Iodine Status Modifies the Association between Fluoride Exposure in Pregnancy and Preschool Boys’ Intelligence
Abstract
1. Introduction
2. Materials and Methods
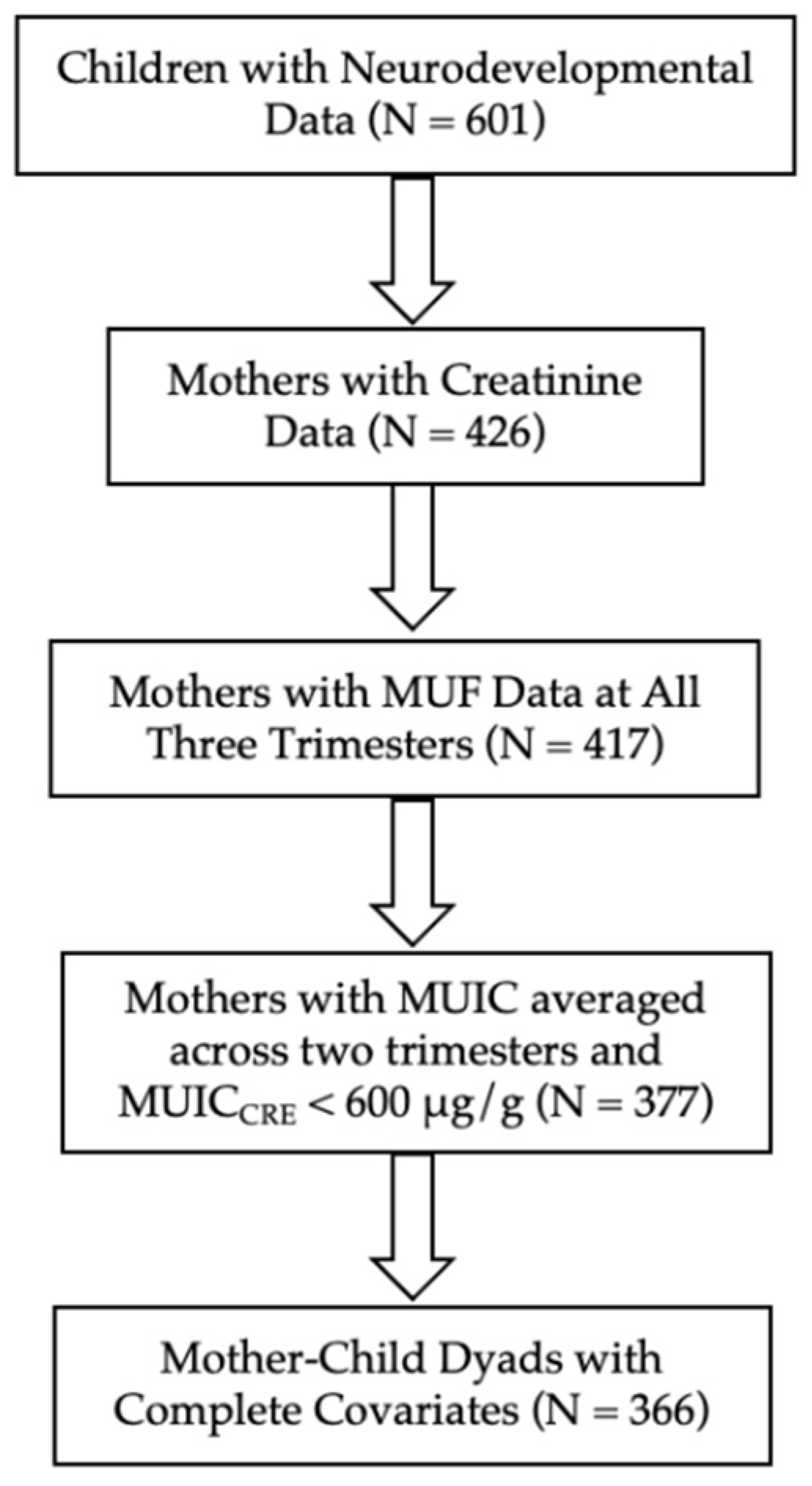
2.1. Participants
2.2. Urine Collection
2.3. Maternal Urinary Fluoride Concentration
2.4. Maternal Urinary Iodine Concentration
2.5. Correcting for Variability in Urinary Dilution
2.6. Children’s Full-Scale Intelligence Quotient
2.7. Covariates
2.8. Statistical Analyses
3. Results
Three-Way Interaction Model
4. Discussion
Strengths and Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Lu, Y.; Sun, Z.R.; Wu, L.N.; Wang, X.; Lu, W.; Liu, S.S. Effect of High-Fluoride Water on Intelligence in Children. Fluoride 2000, 33, 74–78. [Google Scholar]
- Xiang, Q.; Liang, Y.; Chen, L.; Wang, C.; Chen, B.; Chen, X.; Zhou, M. Effect of Fluoride in Drinking Water on Children’s Intelligence. Fluoride 2003, 36, 84–94. [Google Scholar]
- Zhao, L.B.; Liang, G.H.; Zhang, D.N.; Wu, X.R. Effect of a High Fluoride Water Supply on Children’s Intelligence. Fluoride 1996, 29, 190–192. [Google Scholar]
- Bashash, M.; Thomas, D.; Hu, H.; Martinez-Mier, E.A.; Sanchez, B.N.; Basu, N.; Peterson, K.E.; Ettinger, A.S.; Wright, R.; Zhang, Z.; et al. Prenatal Fluoride Exposure and Cognitive Outcomes in Children at 4 and 6–12 Years of Age in Mexico. Environ. Health Perspect. 2017, 125, 97017. [Google Scholar] [CrossRef]
- Till, C.; Green, R.; Flora, D.; Hornung, R.; Martinez-Mier, E.A.; Blazer, M.; Farmus, L.; Ayotte, P.; Muckle, G.; Lanphear, B. Fluoride Exposure from Infant Formula and Child IQ in a Canadian Birth Cohort. Environ. Int. 2020, 134, 105315. [Google Scholar] [CrossRef]
- Green, R.; Lanphear, B.; Hornung, R.; Flora, D.; Martinez-Mier, E.A.; Neufeld, R.; Ayotte, P.; Muckle, G.; Till, C. Association between Maternal Fluoride Exposure during Pregnancy and IQ Scores in Offspring in Canada. JAMA Pediatr. 2019, 173, 940–948. [Google Scholar] [CrossRef]
- Chaitanya, N.; Karunakar, P.; Allam, N.; Priya, M.; Alekhya, B.; Nauseen, S. A Systematic Analysis on Possibility of Water Fluoridation Causing Hypothyroidism. Indian J. Dent. Res. 2018, 29, 358–363. [Google Scholar] [CrossRef]
- Wang, M.; Liu, L.; Li, H.; Li, Y.; Liu, H.; Hou, C.; Zeng, Q.; Li, P.; Zhao, Q.; Dong, L.; et al. Thyroid Function, Intelligence, and Low-Moderate Fluoride Exposure among Chinese School-Age Children. Environ. Int. 2020, 134, 105229. [Google Scholar] [CrossRef]
- Khandare, A.L.; Validandi, V.; Gourineni, S.R.; Gopalan, V.; Nagalla, B. Dose-Dependent Effect of Fluoride on Clinical and Subclinical Indices of Fluorosis in School Going Children and Its Mitigation by Supply of Safe Drinking Water for 5 Years: An Indian Study. Environ. Monit. Assess. 2018, 190, 1–8. [Google Scholar] [CrossRef]
- KheradPisheh, Z.; Mirzaei, M.; Mahvi, A.H.; Mokhtari, M.; Azizi, R.; Fallahzadeh, H.; Ehrampoush, M.H. Impact of Drinking Water Fluoride on Human Thyroid Hormones: A Case-Control Study. Sci. Rep. 2018, 8, 2674. [Google Scholar] [CrossRef]
- Peckham, S.; Lowery, D.; Spencer, S. Are Fluoride Levels in Drinking Water Associated with Hypothyroidism Prevalence in England? A Large Observational Study of GP Practice Data and Fluoride Levels in Drinking Water. J. Epidemiol. Community Health 2015, 69, 619–624. [Google Scholar] [CrossRef] [PubMed]
- National Research Council. Fluoride in Drinking Water; A Scientific Review of EPA’s Standards; National Academies Press: Washington, DC, USA, 2006; ISBN 9780309101288. [Google Scholar]
- Institute of Medicine. Dietary Reference Intakes for Vitamin A, Vitamin K, Arsenic, Boron, Chromium, Copper, Iodine, Iron, Manganese, Molybdenum, Nickel, Silicon, Vanadium, and Zinc: A Report of the Panel on Micronutrients… [et al.], Standing Committee on the Scientific Eva; National Academies Press: Cambridge, MA, USA, 2001. [Google Scholar]
- Murcia, M.; Espada, M.; Julvez, J.; Llop, S.; Lopez-Espinosa, M.J.; Vioque, J.; Basterrechea, M.; Rianõ, I.; González, L.; Alvarez-Pedrerol, M.; et al. Iodine Intake from Supplements and Diet during Pregnancy and Child Cognitive and Motor Development: The INMA Mother and Child Cohort Study. J. Epidemiol. Community Health 2018, 72, 216–222. [Google Scholar] [CrossRef] [PubMed]
- de Escobar, G.M.; Obregón, M.J.; Escobar del Rey, F. Maternal Thyroid Hormones Early in Prenancy and Fetal Brain Development. Best Pract. Res. Clin. Endocrinol. Metab. 2004, 18, 225–248. [Google Scholar] [CrossRef]
- Glinoer, D. The Regulation of Thyroid Function during Normal Pregnancy: Importance of the Iodine Nutrition Status. Best Pract. Res. Clin. Endocrinol. Metab. 2004, 18, 133–152. [Google Scholar] [CrossRef]
- Katz, P.M.; Leung, A.M.; Braverman, L.E.; Pearce, E.N.; Tomlinson, G.; He, X.; Vertes, J.; Okun, N.; Walfish, P.G.; Feig, D.S. Iodine Nutrition during Pregnancy in Toronto, Canada. Endocr. Pract. 2013, 19, 206–211. [Google Scholar] [CrossRef] [PubMed][Green Version]
- De Escobar, G.M.; Obregón, M.J.; Del Rey, F.E. Iodine Deficiency and Brain Development in the First Half of Pregnancy. Public Health Nutr. 2007, 10, 1554–1570. [Google Scholar] [CrossRef] [PubMed]
- Zimmermann, M.B. Iodine Deficiency in Pregnancy and the Effects of Maternal Iodine Supplementation on the Offspring: A Review. Am. J. Clin. Nutr. 2009, 89, 668–672. [Google Scholar] [CrossRef] [PubMed]
- Melse-Boonstra, A.; Jaiswal, N. Iodine Deficiency in Pregnancy, infancy, and childhood and its consequences for brain development. Best Pract. Res. Clin. Endocrinol. Metab. 2010, 24, 29–38. [Google Scholar] [CrossRef] [PubMed]
- Bath, S.C. The Effect of Iodine Deficiency during Pregnancy on Child Development. Proc. Nutr. Soc. 2019, 78, 150–160. [Google Scholar] [CrossRef]
- Pearce, E.N. Effects of Iodine Deficiency in Pregnancy. J. Trace Elem. Med. Biol. 2012, 26, 131–133. [Google Scholar] [CrossRef]
- Bath, S.C.; Steer, C.D.; Golding, J.; Emmett, P.; Rayman, M.P. Effect of Inadequate Iodine Status in UK Pregnant Women on Cognitive Outcomes in Their Children: Results from the Avon Longitudinal Study of Parents and Children (ALSPAC). Lancet 2013, 382, 331–337. [Google Scholar] [CrossRef]
- Levie, D.; Korevaar, T.I.M.; Bath, S.C.; Murcia, M.; Dineva, M.; Llop, S.; Espada, M.; Van Herwaarden, A.E.; De Rijke, Y.B.; Ibarluzea, J.M.; et al. Association of Maternal Iodine Status with Child IQ: A Meta-Analysis of Individual Participant Data. J. Clin. Endocrinol. Metab. 2019, 104, 5957–5967. [Google Scholar] [CrossRef] [PubMed]
- Ghassabian, A.; Steenweg-de Graaff, J.; Peeters, R.P.; Ross, H.A.; Jaddoe, V.W.; Hofman, A.; Verhulst, F.C.; White, T.; Tiemeier, H. Maternal Urinary Iodine Concentration in Pregnancy and Children’s Cognition: Results from a Population-Based Birth Cohort in an Iodine-Sufficient Area. BMJ Open 2014, 4, e005520. [Google Scholar] [CrossRef] [PubMed]
- Rebagliato, M.; Murcia, M.; Álvarez-Pedrerol, M.; Espada, M.; Fernández-Somoano, A.; Lertxundi, N.; Navarrete-Muñoz, E.M.; Forns, J.; Aranbarri, A.; Llop, S.; et al. Iodine Supplementation during Pregnancy and Infant Neuropsychological Development. Am. J. Epidemiol. 2013, 177, 944–953. [Google Scholar] [CrossRef]
- Ren, D.; Li, K.; Liu, D. A Study of the Intellectual Ability of 8–14 Year-Old Children in High Fluoride, Low Iodine Areas. Fluoride 2008, 41, 319–320. [Google Scholar]
- Fa-Fu, L.; Aihaiti, H.X.Z.; Jin, U.; Ji-Yong, J.; Maimaiti, A. The Relationship of a Low-Iodine and High- Fluoride Environment to Subclinical Cretinism in Xinjiang. Iodine Defic. Disord. Newsl. 1991, 7, 24–25. [Google Scholar]
- Wang, J.; Ge, Y.; Ning, H.; Wang, S. Effects of High Fluoride and Low Iodine on Biochemical Indexes of the Brain and Learning-Memory of Offspring Rats. Fluoride 2004, 37, 201–208. [Google Scholar]
- Hong, J.H.; Ge, Y.M.; Ning, H.M. Effects of High Fluoride and Low Iodine on Learning-Memory and TchE of Brain in Offspring Rats. China Prev. Med. 2005, 6, 489–491. [Google Scholar]
- Mioto, V.C.B.; de Castro Nassif Gomes Monteiro, A.C.; De Camargo, R.Y.A.; Borel, A.R.; Catarino, R.M.; Kobayashi, S.; Chammas, M.C.; Marui, S. High Prevalence of Iodine Deficiency in Pregnant Women Living in Adequate Iodine Area. Endocr. Connect. 2018, 7, 762–767. [Google Scholar] [CrossRef]
- Perrine, C.G.; Herrick, K.A.; Gupta, P.M.; Caldwell, K.L.; Activity, P.; Surveys, N.E. Iodine Status of Pregnant Women and Women of Reproductive Age in the United States. Thyroid 2019, 29, 153–154. [Google Scholar] [CrossRef]
- Green, R.; Rubenstein, J.; Popoli, R.; Capulong, R.; Till, C. Sex-Specific Neurotoxic Effects of Early-Life Exposure to Fluoride: A Review of the Epidemiologic and Animal Literature. Curr. Epidemiol. Rep. 2020, 7, 263–273. [Google Scholar] [CrossRef] [PubMed]
- Arbuckle, T.E.; Fraser, W.D.; Fisher, M.; Davis, K.; Liang, C.L.; Lupien, N.; Bastien, S.; Velez, M.P.; Von Dadelszen, P.; Hemmings, D.G.; et al. Cohort Profile: The Maternal-Infant Research on Environmental Chemicals Research Platform. Paediatr. Perinat. Epidemiol. 2013, 27, 415–425. [Google Scholar] [CrossRef] [PubMed]
- Li, F.; Wan, S.; Zhang, L.; Li, B.; He, Y.; Shen, H.; Liu, L. A Meta-Analysis of the Effect of Iodine Excess on the Intellectual Development of Children in Areas with High Iodine Levels in Their Drinking Water. Biol. Trace Elem. Res. 2022, 200, 1580–1590. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Worldwide Iodine Status. In WHO Global Database on Iodine Deficiency; Department of Nutrition for Health and Development World Health Organization: Geneva, Switzerland, 2004. [Google Scholar]
- Luo, J.; Li, C.; Zhang, X.; Shan, Z.; Teng, W. Reference Intervals of the Ratio of Urine Iodine to Creatinine in Pregnant Women in an Iodine-Replete Area of China. Biol. Trace Elem. Res. 2020, 199, 62–69. [Google Scholar] [CrossRef]
- Till, C.; Green, R.; Grundy, J.G.; Hornung, R.; Neufeld, R.; Martinez-Mier, E.A.; Ayotte, P.; Muckle, G.; Lanphear, B. Community Water Fluoridation and Urinary Fluoride Concentrations in a National Sample of Pregnant Women in Canada. Environ. Health Perspect. 2018, 126, 107001. [Google Scholar] [CrossRef]
- Martínez-Mier, E.A.; Cury, J.A.; Heilman, J.R.; Katz, B.P.; Levy, S.M.; Li, Y.; Maguire, A.; Margineda, J.; O’Mullane, D.; Phantumvanit, P.; et al. Development of Gold Standard Ion-Selective Electrode-Based Methods for Fluoride Analysis. Caries Res. 2011, 45, 3–12. [Google Scholar] [CrossRef]
- Zimmermann, M.B.; Andersson, M. Assessment of Iodine Nutrition in Populations: Past, Present, and Future. Nutr. Rev. 2012, 70, 553–570. [Google Scholar] [CrossRef]
- Li, C.; Peng, S.; Zhang, X.; Xie, X.; Wang, D.; Mao, J.; Teng, X.; Shan, Z.; Teng, W. The Urine Iodine to Creatinine as an Optimal Index of Iodine during Pregnancy in an Iodine Adequate Area in China. J. Clin. Endocrinol. Metab. 2016, 101, 1290–1298. [Google Scholar] [CrossRef]
- Caldwell, B.M.; Bradley, R.H. Home Observation for Measurement of the Environment; University of Arkansas: Little Rock, AR, USA, 1979. [Google Scholar]
- Bauer, D.J.; Curran, P.J.; Thurstone, L.L. Probing Interactions in Fixed and Multilevel Regression: Inferential and Graphical Techniques. Multivariate Behav. Res. 2005, 40, 373–400. [Google Scholar] [CrossRef]
- Van Mil, N.H.; Tiemeier, H.; Bongers-Schokking, J.J.; Ghassabian, A.; Hofman, A.; Hooijkaas, H.; Jaddoe, V.W.V.; de Muinck Keizer-Schrama, S.M.; Steegers, E.A.P.; Visser, T.J.; et al. Low Urinary Iodine Excretion during Early Pregnancy Is Associated with Alterations in Executive Functioning in Children. J. Nutr. 2012, 142, 2167–2174. [Google Scholar] [CrossRef]
- Du, Y.; Zhou, G.; Gong, B.; Ma, J.; An, N.; Gao, M.; Yang, M.; Ma, Q.; Huang, H.; Zuo, Q.; et al. Iodine Modifies the Susceptibility of Thyroid to Fluoride Exposure in School-Age Children: A Cross-Sectional Study in Yellow River Basin, Henan, China. Biol. Trace Elem. Res. 2021, 199, 3658–3666. [Google Scholar] [CrossRef] [PubMed]
- Ge, Y.; Niu, R.; Zhang, J.; Wang, J. Proteomic Analysis of Brain Proteins of Rats Exposed to High Fluoride and Low Iodine. Arch. Toxicol. 2011, 85, 27–33. [Google Scholar] [CrossRef] [PubMed]
- Ge, Y.; Ning, H.; Wang, S.; Wang, J. Effects of High Fluoride and Low Iodine on Brain Histopathology in Offspring Rats. Fluoride 2005, 38, 127–132. [Google Scholar]
- Ge, Y.; Ning, H.; Feng, C.; Wang, H.; Yan, X.; Wang, S.; Wang, J. Apoptosis in Brain Cells of Offspring Rats Exposed to High Fluoride and Low Iodine. Fluoride 2006, 39, 173–178. [Google Scholar]
- Malin, A.J.; Riddell, J.; McCague, H.; Till, C. Fluoride Exposure and Thyroid Function among Adults Living in Canada: Effect Modification by Iodine Status. Environ. Int. 2018, 121, 667–674. [Google Scholar] [CrossRef] [PubMed]
- Waugh, D.T. Fluoride exposure induces inhibition of sodium/iodide symporter (NIS) contributing to impaired iodine absorption and iodine deficiency: Molecular mechanisms of inhibition and implications for public health. Int. J. Environ. Res. Public Health 2019, 16, 1086. [Google Scholar] [CrossRef] [PubMed]
- Singh, N.; Verma, K.G.; Verma, P.; Sidhu, G.K.; Sachdeva, S. A comparative study of fluoride ingestion levels, serum thyroid hormone & TSH level derangements, dental fluorosis status among school children from endemic and non-endemic fluorosis areas. Springerplus 2014, 3, 7. [Google Scholar] [CrossRef] [PubMed]
- Zhao, W.; Zhu, H.; Yu, Z.; Aoki, K.; Misumi, J.; Zhang, X. Long-Term Effects of Various Iodine and Fluorine Doses on the Thyroid and Fluorosis in Mice. Endocr. Regul. 1998, 32, 63–70. [Google Scholar]
- Guan, Z.Z.; Zhuang, Z.-J.; Yang, P.-S.; Pan, S. Synergistic Action of Iodine-Deficiency and Fluorine-Intoxication of Rat Thyroid. Chin. Med. J. 1988, 101, 679–684. [Google Scholar]
- Rovet, J.F. The Role of Thyroid Hormones for Brain Development and Cognitive Function. Endocr. Dev. 2014, 26, 26–43. [Google Scholar] [CrossRef]
- Moog, N.K.; Entringer, S.; Heim, C.; Wadhwa, P.D.; Kathmann, N.; Buss, C. Influence of Maternal Thyroid Hormones during Gestation on Fetal Brain Development. Neuroscience 2017, 342, 68–100. [Google Scholar] [CrossRef] [PubMed]
- Prezioso, G.; Giannini, C.; Chiarelli, F. Effect of Thyroid Hormones on Neurons and Neurodevelopment. Horm. Res. Paediatr. 2018, 90, 73–81. [Google Scholar] [CrossRef]
- Jansen, T.A.; Korevaar, T.I.M.; Mulder, T.A.; White, T.; Muetzel, R.L.; Peeters, R.P.; Tiemeier, H. Maternal Thyroid Function during Pregnancy and Child Brain Morphology: A Time Window-Specific Analysis of a Prospective Cohort. Lancet Diabetes Endocrinol. 2019, 7, 629–637. [Google Scholar] [CrossRef]
- Miranda, A.; Sousa, N. Maternal Hormonal Milieu Influence on Fetal Brain Development. Brain Behav. 2018, 8, e00920. [Google Scholar] [CrossRef] [PubMed]
- Zimmermann, M.B. The Effects of Iodine Deficiency in Pregnancy and Infancy. Paediatr. Perinat. Epidemiol. 2012, 26, 108–117. [Google Scholar] [CrossRef] [PubMed]
- Hall, M.; Green, R.; Goodman, C.V.; Farmus, L.; Lanphear, B.; Martinez-Mier, A.; Hornung, R.; Ayotte, P.; Till, C. Fluoride Exposure and Hypothyroidism in a Canadian Pregnancy Cohort. Birth Defects Res. 2021, 113, 804. [Google Scholar]
- Batista, G.; Hensch, T.K. Critical Period Regulation by Thyroid Hormones: Potential Mechanisms and Sex-Specific Aspects. Front. Mol. Neurosci. 2019, 12, 77. [Google Scholar] [CrossRef]
- Duarte-Guterman, P.; Navarro-Martín, L.; Trudeau, V.L. Mechanisms of Crosstalk between Endocrine Systems: Regulation of Sex Steroid Hormone Synthesis and Action by Thyroid Hormones. Gen. Comp. Endocrinol. 2014, 203, 69–85. [Google Scholar] [CrossRef]
- Baksi, S.; Pradhan, A. Thyroid Hormone: Sex-Dependent Role in Nervous System Regulation and Disease. Biol. Sex Differ. 2021, 12, 25. [Google Scholar] [CrossRef]
- Li, P.; Teng, Y.; Ru, X.; Liu, Z.; Han, Y.; Tao, F.; Huang, K. Sex-Specific Effect of Maternal Thyroid Hormone Trajectories on Preschoolers’ Behavioral Development: A Birth Cohort Study. J. Clin. Endocrinol. Metab. 2022, 107, e2037–e2046. [Google Scholar] [CrossRef]
- König, F.; Andersson, M.; Hotz, K.; Aeberli, I.; Zimmermann, M.B. Ten Repeat Collections for Urinary Iodine from Spot Samples or 24-Hour Samples Are Needed to Reliably Estimate Individual Iodine Status in Women. J. Nutr. 2011, 141, 2049–2054. [Google Scholar] [CrossRef] [PubMed]

| Demographic Characteristic (Mean ± SD or N (%)) | Complete Data (N = 366) | Incomplete Data (N = 211) | p |
|---|---|---|---|
| Mothers | |||
| Maternal Age (years) | 32.50 ± 4.51 | 32.55 ± 4.62 | 0.899 |
| Married or Common Law | 353 (96.54) | 205 (97.16) | 0.646 |
| White | 334 (91.26) | 181 (85.78) | 0.041 |
| Bachelor’s Degree or Higher | 243 (66.39) | 142 (67.30) | 0.824 |
| Taking a prenatal multivitamin | 319 (87.40) | 175 (82.94) | 0.140 |
| HOME Score | 47.23 ± 4.44 | 47.40 ± 4.10 | 0.649 |
| Children | |||
| Male | 186 (50.82) | 98 (46.44) | 0.311 |
| Age at Testing (years) | 3.44 ± 0.32 | 3.40 ± 0.31 | 0.144 |
| Urinary Measurement | All | Boys | Girls | ||||
|---|---|---|---|---|---|---|---|
| n | Median (IQR) | n | Median (IQR) | n | Median (IQR) | p 1 | |
| MUFCRE (mg/g) | 366 | 0.61 (0.49) | 186 | 0.63 (0.52) | 180 | 0.61 (0.48) | 0.538 |
| MUICCRE (μg/g) | 366 | 294 (181) | 186 | 309 (181) | 180 | 287 (203) | 0.059 |
| Low | 86 | 148 (47) | 31 | 131 (73) | 55 | 152 (37) | 0.083 |
| Adequate | 280 | 341 (165) | 155 | 348 (187) | 125 | 336 (146) | 0.893 |
| Outcome | n | Mean ± SD | n | Mean ± SD | n | Mean ± SD | p 1 |
| FSIQ | 366 | 107.46 ± 13.75 | 186 | 105.25 ± 14.90 | 180 | 109.75 ± 12.09 | 0.002 |
| Variable | B | SE(B) | p |
|---|---|---|---|
| MUFCRE (mg/g) | −5.89 | 1.85 | 0.002 |
| MUICCRE (μg/g) | −0.03 | 0.01 | 0.023 |
| Sex | −3.09 | 2.17 | 0.155 |
| MUFCRE × MUICCRE | 0.02 | 0.01 | 0.042 |
| MUFCRE × Sex | 8.51 | 2.40 | <0.001 |
| MUICCRE × Sex | 0.03 | 0.02 | 0.042 |
| MUFCRE × MUICCRE × Sex | −0.04 | 0.02 | 0.019 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Goodman, C.V.; Hall, M.; Green, R.; Chevrier, J.; Ayotte, P.; Martinez-Mier, E.A.; McGuckin, T.; Krzeczkowski, J.; Flora, D.; Hornung, R.; et al. Iodine Status Modifies the Association between Fluoride Exposure in Pregnancy and Preschool Boys’ Intelligence. Nutrients 2022, 14, 2920. https://doi.org/10.3390/nu14142920
Goodman CV, Hall M, Green R, Chevrier J, Ayotte P, Martinez-Mier EA, McGuckin T, Krzeczkowski J, Flora D, Hornung R, et al. Iodine Status Modifies the Association between Fluoride Exposure in Pregnancy and Preschool Boys’ Intelligence. Nutrients. 2022; 14(14):2920. https://doi.org/10.3390/nu14142920
Chicago/Turabian StyleGoodman, Carly V., Meaghan Hall, Rivka Green, Jonathan Chevrier, Pierre Ayotte, Esperanza Angeles Martinez-Mier, Taylor McGuckin, John Krzeczkowski, David Flora, Richard Hornung, and et al. 2022. "Iodine Status Modifies the Association between Fluoride Exposure in Pregnancy and Preschool Boys’ Intelligence" Nutrients 14, no. 14: 2920. https://doi.org/10.3390/nu14142920
APA StyleGoodman, C. V., Hall, M., Green, R., Chevrier, J., Ayotte, P., Martinez-Mier, E. A., McGuckin, T., Krzeczkowski, J., Flora, D., Hornung, R., Lanphear, B., & Till, C. (2022). Iodine Status Modifies the Association between Fluoride Exposure in Pregnancy and Preschool Boys’ Intelligence. Nutrients, 14(14), 2920. https://doi.org/10.3390/nu14142920







