Rethinking Responsive Feeding: Insights from Bangladesh
Abstract
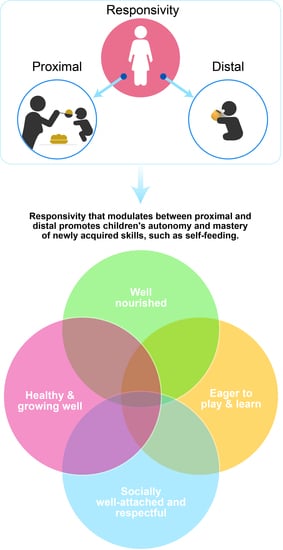
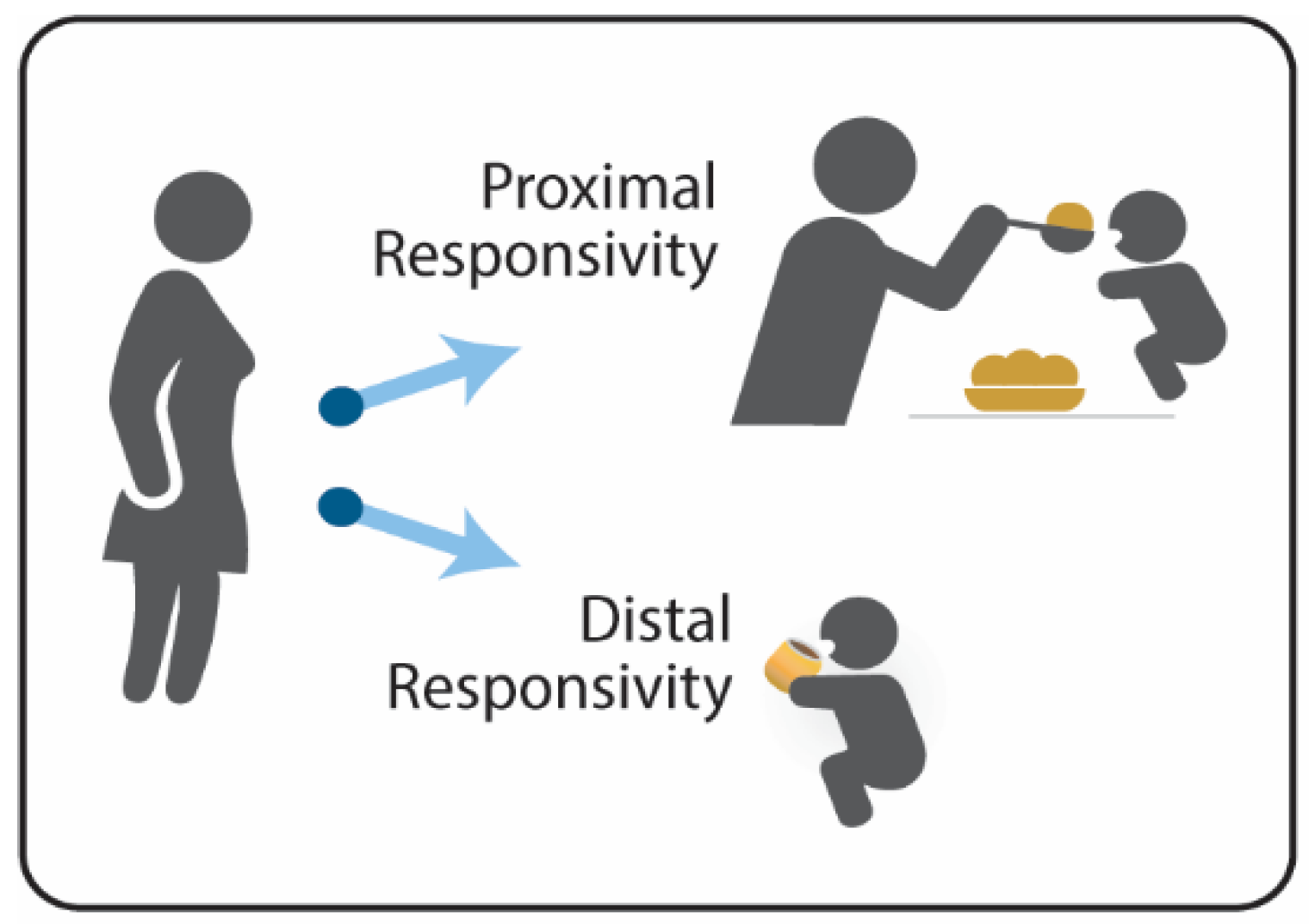
:1. Introduction
2. Materials and Methods
2.1. Procedure
2.2. Measures
2.3. Reliability Testing of Outcome Measures
2.4. Video Coding
2.5. Sample Size Calculation
2.6. Statistical Plan
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- UNICEF. The State of the World’s Children 2019: Children, Food and Nutrition: Growing Well in a Changing World; UNICEF: New York, NY, USA, 2019.
- Indicators for Assessing Infant and Young Child Feeding Practices. Available online: https://data.unicef.org/resources/indicators-for-assessing-infant-and-young-child-feeding-practices/ (accessed on 26 May 2022).
- Black, M.M.; Aboud, F.E. Responsive Feeding is Embedded in a Theoretical Framework of Responsive Parenting. J. Nutr. 2011, 141, 490–494. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jansen, E.; Williams, K.E.; Mallan, K.M.; Nicholson, J.M.; Daniels, L.A. Bidirectional Associations Between Mothers’ Feeding Practices and Child Eating Behaviours. Int. J. Behav. Nutr. Phys. Act. 2018, 15, 3. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bentley, M.E.; Wasser, H.M.; Creed-Kanashiro, H.M. Responsive Feeding and Child Undernutrition in Low- and Middle-Income Countries. J. Nutr. Educ. 2011, 141, 502–507. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Naila, N.; Nahar, B.; Lazarus, M.; Ritter, G.; Hossain, M.; Mahfuz, M.; Ahmed, T.; Denno, D.; Walson, J.; Ickes, S. “Those Who Care Much, Understand Much”. Maternal Perceptions of Children’s Appetite: Perspectives from Urban and Rural Caregivers of Diverse Parenting Experience in Bangladesh. Matern. Child Nutr. 2018, 14, e12473. [Google Scholar] [CrossRef]
- Hurley, K.M.; Cross, M.B.; Hughes, S.O. A Systematic Review of Responsive Feeding and Child Obesity in High-Income Countries. J. Nutr. 2011, 141, 495–501. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- PAHO/WHO. Guiding Principles for Complementary Feeding of the Breastfed Child; Pan American Health Organization/World Health Organization: Washington, DC, USA, 2003. [Google Scholar]
- WHO. Guiding Principles for Feeding Non-Breastfed Children 6–24 Months of Age; World Health Organization: Geneva, Switzerland, 2005. [Google Scholar]
- WHO. Improving Early Childhood Development: WHO Guideline; World Health Organization: Geneva, Switzerland, 2020. [Google Scholar]
- Black, M.M.; Walker, S.P.; Fernald, L.C.H.; Andersen, C.T.; DiGirolamo, A.M.; Lu, C.; McCoy, D.C.; Fink, G.; Shawar, Y.R.; Shiffman, J.; et al. Early Childhood Development Coming of Age: Science through the Life Course. Lancet 2016, 389, 10064. [Google Scholar] [CrossRef] [Green Version]
- Sall, N.S.; Begin, F.; Dupuis, J.B.; Bourque, J.; Menasria, L.; Main, B.; Vong, L.; Hun, V.; Raminashvili, D.; Chea, C.; et al. A Measurement Scale to Assess Responsive Feeding Among Cambodian Young Children. Matern. Child Nutr. 2020, 16, e12956. [Google Scholar] [CrossRef] [PubMed]
- Pallewaththa, P.; Agampodi, T.C.; Agampodi, S.B.; Perez-Escamilla, R.; Siribaddana, S. Measuring Responsive Feeding in Sri Lanka: Development of the Responsive Feeding Practices Assessment Tool. J. Nutr. Educ. Behav. 2021, 53, 489–502. [Google Scholar] [CrossRef] [PubMed]
- Hodges, E.; Johnson, S.L.; Hughes, S.O.; Hopkinson, J.M.; Butte, N.F.; Fisher, J.O. Responsiveness to Child Feeding Cues Scale. Appetite 2013, 65, 210–219. [Google Scholar] [CrossRef] [Green Version]
- Vygotsky, L.S. Mind in Society: The Development of Higher Psychological Processes; Harvard University Press: Cambridge, MA, USA, 1978. [Google Scholar]
- Bergmeier, H.J.; Skouteris, H.; Hetherington, M.M.; Rodgers, R.F.; Campbell, K.J.; Cox, R. Do Maternal Perceptions of Child Eating and Feeding Help to Explain the Disconnect between Reported and Observed Feeding Practices: A Follow-Up Study. Matern. Child Nutr. 2017, 13, e12420. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Heller, R.L.; Mobley, A.R. Instruments Assessing Parental Responsive Feeding in Children Ages Birth to 5 Years: A Systematic Review. Appetite 2019, 138, 23–51. [Google Scholar] [CrossRef]
- Sameroff, A.J. The Transactional Model of Development: How Children and Contexts Shape Each Other; American Psychological Association Press: Washington, DC, USA, 2009. [Google Scholar]
- Moore, A.C.; Akhter, S.; Aboud, F.E. Responsive Complementary Feeding in Rural Bangladesh. Soc. Sci. Med. 2006, 62, 1917–1930. [Google Scholar] [CrossRef] [PubMed]
- Pelto, G.H. Improving Complementary Feeding Practices and Responsive Parenting as a Primary Component of Interventions to Prevent Malnutrition in Infancy and Early Childhood. Pediatrics 2000, 106, 1300. [Google Scholar] [CrossRef] [PubMed]
- Murphy, M.K.; Black, N.A.; Lamping, D.L.; McKee, C.M.; Sanderson, C.F.B.; Askham, J.; Marteau, T. Consensus Development Methods, and their Use in Clinical Guideline Development. Health Technol. Assess. 1998, 2, 1–88. [Google Scholar] [CrossRef] [Green Version]
- Schellenberg, J.A.; Victora, C.G.; Mushi, A.; de Savigny, D.; Schellenberg, D.; Mshinda, H.; Bryce, J. Inequities among the Very Poor: Health Care for Children in Rural Southern Tanzania. Lancet 2003, 361, 561–566. [Google Scholar] [CrossRef]
- Coates, J.; Swindale, A.; Bilinsky, P. Household Food Insecurity Access Scale (HFIAS) for Measurement of Food Access: Indicator Guide; Academy for Educational Development, Food and Nutrition Technical Assistance Project (FANTA): Washington, DC, USA, 2007. [Google Scholar]
- WHO and Partners. Indicators for Assessing Infant and Young Child Feeding Practices. Part I Definitions; World Health Organization: Geneva, Switzerland, 2008. [Google Scholar]
- WHO and Partners. Indicators for Assessing Infant and Young Child Feeding Practices. Part 2 Measurement; WHO: Geneva, Switzerland, 2010. [Google Scholar]
- WHO Multicenter Growth Reference Study Group. WHO Child Growth Standards Based on Length/Height, Weight and Age. Acta Paediatr. 2006, 450, 76–85. [Google Scholar] [CrossRef]
- NCSS Statistical Software LLC. PASS 2020 Power Analysis and Sample Size Software; NCSS Statistical Software LLC: Kaysville, UT, USA, 2020. [Google Scholar]
- Vaughn, A.E.; Ward, D.S.; Fisher, J.O.; Faith, M.S.; Hughes, S.O.; Kremers, S.P.; Musher-Eizenman, D.R.; O’Connor, T.M.; Patrick, H.; Power, T.G. Fundamental Constructs in Food Parenting Practices: A Content Map to Guide Future Research. Nutr. Rev. 2016, 74, 98–117. [Google Scholar] [CrossRef] [Green Version]
- Sherry, B.; McDivitt, J.; Birch, L.L.; Cook, F.H.; Sanders, S.; Prish, J.L.; Francis, L.A.; Scanlon, K.S. Attitudes, Practices, and Concerns About Child Feeding and Child Weight Status Among Socioeconomically Diverse White, Hispanic, and African-American Mothers. J. Am. Diet. Assoc. 2004, 104, 215–221. [Google Scholar] [CrossRef]
- Blume, J.; Park, S.; Cox, M.; Mastergeorge, A.M. Explicating Child-Driven Patterns of Parent-Child Responsivity in Fragile Families: A Longitudinal Approach. Front. Pediatr. 2022, 10, 813486. [Google Scholar] [CrossRef]
- Aboud, F.E.; Akhter, S. A Cluster-Randomized Evaluation of a Responsive Stimulation and Feeding Intervention in Bangladesh. Pediatrics 2011, 127, e1191–e1197. [Google Scholar] [CrossRef]
- Bornstein, M.H. Children’s Parents. In Ecological Settings and Processes in Developmental Systems, 7th ed.; Bornstein, M.H., Leventhal, T., Eds.; Handbook of Child Psychology and Developmental Science: Hoboken, NJ, USA, 2015; Volume 4. [Google Scholar]
- Pak-Gorstein, S.; Haq, A.; Graham, E.A. Cultural Influences on Infant Feeding Practices. Pediatr. Rev. 2009, 30, e11–e21. [Google Scholar] [CrossRef]
- Affleck, W.; Pelto, G. Caregivers’ Responses to an Intervention to Improve Young Child Feeding Behaviors in Rural Bangladesh: A Mixed Method Study of the Facilitators and Barriers to Change. Soc. Sci. Med. 2012, 75, 651–658. [Google Scholar] [CrossRef] [PubMed]
- Landry, S.H.; Smith, K.E.; Swank, P.R. Responsive Parenting: Establishing Early Foundations for Social, Communication, and Independent Problem-Solving Skills. Dev. Psychol. 2006, 42, 627–642. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pérez-Escamilla, R.; Segura-Pérez, S.; Lott, M. RWJF HER Expert Panel on Best Practices for Promoting Healthy Nutrition, Feeding Patterns, and Weight Status for Infants and Toddlers from Birth to 24 Months. In Feeding Guidelines for Infants and Young Toddlers: A Responsive Parenting Approach; Healthy Eating Research-Robert Wood Johnson Foundation: Durham, NC, USA, 2017. [Google Scholar]
- Newnham, C.A.; Milgrom, J.; Skouteris, H. Effectiveness of a Modified Mother-Infant Transaction Program on Outcomes for Preterm Infants from 3 to 24 Months of Age. Infant Behav. Dev. 2009, 32, 17–26. [Google Scholar] [CrossRef] [PubMed]
| Characteristics | Overall N = 67 | Proximal Responsivity N = 38 | Distal Responsivity N = 29 | p-Value |
|---|---|---|---|---|
| Mother | ||||
| Maternal age (years), mean (SD) | 24.9 (5.6) | 25.5 (5.7) | 24.2 (5.5) | 0.342 |
| Maternal education | ||||
| None, n (%) | 6 (9.0) | 4 (11) | 2 (7) | 0.949 |
| 1–5 years, n (%) | 27 (40.3) | 15 (39.5) | 12 (39.4) | |
| 6–8 years, n (%) | 25 (37.2) | 14 (36.5) | 11 (39.6) | |
| Secondary School Certificate, n (%) | 4 (6.0) | 2 (5) | 2 (7) | |
| Higher Secondary Certificate, n (%) | 5 (7.5) | 3 (8) | 2 (7) | |
| Paternal education | ||||
| None | 4 (6.0) | 1 (2.6) | 3 (10.3) | 0.645 |
| 1–5 years, n (%) | 27 (40.3) | 19 (50.0) | 8 (27.6) | |
| 6–8 years, n (%) | 20 (29.8) | 8 (21.0) | 12 (41.4) | |
| Secondary School Certificate, n (%) | 6 (9.0) | 3 (7.9) | 3 (10.3) | |
| Higher Secondary Certificate, n (%) | 10 (14.9) | 7 (18.4) | 3 (10.3) | |
| Religion | ||||
| Islam, n (%) | 66 (98.5) | 38 (100.0) | 28 (96.6) | 0.249 |
| Hindu, n (%) | 1 (1.4) | 0 (0.0) | 1 (3.5) | |
| Finances | ||||
| Total number of children mean (SD) | 1.8 (0.9) | 1.8 (0.9) | 1.7 (0.9) | 0.768 |
| Monthly income, taka, mean (SD) | 15410.5 (8081.0) | 15697.4 (8133.6) | 15034.5 (8139.3) | 0.742 |
| Monthly income, dollars, mean (SD) * | 165.90 (87.51) | 168.90 (87.51) | 161.77 (87.95) | |
| Monthly Financial Deficit ** | ||||
| Always, n (%) | 13 (19.4) | 6 (15.8) | 7 (24.1) | 0.665 |
| Sometimes, n (%) | 38 (56.7) | 23 (60.5) | 15 (51.7) | |
| Never, n (%) | 9 (23.7) | 7 (24.1) | 16 (23.9) | |
| Food security *** | ||||
| Food secure, n (%) | 25 (37.3) | 15 (39.5) | 10 (34.5) | 0.994 |
| Mildly food insecure, n (%) | 14 (20.9) | 7 (18.4) | 4 (24.1) | |
| Moderately food insecure, n (%) | 12 (17.9) | 7 (18.4) | 5 (17.2) | |
| Severely food insecure, n (%) | 16 (23.9) | 9 (23.7) | 7 (24.1) | |
| Child | ||||
| Female, n (%) | 26 (38.8) | 13 (34.2) | 13 (44.8) | 0.377 |
| Age (months), mean | 12.8 (3.4) | 12.5 (3.8) | 13.2 (2.8) | 0.440 |
| Growth **** | ||||
| Weight-for-age z-score (WAZ), mean (SD) | −0.7 (0.9) | −0.8 (0.9) | −0.6 (0.8) | 0.597 |
| Length-for-age z-score (LAZ), mean (SD) | −1.2 (1.0) | −1.2 (1.0) | −1.1 (0.9) | 0.612 |
| Weight-for-length z-score (WLZ), mean (SD) | −0.2 (0.9) | −0.2 (1.0) | −0.1 (0.8) | 0.897 |
| Underweight (<−2 WAZ), n (%) | 4 (6.0) | 3 (7.9) | 1 (3.5) | 0.447 |
| Stunted (<−2 LAZ), n (%) | 10 (14.9) | 7 (18.4) | 3 (10.3) | 0.358 |
| Wasted (<−2 WLZ), n (%) | 1 (1.5) | 1 (2.6) | 0 (0.0) | 0.379 |
| Diet during previous 24-h | ||||
| Breastfed, n (%) | 64 (95.5) | 36 (94.7) | 28 (96.6) | 0.722 |
| Minimum dietary diversity, n (%) ***** | 49 (73.1) | 28 (73.7) | 21 (72.4) | 0.908 |
| Minimum meal frequency, n (%) ****** | 48 (71.6) | 26 (68.4) | 22 (72.4) | 0.503 |
| Food groups consumed, n (%) | ||||
| Grains, Rice, Tubers | 66 (98.5) | 38 (100.0) | 28 (96.6) | 0.249 |
| Legumes/Nuts | 39 (58.2) | 20 (52.6) | 19 (65.5) | 0.289 |
| Dairy | 34 (50.8) | 18 (47.4) | 16 (55.2) | 0.527 |
| Flesh Foods | 41 (61.2) | 23 (60.5) | 18 (62.1) | 0.898 |
| Eggs | 31 (46.3) | 17 (44.7) | 14 (48.3) | 0.774 |
| Fruits & Vegetables high in Vitamin A | 25 (37.3) | 18 (47.4) | 7 (24.1) | 0.051 |
| Other Fruits and vegetables | 42 (62.7) | 21 (55.3) | 21 (72.4) | 0.150 |
| Number | Item | Mean (SD) * |
|---|---|---|
| Quartile 1 | ||
| 35. | How concerned are you that your child eats too much? | 1.0 (0.2) |
| 32. | How concerned are you that your child weighs too much? | 1.1 (0.5) |
| 20. | How often do you talk on the mobile phone during your child’s meals? | 1.1 (0.3) |
| 7. | How often do you eat a meal with your child? | 1.3 (0.5) |
| 8. | How often are you in an unhappy mood while your child is eating? | 1.3 (0.6) |
| 16. | How often do you threaten your child to get him/her to eat? | 1.4 (0.7) |
| 27. | How often do you feel hassled or stressed during meals with your child? | 1.5 (0.9) |
| 5. | How often do you raise your voice (e.g., eat eat) to get your child to eat? | 1.6 (0.8) |
| 25. | How often do you restrict your child’s arms during meals? | 1.8 (1.1) |
| Quartile 2 | ||
| 24. | How often do you hold your child in your lap during meals? | 1.9 (1.1) |
| 36. | How concerned are you about what your child eats? | 1.9 (1.2) |
| 30. | How often does your child eat meals at the same time every day? | 1.9 (1.1) |
| 10. | How often does your child stay seated during the meal? | 1.9 (1.2) |
| 9. | How often do you show your child that you are happy or unhappy with how your child is eating? | 2.0 (1.2) |
| 21. | How often do you encourage your child to touch the food during meals? | 2.0 (1.0) |
| 37. | How important is it for your child to finish all his/her food? | 2.0 (1.1) |
| 15. | How often do you promise to give your child something if he/she eats? | 2.1 (1.1) |
| 14. | How often does your child have a poor appetite during meals? | 2.2 (0.9) |
| 18. | How often is your child upset or distressed during meals? | 2.2 (1.0) |
| 22. | How often does your child feed him/herself at least one bite of food during meals? | 2.2 (1.0) |
| Quartile 3 | ||
| 2. | How often do you pressure your child to eat? | 2.3 (1.2) |
| 1. | How often does your child refuse to eat most of the meal? | 2.5 (1.1) |
| 19. | How often does your child have a good appetite during meals? | 2.3 (0.8) |
| 13. | How often is your child in a happy mood while he/she is eating? | 2.4 (0.9) |
| 3. | How often do you use a toy, TV, or mobile phone to get your child to eat? | 2.4 (1.2) |
| 4. | How often do you distract your child without a toy or other object (e.g., airplane game) to get him/her to eat? | 2.5 (1.1) |
| 11. | How often does your child let you know when he/she is hungry? | 2.7 (1.0) |
| 34. | How concerned are you about your child’s health? | 2.7 (1.2) |
| Quartile 4 | ||
| 23. | How often do you wash your child’s hands before meals? | 2.8 (1.3) |
| 31. | How concerned are you that your child does not weigh enough? | 2.8 (1.3) |
| 38. | How confident are you that your child eats enough food? | 2.9 (1.0) |
| 33. | How concerned are you that your child does not eat enough? | 3.0 (1.1) |
| 12. | How often does your child let you know when he/she is full? | 3.0 (1.1) |
| 6. | How often are you in a happy mood while you child is eating? | 3.3 (0.7) |
| 28. | How often do you feel happy during meals with your child? | 3.3 (0.8) |
| 26. | How often is your child positioned so he/she can see your face during meals? | 3.3 (1.0) |
| 29. | How often are you positioned so you can see your child’s face during meals? | 3.6 (0.7) |
| 17. | How often do you talk to your child during meals? | 3.6 (0.7) |
| Item | Variable | OR (95% CI) | p-Value | Distal vs. Proximal |
|---|---|---|---|---|
| Age | Infant age (months) | 1.31 (0.96, 1.78) | 0.089 | |
| Q2 | How often do you pressure your child to eat? | 7.98 (2.22, 28.73) | 0.002 | Distal |
| Q6 | How often are you in a happy mood while your child is eating? | 0.28 (0.08, 1.01) | 0.051 | Proximal |
| Q10 | How often does your child stay seated during the meal? | 0.16 (0.05, 0.46) | <0.001 | Proximal |
| Q13 | How often is your child in a happy mood while he/she is eating? | 5.36 (1.46, 19.64) | 0.011 | Distal |
| Q17 | How often do you talk to your child during meals? | 0.25 (0.06, 1.01) | 0.051 | Proximal |
| Q23 | How often do you wash your child’s hands before meals? | 0.29 (0.13, 0.67) | 0.004 | Proximal |
| Q27 | How often do you feel hassled or stressed during meals with your child? | 0.22 (0.07, 0.68) | 0.008 | Proximal |
| Q29 | How often are you positioned so you can see your child’s face during meals? | 13.11 (2.09, 82.41) | 0.006 | Distal |
| Q33 | How concerned are you that your child does not eat enough? | 0.15 (0.04, 0.58) | 0.006 | Proximal |
| Predicted (Self-Report Feeding Questionnaire) | Observed (Video Ratings) | |
|---|---|---|
| Distal | Proximal | |
| n/N (Col %) | n/N (Col %) | |
| Distal | 26/29 (90%) | 4/38 (11%) |
| Proximal | 3/29 (10%) | 34/38 (89%) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Black, M.M.; Tofail, F.; Hodges, E.A.; Bann, C.M.; Hamadani, J.D.; Aktar, S.; Lutter, C.K. Rethinking Responsive Feeding: Insights from Bangladesh. Nutrients 2022, 14, 3156. https://doi.org/10.3390/nu14153156
Black MM, Tofail F, Hodges EA, Bann CM, Hamadani JD, Aktar S, Lutter CK. Rethinking Responsive Feeding: Insights from Bangladesh. Nutrients. 2022; 14(15):3156. https://doi.org/10.3390/nu14153156
Chicago/Turabian StyleBlack, Maureen M., Fahmida Tofail, Eric A. Hodges, Carla M. Bann, Jena D. Hamadani, Shirina Aktar, and Chessa K. Lutter. 2022. "Rethinking Responsive Feeding: Insights from Bangladesh" Nutrients 14, no. 15: 3156. https://doi.org/10.3390/nu14153156
APA StyleBlack, M. M., Tofail, F., Hodges, E. A., Bann, C. M., Hamadani, J. D., Aktar, S., & Lutter, C. K. (2022). Rethinking Responsive Feeding: Insights from Bangladesh. Nutrients, 14(15), 3156. https://doi.org/10.3390/nu14153156