Predictive Equation to Estimate Resting Metabolic Rate in Older Chilean Women
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Sample
2.3. Anthropometric Measurements
2.4. Body Composition
2.5. Indirect Calorimetry (IC)
2.6. Adequacy of Predictive Equations with Resting Metabolic Rate Measured by Indirect Calorimetry (RMR IC)
2.7. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Manini, T. Energy expenditure and aging. Ageing Res. Rev. 2010, 9, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Pinheiro, A.; Esteves de Oliveira, F.; Duarte, R.; Esteves, E.; Bressan, J. Energy expenditure: Components and evaluation methods. Nutr. Hosp. 2011, 26, 430–440. [Google Scholar] [CrossRef]
- Mataix, J.; Martínez, J.A. Balance de energía corporal. In Nutrición y Alimentación Humana; Matrix, J., Ed.; Ocean/Ergon: Barcelona, Spain, 2006; pp. 703–722. [Google Scholar]
- Mahan, L.; Escott-Stump, S.; Raymond, J. Dietoterapia de Krause, 12th ed.; Elsevier: Amsterdam, The Netherlands, 2009; p. 1263. [Google Scholar]
- Westerner, K. Control of energy expenditure in humans. Eur. J. Clin. Nutr. 2017, 71, 340–344. [Google Scholar]
- Nelson, K.; Weinsier, R.; Long, C.; Schutz, Y. Prediction of resting energy expenditure from fat-free mass and fat mass. Am. J. Clin. Nutr. 1992, 56, 848–856. [Google Scholar] [CrossRef] [PubMed]
- Rising, R.; Harper, I.; Fontvielle, A.; Ferraro, R.; Spraul, M.; Ravussin, E. Determinants of total daily energy expenditure: Variability in physical activity. Am. J. Clin. Nutr. 1994, 59, 800–804. [Google Scholar] [CrossRef]
- Maury-Sintjago, E.; Rodríguez-Fernández, A.; Parra-Flores, J.; Ruíz-De la Fuente, M. Obese women have a high carbohydrate intake without changes in the resting metabolic rate in the luteal phase. Nutrients 2022, 14, 1997. [Google Scholar] [CrossRef]
- Millet, L.; Barbe, P.; Lafontan, M.; Berlan, M.; Galitzky, J. Catecholamine effects on lipolysis and blood flow in human abdominal and femoral adipose tissue. J. Appl. Physiol. 1998, 85, 181–188. [Google Scholar] [CrossRef]
- Lührmann, P.; Herbert, B.; Neuhäuser-Berthold, N. Effects of fat mass and body fat distribution on resting metabolic rate in the elderly. Metabolism 2001, 50, 972–975. [Google Scholar] [CrossRef] [PubMed]
- Van Gaal, L.; Vanuytsel, J.; Vansant, G.; De Leeuw, I. Sex hormones, body fat distribution, resting metabolic rate and glucose-induced thermogenesis in premenopausal obese women. Int. J. Obes. Relat. Metab. Disord. 1994, 18, 333–338. [Google Scholar]
- Den Besten, C.; Vansant, G.; Weststrate, J.; Deurenberg, P. Resting metabolic rate and diet-induced thermogenesis in abdominal and luteal femoral obese women before and after weight reduction. Am. J. Clin. Nutr. 1988, 47, 840–847. [Google Scholar] [CrossRef]
- Elia, M.; Ritz Stubbs, R. Total energy expenditure in the elderly. Eur. J. Clin. Nutr. 2000, 54, 92–103. [Google Scholar] [CrossRef] [PubMed]
- Zamboni, M.; Zoico, E.; Scartezzini, T.; Mazzali, G.; Tosoni, P.; Zivelonghi, A.; Gallagher, D.; De Pergola, G.; Di Francesco, V.; Bosello, O. Body composition changes in stable-weight elderly subjects: The effect of sex. Aging Clin. Exp. Res. 2003, 15, 321–327. [Google Scholar] [CrossRef]
- Rankinen, T.; Kim, S.; Pérusse, L.; Després, J.; Bouchard, C. The prediction of abdominal visceral fat level from body composition and anthropometry: ROC analysis. Int. J. Obes. Relat. Metab. Disord. 1999, 23, 801–809. [Google Scholar] [CrossRef] [PubMed]
- Compher, C.; Frankenfield, D.; Keim, N.; Roth-Yousey, L. Best practice methods to apply to measurement of resting metabolic rate in adults: A systematic review. J. Am. Diet. Assoc. 2006, 106, 881–903. [Google Scholar] [CrossRef]
- Coper, J.A.; Watrs, A.C.; O’ Briend, M.J.; Luke, A.; Dobratz, J.R.; Earthman, C.P. Assesing validity and reliability of resting metabolic rate in six gas analysis systems. J. Am. Diet. Assoc. 2009, 109, 128–132. [Google Scholar] [CrossRef]
- Harris-Benedict, J. A Biometric Study of Basal Metabolism in Man; Carnegie Institute of Washington: Washington, DC, USA, 1919. [Google Scholar]
- FAO/WHO/UNU. Energy and Protein Requirements; Technical Report Series; World Health Organ: Geneva, Switzerland, 1985. [Google Scholar]
- Mifflin, M.D.; St Jeor, S.T.; Hill, L.A.; Scott, B.J.; Daugherty, S.A.; Koh, Y.O. A new predictive equation for resting energy expenditure in healthy individuals. J. Am. Clin. Nutr. 1990, 51, 241–247. [Google Scholar] [CrossRef] [PubMed]
- Seagle, H.M.; Strain, G.W.; Makris, A.; Reeves, R.S. Position of the American Dietetic Association: Weight management. J. Am. Diet. Assoc. 2009, 109, 330–346. [Google Scholar] [CrossRef] [PubMed]
- Muller, M.J.; Bosy-Westpha, A.L.; Klau, S.; Kreymann, G.; Luhrmann, P.M.; Neuhauser-Berthold, M. World Health Organization equations have shortcomings for predicting resting energy expenditure in person from a modern, affluent population: Generation of a new reference standard from a retrospective analysis of a German database of resting energy expenditure. Am. J. Clin. Nutr. 2004, 80, 1379–1390. [Google Scholar] [CrossRef] [PubMed]
- Johnstone, A.M.; Rance, K.A.; Murison, S.; Duncan, J.; Speakman, J. Additional anthropometric measures may improve the predictability of basal metabolic rate in adult subjects. Eur. J. Clin. Nutr. 2006, 60, 1437–1444. [Google Scholar] [CrossRef]
- Madden, A.; Mulrooney, H.; Shah, S. Estimation of energy expenditure using prediction equations in overweight and obese adults: A systematic review. J. Hum. Nutr. Diet. 2016, 29, 458–476. [Google Scholar] [CrossRef] [PubMed]
- Khalaj Hedayati, K.; Dittmar, M. Body circumferences are predictors of weight adjusted resting energy expenditure in older people. J. Nutr. Health Aging 2011, 15, 803–808. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization (WHO). Obesity: Preventing and Managing the Global Epidemic: Report of a WHO Consultation on Obesity; Report No.: WHO/NUT/NCD/98.1; World Health Organization: Geneva, Switzerland, 1998; p. 276. Available online: http://www.who.int/iris/handle/10665/63854 (accessed on 12 May 2022).
- Gordon, C.; Cameron, W.; Rochet, A. Stature, recumbent length, and weight. In Anthropometric Standardization Reference Manual; Lohman, T., Roche, A., Martorell, R., Eds.; Human Kinetics Books: Champaign, IL, USA, 1988; pp. 3–8. [Google Scholar]
- Callaway, W.; Cameron, A.; Bouchard, C.; Himes, J.; Lohman, T.; Martín, A. Circumferences. In Anthropometric Standardization Reference Manual; Lohman, T., Roche, A., Martorell, R., Eds.; Human Kinetics Books: Champaign, IL, USA, 1988; pp. 39–54. [Google Scholar]
- Harrison, G.; Buskirk, E.; Carter, J.; Johnston, F.; Lohman, T.; Pollock, M. Skinfold thicknesses and measurement technique. In Anthropometric Standardization Reference Manual; Lohman, T., Roche, A., Martorell, R., Eds.; Human Kinetics Books: Champaign, IL, USA, 1988; pp. 55–70. [Google Scholar]
- Kuczmarski, M.F.; Kuczmarski, R.J.; Najjar, M. Descriptive anthropometric reference data for older Americans. J. Am. Diet. Assoc. 2000, 100, 59–66. [Google Scholar] [CrossRef]
- Siri, W.E. Body composition from fluid spaces and density: Analysis of methods. In Techniques for Measuring Body Composition; Brozeck, J., Henschel, A., Eds.; National Academy of Sciences: Washington, DC, USA, 1961; pp. 223–244. [Google Scholar]
- Durnin, J.; Womersley, J. Body fat assessed from total body density and its estimation from skinfold thickness: Measurements on 481 men and women aged from 16 to 72 Years. Br. J. Nutr. 1974, 32, 77–97. [Google Scholar] [CrossRef] [PubMed]
- Boullata, J.; Williamns, J.; Cottrell, F.; Hudson, L.; Compher, C. Accurate determination of energy need in hospitalized patient. J. Am. Diet. Assoc. 2007, 107, 393–401. [Google Scholar] [CrossRef]
- Wasyluk, W.; Zwolak, A.; Jonckheer, J.; DeWaele, E.; Dabrowski, W. Methodological Aspects of Indirect Calorimetry in Patients with Sepsis—Possibilities and Limitations. Nutrients 2022, 14, 930. [Google Scholar] [CrossRef] [PubMed]
- Carrasco, F.; Reyes, E.; Núñez, C.; Riedemann, K.; Rimler, O.; Sánchez, G. Measured and predicted resting energy expenditure in obese and non-obese Chilean subjects. A proposal of predictive equations for the Chilean population. Rev. Med. Chile 2002, 130, 51–60. [Google Scholar] [CrossRef] [PubMed]
- Frankenfield, D.; Roth-Yousey, L.; Compher, C. Comparison of predictive equations for resting metabolic rate in healthy nonobese and obese adults: A systematic review. J. Am. Diet. Assoc. 2005, 105, 775–789. [Google Scholar] [CrossRef] [PubMed]
- Ravussin, E.; Bogardus, C. Relationship of genetics, age, and physical fitness to daily energy expenditure and fuel utilization. Am. J. Clin. Nutr. 1989, 49, 968–975. [Google Scholar] [CrossRef]
- Haghayegh, S.; Kang, H.A.; Khoshnevis, S.; Smolensky, M.H.; Diller, K.R. A comprehensive guideline for Bland-Altman and intra class correlation calculations to properly compare two methods of measurement and interpret findings. Physiol. Meas. 2020, 41, 055012. [Google Scholar] [CrossRef] [PubMed]
- Luhrmann, P.; Edelmann-Schafer, B.; Neuhauser-Berthold, M. Changes in resting metabolic rate in an elderly German population: Cross-sectional and longitudinal data. J. Nutr. Health Aging 2010, 14, 232–236. [Google Scholar] [CrossRef]
- Arner, P.; Engfeldt, P.; Lithell, H. Site differences in the basal metabolism of subcutaneous fat in obese women. J. Clin. Endo-crinol. Metab. 1981, 53, 948–952. [Google Scholar] [CrossRef] [PubMed]
- Godínez, S.; Marmolejo, G.; Márquez, E.; Siordia, J.; Baeza, R. Visceral fat and its importance in obesity. Rev. Endocrinol. Nutr. 2002, 10, 121–134. [Google Scholar]
- Bouchard, C.; Bray, G.; Hubbard, V. Basic and clinical aspects of regional fat distribution 1-3. Am. J. Clin. Nutr. 1990, 52, 946–950. [Google Scholar] [CrossRef] [PubMed]
- Björntorp, P. Classification of obese patients and complications related to the distribution of surplus fat. Am. J. Clin. Nutr. 1987, 45, 1120–1126. [Google Scholar] [CrossRef]
- Wajchenberg, B. Subcutaneous and visceral adipose tissue: Their relation to the metabolic syndrome. Endocr. Rev. 2000, 21, 697–738. [Google Scholar] [CrossRef] [PubMed]
- Ruiz-De La Fuente, M.; De La Maza, M. Body composition of 20 to 40 years old obese women of high and low socioeconomic status. Rev. Chil. Nutr. 2007, 34, 251–257. [Google Scholar] [CrossRef]
- National Health and Medical Research Council. Clinical Practice Guidelines for the Management of Overweight and Obesity in Adults, Adolescents and Children in Australia; National Health and Medical Research Council: Canberra, Australia, 2013. [Google Scholar]
- Ponti, F.; Santoro, A.; Mercatelli, D.; Gasperini, C.; Conte, M.; Martucci, M.; Sangiorgi, L.; Franceschi, C.; Bazzocchi, A. Aging and Imaging Assessment of Body Composition: From Fat to Facts. Front. Endocrinol. 2020, 14, 861. [Google Scholar] [CrossRef] [PubMed]
- Neuhauser-Berthold, M.; Herbert, B.M.; Luhrmann, P.M.; Sultemeier, A.A.; Blum, W.F.; Frey, J.; Hebebrand, J. Resting metabolic rate, body composition, and serum leptin concentrations in a free-living elderly population. Eur. J. Endocrinol. 2000, 142, 486–492. [Google Scholar] [CrossRef][Green Version]
- Weststrate, J.; Dekker, J.; Stoel, M.; Begheijn, L.; Deurenberg, P.; Hautvast, J. Resting energy expenditure in women: Impact of obesity and body-fat distribution. Metabolism 1990, 39, 11–17. [Google Scholar] [CrossRef]
- Yangmei, L.; Yanxia, M.; Liangmei, Q.; Jinhui, Z.; Yu, H.; Minwen, Z. Controlling energetic intake based on a novel logistic regression model for the metabolic syndrome in a Chinese population. Br. J. Nutr. 2011, 105, 256–262. [Google Scholar] [CrossRef] [PubMed]
- Lv, Y.; Miao, Y.; Qiao, L.; Liu, Y.; Zhang, X.; Zhang, J.; Zhang, R.; Nan, J.; Chi, F.; Zhang, L.; et al. Development and application of a new equation for estimating energy requirement in metabolic syndrome in a Chinese population. Int. J. Clin. Exp. Med. 2017, 10, 13721–13731. [Google Scholar]
- Antunes, H.; Santos, R.; Boscolo, R.; Bueno, O.; Mello, M. Análise da taxa metabólica basal de idosos do sexo masculino antes e seis meses após exercícios de resistência. Rev. Bras. Med. Esporte 2005, 11, 71–75. [Google Scholar] [CrossRef]
- Bonganha, V.; Libardi, C.A.; Santos, C.F.; De Souza, G.V.; Conceição, M.S.; Chacon-Mikahil, M.P.; Madruga, V.A. Predictive equations overestimate the resting metabolic rate in postmenopausal women. J. Nutr. Health Aging 2013, 17, 211–214. [Google Scholar] [CrossRef] [PubMed]
- Achamrah, N.; Jesus, P.; Grigioni, S.; Rimbert, A.; Petit, A.; Déchelotte, P.; Folope, V.; Coëffier, M. Validity of Predictive Equations for Resting Energy Expenditure Developed for Obese Patients: Impact of Body Composition Method. Nutrients 2018, 10, 63. [Google Scholar] [CrossRef] [PubMed]

| Variable | Women (n = 45) Mean ± SD |
|---|---|
| Age (years) | 66.0 ± 3.8 |
| Weight (kg) | 66.2 ± 11.2 |
| Height (m) | 1.5 ± 0.1 |
| BMI (kg/m2) | 28.3 ± 4.3 |
| AC (cm) | 32.3 ± 4.2 |
| BSF (mm) | 16.7 ± 9.1 |
| TSF (mm) | 21.0 ± 8.9 |
| SSF/(mm) | 24.8 ± 10.8 |
| SBSF (mm) | 23.8 ± 9.5 |
| Sum of skinfolds (mm) | 118.5 ± 38.7 |
| FM (kg) | 29.6 ± 7.5 |
| FFM (Kg) | 36.6 ± 4.7 |
| WC (cm) | 90.0 ± 11.1 |
| RMR IC (kcal/day) | 1083.6 ± 171.9 |
| Regression Equation | p | R2 | SEE | β |
|---|---|---|---|---|
| RMR = 1505.3 − 16.4 AGE + 7.3 WC | <0.01 | 0.44 | 131.7 | (−0.37; 0.47) |
| RMR = 1808.6 − 14.9 AGE + 8.7 FM | <0.01 | 0.35 | 141.2 | (−0.33; 0.38) |
| RMR = 1199.0 − 14.4 AGE + 22.8 FFM | <0.01 | 0.59 | 112.4 | (−0.32; 0.62) |
| RMR = 1231.6 − 15.0 AGE − 1.4 FM + 24.2 FFM | <0.01 | 0.59 | 113.1 | (−0.34; −0.07; 0.66) |
| RMR = 1012.0 − 17.6 AGE − 11.8 FM + 23.0 FFM + 8.1 WC | <0.01 | 0.65 | 105.5 | (−0.39; −0.52; 0.62; 0.53) |
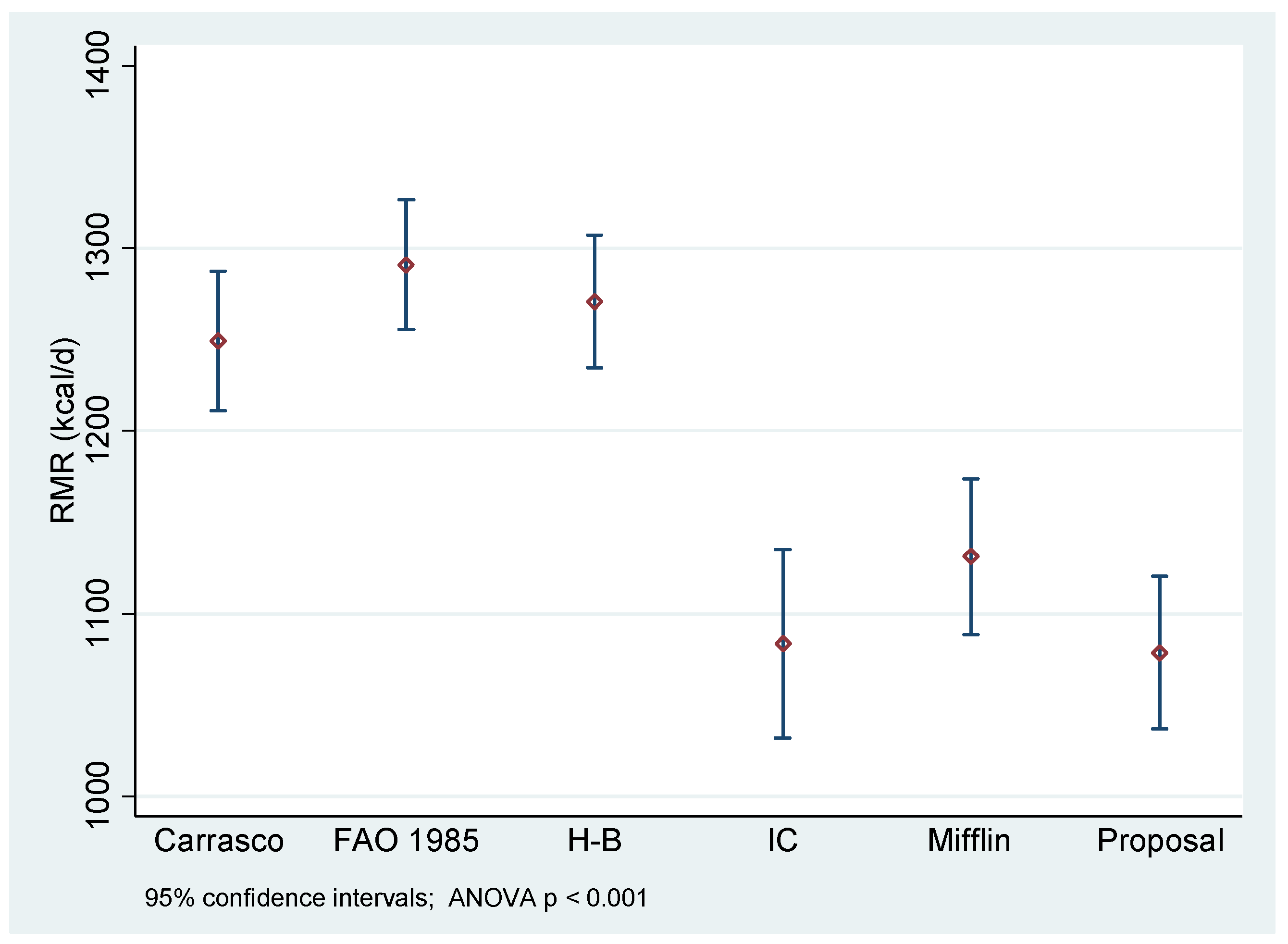
| Predictive Equation | Underestimation (<90%) | Adequacy (90% to 110%) | Overestimation (>110%) |
|---|---|---|---|
| Proposal | 8.8 | 80 | 11 |
| Mifflin-St Jeor | 8.8 | 60 | 41 |
| Harris–Benedict | 0 | 20 | 80 |
| FAO/WHO/UNU | 0 | 20 | 80 |
| Carrasco | 4.4 | 24 | 71 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Maury-Sintjago, E.; Muñoz-Mendoza, C.; Rodríguez-Fernández, A.; Ruíz-De la Fuente, M. Predictive Equation to Estimate Resting Metabolic Rate in Older Chilean Women. Nutrients 2022, 14, 3199. https://doi.org/10.3390/nu14153199
Maury-Sintjago E, Muñoz-Mendoza C, Rodríguez-Fernández A, Ruíz-De la Fuente M. Predictive Equation to Estimate Resting Metabolic Rate in Older Chilean Women. Nutrients. 2022; 14(15):3199. https://doi.org/10.3390/nu14153199
Chicago/Turabian StyleMaury-Sintjago, Eduard, Carmen Muñoz-Mendoza, Alejandra Rodríguez-Fernández, and Marcela Ruíz-De la Fuente. 2022. "Predictive Equation to Estimate Resting Metabolic Rate in Older Chilean Women" Nutrients 14, no. 15: 3199. https://doi.org/10.3390/nu14153199
APA StyleMaury-Sintjago, E., Muñoz-Mendoza, C., Rodríguez-Fernández, A., & Ruíz-De la Fuente, M. (2022). Predictive Equation to Estimate Resting Metabolic Rate in Older Chilean Women. Nutrients, 14(15), 3199. https://doi.org/10.3390/nu14153199