Validation of 4 Estimating Methods to Evaluate 24-h Urinary Sodium Excretion: Summer and Winter Seasons for College Students in China
Abstract
:1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Data Collection
2.3. 24-h Urine Collection and Measurements
2.4. Estimation of 24-h Sodium Excretion from Spot Urine Samples
2.5. Statistical Analysis
3. Results
3.1. Basic Characteristics
3.2. The Variability of 24-h Urine Collection in Different Seasons
3.3. The Bias between Mean Measured and Predicted 24-h Urinary Sodium Excretions (from Group Levels)
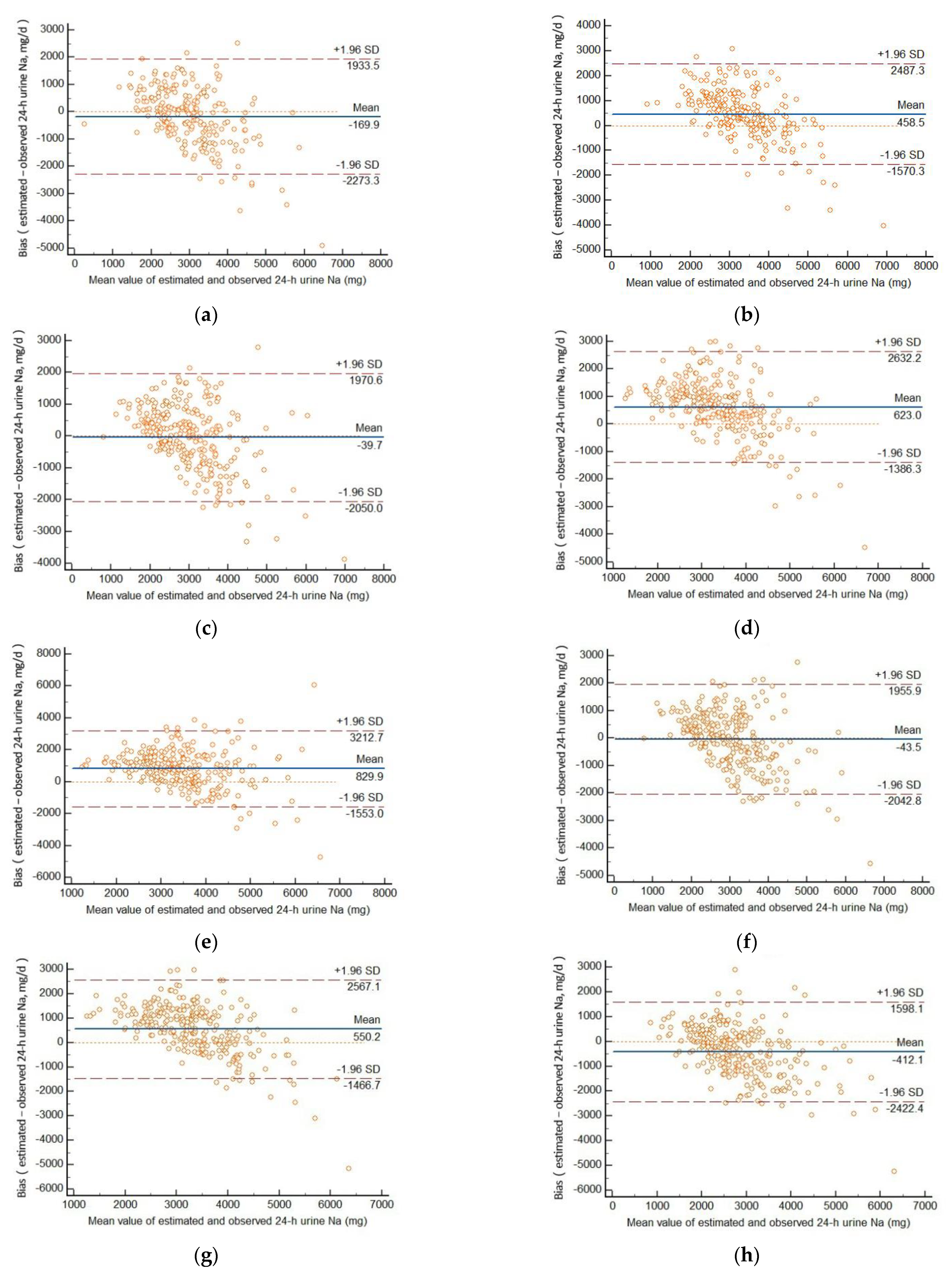
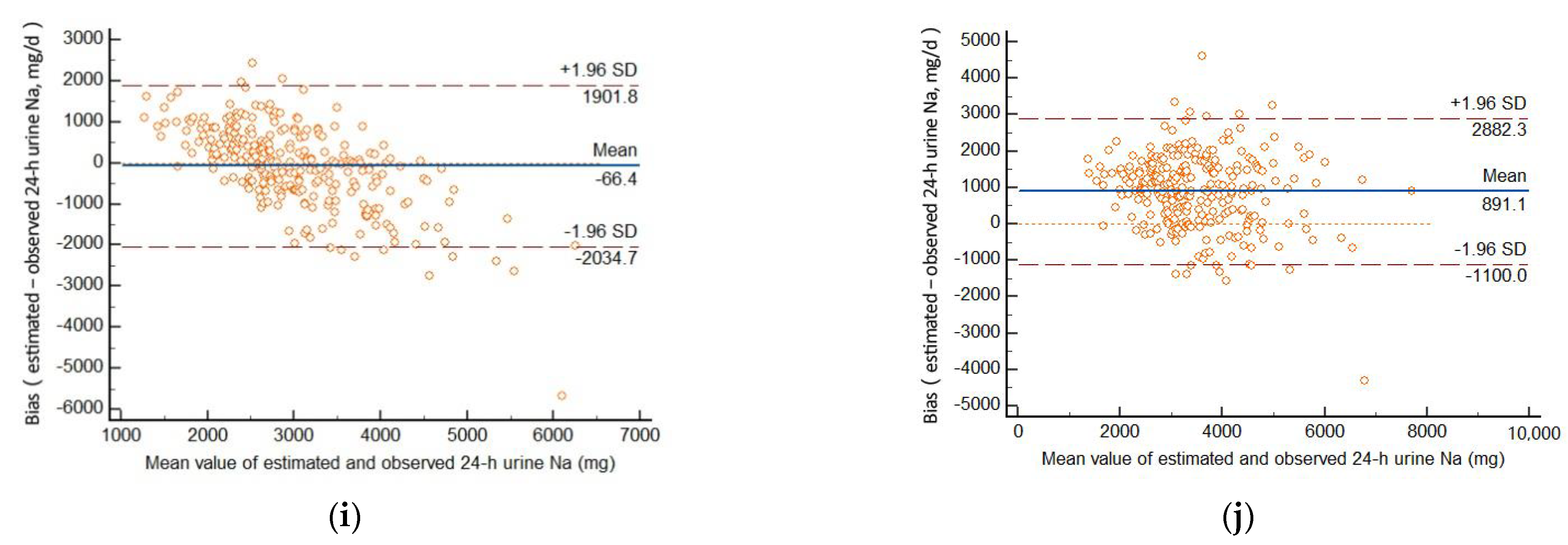
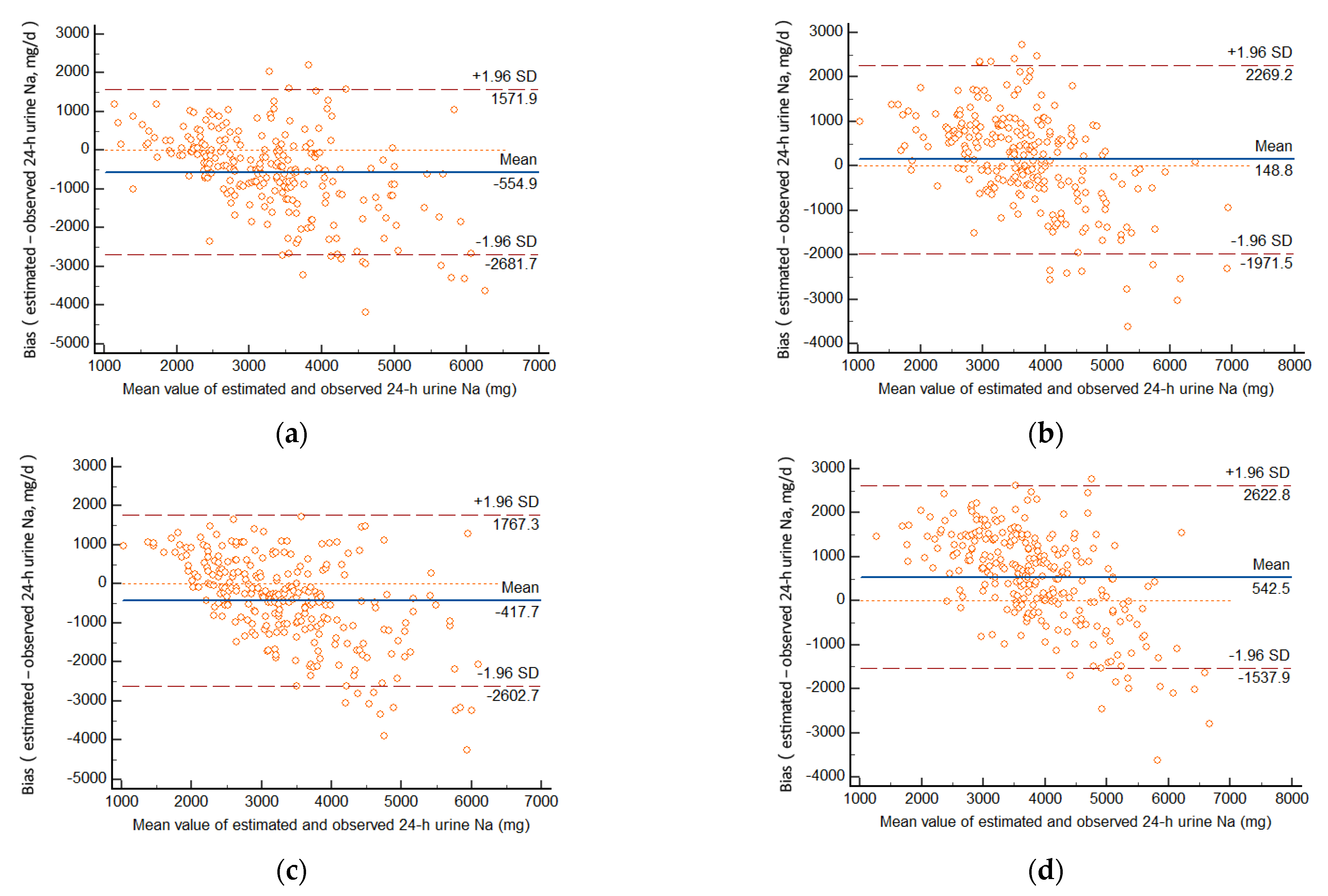
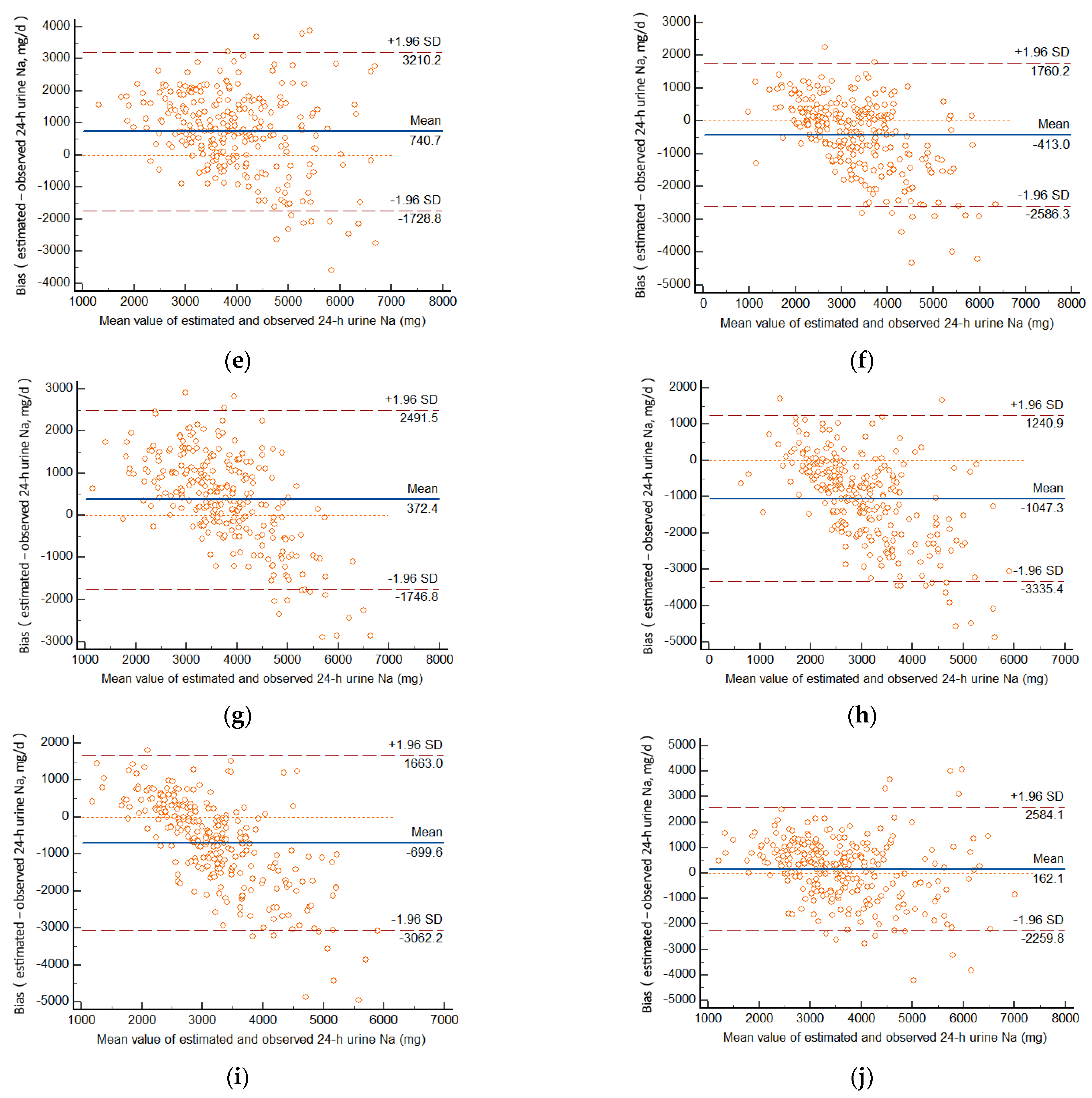
3.4. Relative Individual Differences in Predicted and Measured 24-h Urinary Sodium Excretion
3.5. Individual Correlations with Measured 24-h Urinary Sodium Excretion
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- He, F.J.; Macgregor, G.A. Reducing Population Salt Intake Worldwide: From Evidence to Implementation. Prog. Cardiovasc. Dis. 2010, 52, 363–382. [Google Scholar] [CrossRef] [PubMed]
- Myers, V.H.; Champagne, C.M. Nutritional effects on blood pressure. Curr. Opin. Lipidol. 2007, 18, 20–24. [Google Scholar] [CrossRef] [PubMed]
- Bibbins-Domingo, K.; Chertow, G.M.; Coxson, P.G.; Moran, A.; Lightwood, J.M.; Pletcher, M.J.; Goldman, L. Projected Effect of Dietary Salt Reductions on Future Cardiovascular Disease. N. Engl. J. Med. 2010, 362, 590–599. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- He, F.J.; MacGregor, G.A. A comprehensive review on salt and health and current experience of worldwide salt reduction programmes. J. Hum. Hypertens. 2009, 23, 363–384. [Google Scholar] [CrossRef] [PubMed]
- Joossens, J.V.; Hill, M.J.; Elliott, P.; Stamler, R.; Stamler, J.; Lesaffre, E.; Dyer, A.; Nichols, R.; Kesteloot, H. Dietary salt, nitrate and stomach cancer mortality in 24 countries. Int. J. Epidemiol. 1996, 25, 494–504. [Google Scholar] [CrossRef] [PubMed]
- Beaglehole, R.; Bonita, R.; Horton, R.; Adams, C.; Alleyne, G.; Asaria, P.; Baugh, V.; Bekedam, H.; Billo, N.; Casswell, S.; et al. Priority actions for the non-communicable disease crisis. Lancet 2011, 377, 1438–1447. [Google Scholar] [CrossRef]
- World Health Organization. Reducing Salt Intake in Populations: Report of a WHO Forum and Technical Meeting, 5–7 October 2006, Paris, France; World Health Organization: Geneva, Switzerland, 2007; pp. 109–116. [Google Scholar]
- World Health Organization. Guideline: Sodium Intake for Adults and Children; World Health Organization: Geneva, Switzerland, 2012. [Google Scholar]
- NHC. Report on Chinese Residents’ Chronic Disease and Nutrition 2020; People’ Medical Publishing House: Beijing, China, 2021; p. 100. [Google Scholar]
- GBD 2017 Diet Collaborators. Health effects of dietary risks in 195 countries, 1990–2017: A systematic analysis for the Global Burden of Disease Study 2017. Lancet 2019, 393, 1958–1972. [Google Scholar]
- He, Y.; Li, Y.; Yang, X.; Hemler, E.C.; Fang, Y.; Zhao, L.; Zhang, J.; Yang, Z.; Wang, Z.; He, L.; et al. The dietary transition and its association with cardiometabolic mortality among Chinese adults, 1982–2012: A cross-sectional population-based study. Lancet Diabetes Endocrinol. 2019, 7, 540–548. [Google Scholar] [CrossRef]
- Brown, I.J.; Tzoulaki, I.; Candeias, V.; Elliott, P. Salt intakes around the world: Implications for public health. Int. J. Epidemiol. 2009, 38, 791–813. [Google Scholar] [CrossRef] [Green Version]
- Institute of Medicine Committee on Strategies to Reduce Sodium Intake. The National Academies Collection: Reports funded by National Institutes of Health. In Strategies to Reduce Sodium Intake in the United States; Henney, J.E., Taylor, C.L., Boon, C.S., Eds.; National Academies Press: Washington, DC, USA, 2010; p. s10. [Google Scholar]
- World Health Organization. Strategies to monitor and evaluate population sodium consumption and sources of sodium in the diet: Report of a joint technical meeting convened by WHO and the Government of Canada. Psychosom. Med. 2011, 21, 218–227. [Google Scholar]
- Sasaki, S.; Yanagibori, R.; Amano, K. Validity of a self-administered diet history questionnaire for assessment of sodium and potassium: Comparison with single 24-hour urinary excretion. Jpn. Circ. J. 1998, 62, 431–435. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Staessen, J.; Broughton, P.M.; Fletcher, A.E.; Markowe, H.L.; Marmot, M.G.; Rose, G.; Semmence, A.; Shipley, M.J.; Bulpitt, C.J. The assessment of the relationship between blood pressure and sodium intake using whole-day, daytime and overnight urine collections. J. Hypertens. 1991, 9, 1035–1040. [Google Scholar] [CrossRef] [PubMed]
- Zhang, L.; Zhao, F.; Zhang, P.; Gao, J.; Liu, C.; He, F.J.; Lin, C.-P. A Pilot Study to Validate a Standardized One-Week Salt Estimation Method Evaluating Salt Intake and Its Sources for Family Members in China. Nutrients 2015, 7, 751–763. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Brown, I.J.; Dyer, A.R.; Chan, Q.; Cogswell, M.E.; Ueshima, H.; Stamler, J.; Elliott, P.; Grp, I.C.R. Estimating 24-Hour Urinary Sodium Excretion from Casual Urinary Sodium Concentrations in Western Populations. Am. J. Epidemiol. 2013, 177, 1180–1192. [Google Scholar] [CrossRef] [Green Version]
- Kawasaki, T.; Itoh, K.; Uezono, K.; Sasaki, H. A simple method for estimating 24-h urinary sodium and potassium excretion from 2nd morning voiding urine specimen in adults. Clin. Exp. Pharmacol. Physiol. 1993, 20, 7–14. [Google Scholar] [CrossRef]
- Tanaka, T.; Okamura, T.; Miura, K.; Kadowaki, T.; Ueshima, H.; Nakagawa, H.; Hashimoto, T. A simple method to estimate populational 24-h urinary sodium and potassium excretion using a casual urine specimen. J. Hum. Hypertens. 2002, 16, 97–103. [Google Scholar] [CrossRef] [Green Version]
- Han, W.; Sun, N.; Chen, Y.; Wang, H.; Xi, Y.; Ma, Z. Validation of the Spot Urine in Evaluating 24-Hour Sodium Excretion in Chinese Hypertension Patients. Am. J. Hypertens. 2015, 28, 1368–1375. [Google Scholar] [CrossRef] [Green Version]
- Wang, C.Y.; Cogswell, M.E.; Loria, C.M.; Chen, T.C.; Pfeiffer, C.M.; Swanson, C.A.; Caldwell, K.L.; Perrine, C.G.; Carriquiry, A.L.; Liu, K.; et al. Urinary excretion of sodium, potassium, and chloride, but not iodine, varies by timing of collection in a 24-hour calibration study. J. Nutr. 2013, 143, 1276–1282. [Google Scholar] [CrossRef] [Green Version]
- Mente, A.; O’Donnell, M.J.; Dagenais, G.; Wielgosz, A.; Lear, S.A.; McQueen, M.J.; Jiang, Y.; Xingyu, W.; Jian, B.; Calik, K.B.; et al. Validation and comparison of three formulae to estimate sodium and potassium excretion from a single morning fasting urine compared to 24-h measures in 11 countries. J. Hypertens. 2014, 32, 1005–1014, discussion 1015. [Google Scholar] [CrossRef]
- Xu, J.; Du, X.; Bai, Y.; Fang, L.; Liu, M.; Ji, N.; Zhong, J.; Yu, M.; Wu, J. Assessment and validation of spot urine in estimating the 24-h urinary sodium, potassium, and sodium/potassium ratio in Chinese adults. J. Hum. Hypertens. 2020, 34, 184–192. [Google Scholar] [CrossRef] [Green Version]
- Ma, W.; Yin, X.; Zhang, R.; Liu, F.; Yang, D.; Fan, Y.; Rong, J.; Tian, M.; Yu, Y. Validation and Assessment of Three Methods to Estimate 24-h Urinary Sodium Excretion from Spot Urine Samples in High-Risk Elder Patients of Stroke from the Rural Areas of Shaanxi Province. Int. J. Environ. Res. Public Health 2017, 14, 1211. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cogswell, M.E.; Wang, C.-Y.; Chen, T.-C.; Pfeiffer, C.M.; Elliott, P.; Gillespie, C.D.; Carriquiry, A.L.; Sempos, C.T.; Liu, K.; Perrine, C.G.; et al. Validity of predictive equations for 24-h urinary sodium excretion in adults aged 18–39 y. Am. J. Clin. Nutr. 2013, 98, 1502–1513. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dong, J.; Yan, Y.; Fan, H.; Zhao, X.; Mi, J. Accuracy Validation of 8 Equations to Estimate 24-Hour Sodium by Spot Urine in Young Adolescents. Am. J. Hypertens. 2019, 32, 257–264. [Google Scholar] [CrossRef]
- Xu, J.; Zhang, J.; Liu, M.; Bai, Y.; Wu, J. Estimating 24-Hour Sodium Excretion from Spot Urine Samples in Chinese Adults: Can Spot Urine Substitute 24-Hour Urine Samples? Nutrients 2020, 12, 798. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zhang, Y.; Peng, Y.; Li, K.; Peng, X. Assessing whether a spot urine specimen can predict 24-h urinary sodium excretion accurately: A validation study. J. Hypertens. 2019, 37, 99–108. [Google Scholar] [CrossRef] [PubMed]
| Total (n = 268) | Male (n = 138) | Female (n = 130) | |
|---|---|---|---|
| n (%) | 268 (100) | 138 (51.5) | 130 (48.5) |
| Age (year) | 19.9 ± 1.8 | 20.2 ± 1.9 | 19.5 ± 1.6 |
| Weight (kg) | 61.7 ± 13.4 | 68.9 ± 13.4 | 54.1 ± 8.4 |
| Height (cm) | 166.8 ± 8.7 | 172.8 ± 6.3 | 160.4 ± 5.9 |
| WC 1 (cm) | 73.3 ± 10.4 | 78.6 ± 10.3 | 67.7 ± 6.9 |
| BMI 2 (kg/m2) | 22.1 ± 3.7 | 23.1 ± 4.3 | 21.0 ± 2.7 |
| SBP 3 (mmHg) | 114.9 ± 14.0 | 123.3 ± 12.5 | 106.0 ± 9.1 |
| DBP 4 (mmHg) | 74.3 ± 8.1 | 77.0 ± 8.6 | 71.5 ± 6.6 |
| Heart rate (bpm) | 79.9 ± 12.9 | 78.7 ± 12.6 | 81.1 ± 13.2 |
| Summer | Winter | t | p | |
|---|---|---|---|---|
| Urinary volume (mL) | 1334.6 ± 654.5 | 1586.9 ± 655.1 | −6.124 | <0.001 |
| Sodium excretion (mg/d) | 3048.4 ± 1225.9 | 3564.7 ± 1369.6 | −5.696 | <0.001 |
| Potassium excretion (mg/d) | 1004.8 ± 364.2 | 1112.6 ± 357.6 | −3.934 | <0.001 |
| Creatinine excretion (mg/d) | 1285.1 ± 422.4 | 1294.6 ± 411.2 | −0.466 | 0.642 |
| Urinary Na/K (mg/mg) | 3.2 ± 1.3 | 3.4 ± 1.4 | −1.580 | 0.115 |
| Total (mg/d) | Male (mg/d) | Female (mg/d) | Predicted Value—Measured Value (95%CI) (mg/d) | r | p | Probability That Estimated Value Exists Within Mean ± 1.96 SD | |
|---|---|---|---|---|---|---|---|
| Measured 24-h sodium excretion | 3043.0 ± 1223.3 | 3372.5 ± 1304.4 | 2688.3 ± 1201.1 | Reference | — | — | Reference |
| Kawasaki | 3934.2 ± 1058.5 | 4278.3 ± 1112.6 | 3563.7 ± 858.0 | 891.1 (769.9, 1012.4) | 0.612 | <0.001 | 5.2% 14/268 |
| INTERSALT | |||||||
| Morning | 2934.9 ± 775.7 | 3387.0 ± 689.8 | 2535.3 ± 528.5 | −169.9 (−312.5, −27.3) | 0.537 | <0.001 | 5.1% 11/216 |
| Afternoon | 3025.7 ± 801.0 | 3940.5 ± 752.5 | 2535.3 ± 504.0 | −39.7 (−164.7, 85.3) | 0.557 | <0.001 | 4.7% 12/257 |
| Evening | 3016.7 ± 791.7 | 3462.0 ± 748.4 | 2547.4 ± 518.9 | −43.5 (−166.4, 79.5) | 0.559 | <0.001 | 4.9% 13/263 |
| Overnight | 2630.9 ± 771.4 | 2983.0 ± 824.6 | 2251.8 ± 478.3 | −412.1 (−534.6, −289.7) | 0.551 | <0.001 | 4.5% 12/268 |
| Tanaka | |||||||
| Morning | 3563.4 ± 712.2 | 3678.6 ± 689.6 | 3441.7 ± 718.6 | 458.5 (321.0, 596.0) | 0.577 | <0.001 | 4.6% 10/216 |
| Afternoon | 3688.4 ± 739.1 | 3720.4 ± 722.5 | 3654.6 ± 757.5 | 623.0 (498.0, 747.9) | 0.552 | <0.001 | 5.8% 15/257 |
| Evening | 3610.3 ± 676.6 | 3682.4 ± 685.7 | 3534.3 ± 660.9 | 550.2 (426.2, 674.2) | 0.541 | <0.001 | 4.9% 13/263 |
| Overnight | 2976.6 ± 626.8 | 3038.6 ± 653.7 | 2909.8 ± 591.9 | −66.4 (−186.3, 53.4) | 0.574 | <0.001 | 4.1% 11/268 |
| Sun’s | 3895.3 ± 966.5 | 3768.7 ± 938.6 | 4028.8 ± 981.2 | 829.9 (681.7, 978.0) | 0.406 | <0.001 | 4.7% 12/257 |
| Total (mg/d) | Male (mg/d) | Female (mg/d) | Predicted Value—Measured Value (95%CI) (mg/d) | r | p | Probability that Estimated Value Exists Within Mean ± 1.96 SD | |
|---|---|---|---|---|---|---|---|
| Measured 24-h sodium excretion | 3563.7 ± 1370.0 | 4034.0 ± 1354.6 | 3062.3 ± 1190.6 | Reference | — | — | Reference |
| Kawasaki | 3726.3 ± 1086.9 | 4160.9 ± 1141.6 | 3265.1 ± 803.0 | 162.1 (13.5, 310.7) | 0.515 | <0.001 | 4.5% 12/268 |
| INTERSALT | |||||||
| Morning | 3084.7 ± 863.2 | 3591.6 ± 788.6 | 2519.1 ± 546.7 | −554.9 (−693.2, −416.6) | 0.597 | <0.001 | 5.0% 12/239 |
| Afternoon | 3144.3 ± 808.3 | 3583.6 ± 775.1 | 2678.1 ± 537.4 | −417.7 (−551.7, −283.6) | 0.581 | <0.001 | 4.1% 11/268 |
| Evening | 3149.2 ± 831.0 | 3665.0 ± 689.0 | 2601.8 ± 0570.3 | −413.0 (−546.4, −279.7) | 0.587 | <0.001 | 4.1% 11/268 |
| Overnight | 2515.9 ± 755.1 | 2673.7 ± 854.3 | 2340.2 ± 595.8 | −1047.3 (−1187.7, −906.9) | 0.524 | <0.001 | 4.5% 12/268 |
| Tanaka | |||||||
| Morning | 3753.1 ± 830.3 | 4011.4 ± 816.6 | 3501.2 ± 766.5 | 148.8 (11.0, 286.7) | 0.599 | <0.001 | 6.3% 15/239 |
| Afternoon | 4105.8 ± 782.6 | 4196.7 ± 751.2 | 4009.3 ± 806.2 | 542.5 (414.8, 670.1) | 0.635 | <0.001 | 4.5% 12/268 |
| Evening | 3939.7 ± 745.1 | 4016.9 ± 663.3 | 3857.8 ± 817.8 | 372.4 (242.3, 502.4) | 0.618 | <0.001 | 5.2% 14/268 |
| Overnight | 2864.8 ± 610.0 | 2901.8 ± 661.1 | 2825.8 ± 557.1 | −699.6 (−844.6, −554.6) | 0.476 | <0.001 | 3.4% 9/268 |
| Sun’s | 4309.1 ± 1026.0 | 4229.3 ± 934.1 | 4364.0 ± 1105.1 | 740.7 (589.2, 892.2) | 0.476 | <0.001 | 4.9% 13/268 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gong, W.; Ma, Y.; Zhang, Z.; Liang, J.; Zhang, J.; Ding, G. Validation of 4 Estimating Methods to Evaluate 24-h Urinary Sodium Excretion: Summer and Winter Seasons for College Students in China. Nutrients 2022, 14, 2736. https://doi.org/10.3390/nu14132736
Gong W, Ma Y, Zhang Z, Liang J, Zhang J, Ding G. Validation of 4 Estimating Methods to Evaluate 24-h Urinary Sodium Excretion: Summer and Winter Seasons for College Students in China. Nutrients. 2022; 14(13):2736. https://doi.org/10.3390/nu14132736
Chicago/Turabian StyleGong, Weiyi, Yuxia Ma, Zechen Zhang, Jufeng Liang, Jiguo Zhang, and Gangqiang Ding. 2022. "Validation of 4 Estimating Methods to Evaluate 24-h Urinary Sodium Excretion: Summer and Winter Seasons for College Students in China" Nutrients 14, no. 13: 2736. https://doi.org/10.3390/nu14132736
APA StyleGong, W., Ma, Y., Zhang, Z., Liang, J., Zhang, J., & Ding, G. (2022). Validation of 4 Estimating Methods to Evaluate 24-h Urinary Sodium Excretion: Summer and Winter Seasons for College Students in China. Nutrients, 14(13), 2736. https://doi.org/10.3390/nu14132736






