Mealtime Regularity Is Associated with Dietary Balance among Preschool Children in Japan—A Study of Lifestyle Changes during the COVID-19 Pandemic
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Participants and Design
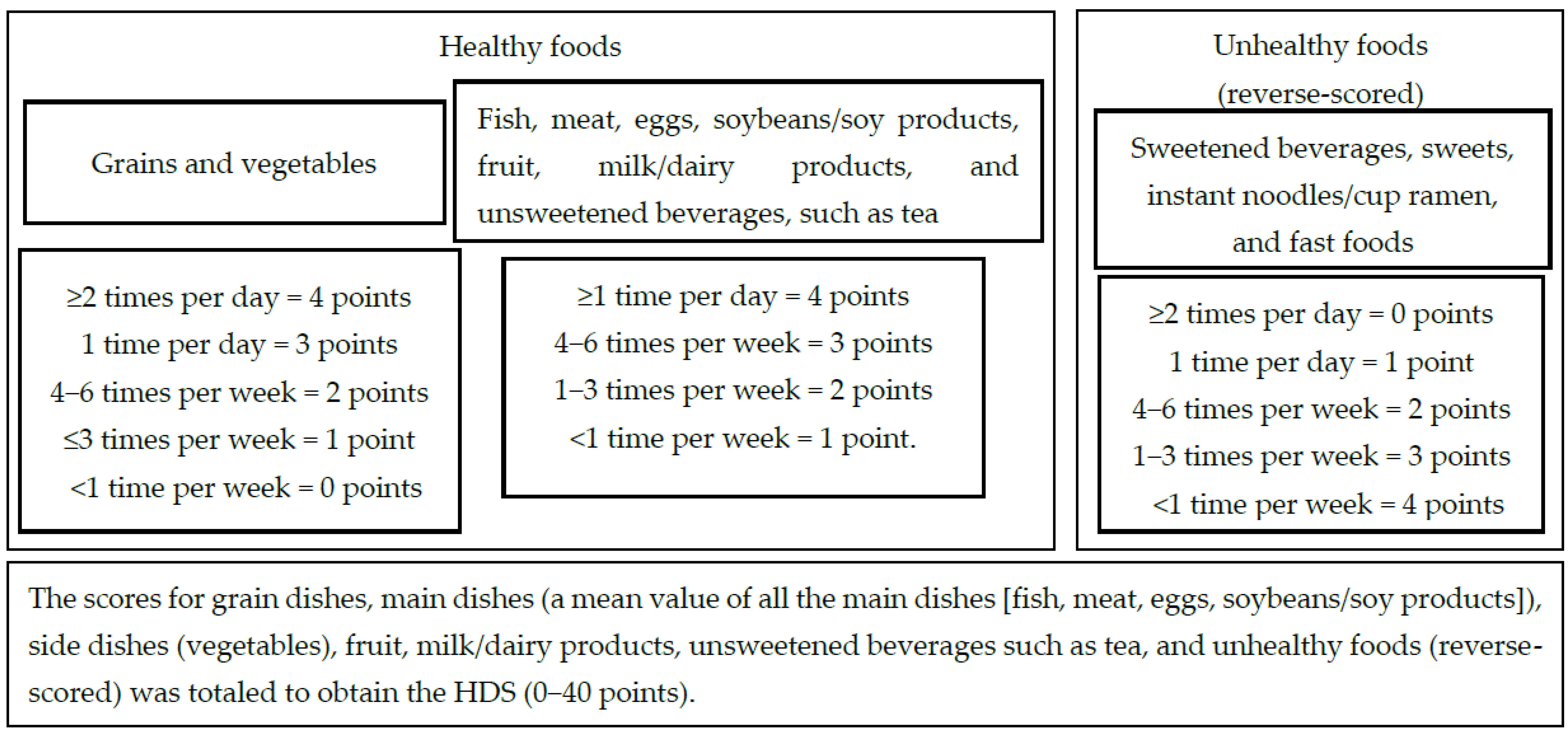
2.2. Calculating the Healthy Diet Score (HDS)
2.3. Changes in the HDS during COVID-19: Changed-Healthy Diet Score (C-HDS)
2.4. Ethical Considerations
2.5. Analysis
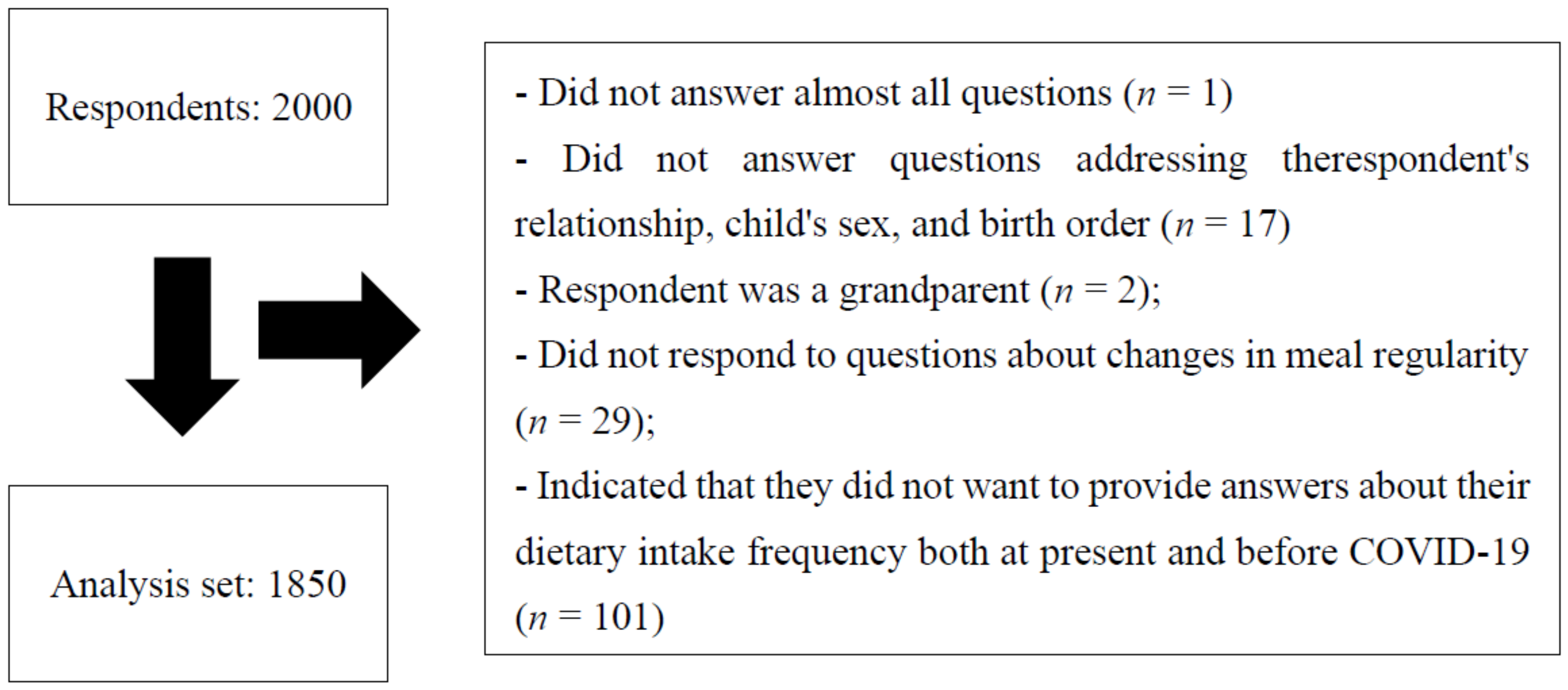
2.5.1. Data Set for Analysis
2.5.2. Statistical Analysis
3. Results
3.1. Comparison of Participant Characteristics according to Changes in Mealtime Regularity Compared with before COVID-19
3.2. Comparison of the Healthy Diet Score (HDS) according to Changes in Mealtime Regularity Compared with before COVID-19
3.3. Multiple Regression Analyses with the Healthy Diet Score (HDS) as the Dependent Variable
3.4. Multiple Logistic Regression Analysis with the Change in Healthy Diet Score (C-HDS) as the Dependent Variable
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Pietrobelli, A.; Pecoraro, L.; Ferruzzi, A.; Heo, M.; Faith, M.; Zoller, T.; Antoniazzi, F.; Piacentini, G.; Fearnbach, S.N.; Heymsfield, S.B. Effects of COVID-19 Lockdown on Lifestyle Behaviors in Children with Obesity Living in Verona, Italy: A Longitudinal Study. Obesity 2020, 28, 1382–1385. [Google Scholar] [CrossRef] [PubMed]
- Carroll, N.; Sadowski, A.; Laila, A.; Hruska, V.; Nixon, M.; Ma, D.W.L.; Haines, J.; On Behalf of The Guelph Family Health Study. The Impact of COVID-19 on Health Behavior, Stress, Financial and Food Security among Middle to High Income Canadian Families with Young Children. Nutrients 2020, 12, 2352. [Google Scholar] [CrossRef] [PubMed]
- Androutsos, O.; Perperidi, M.; Georgiou, C.; Chouliaras, G. Lifestyle Changes and Determinants of Children’s and Adolescents’ Body Weight Increase during the First COVID-19 Lockdown in Greece: The COV-EAT Study. Nutrients 2021, 13, 930. [Google Scholar] [CrossRef] [PubMed]
- National Center for Child Health and Development. Corona × Children’s Questionnaire 1st Survey Report. Available online: https://www.ncchd.go.jp/center/activity/covid19_kodomo/report/CxC1_finalrepo_20210306revised.pdf (accessed on 24 January 2022). (In Japanese)
- Shimpo, M.; Akamatsu, R.; Kojima, Y.; Yokoyama, T.; Okuhara, T.; Chiba, T. Factors Associated with Dietary Change since the Outbreak of COVID-19 in Japan. Nutrients 2021, 13, 2039. [Google Scholar] [CrossRef]
- Ministry of Health, Labour, and Welfare of Japan. National Nutrition Survey on Preschool Children. 2015. Available online: https://www.mhlw.go.jp/file/06-Seisakujouhou-11900000-Koyoukintoujidoukateikyoku/0000134460.pdf (accessed on 8 February 2022). (In Japanese)
- Fukuda, K.; Hasegawa, T.; Kawahashi, I.; Imada, S. Preschool children’s eating and sleeping habits: Late rising and brunch on weekends is related to several physical and mental symptoms. Sleep Med. 2019, 61, 73–81. [Google Scholar] [CrossRef]
- Yoshizaki, T.; Tada, Y.; Hida, A.; Sunami, A.; Yokoyama, Y.; Togo, F.; Kawano, Y. Influence of dietary behavior on the circadian rhythm of the autonomic nervous system as assessed by heart rate variability. Physiol. Behav. 2013, 118, 122–128. [Google Scholar] [CrossRef]
- Yoshizaki, T.; Tada, Y.; Hida, A.; Sunami, A.; Yokoyama, Y.; Yasuda, J.; Nakai, A.; Togo, F.; Kawano, Y. Effects of feeding schedule changes on the circadian phase of the cardiac autonomic nervous system and serum lipid levels. Eur. J. Appl. Physiol. 2013, 113, 2603–2611. [Google Scholar] [CrossRef]
- Ministry of Agriculture, Forestry, and Fisheries. The Fourth Basic Plan for the Promotion of Shokuiku. 2021. Available online: https://www.maff.go.jp/j/syokuiku/attach/pdf/kannrennhou-30.pdf (accessed on 8 February 2022).
- Yoshiike, N.; Hayashi, F.; Takemi, Y.; Mizoguchi, K.; Seino, F. A new food guide in Japan: The Japanese food guide Spinning Top. Nutr. Rev. 2007, 65, 149–154. [Google Scholar] [CrossRef]
- Ishikawa, M.; Eto, K.; Haraikawa, M.; Yoshiike, N.; Yokoyama, T. Relationship between parents’ dietary care and food diversity among preschool children in Japan. Public Health Nutr. 2021, 25, 1–12. [Google Scholar] [CrossRef]
- Food and Agriculture Organization of the United Nations (FAO). Dietary Assessment: A Resource Guide to Method Selection and Application in Low Resource Settings. Rome. 2018. Available online: https://www.fao.org/3/i9940en/I9940EN.pdf (accessed on 8 February 2022).
- Kesztyüs, D.; Traub, M.; Lauer, R.; Kesztyüs, T.; Steinacker, J.M. Skipping breakfast is detrimental for primary school children: Cross-sectional analysis of determinants for targeted prevention. BMC Public Health 2017, 17, 258. [Google Scholar] [CrossRef] [Green Version]
- Ministry of Health, Labour, and Welfare of Japan. Report of the Study Group on the Healthy Development of Children through Diet (From the Perspective of So-Called “Shokuiku”). Available online: https://www.mhlw.go.jp/shingi/2004/02/dl/s0219-4a.pdf (accessed on 8 February 2022). (In Japanese)
- Pourrostami, K.; Heshmat, R.; Hemati, Z.; Heidari-Beni, M.; Qorbani, M.; Motlagh, M.E.; Raeisi, A.; Shafiee, G.; Ziaodini, H.; Beshtar, S.; et al. Association of fruit and vegetable intake with meal skipping in children and adolescents: The CASPIAN-V study. Eat. Weight Disord. 2020, 25, 903–910. [Google Scholar] [CrossRef] [PubMed]
- Kelishadi, R.; Mozafarian, N.; Qorbani, M.; Motlagh, M.E.; Safiri, S.; Ardalan, G.; Keikhah, M.; Rezaei, F.; Heshmat, R. Is snack consumption associated with meal skipping in children and adolescents? The CASPIAN-IV study. Eat. Weight Disord. 2017, 22, 321–328. [Google Scholar] [CrossRef] [PubMed]
- Zahra, J.; Ford, T.; Jodrell, D. Cross-sectional survey of daily junk food consumption, irregular eating, mental and physical health and parenting style of British secondary school children. Child Care Health Dev. 2014, 40, 481–491. [Google Scholar] [CrossRef]
- Tada, Y.; Furukawa, C.; Miura, R.; Matsunaga, H.; Furusho, T.; Goto, S.; Usui, J.; Hashimoto, M.; Hida, A.; Kawano, Y. Relationship between Evening Meal Vegetable Consumption, Snacks, and Outdoor Play among Early Elementary School Children. J. Jpn. Soc. Shokuiku 2017, 11, 13–23. (In Japanese) [Google Scholar] [CrossRef]
- Kostecka, M. The influence of preschool children’s diets on the risk of lifestyle diseases. A pilot study. Rocz. Panstw. Zakl. Hig. 2018, 69, 139–145. [Google Scholar] [PubMed]
- Krebs-Smith, S.M.; Pannucci, T.E.; Subar, A.F.; Kirkpatrick, S.I.; Lerman, J.L.; Tooze, J.A.; Wilson, M.M.; Reedy, J. Update of the Healthy Eating Index: HEI-2015. J. Acad. Nutr. Diet. 2018, 118, 1591–1602. [Google Scholar] [CrossRef] [Green Version]
- Jun, S.; Zeh, M.J.; Eicher-Miller, H.A.; Bailey, R.L. Children’s Dietary Quality and Micronutrient Adequacy by Food Security in the Household and among Household Children. Nutrients 2019, 11, 965. [Google Scholar] [CrossRef] [Green Version]
- Carroll, J.E.; Price, G.; Longacre, M.R.; Hendricks, K.M.; Langeloh, G.; Beach, P.; Dalton, M.A.; Emond, J.A. Associations between advertisement-supported media exposure and dietary quality among preschool-age children. Appetite 2021, 166, 105465. [Google Scholar] [CrossRef]
- Heidari-Beni, M.; Riahi, R.; Massoudi, S.; Qorbani, M.; Kelishadi, R. Association between dietary diversity score and anthropometric indices among children and adolescents: The weight disorders survey in the CASPIAN-IV study. J. Sci. Food Agric. 2021, 101, 5075–5081. [Google Scholar] [CrossRef]
- Fernandez, C.; Kasper, N.M.; Miller, A.L.; Lumeng, J.C.; Peterson, K.E. Association of Dietary Variety and Diversity with Body Mass Index in US Preschool Children. Pediatrics 2016, 137, e20152307. [Google Scholar] [CrossRef] [Green Version]
- Archero, F.; Ricotti, R.; Solito, A.; Carrera, D.; Civello, F.; Di Bella, R.; Bellone, S.; Prodam, F. Adherence to the Mediterranean diet among school children and adolescents living in Northern Italy and unhealthy food behaviors associated to overweight. Nutrients 2018, 10, 1322. [Google Scholar] [CrossRef] [PubMed] [Green Version]
| Became Regular | Originally Regular, No Change | Became Irregular | Originally Irregular, No Change | ||||||
|---|---|---|---|---|---|---|---|---|---|
| (n = 125) | (n = 1514) | (n = 63) | (n = 148) | ||||||
| Respondent’s relationship to the child | Father | 56 | (44.8) | 618 | (40.8) | 22 | (34.9) | 74 | (50.0) |
| Mother | 69 | (55.2) | 896 | (59.2) | 41 | (65.1) | 74 | (50.0) | |
| Employment status of the child’s mother | Employed | 78 | (62.4) | 827 | (54.6) | 38 | (60.3) | 74 | (50.0) |
| Other | 47 | (37.6) | 687 | (45.4) | 25 | (39.7) | 74 | (50.0) | |
| Child’s sex | Boy | 69 | (55.2) | 752 | (49.7) | 30 | (47.6) | 68 | (45.9) |
| Girl | 56 | (44.8) | 762 | (50.3) | 33 | (52.4) | 80 | (54.1) | |
| Child’s age (years) | 3.2 | ±1.4 | 3.4 | ±1.4 | 3.2 | ±1.4 | 2.9 | ±1.4 | |
| Height (cm) | 105.6 | ±12.1 | 105.9 | ±11.4 | 105.6 | ±12.1 | 102.9 | ±11.5 | |
| Weight (kg) | 17.3 | ±4.6 | 17.3 | ±3.9 | 17.2 | ±4.1 | 16.5 | ±3.7 | |
| BMI percentile | 46.7 | ±36.0 | 44.9 | ±34.2 | 39.7 | ±32.0 | 49.9 | ±33.2 | |
| Became Regular | Originally Regular, No Change | Became Irregular | Originally Irregular, No Change | p Value * | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| (n = 125) | (n = 1514) | (n = 63) | (n = 148) | |||||||
| Wakeup time | Before 8 a.m. on weekdays and holidays | 83 | (66.4) | 1066 | (70.4) | 32 | (50.8) | 54 | (36.5) | <0.001 |
| Other | 42 | (33.6) | 448 | (29.6) | 31 | (49.2) | 94 | (63.5) | ||
| Bed time | Before 10 p.m. on weekdays and holidays | 91 | (72.8) | 1156 | (76.4) | 34 | (54.0) | 53 | (35.8) | <0.001 |
| Other | 34 | (27.2) | 358 | (23.6) | 29 | (46.0) | 95 | (64.2) | ||
| Physical activity time (weekdays) | <1 h (/day) | 68 | (54.4) | 708 | (47.0) | 35 | (55.6) | 74 | (51.0) | 0.200 |
| ≥1 h (/day) | 57 | (45.6) | 799 | (53.0) | 28 | (44.4) | 71 | (49.0) | ||
| Physical activity time (holidays) | <1 h (/day) | 69 | (55.2) | 743 | (49.3) | 35 | (55.6) | 74 | (50.7) | 0.485 |
| ≥1 h (/day) | 56 | (44.8) | 764 | (50.7) | 28 | (44.4) | 72 | (49.3) | ||
| Screen time (weekdays) | <2 h (/day) | 97 | (79.5) | 1219 | (80.8) | 44 | (71.0) | 98 | (66.7) | <0.001 |
| ≥2 h (/day) | 25 | (20.5) | 289 | (19.2) | 18 | (29.0) | 49 | (33.3) | ||
| Screen time (holidays) | <2 h (/day) | 85 | (69.7) | 983 | (65.2) | 37 | (59.7) | 76 | (52.4) | 0.009 |
| ≥2 h (/day) | 37 | (30.3) | 525 | (34.8) | 25 | (40.3) | 69 | (47.6) | ||
| Frequency of defecation | Almost every day | 94 | (76.4) | 1072 | (70.9) | 34 | (54.0) | 105 | (71.4) | 0.014 |
| Other | 29 | (23.6) | 439 | (29.1) | 29 | (46.0) | 42 | (28.6) | ||
| Snack frequency | 0−1 time (/day) | 79 | (64.8) | 1056 | (70.1) | 31 | (50.0) | 84 | (57.9) | <0.001 |
| 2 times (/day) | 37 | (30.3) | 390 | (25.9) | 25 | (40.3) | 40 | (27.6) | ||
| ≥3 times (/day) | 6 | (4.9) | 60 | (4.0) | 6 | (9.7) | 21 | (14.5) | ||
| Breakfast frequency | Eat every day | 112 | (89.6) | 1442 | (95.2) | 47 | (74.6) | 116 | (78.4) | <0.001 |
| Other | 13 | (10.4) | 72 | (4.8) | 16 | (25.4) | 32 | (21.6) | ||
| Eat together (breakfast) | Eat with an adult | 106 | (86.2) | 1249 | (82.7) | 51 | (81.0) | 97 | (67.4) | <0.001 |
| Other | 17 | (13.8) | 262 | (17.3) | 12 | (19.0) | 47 | (32.6) | ||
| Eat together (dinner) | Eat with an adult | 122 | (97.6) | 1457 | (96.4) | 61 | (96.8) | 135 | (91.8) | 0.041 |
| Other | 3 | (2.4) | 55 | (3.6) | 2 | (3.2) | 12 | (8.2) | ||
| How often the respondent cooks | 1−2 times per week | 36 | (28.8) | 469 | (31.2) | 20 | (31.7) | 55 | (37.9) | 0.474 |
| 3−6 times per week | 27 | (21.6) | 330 | (22.0) | 17 | (27.0) | 34 | (23.4) | ||
| Every day | 62 | (49.6) | 702 | (46.8) | 26 | (41.3) | 56 | (38.6) | ||
| Frequency with which the child is involved in cooking | Rarely | 41 | (32.8) | 672 | (44.4) | 17 | (27.4) | 82 | (55.4) | <0.001 |
| ≥1 time per week | 84 | (67.2) | 840 | (55.6) | 45 | (72.6) | 66 | (44.6) | ||
| Someone in the family works remotely | 51 | (40.8) | 390 | (25.8) | 25 | (39.7) | 28 | (18.9) | <0.001 | |
| Financial security | Yes | 54 | (43.5) | 567 | (37.5) | 24 | (38.1) | 38 | (25.7) | 0.003 |
| Neither yes nor no | 42 | (33.9) | 459 | (30.4) | 19 | (30.2) | 42 | (28.4) | ||
| No | 28 | (22.6) | 484 | (32.1) | 20 | (31.7) | 68 | (45.9) | ||
| Has free time | Yes | 40 | (32.3) | 452 | (29.9) | 16 | (25.4) | 29 | (19.6) | 0.039 |
| Neither yes nor no | 44 | (35.5) | 479 | (31.7) | 15 | (23.8) | 52 | (35.1) | ||
| No | 40 | (32.3) | 580 | (38.4) | 32 | (50.8) | 67 | (45.3) | ||
| Became Regular | Originally Regular, No Change | Became Irregular | Originally Irregular, No Change | p Value | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| (n = 125) | (n = 1516) | (n = 63) | (n = 148) | ||||||||||
| Current intake of the different food groups | |||||||||||||
| Healthy Diet Score * (0−40 points) | 29.7 | ±4.7 | a | 31.6 | ±4.0 | abc | 29.6 | ±4.8 | b | 28.3 | ±4.6 | c | <0.001 |
| Grain dishes, main dishes (mean), and side dishes (0−12 points) | 9.1 | ±2.4 | a | 9.3 | ±1.8 | b | 8.6 | ±2.5 | 8.2 | ±2.2 | ab | <0.001 | |
| Grain dishes, main dishes (mean), side dishes, fruit, and dairy products (0−20 points) | 15.3 | ±3.8 | a | 15.7 | ±3.0 | b | 14.8 | ±3.9 | 13.9 | ±3.3 | ab | <0.001 | |
| Grain dishes, main dishes (total), side dishes, fruit, and dairy products ** (0−32 points) | 23.8 | ±6.0 | a | 23.8 | ±4.6 | b | 22.8 | ±5.7 | 21.1 | ±5.1 | ab | <0.001 | |
| Infrequently consuming unhealthy foods (0−16 points) † | 11.0 | ±3.8 | a | 12.2 | ±2.7 | ab | 11.4 | ±3.3 | 11.0 | ±2.9 | b | <0.001 | |
| Changes compared with before the pandemic # | |||||||||||||
| Changed Healthy Diet Score # (−13~+13) | 0.8 | ±2.3 | abc | 0.1 | ±1.3 | a | −0.1 | ±1.6 | b | 0.0 | ±1.0 | c | <0.001 |
| Increased score (−4~9 points) | 0.9 | ±2.0 | ab | 0.1 | ±1.1 | a | 0.3 | ±1.5 | 0.0 | ±0.9 | b | <0.001 | |
| Decreased score (−9~4 points) | −0.1 | ±1.0 | 0.0 | ±0.5 | a | −0.4 | ±0.9 | ab | 0.0 | ±0.5 | b | <0.001 | |
| Item Category | Simple Regression | Model 1 | Model 2 | |||||
|---|---|---|---|---|---|---|---|---|
| Standardized Coefficient β | p Value | Standardized Coefficient β | p Value | Standardized Coefficient | p Value | |||
| Basic attributes | Relationship to child | 0.163 | <0.001 | 0.156 | <0.001 | 0.110 | <0.001 | # |
| Employment status of child’s mother | −0.061 | 0.009 | −0.038 | 0.119 | −0.006 | 0.788 | ||
| Child’s sex | 0.018 | 0.448 | 0.026 | 0.280 | 0.040 | 0.070 | ||
| Child’s age | −0.043 | 0.065 | −0.019 | 0.425 | −0.075 | 0.001 | # | |
| BMI percentile | −0.051 | 0.037 | −0.036 | 0.137 | −0.016 | 0.462 | ||
| Lifestyle habits | Wakeup time (weekdays and holidays) | −0.143 | <0.001 | −0.052 | 0.028 | −0.054 | 0.025 | # |
| Bed time (weekdays and holidays) | −0.174 | <0.001 | −0.079 | 0.001 | −0.093 | <0.001 | # | |
| Physical activity time (weekdays) | 0.079 | 0.008 | 0.033 | 0.196 | ||||
| Physical activity time (holidays) | 0.079 | 0.001 | 0.045 | 0.075 | 0.077 | <0.001 | # | |
| Screen time (weekdays) | −0.101 | <0.001 | −0.009 | 0.757 | ||||
| Screen time (holidays) | −0.089 | 0.001 | −0.027 | 0.326 | ||||
| Frequency of defecation | 0.136 | <0.001 | 0.101 | <0.001 | 0.107 | <0.001 | # | |
| Snack frequency | −0.291 | <0.001 | −0.233 | <0.001 | −0.236 | <0.001 | # | |
| Breakfast frequency | 0.249 | <0.001 | 0.141 | <0.001 | 0.137 | <0.001 | # | |
| Originally regular meal times | 0.229 | <0.001 | 0.139 | <0.001 | 0.131 | <0.001 | # | |
| Household circumstances | Eat together (breakfast) | 0.070 | 0.003 | 0.059 | 0.013 | 0.022 | 0.326 | |
| Eat together (dinner) | 0.062 | 0.008 | 0.051 | 0.031 | 0.034 | 0.134 | ||
| How often the respondent cooks | ||||||||
| Every day | 0.192 | <0.001 | 0.187 | <0.001 | 0.092 | 0.007 | # | |
| 3−6 times a week | −0.099 | <0.001 | −0.007 | 0.795 | −0.013 | 0.650 | ||
| Rarely | - | - | - | |||||
| Frequency with which the child is involved in cooking | 0.034 | 0.149 | 0.017 | 0.468 | ||||
| Someone in the family works remotely | −0.024 | 0.305 | −0.022 | 0.336 | ||||
| Financial security | ||||||||
| Yes | 0.067 | 0.004 | 0.028 | 0.319 | 0.021 | 0.423 | ||
| No | −0.062 | 0.008 | −0.061 | 0.034 | −0.021 | 0.419 | ||
| Neither yes nor no | - | - | - | |||||
| Has free time | ||||||||
| Yes | 0.033 | 0.151 | 0.035 | 0.202 | ||||
| No | 0.011 | 0.647 | 0.052 | 0.064 | ||||
| Neither yes nor no | - | - | - | |||||
| n (%) | Increase # | p Value | Decrease # | p Value | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| OR (95% CI) | OR (95% CI) | ||||||||||||
| Meal regularity | Became regular | 125 | (6.7) | 2.21 | (1.35 | − | 3.61) | 0.002 | 1.50 | (0.80 | − | 2.80) | 0.205 |
| Became irregular | 63 | (3.4) | 1.23 | (0.60 | − | 2.53) | 0.564 | 1.85 | (0.92 | − | 3.72) | 0.083 | |
| No change | 1664 | (89.8) | 1.00 | 1.00 | |||||||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tada, Y.; Ueda, Y.; Sasaki, K.; Sugiura, S.; Suzuki, M.; Funayama, H.; Akiyama, Y.; Haraikawa, M.; Eto, K. Mealtime Regularity Is Associated with Dietary Balance among Preschool Children in Japan—A Study of Lifestyle Changes during the COVID-19 Pandemic. Nutrients 2022, 14, 2979. https://doi.org/10.3390/nu14142979
Tada Y, Ueda Y, Sasaki K, Sugiura S, Suzuki M, Funayama H, Akiyama Y, Haraikawa M, Eto K. Mealtime Regularity Is Associated with Dietary Balance among Preschool Children in Japan—A Study of Lifestyle Changes during the COVID-19 Pandemic. Nutrients. 2022; 14(14):2979. https://doi.org/10.3390/nu14142979
Chicago/Turabian StyleTada, Yuki, Yukari Ueda, Kemal Sasaki, Shiro Sugiura, Mieko Suzuki, Hiromi Funayama, Yuka Akiyama, Mayu Haraikawa, and Kumi Eto. 2022. "Mealtime Regularity Is Associated with Dietary Balance among Preschool Children in Japan—A Study of Lifestyle Changes during the COVID-19 Pandemic" Nutrients 14, no. 14: 2979. https://doi.org/10.3390/nu14142979
APA StyleTada, Y., Ueda, Y., Sasaki, K., Sugiura, S., Suzuki, M., Funayama, H., Akiyama, Y., Haraikawa, M., & Eto, K. (2022). Mealtime Regularity Is Associated with Dietary Balance among Preschool Children in Japan—A Study of Lifestyle Changes during the COVID-19 Pandemic. Nutrients, 14(14), 2979. https://doi.org/10.3390/nu14142979






