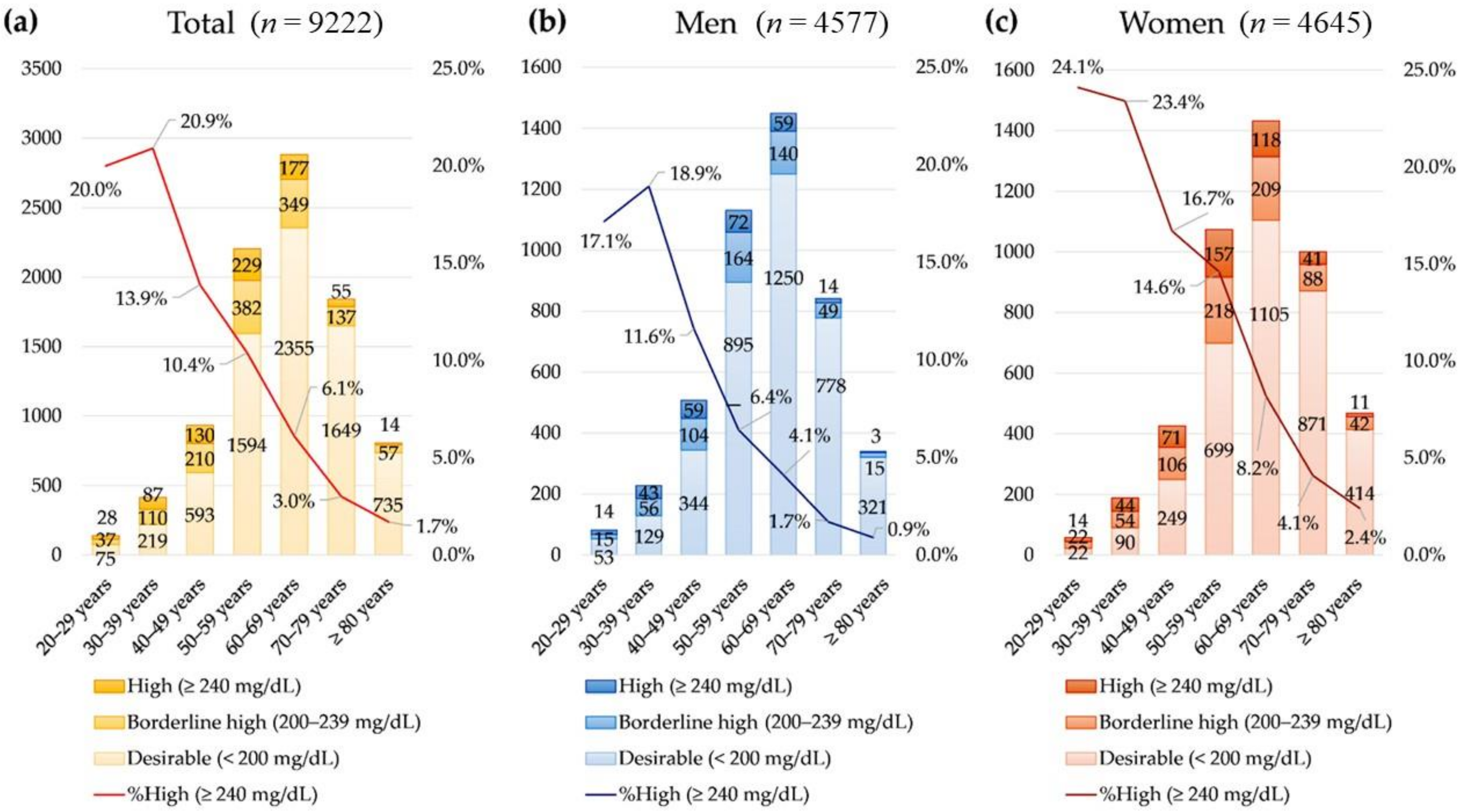
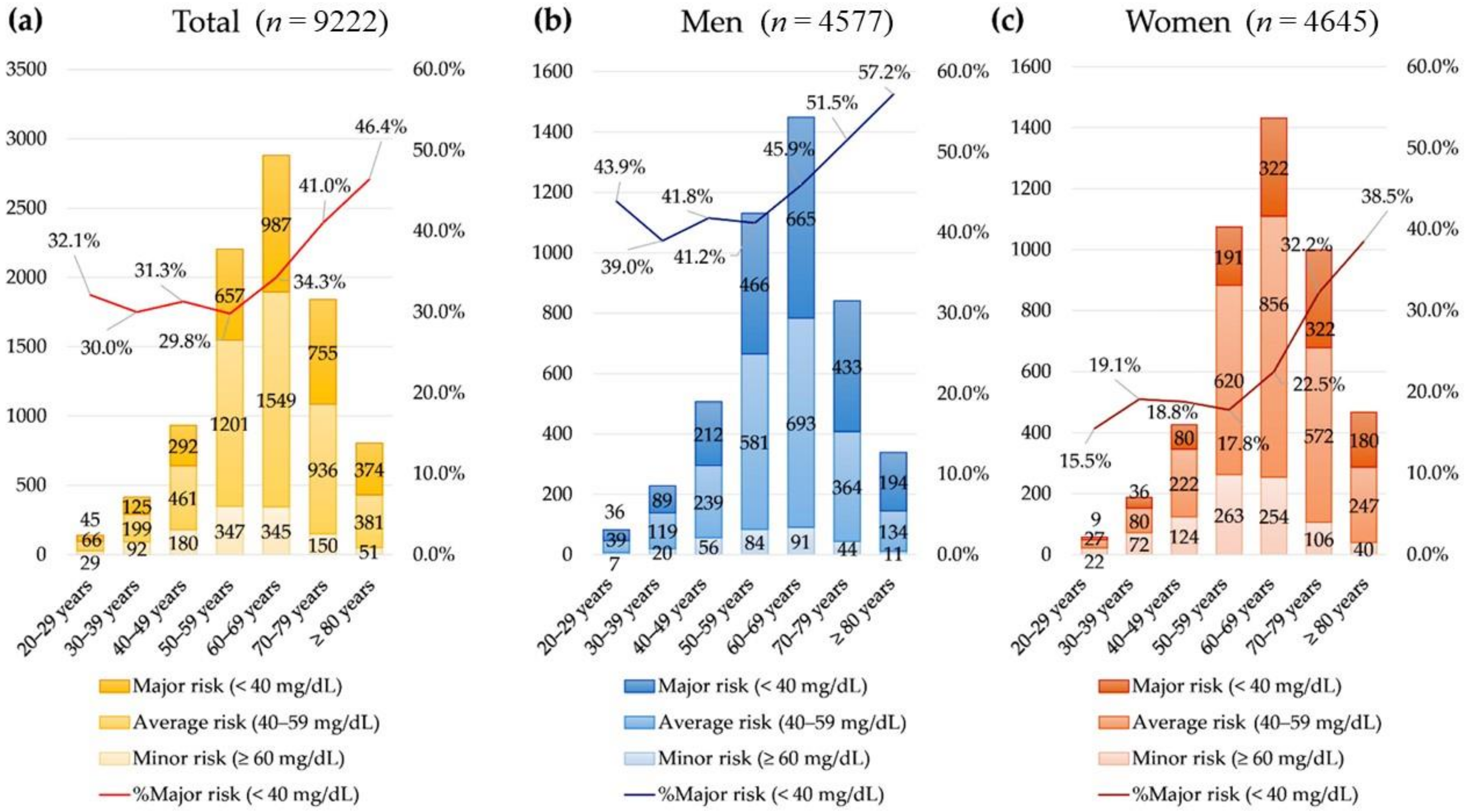
3.2. Lipid Test Results
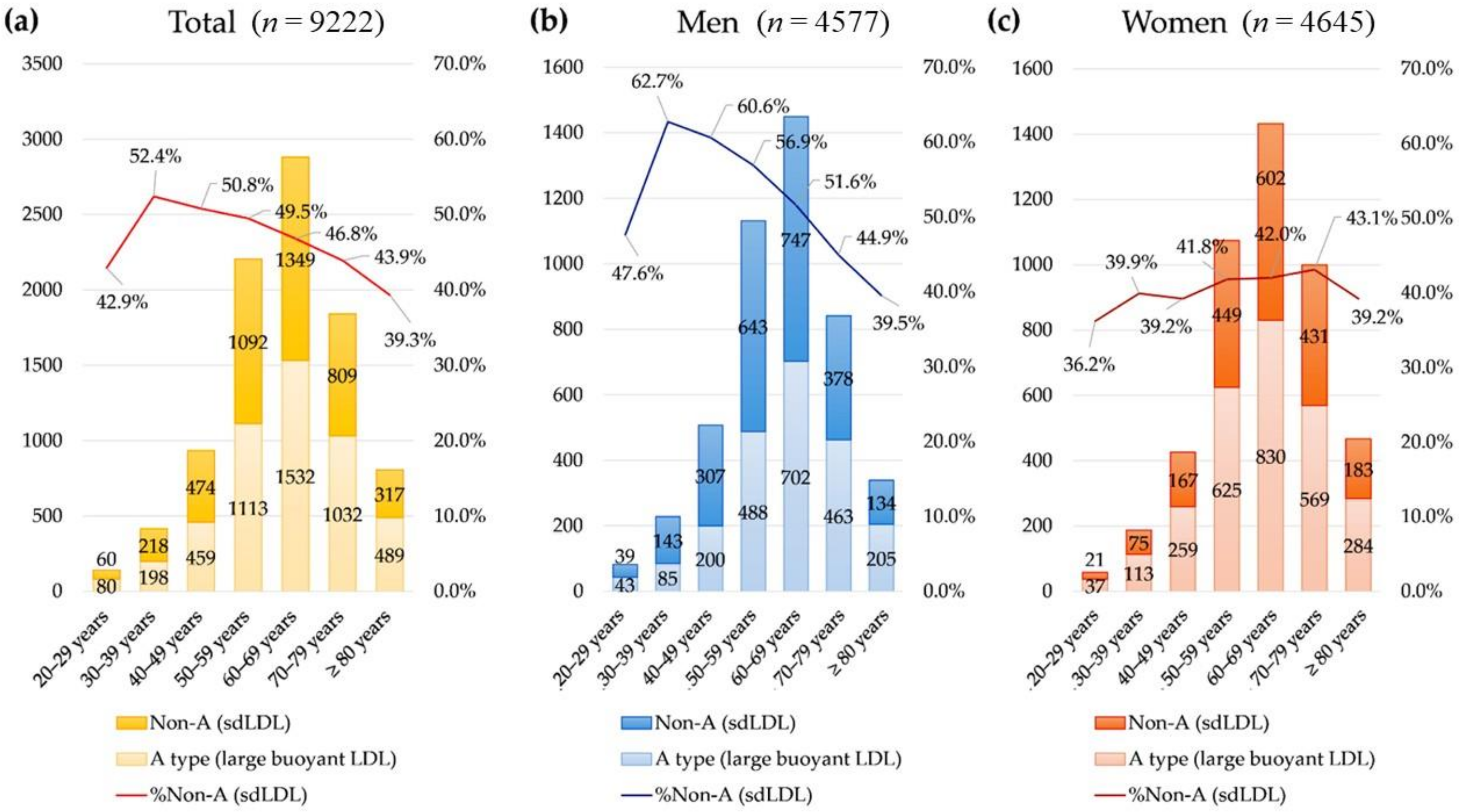
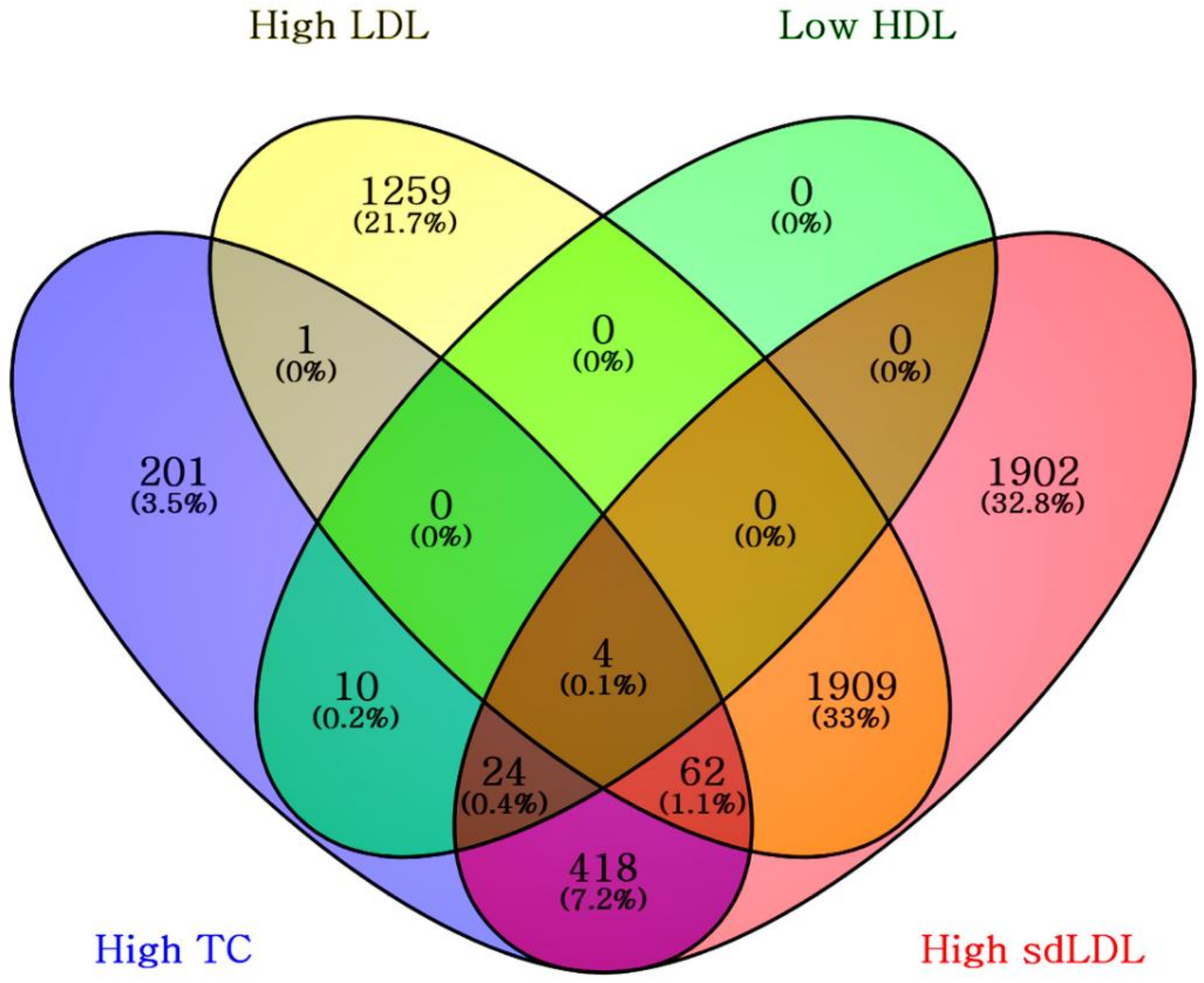
3.3. Presence of Small Dense LDL in Addition to Conventional Lipids
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III). Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) final report. Circulation 2002, 106, 3143–3421. [Google Scholar] [CrossRef]
- Sampson, M.; Wolska, A.; Warnick, R.; Lucero, D.; Remaley, A.T. A New Equation Based on the Standard Lipid Panel for Calculating Small Dense Low-Density Lipoprotein-Cholesterol and Its Use as a Risk-Enhancer Test. Clin. Chem. 2021, 67, 987–997. [Google Scholar] [CrossRef] [PubMed]
- Michos, E.D.; McEvoy, J.W.; Blumenthal, R.S. Lipid Management for the Prevention of Atherosclerotic Cardiovascular Disease. N. Engl. J. Med. 2019, 381, 1557–1567. [Google Scholar] [CrossRef] [PubMed]
- Rizvi, A.A.; Stoian, A.P.; Janez, A.; Rizzo, M. Lipoproteins and Cardiovascular Disease: An Update on the Clinical Significance of Atherogenic Small, Dense LDL and New Therapeutical Options. Biomedicines 2021, 9, 1579. [Google Scholar] [CrossRef] [PubMed]
- Choi, R.; Lee, S.G.; Lee, E.H. Lipoprotein(a) in the Korean Pediatric Population Visiting Local Clinics and Hospitals. Nutrients 2022, 14, 2820. [Google Scholar] [CrossRef] [PubMed]
- Choi, R.; Park, M.-J.; Oh, Y.; Kim, S.H.; Lee, S.G.; Lee, E.H. Validation of multiple equations for estimating low-density lipoprotein cholesterol levels in Korean adults. Lipids Health Dis. 2021, 20, 111. [Google Scholar] [CrossRef] [PubMed]
- Gerber, P.A.; Nikolic, D.; Rizzo, M. Small, dense LDL: An update. Curr. Opin. Cardiol. 2017, 32, 454–459. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Superko, H.; Garrett, B. Small Dense LDL: Scientific Background, Clinical Relevance, and Recent Evidence Still a Risk Even with “Normal” LDL-C Levels. Biomedicines 2022, 10, 829. [Google Scholar] [CrossRef] [PubMed]
- Kwiterovich, P.O., Jr. Clinical relevance of the biochemical, metabolic, and genetic factors that influence low-density lipoprotein heterogeneity. Am. J. Cardiol. 2002, 90, 30i–47i. [Google Scholar] [CrossRef]
- Jin, X.; Yang, S.; Lu, J.; Wu, M. Small, Dense Low-Density Lipoprotein-Cholesterol and Atherosclerosis: Relationship and Therapeutic Strategies. Front. Cardiovasc. Med. 2022, 8, 804214. [Google Scholar] [CrossRef] [PubMed]
- McNamara, J.R.; Small, D.M.; Li, Z.; Schaefer, E.J. Differences in LDL subspecies involve alterations in lipid composition and conformational changes in apolipoprotein B. J. Lipid Res. 1996, 37, 1924–1935. [Google Scholar] [CrossRef]
- Ikezaki, H.; Lim, E.; Cupples, L.A.; Liu, C.T.; Asztalos, B.F.; Schaefer, E.J. Small Dense Low-Density Lipoprotein Cholesterol Is the Most Atherogenic Lipoprotein Parameter in the Prospective Framingham Offspring Study. J. Am. Heart Assoc. 2021, 10, e019140. [Google Scholar] [CrossRef] [PubMed]
- Thongtang, N.; Diffenderfer, M.R.; Ooi, E.M.M.; Barrett, P.H.R.; Turner, S.M.; Le, N.-A.; Brown, W.V.; Schaefer, E.J. Metabolism and proteomics of large and small dense LDL in combined hyperlipidemia: Effects of rosuvastatin. J. Lipid Res. 2017, 58, 1315–1324. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mora, S.; Caulfield, M.; Wohlgemuth, J.; Chen, Z.; Superko, H.R.; Rowland, C.M.; Glynn, R.J.; Ridker, P.M.; Krauss, R.M. Atherogenic Lipoprotein Subfractions Determined by Ion Mobility and First Cardiovascular Events After Random Allocation to High-Intensity Statin or Placebo: The Justification for the Use of Statins in Prevention: An Intervention Trial Evaluating Rosuvastatin (JUPITER) Trial. Circulation. 2015, 132, 2220–2229. [Google Scholar] [PubMed] [Green Version]
- Kinoshita, M.; Yokote, K.; Arai, H.; Iida, M.; Ishigaki, Y.; Ishibashi, S.; Umemoto, S.; Egusa, G.; Ohmura, H.; Okamura, T.; et al. Japan Atherosclerosis Society (JAS) Guidelines for Prevention of Atherosclerotic Cardiovascular Diseases 2017. J. Atheroscler. Thromb. 2018, 25, 846–984. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rhee, E.-J.; Kim, H.C.; Kim, J.H.; Lee, E.Y.; Kim, B.J.; Kim, E.M.; Song, Y.; Lim, J.H.; Kim, H.J.; Choi, S.; et al. 2018 Guidelines for the management of dyslipidemia. Korean J. Intern. Med. 2019, 34, 723–771. [Google Scholar] [CrossRef] [Green Version]
- Huh, H.J.; Park, B.T.; Lee, S.Y.; Kang, E.S.; Park, H.D. Establishing reference intervals for LDL subfractions in a Korean population using the Lipoprint LDL system. Clin. Chem. Lab. Med. 2013, 51, e179–e182. [Google Scholar] [CrossRef] [PubMed]
- Cho, S.M.J.; Lee, H.; Lee, H.H.; Baek, J.; Heo, J.E.; Joo, H.J.; Hong, S.J.; Kim, H.C. Dyslipidemia Fact Sheets in Korea 2020: An Analysis of Nationwide Population-based Data. J. Lipid Atheroscler. 2021, 10, 202–209. [Google Scholar] [CrossRef]
| Characteristics | Total (n = 9222) | Men (n = 4577) | Women (n = 4645) | |
|---|---|---|---|---|
| Age, years (median, IQR) | 62.8 (54.5 to 71.8) | 62.0 (53.2 to 70.5) | 63.7 (55.8 to 73.0) | |
| Age group (n, %) | 20–29 years | 140 (1.5%) | 82 (1.8%) | 58 (1.2%) |
| 30–39 years | 416 (4.5%) | 228 (5.0%) | 188 (4.0%) | |
| 40–49 years | 933 (10.1%) | 507 (11.1%) | 426 (9.2%) | |
| 50–59 years | 2205 (23.9%) | 1131 (24.7%) | 1074 (23.1%) | |
| 60–69 years | 2881 (31.2%) | 1449 (31.7%) | 1432 (30.8%) | |
| 70–79 years | 1841 (20.0%) | 841 (18.4%) | 1000 (21.5%) | |
| ≥80 years | 806 (8.7%) | 339 (7.4%) | 467 (10.1%) | |
| Lipid test (median, IQR) | Total cholesterol, mg/dL | 160 (136 to 193) | 153 (131 to 185) | 167 (142 to 201) |
| HDL cholesterol, mg/dL | 44 (37 to 52) | 41 (35 to 48) | 47 (40 to 56) | |
| LDL cholesterol, mg/dL | 51 (38 to 70) | 49 (37 to 67) | 53 (40 to 74) | |
| Small dense LDL cholesterol, mg/dL | 4 (2 to 11) | 5 (2 to 12) | 4 (1 to 10) | |
| Mean LDL absorbance, Å | 268 (264 to 270) | 267 (263 to 270) | 269 (265 to 271) | |
| NCEP ATP III classification (n, %) | ||||
| Total cholesterol | Desirable (<200 mg/dL) | 7220 (78.3%) | 3770 (82.4%) | 3450 (74.3%) |
| Borderline high (200–239 mg/dL) | 1282 (13.9%) | 543 (11.9%) | 739 (15.9% | |
| High (≥240 mg/dL) | 720 (7.8%) | 264 (5.8%) | 456 (9.8%) | |
| HDL cholesterol | Low (major risk, <40 mg/dL) | 1194 (12.9%) | 313 (6.8%) | 881 (19.0%) |
| Average risk (40–59 mg/dL) | 4793 (52.0%) | 2169 (47.4%) | 1140 (24.5%) | |
| High (minor risk, ≥60 mg/dL) | 3235 (35.1%) | 2095 (45.8%) | 4209 (90.6%) | |
| LDL cholesterol | Optimal (<100 mg/dL) | 8517 (92.4%) | 4308 (94.1%) | 4209 (90.6%) |
| Near optimal/above optimal (100–129 mg/dL) | 552 (6.0%) | 222 (4.9%) | 330 (7.1%) | |
| Borderline high (135–159 mg/dL) | 115 (1.2%) | 36 (0.8%) | 79 (1.7%) | |
| High (160–189 mg/dL) | 24 (0.3%) | 9 (0.2%) | 15 (0.3%) | |
| Very high (≥190 mg/dL) | 14 (0.2%) | 2 (<0.1%) | 12 (0.3%) | |
| LDL phenotype (n, %) | Large buoyant LDL predominant (A type, ≥268 Å) | 4903 (53.2%) | 2186 (47.8%) | 2717 (58.5%) |
| Small dense LDL predominant (non-A type, <268 Å) | 4319 (46.8%) | 2391 (52.2%) | 1928 (41.5%) | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Choi, R.; Lee, S.G.; Lee, E.H. Utilization of Small Dense Low-Density Lipoprotein Cholesterol Testing in Korean Patients Visiting Local Clinics and Hospitals. Nutrients 2022, 14, 3246. https://doi.org/10.3390/nu14153246
Choi R, Lee SG, Lee EH. Utilization of Small Dense Low-Density Lipoprotein Cholesterol Testing in Korean Patients Visiting Local Clinics and Hospitals. Nutrients. 2022; 14(15):3246. https://doi.org/10.3390/nu14153246
Chicago/Turabian StyleChoi, Rihwa, Sang Gon Lee, and Eun Hee Lee. 2022. "Utilization of Small Dense Low-Density Lipoprotein Cholesterol Testing in Korean Patients Visiting Local Clinics and Hospitals" Nutrients 14, no. 15: 3246. https://doi.org/10.3390/nu14153246
APA StyleChoi, R., Lee, S. G., & Lee, E. H. (2022). Utilization of Small Dense Low-Density Lipoprotein Cholesterol Testing in Korean Patients Visiting Local Clinics and Hospitals. Nutrients, 14(15), 3246. https://doi.org/10.3390/nu14153246






