Association between Early Life Famine Exposure and Metabolic Syndrome in Adulthood
Abstract
:1. Introduction
2. Materials and Methods
2.1. Data Source
2.2. Research Subjects
- (1)
- Non-exposed group: adults born between 01.10.1962 and 30.09.1964.
- (2)
- Fetal exposure group: adults born between 01.10.1959 and 30.09.1961.
- (3)
- Early childhood exposure group: adults born between 01.10.1956 and 30.09.1958.
- (4)
- Middle childhood exposure group: adults born between 01.10.1954 and 30.09.1956.
- (5)
- Late childhood exposure group: adults born between 01.10.1952 and 30.09.1954.
2.3. Survey Content and Method
2.4. Quality Control
2.5. MetS Diagnostic Criteria and Its Related Definitions
2.5.1. Diagnostic Criteria
- (1)
- A waist circumference of ≥90 cm for men and ≥80 cm for women;
- (2)
- A systolic blood pressure of ≥130 mmHg or a diastolic blood pressure of ≥85 mmHg or receiving anti-hypertension treatment;
- (3)
- A fasting triglyceride level of ≥1.7 mmol/L or receiving corresponding treatment;
- (4)
- A high-density lipoprotein cholesterol (HDL-C) level of <1.03 mmol/L for men and <1.30 mmol/L for women or receiving corresponding treatment;
- (5)
- A fasting plasma glucose (FPG) level of ≥5.6 mmol/L or receiving anti-diabetes treatment or reporting previously physician-diagnosed diabetes.
2.5.2. Definition of Famine Severity
2.5.3. Relevant Definitions
- (1)
- Area of the country: the southern provinces are Shanghai, Jiangsu, Zhejiang, Anhui, Fujian, Jiangxi, Hubei, Hunan, Guangdong, Guangxi, Hainan, Chongqing, Sichuan, Guizhou and Yunnan, 15 provinces in total. The northern provinces are Beijing, Tianjin, Hebei, Shanxi, Inner Mongolia, Liaoning, Jilin, Heilongjiang, Shandong, Henan, Tibet, Shaanxi, Gansu, Ningxia, Qinghai and Xinjiang, 16 provinces in total,
- (2)
- Body mass index (BMI): described by non-overweight or obese group (BMI < 24 kg/m2) and overweight or obese group (BMI ≥ 24 kg/m2).
- (3)
- Education level: low (primary school or below), medium (junior school) and high (high school and higher).
- (4)
- Income: divided into low level, medium level, high level and very high level by quintile.
- (5)
- Smoking was divided into smoking and non-smoking.
- (6)
- Drinking was divided into drinking and non-drinking.
- (7)
- Physically inactive: within one week, less than 150 min of moderate-intensity activity, less than 75 min of high-intensity activity or less than 150 min of above activity [15].
- (8)
- Family history of hypertension (or diabetes) was defined as one or more lineal relatives being diagnosed with hypertension (or diabetes).
- (9)
- Dietary pattern: The dietary pattern was established by using factor analysis, which was divided into egg, milk and fruit pattern, aquatic vegetable and meat pattern and staple food soybean and nut pattern.
2.6. Statistical Analysis
2.6.1. Descriptions and Tests
2.6.2. Association between Famine Exposure and MetS in Adulthood
3. Results
3.1. Sample Description
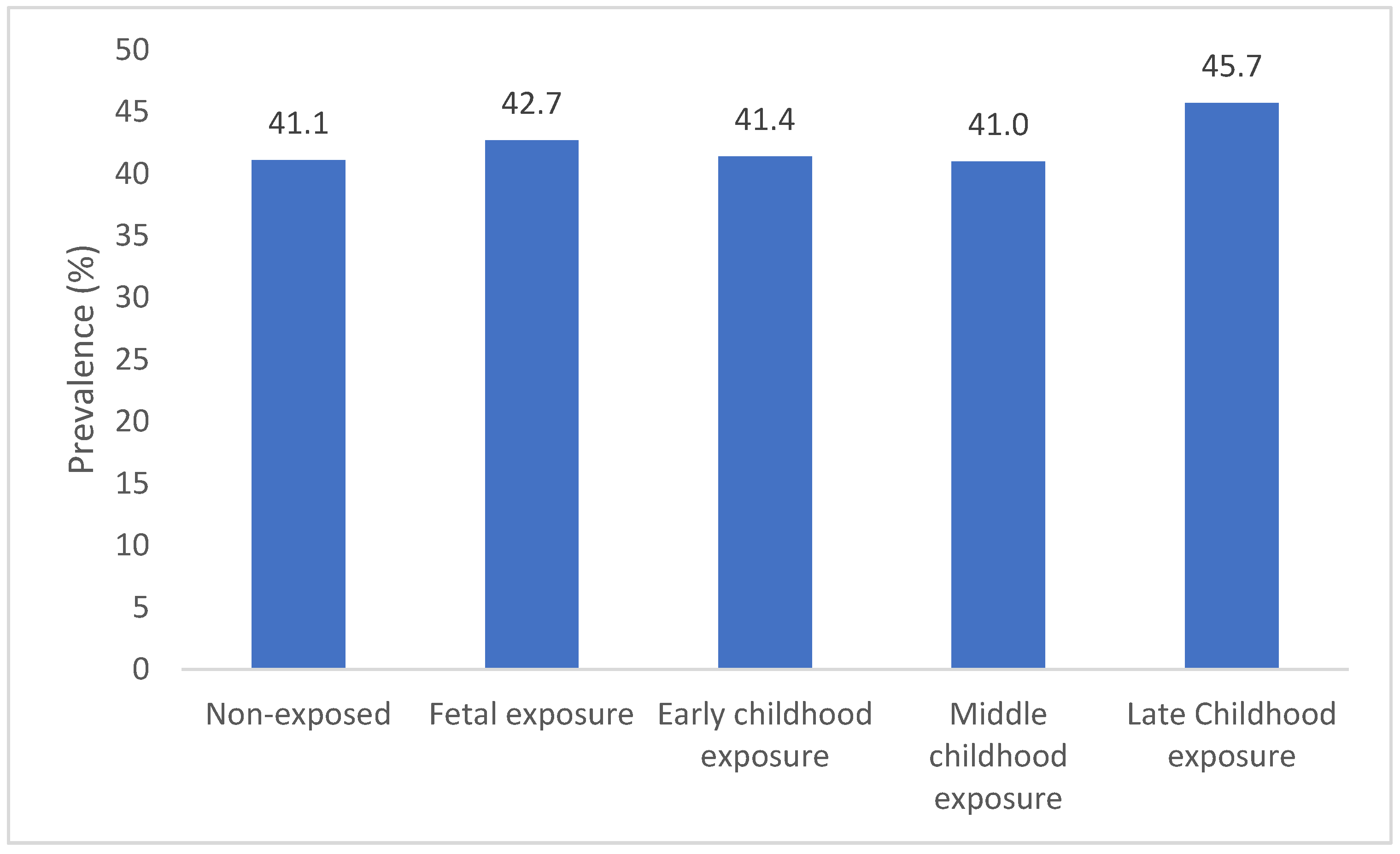
3.2. Prevalence of MetS
3.3. Association between Famine Exposure and MetS in Adulthood
3.4. Stratified Analysis
4. Discussion
4.1. Sex Differences in Early Life Famine Exposure and MetS
4.2. Different BMI of Early Life Famine Exposure and MetS
4.3. Different Famine Severity of Early Life Famine Exposure and MetS
4.4. Different Areas of Early Life Famine Exposure and MetS
4.5. Possible Mechanisms
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Saklayen, M.G. The Global Epidemic of the Metabolic Syndrome. Curr. Hypertens. Rep. 2018, 20, 12. [Google Scholar] [CrossRef] [Green Version]
- Aguilar, M.; Bhuket, T.; Torres, S.; Liu, B.; Wong, R.J. Prevalence of the metabolic syndrome in the United States, 2003–2012. JAMA 2015, 313, 1973–1974. [Google Scholar] [CrossRef] [PubMed]
- Lim, S.; Shin, H.; Song, J.H.; Kwak, S.H.; Kang, S.M.; Won Yoon, J.; Choi, S.H.; Cho, S.I.; Park, K.S.; Lee, H.K.; et al. Increasing Prevalence of Metabolic Syndrome in Korea: The Korean National Health and Nutrition Examination Survey for 1998–2007. Diabetes Care 2011, 34, 1323–1328. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gu, D.; Reynolds, K.; Wu, X.; Chen, J.; Duan, X.; Reynolds, R.F.; Whelton, P.K.; He, J.; InterASIA Collaborative Group. Prevalence of the metabolic syndrome and overweight among adults in China. Lancet 2005, 365, 1398–1405. [Google Scholar] [CrossRef]
- Li, Y.; Zhao, L.; Yu, D.; Wang, Z.; Ding, G. Metabolic syndrome prevalence and its risk factors among adults in China: A nationally representative cross-sectional study. PLoS ONE 2018, 13, e199293. [Google Scholar]
- Wang, G.; Li, L.; Pan, Y.; Tian, G.; Lin, W.; Li, Z.; Chen, Z.; Gong, Y.; Kikano, G.E.; Stange, K.C.; et al. Prevalence of metabolic syndrome among urban community residents in China. BMC Public Health 2013, 13, 599. [Google Scholar] [CrossRef] [Green Version]
- Barker, D.J.; Osmond, C. Infant mortality, childhood nutrition, and ischaemic heart disease in England and Wales. Lancet 1986, 1, 1077–1081. [Google Scholar] [CrossRef]
- Barker, D.J.P. The Developmental Origins of Adult Disease. J. Am. Coll. Nutr. 2004, 23, 588S–595S. [Google Scholar] [CrossRef]
- Yan, X.; Zhao, X.; Li, J.; He, L.; Xu, M. Effects of early-life malnutrition on neurodevelopment and neuropsychiatric disorders and the potential mechanisms. Prog. Neuropsychopharmacol. Biol. Psychiatry 2018, 83, 64–75. [Google Scholar] [CrossRef]
- Campbell, G.J.; Senior, A.M.; Bell-Anderson, K.S. Metabolic Effects of High Glycaemic Index Diets: A Systematic Review and Meta-Analysis of Feeding Studies in Mice and Rats. Nutrients 2017, 9, 646. [Google Scholar] [CrossRef] [Green Version]
- Yu, D.; Zhao, L.; Zhang, J.; Yang, Z.; Ding, G. China Nutrition and Health Surveys (19822017). China CDC Wkly. 2021, 3, 193–195. [Google Scholar] [CrossRef] [PubMed]
- Yu, C.; Wang, J.; Wang, F.; Han, X.; Hu, H.; Yuan, J.; Miao, X.; Yao, P.; Wei, S.; Wang, Y.; et al. Victims of Chinese famine in early life have increased risk of metabolic syndrome in adulthood. Nutrition 2018, 53, 20–25. [Google Scholar] [CrossRef]
- Grundy, S.M.; Cleeman, J.I.; Daniels, S.R.; Donato, K.A.; Eckel, R.H.; Franklin, B.A.; Gordon, D.J.; Krauss, R.M.; Savage, P.J.; Smith, S.C.; et al. Diagnosis and Management of the Metabolic Syndrome. Circulation 2005, 112, 2735–2752. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shi, Z.; Nicholls, S.J.; Taylor, A.W.; Magliano, D.J.; Appleton, S.; Zimmet, P. Early life exposure to Chinese famine modifies the association between hypertension and cardiovascular disease. J. Hypertens. 2018, 36, 54–60. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. WHO Guidelines on Physical Activity and Sedentary Behaviour; World Health Organization: Geneva, Switzerland, 2020. [Google Scholar]
- Arage, G.; Belachew, T.; Hassen, H.; Abera, M.; Abdulhay, F.; Abdulahi, M.; Hassen, A.K. Effects of prenatal exposure to the 1983–1985 Ethiopian great famine on the metabolic syndrome in adults: A historical cohort study. Br. J. Nutr. 2020, 124, 1052–1060. [Google Scholar] [CrossRef]
- de Rooij, S.R.; Painter, R.C.; Holleman, F.; Bossuyt, P.M.; Roseboom, T.J. The metabolic syndrome in adults prenatally exposed to the Dutch famine. Am. J. Clin. Nutr. 2007, 86, 1219–1224. [Google Scholar] [CrossRef]
- Smil, V. China’s great famine: 40 years later. BMJ 1999, 319, 1619–1621. [Google Scholar] [CrossRef] [Green Version]
- Roseboom, T.; Painter, R.; de Rooij, S. Prenatal Famine Exposure and Long-Term Consequences for Anthropometry and Adult Health; Springer: New York, NY, USA, 2012; pp. 1021–1032. [Google Scholar]
- Wang, N.; Wang, X.; Li, Q.; Han, B.; Chen, Y.; Zhu, C.; Chen, Y.; Lin, D.; Wang, B.; Jensen, M.D.; et al. The famine exposure in early life and metabolic syndrome in adulthood. Clin. Nutr. 2017, 36, 253–259. [Google Scholar] [CrossRef] [Green Version]
- Eriksson, J.G.; Kajantie, E.; Osmond, C.; Thornburg, K.; Barker, D.J.P. Boys live dangerously in the womb. Am. J. Hum. Biol. 2010, 22, 330–335. [Google Scholar] [CrossRef] [Green Version]
- Song, S. Does famine influence sex ratio at birth? Evidence from the 1959–1961 Great Leap Forward Famine in China. Proc. R. Soc. B Biol. Sci. 2012, 279, 2883–2890. [Google Scholar] [CrossRef] [Green Version]
- Roseboom, T.J.; van der Meulen, J.H.P.; Ravelli, A.C.J.; Osmond, C.; Barker, D.J.P.; Bleker, O.P. Effects of prenatal exposure to the Dutch famine on adult disease in later life: An overview. Mol. Cell. Endocrinol. 2001, 185, 93–98. [Google Scholar] [CrossRef]
- Li, Y.; Jaddoe, V.W.; Qi, L.; He, Y.; Wang, D.; Lai, J.; Zhang, J.; Fu, P.; Yang, X.; Hu, F.B. Exposure to the Chinese Famine in Early Life and the Risk of Metabolic Syndrome in Adulthood. Diabetes Care 2011, 34, 1014–1018. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wang, Z.; Li, C.; Yang, Z.; Zou, Z.; Ma, J. Infant exposure to Chinese famine increased the risk of hypertension in adulthood: Results from the China Health and Retirement Longitudinal Study. BMC Public Health 2016, 16, 435. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wang, Z.; Zou, Z.; Wang, S.; Yang, Z.; Ma, J. Chinese famine exposure in infancy and metabolic syndrome in adulthood: Results from the China health and retirement longitudinal study. Eur. J. Clin. Nutr. 2018, 73, 724–732. [Google Scholar] [CrossRef]
- Peng, Y.; Hai, M.; Li, P.; Chen, Y. Association of Exposure to Chinese Famine in Early Life with the Risk of Metabolic Syndrome in Adulthood. Ann. Nutr. Metab. 2020, 76, 140–146. [Google Scholar] [CrossRef]
- Liu, D.; Yu, D.; Zhao, L.; Fang, H.; Zhang, J.; Wang, J.; Yang, Z.; Zhao, W. Exposure to Famine During Early Life and Abdominal Obesity in Adulthood: Findings from the Great Chinese Famine During 1959–1961. Nutrients 2019, 11, 903. [Google Scholar] [CrossRef] [Green Version]
- Zhao, L.Y.; Liu, D.; Yu, D.M.; Zhang, J.; Wang, J.Z.; Zhao, W.H. Challenges Brought about by Rapid Changes in Chinese Diets: Comparison with Developed Countries and Implications for Further Improvement. Biomed. Environ. Sci. 2018, 31, 781–786. [Google Scholar]
- Lussana, F.; Painter, R.C.; Ocke, M.C.; Buller, H.R.; Bossuyt, P.M.; Roseboom, T.J. Prenatal exposure to the Dutch famine is associated with a preference for fatty foods and a more atherogenic lipid profile. Am. J. Clin. Nutr. 2008, 88, 1648–1652. [Google Scholar] [CrossRef]
- Barua, S.; Junaid, M.A. Lifestyle, pregnancy and epigenetic effects. Epigenomics 2015, 7, 85–102. [Google Scholar] [CrossRef]
| Non-Exposed Group | Fetal Exposure Group | Early Childhood Exposure Group | Middle Childhood Exposure Group | Late Childhood Exposure Group | |
|---|---|---|---|---|---|
| Date of birth a | 1962–1964 | 1959–1961 | 1956–1958 | 1954–1956 | 1952–1954 |
| N | 2787 | 1656 | 2399 | 2496 | 2527 |
| Age (years), M (IQR) | 52.2 (1.0) | 55.3 (1.0) * | 58.2 (1.0) * | 60.2 (1.0) * | 62.1 (1.0) * |
| Male, n (%) | 1233 (44.2) | 714 (43.1) | 1073 (44.7) | 1126 (45.1) | 1160 (45.9) |
| Areas with severe famine, n (%) | 1705 (61.2) | 868 (52.4) * | 1376 (57.4) * | 1516 (60.7) | 1476 (58.4) * |
| South, n (%) | 1363 (48.9) | 775 (46.8) | 1268 (52.9) * | 1335 (53.5) * | 1393 (55.1) * |
| City, n (%) | 1141 (40.9) | 749 (45.2) * | 1048 (43.7) * | 1086 (43.5) | 1129 (44.7) * |
| BMI, n (%) | |||||
| <24 | 1148 (41.2) | 748 (45.2) * | 1068 (44.5) * | 1181 (47.3) * | 1158 (45.8) * |
| ≥24 | 1639 (58.8) | 908 (54.8) | 1331 (55.5) | 1315 (52.7) | 1369 (54.2) |
| Education level, n (%) | |||||
| Low | 1038 (37.2) | 634 (38.3) * | 1192 (49.7) * | 1403 (56.2) * | 1609 (63.7) * |
| Medium | 1107 (39.7) | 538 (32.5) | 662 (27.6) | 653 (26.2) | 609 (24.1) |
| High | 642 (23.0) | 484 (29.2) | 545 (22.7) | 440 (17.6) | 309 (12.2) |
| Income, n (%) | |||||
| Low | 462 (16.6) | 275 (16.6) | 415 (17.3) | 531 (21.3) * | 549 (21.7) * |
| Medium | 863 (31.0) | 504 (30.4) | 766 (31.9) | 796 (31.9) | 775 (30.7) |
| High | 689 (24.7) | 376 (22.7) | 560 (23.3) | 522 (20.9) | 533 (21.1) |
| Very high | 773 (27.7) | 501 (30.3) | 658 (27.4) | 647 (25.9) | 670 (26.5) |
| Smoking, n (%) | 785 (28.2) | 455 (27.5) | 665 (27.7) | 693 (27.8) | 672 (26.6) |
| Drinking, n (%) | 1087 (39.0) | 591 (35.7) * | 850 (35.4) * | 859 (34.4) * | 896 (35.5) * |
| Physically inactive, n (%) | 640 (23.0) | 403 (24.3) | 573 (23.9) | 596 (23.9) | 679 (26.9) * |
| Family history of hypertension, n (%) | 1052 (37.8) | 662 (40.0) | 876 (36.5) | 837 (33.5) * | 863 (34.2) * |
| Family history of diabetes, n (%) | 299 (10.7) | 218 (13.2) * | 242 (10.1) | 280 (11.2) | 236 (9.3) |
| Dietary pattern, n (%) | |||||
| Egg, milk and fruit pattern | 818 (29.4) | 574 (34.7) * | 739 (30.8) | 811 (32.5) * | 822 (32.5) * |
| Aquatic vegetable and meat pattern | 980 (35.2) | 507 (30.6) | 874 (36.4) | 779 (31.2) | 797 (31.5) |
| Staple food soybean and nut pattern | 989 (35.5) | 575 (34.7) | 786 (32.8) | 906 (36.3) | 908 (35.9) |
| Non-Exposed Group | Fetal Exposure Group | Early Childhood Exposure Group | Middle Childhood Exposure Group | Late Childhood Exposure Group | |
|---|---|---|---|---|---|
| Unadjusted | 1.00 (Ref.) | 1.08 (0.95–1.22) | 1.13 (1.01–1.26) * | 1.12 (1.00–1.25) * | 1.24 (1.12–1.39) * |
| Model I | 1.00 (Ref.) | 1.15 (0.95–1.38) | 1.27 (1.00–1.60) * | 1.24 (0.96–1.60) | 1.37 (1.03–1.83) * |
| Model II | 1.00 (Ref.) | 1.13 (0.94–1.37) | 1.35 (1.06–1.72) * | 1.33 (1.02–1.73) * | 1.49 (1.11–2.00) * |
| Model III | 1.00 (Ref.) | 1.23 (1.00–1.51) * | 1.44 (1.11–1.87) * | 1.50 (1.13–1.99) * | 1.67 (1.21–2.30) * |
| Stratification Factors | Non-Exposed Group | Fetal Exposure Group | Early Childhood Exposure Group | Middle Childhood Exposure Group | Late Childhood Exposure Group |
|---|---|---|---|---|---|
| Sex | |||||
| Male | 1.00 (Ref.) | 1.33 (0.96–1.84) | 1.42 (0.94–2.14) | 1.28 (0.81–2.00) | 1.35 (0.82–2.23) |
| Female | 1.00 (Ref.) | 1.21 (0.93–1.56) | 1.51 (1.08–2.12) * | 1.73 (1.20–2.49) * | 2.01 (1.33–3.04) * |
| BMI, kg/m² | |||||
| <24 | 1.00 (Ref.) | 1.02 (0.72–1.46) | 1.25 (0.80–1.96) | 1.13 (0.69–1.83) | 1.10 (0.64–1.89) |
| ≥24 | 1.00 (Ref.) | 1.38 (1.07–1.78) * | 1.59 (1.15–2.20) * | 1.79 (1.25–2.56) * | 2.17 (1.45–3.24) * |
| Famine severity | |||||
| Less severe | 1.00 (Ref.) | 1.14 (0.84–1.53) | 1.38 (0.94–2.02) | 1.48 (0.97–2.26) | 1.44 (0.89–2.33) |
| Serious | 1.00 (Ref.) | 1.34 (1.01–1.77) * | 1.54 (1.08–2.21) * | 1.56 (1.06–2.30) * | 1.91 (1.24–2.93) * |
| Residence location | |||||
| City | 1.00 (Ref.) | 1.38 (1.02–1.86) * | 1.71 (1.16–2.51) * | 1.80 (1.18–2.74) * | 2.04 (1.27–3.28) * |
| Countryside | 1.00 (Ref.) | 1.11 (0.84–1.47) | 1.25 (0.88–1.79) | 1.28 (0.87–1.88) | 1.40 (0.91–2.17) |
| Area of the country | |||||
| South | 1.00 (Ref.) | 1.32 (0.98–1.77) | 1.75 (1.20–2.57) * | 1.64 (1.08–2.48) * | 1.93 (1.22–3.07) * |
| North | 1.00 (Ref.) | 1.15 (0.87–1.52) | 1.20 (0.84–1.71) | 1.40 (0.94–2.07) | 1.48 (0.95–2.31) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yao, F.; Zhao, L.; Yang, Y.; Piao, W.; Fang, H.; Ju, L.; Guo, Q.; Yu, D. Association between Early Life Famine Exposure and Metabolic Syndrome in Adulthood. Nutrients 2022, 14, 2881. https://doi.org/10.3390/nu14142881
Yao F, Zhao L, Yang Y, Piao W, Fang H, Ju L, Guo Q, Yu D. Association between Early Life Famine Exposure and Metabolic Syndrome in Adulthood. Nutrients. 2022; 14(14):2881. https://doi.org/10.3390/nu14142881
Chicago/Turabian StyleYao, Fan, Liyun Zhao, Yuxiang Yang, Wei Piao, Hongyun Fang, Lahong Ju, Qiya Guo, and Dongmei Yu. 2022. "Association between Early Life Famine Exposure and Metabolic Syndrome in Adulthood" Nutrients 14, no. 14: 2881. https://doi.org/10.3390/nu14142881
APA StyleYao, F., Zhao, L., Yang, Y., Piao, W., Fang, H., Ju, L., Guo, Q., & Yu, D. (2022). Association between Early Life Famine Exposure and Metabolic Syndrome in Adulthood. Nutrients, 14(14), 2881. https://doi.org/10.3390/nu14142881






