Abstract
Background: COVID-19 has taken on pandemic proportions with growing interest in prognostic factors. Overhydration is a risk factor for mortality in several medical conditions with its role in COVID-19, assessed with bioelectrical impedance (BI), gaining research interest. COVID-19 affects hydration status. The aim was to determine the hydration predictive role on 90 d survival COVID-19 and to compare BI assessments with traditional measures of hydration. Methods: We studied 127 consecutive COVID-19 patients. Hydration status was estimated using a 50 kHz phase-sensitive BI and estimated, compared with clinical scores and laboratory markers to predict mortality. Results: Non-surviving COVID-19 patients had significantly higher hydration 85.2% (76.9–89.3) vs. 73.7% (73.2–82.1) and extracellular water/total body water (ECW/TBW) 0.67 (0.59–0.75) vs. 0.54 (0.48–0.61) (p = 0.001, respectively), compared to surviving. Patients in the highest hydration tertile had increased mortality (p = 0.012), Intensive Care Unit (ICU) admission (p = 0.027), COVID-19 SEIMC score (p = 0.003), and inflammation biomarkers [CRP/prealbumin (p = 0.011)]. Multivariate analysis revealed that hydration status was associated with increased mortality. HR was 2.967 (95%CI, 1.459–6.032, p < 0.001) for hydration and 2.528 (95%CI, 1.664–3.843, p < 0.001) for ECW/TBW, which were significantly greater than traditional measures: CRP/prealbumin 3.057(95%CI, 0.906–10.308, p = 0.072) or BUN/creatinine 1.861 (95%CI, 1.375–2.520, p < 0.001). Hydration > 76.15% or ECW/TBW > 0.58 were the cut-off values predicting COVID-19 mortality with 81.3% and 93.8% sensitivity and 64 and 67.6% specificity, respectively. Hydration status offers a sensitive and specific prognostic test at admission, compared to established poor prognosis parameters. Conclusions and Relevance: Overhydration, indicated as high hydration (>76.15%) and ECW/TBW (>0.58), were significant predictors of COVID-19 mortality. These findings suggest that hydration evaluation with 50 kHz phase-sensitive BI measurements should be routinely included in the clinical assessment of COVID-19 patients at hospital admission, to identify increased mortality risk patients and assist medical care.
1. Introduction
The coronavirus disease 2019 (COVID-19) has high human transmission and considerable mortality rate []. Thus, clinicians actively seek to identify physiological factors associated with increased risk of non-survival.
Researchers continue to identify prognostic factors for morbidity and mortality of SARS-CoV-2 []. Whereas investigations have been focusing on blood biochemical, pre-existing diseases or comorbidities, drug treatments, and basic clinical variables (O2 saturation, temperature, or heart rate), observational reports identify excess fluid accumulation, acral and pulmonary edema in SARS-CoV-2 patients [,]. Emerging evidence identifies bioelectrical impedance (BI) derived hydration status, notable overhydration at admission, as a significant predictor of non-survival in these patients [,]. Overhydration refers to an imbalance in fluid distribution between extracellular water (ECW), and intracellular water (ICW) volumes with the expansion of ECW associated with systemic inflammation and aggressive fluid administration []. Overhydration is a risk factor for mortality in several medical conditions, such as critical illness, heart, and kidney failure, and a significant mortality predictor (OR 4.38; 95%CI, 2.76–6.94) [].
The accurate, rapid bedside hydration assessment in hospitalized patients is a challenge, since available methods are impractical and costly for point-of-care application, have limited precision for an individual, and lack individual-specific normal values []. Physical characteristics such as body weight, blood pressure, central venous pressure, presence/absence of edema, and laboratory analysis are non-specific to provide a reliable estimate of hydration for an individual patient. However, in COVID-19 patients, the validity of these methods is limited by disease characteristics and compliance with the rules for controlling the spread of infection [].
Real-time assessment of hydration status alternatively utilizes bioelectrical impedance estimates and classification with bioelectrical impedance vector analysis (BIVA) measurements [,]. This method is bodyweight independent and relies on sample-specific multiple regression models to classify fluid volumes and distribution for an individual. The BI method relies on the conduction of an applied alternating current by water and electrolytes, and delay of the current by cell membranes and tissue interfaces to derive measurements of resistance (R), which is associated with total body water (TBW) volume, and series reactance (Xc), an index of body cell mass (BCM) relative density [,,]. The geometric relationships of R and Xc demonstrate that the impedance (Z) vector (Z2 = R2 + Xc2) is inversely related to TBW [], and the phase angle (PhA) [PhA = arc tan (Xc/R)•(Π•360°)] is inversely related to tracer dilution measurements of ECW/ICW [] and cumulative fluid balance in critical patients [].
This study aimed to determine whether hydration measurements derived using BI measurements and BIVA, hydration percentage, and ECW/TBW ratio, could predict mortality in a cohort of patients with COVID-19. This study incorporates global clinical scales [COVID-19 Spanish Society of Infectious Diseases and Clinical Microbiology (SEIMC) Score] [] and other laboratory prognostic markers of inflammation and venous congestion [,]. It also compared the predictive value of BI-derived parameters with clinical biochemical indicators of hydration as mortality risk indicators in hospitalized COVID-19 patients.
2. Materials and Methods
2.1. Setting Study
In this single-center, longitudinal cohort study, we enrolled a sample of patients admitted consecutively to a hospital area care for COVID-19 in Infectious Disease Unit, in Virgen Victoria Hospital (Malaga, Spain), measured between 6–17 April 2020 followed by 90 d outcomes. All patients were diagnosed with COVID-19 pneumonia according to World Health Organization interim guidance [] using real-time reverse transcriptase-polymerase chain reaction assays. This study was approved by the Ethics Committee of Virgen Victoria “PhA_COVID-19-201023” (Institutional human review board).
2.2. Measurements
We measured the hydration status of the patients within 72 h after hospital admission. BI measurements were obtained with a 50 kHz, phase-sensitive impedance analyzer (BIA101 Bioimpedance Vector Analyzer (AKERN, Pontassieve, Italy) that introduces 800 μA using the standard tetrapolar supine technique [,].
BIVA was performed [] using the RXc graph to classify hydration status and body soft tissue mass. Resistance is inversely related to fluid content, indirectly reflecting soft tissue mass. The Bioimpedance Analysis (BIA) technique has high technical accurately (R = +/−1%, Xc = +/−2%) daily controlled by a test circuit yielding R = 383 Ω and Xc = 45 Ω, with a low technical error of measurement (0.07–0.30%) and a biological variation of measurement (1.9%) for repeated measurements in healthy adults [,].
The BIA instrument uses Hydragram® software to provide an interpretative evaluation of dehydration or overhydration. The individual fat-free mass (FFM) hydration factor (TBW/FFM, %) is given as a numerical reference. Thus, changes in fluid balance can be recognized fast and reliably, assisting therapy follow-up, as body water volume changes are turned into an easy-to-understand hydration scale. Hydration state [] is expressed as the individual hydration in percentage. Euhydration is described as 72.7–74.3% with overhydration exceeding 74.3% + 1 SD of euhydration and dehydration being less than 72.7% − 1 SD as derived by Moore and others [,].
Biagram® illustrates the distribution of phase-sensitive 50 kHz BI direct measurements of Xc and PhA from the phase-sensitive BI analyzer for an individual []. The measurements are height and weight independent evaluation methods to detect the extracellular/intracellular space proportion in clinical practice. Individual points in different regions of the reference Biagram® graph have specific interpretations of fluids distribution spaces. Points below the lower line of nomogram are related principally to extracellular conductive pathway due to ECW expansion and/or contraction of capacitive membranes, points above the upper line are associated predominantly with alterations of ICW mainly due to dehydration, and points between the lines generally indicate normal extracellular/Intracellular (E/I) proportion [].
Hydration status is described also as the ECW/TBW ratio adjusted by age and gender []. For Male: . For female: . In a healthy state, ECW/TBW ratio should fall within the range 0.360–0.390 [].
Bodyweight and standing height were determined at admission and before BI measurement; weight measurements were with a scale (100 g sensitivity); while height measurements were measured with a 2 mm sensitivity laser height rod. A standardized quality assurance protocol was used by trained healthcare professionals to reduce measurement variability. All BI measurements were obtained with the patient supine on a standard hospital bed, at least five to ten minutes in a supine position before registering BI values, in order to achieve an even fluid distribution from standing to recumbency. This is a well-known phenomenon affecting R and Xc values. Final R and Xc acceptance, only after substantial stabilization of BIA measurement values, is ±2 Ω for R and ±1 Ω for Xc.
2.3. Clinical and Analytical Variables
We determined the following clinical assessments: age, sex, any comorbidities, (e.g., history of diabetes, hypertension, dyslipidemia, obesity, heart disease, pulmonary disease, or kidney failure), signs or symptoms such as dyspnoea, low age-adjusted capillary oxygen saturation (SaO2) on room air and COVID-19 SEIMC score for each patient [], and laboratory tests, including white cell count (SysmexXN-10), neutrophil-to-lymphocyte ratio, creatinine (mg/dL), urea (mg/dL), Na (mEq/L), pre-albumin (mg/dL) (Atellica-Siemens, Erlangen, Germany), C-reactive protein (CRP, mg/L) (Dimension EXL200S), blood urea nitrogen (BUN) , BUN/creatinine ratio (an emerging marker of venous congestion and poor prognosis, whose median population value is 15.0[IQR]:12.9–17.6) [] and CRP/pre-albumin ratio (new inflammatory index and a potential predictor of complications) [].
2.4. Sample Size Calculation
We tested the hypothesis that BI-derived overhydration status indicators were independent predictors of 90 d mortality in a multivariate model. We calculated the sample size using the findings of Basso et al. [], where the effect of overhydration on the mortality showed an OR of 2.64 in critical care patients with a mortality rate of 31.6% in the overhydration compared to the normal hydration status (21.1%) group. Thus, with an alpha error of 0.05, a power of 80%, and a loss rate of 10%, a minimum of 89 patients were needed to attain sufficient power. To account for anticipated mortality, we aimed to recruit 120 patients.
2.5. Statistical Analysis
Statistical analyses of the data were primarily performed using the SPSS program (version 22.0.0 Windows, SPSS-Iberica, Spain). We used descriptive statistics to characterize our cohort of patients. Baseline characteristics were expressed as median and interquartile range (IQR) for continuous variables and as proportions for categorical variables. Furthermore, we categorized hydration percentage into tertiles (T) as T1 [lower 33rd percentiles of hydration status (<73.5%)], T2 [33rd–66th percentiles of hydration status (73.6–79%)], T3 [more than 66th percentile of hydration status (≥79.1%)]. We compared our hydration percentage tertiles with either the ANOVA test or Friedman test according to their distribution. Continuous variables were compared with Student’s t-test or Mann–Whitney U test according to their distribution. Categorical variables were compared with the chi-squared (or Fisher’s exact test). We also analyzed the relationship using Pearson or Spearman correlations models according to normal distribution.
In multivariate analysis, Cox proportional hazards regression was used to assess the relationship between hydration parameters and mortality in COVID-19 patients. Hazard ratio (HR) and their 95% confidence intervals (CI) were calculated. We used three models to analyze hydration status. In the first model, we analyzed hydration percentage (TBW/FFM, %), in the second one we analyzed ECW/TBW, and in the third one we analyzed TBW/weight. HR for death was expressed per 10% increase in hydration percentage, and 0.1 increase in ECW/TBW or TBW/Weight. To prevent potential confounding factors, the results were adjusted for several covariates that were known as potential risk or protective factors for mortality: age (y, continuous); sex (male–female); BMI (kg/m2, continuous); history of diabetes mellitus (absence–diagnosis); high blood pressure (absence–diagnosis); dyslipidaemia (absence–diagnosis); heart disease (absence–diagnosis), kidney failure (absence–diagnosis). We constructed three adjusted models: Model 1: adjusted for sex, age, and BMI. Model 2: additionally adjusted for the previous diagnosis of type 2 diabetes mellitus (T2DM), high blood pressure, dyslipidaemia, heart disease, or kidney failure. Model 3: additionally adjusted for body cell mass index (BCMI). Model 4: additionally adjusted for CRP level. Model 5: additionally adjusted for BUN/creatinine. Statistical significance was set at p < 0.05. Therefore, regarding the relationship between COVID-19 mortality and BI-derived hydration we analyzed multivariate logistic regression model where the response variable was mortality and predictor variables were hydration percentage > 76.15% and ECW/TBW > 0.58. The model then was modified with other factors: age (y, continuous), sex (male–female), BMI (kg/m2, continuous).
We also analyzed the multivariate logistic regression model, where the response variable was mortality and predictor variables were hydration percentage > 76.15% and ECW/TBW > 0.58.
The Kaplan–Meier product-limit estimator at 90 d was used to calculate the cumulative probability of death, estimate survival, and evaluate the difference among the hydration tertiles. The Kaplan–Meier survival curves were compared using log-rank Mantel–Cox) test. The time of origin was the admission day. The event was defined as death and all cases were censored at their last observation. Differences were considered statistically significant with a p-value < 0.05.
Evaluation of the diagnostic performance of individual hydration parameters was based on the receiver operating characteristic (ROC) curve and the area under the curve (AUC). We estimated the accuracy of hydration percentage using AUC by constructing a plot of sensitivity versus 1-specifity. ROC curves were used to determine the optimal cut-off values. These optimal cut-off points for each hydration measurement (ECW/TBW) and prognostic markers (CRP/pre-albumin, BUN/creatinine, COVID-19 SEIMC score) were determined by the point of convergence for greatest sensitivity and specificity by Youden index.
We computed the positive-negative predictive values (PPV-NPV) on Biagram® observing the individual point distribution discriminated by the lower line, using Bayes’ theorem: and .
3. Results
3.1. Global Results
A total of 127 patients were admitted to the area of hospital care for COVID-19 and enrolled in the present study. COVID-19 study participants were predominantly males (59.1%), and their median (IQR) age was 69-y (59–80). Among the patients, 18.1% required additional intensive care in the Intensive Care Unit (ICU). The median length of hospital stay was 15 d (12–27) for the general ward, and 47 d (25–60, p < 0.001) for ICU patients. After 90 d, 111 patients (87.4%) had been discharged alive and 16 (12.6%) had died.
Table 1 shows the hydration parameters, COVID-19 SEIMC score, and biochemical measurements of the COVID-19 admitted patients.

Table 1.
Physical characteristics and biochemical measurements of COVID-19 patients related to survival and mortality.
Patients who did not survive showed a clinical score of greater severity [18.5 points (12.8–21.5) vs. 6 points (4–13), p < 0.001]. Non-survivor patients showed 8.3% high and 91.7% very high category, while survivor patients showed 7.9% low risk, 32.7% moderate risk, 18.8% high risk, and 40.6% very high-risk category of COVID-19 SEIMC score.
Comparing survivors and non-survivor patients, laboratory test also showed a greater BUN/creatinine [31.7 (25.3–43.3) vs. 22.8 (17.4–30.1), p < 0.001] as a marker of venous congestion and CRP/pre-albumin [1.19 (0.24–3.22) vs. 0.09 (0.02–0.31), p = 0.002] indicative of increased inflammatory status.
3.2. Hydration Status and 90 d Mortality
Hydration status distributions of COVID-19 patients based on BI-derived hydration percentage (TBW/FFM, %) showed a 48.8% euhydrated, while up to 43.3% classified with overhydration and 7.9% dehydration patients. In non-survivor patients, severe overhydration was associated with 37.5%, moderate overhydration with 18.8%, and mild overhydration with 25% (Figure 1A).
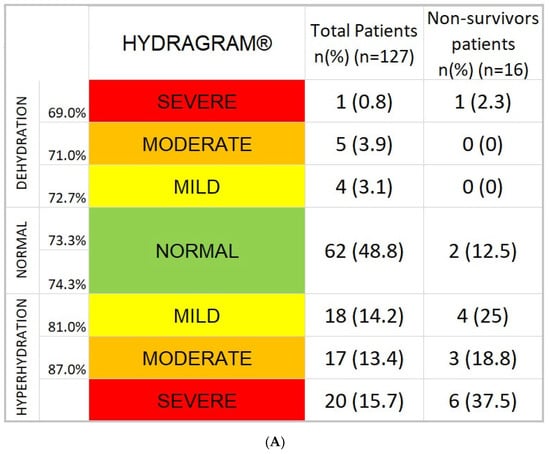
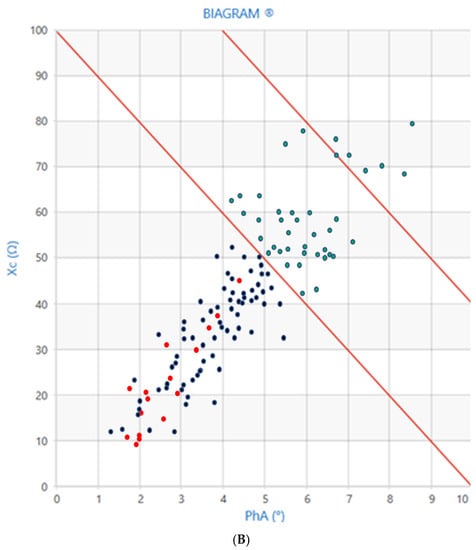
Figure 1.
(A) Hydragram® graph of COVID-19 disease (n = 127). Hydration status distribution of COVID-19 admitted patients showed a situation of hyperhydration associated with COVID-19 (43.3%). (B) Biagram® graph of COVID-19 disease (n = 127): distribution of COVID-19 admitted patients. All casualties are marked with red dots. Blue dots below lower line are false positive, blue dots above lower line true negative. The position of the points is related to the E/I status of the patient based on raw measurements of reactance and phase angle. Points below the lower line are associated with states of expansion of extracellular space greater than intracellular (severe inflammatory process), between the line points are normal E/I and above the upper line extracellular is smaller than intracellular space. The entire cluster of red dots is positioned below the lower discriminating line showing above the line a 100% NPV (negative = survivors) area.
The distribution of individual hydration assessment data points of the COVID-19 patients showed a pattern of broad distribution in areas from dehydration to severe overhydration in the Biagram® nomogram (Figure 1B). Patients who died are grouped in the lower-left region of the graph, consistent with states of overhydration. Biagram® yields 100% NPV or 100% no mortality for subjects placed above the lower line (Figure 1B). Non-survivors had a significantly higher percentage of hydration compared to survivors [85.2% (76.9–89.3) vs. 73.7% (73.2–82.1), p = 0.001] and ECW/TBW [0.67 (0.50–0.75) vs. 0.54 (0.48–0.61), p < 0.001], while TBW adjusted for height (p = 0.429) or weight (p = 0.085) was not different between the groups of patients (Figure 1, Table 1).
Stratification of hydration values reveals greater mortality in the highest percentage hydration tertile (T3 vs. T1; 23.8 vs. 2.4%, p = 0.012) and increased need for ICU admission (T3 vs. T1, 31 vs. 9.5%, p = 0.027). The highest hydration tertile also had significantly increased CRP, CRP/pre-albumin, and more elevated sodium plasma levels, without differences in creatinine, glomerular filtration, or BUN/creatinine. The COVID-19 SEIMC score in the very high-risk category is related to higher hydration status of 62.5% vs. 20.0% (T3 and T1 of hydration percentage) (Table 2).

Table 2.
Characteristics of COVID-19 patients according to tertiles of hydration status (percentage TBW/FFM).
The Kaplan–Meier plot was constructed using tertiles of the hydration distribution. Kaplan–Meier product-limit estimator showed that higher hydration percentage (T3) was significantly linked with higher mortality rates (log-rank test, p = 0.010) (Figure 2). Median of survival time was 79.2 d (68.8–89.6) in T3 (hydration percentage ≥ 79.1%), 89.4 d (82.3–96.5) for T2 (hydration percentage: 73.6–79%) and 95.7 d (93.3–98.2) for T1 tertile (hydration percentage ≤ 73.5%).
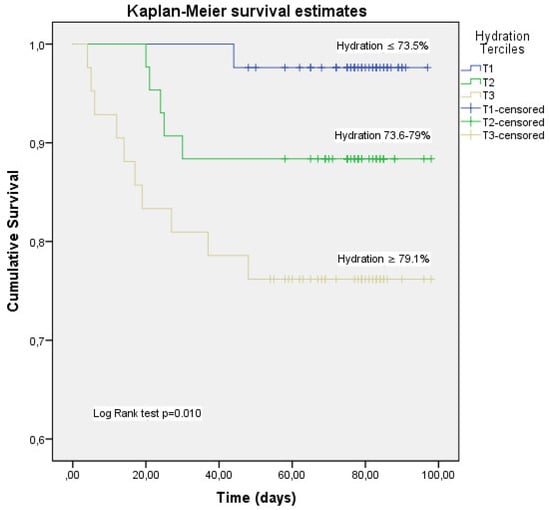
Figure 2.
Kaplan–Meier analysis for the cumulative percentage of surviving patients at 90 days according to hydration percentage tertiles. The 33rd and 66th percentiles of hydration percentage were used as the cut-off point to divide the patients with acute COVID-19 disease into 3 groups (T1, T2, T3) and made the Kaplan–Meier plot. Kaplan–Meier product-limit estimator shower that higher hydration (T3) was significantly linked with higher mortality rates (log-rank test, p = 0.010). Mortality was mainly concentrated in T3.
3.3. Optimal Hydration Parameters Cut-Off Value and 90 d Mortality Prediction in COVID-19 Disease
Using ROC curves, we determined the hydration status measurement cut-off points for predicting mortality. A 76.15% hydration percentage value was the most sensitive (81.3%) and specific (64%) factor, with an AUC was 0.746, for mortality risk prognosis in acute COVID-19. For ECW/TBW, AUC was 0.841, and the 0.58 value was the most sensitive (93.8%) and specific (67.6%) factor for mortality risk prognostic in acute SARS-CoV-2 infection. We compared these data with the cut-off points of mortality prediction using ROC curves for the analytical parameters established as prognostic factors (Figure 3).
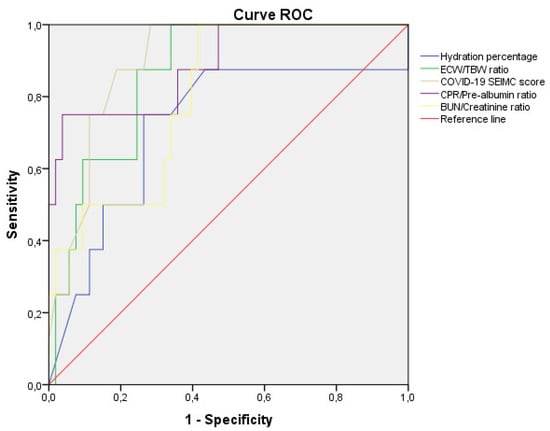
Figure 3.
Comparative analysis of ROC curve of hydration with established prognosis factor in COVID-19 patients. Comparative analysis of the receiver operating characteristic curves of hydration percentage, ECW/TBW ratio, COVID-19 SEIMC clinical score, and analytical indicators (CRP/pre-albumin, BUN/creatinine) for prediction of mortality in patients with COVID-19 (n = 127).
COVID19 SEIMC score greater than 10.5 points, CRP/pre-albumin greater than 0.88, and BUN/creatinine greater than 23.98 were also the cut-off points for predicting mortality in COVID-19 patients. ECW/TBW showed the highest sensitivity concerning the rest of the parameters in predicting mortality at 90 d, while CRP/pre-albumin was the highest specificity (Table 3).

Table 3.
Analysis of the prognostic factors of mortality in COVID-19.
Hydration percentage and ECW/TBW showed a positive correlation with COVID-19 clinical score (r = 0.394, p < 0.001 and r = 0.541, p < 0.001, respectively), CRP (r = 0.220, p = 0.013 and r = 0.283, p = 0.001, respectively), CRP/pre-albumin (r = 0.263, p = 0.026 and r = 0.379, p = 0.001, respectively) and BUN/creatinine (r = 0.218, p = 0.015 and r = 0.281, p = 0.001, respectively). ECW/TBW also showed a positive correlation with hospital stay in survivors of COVID-19 (r = 0.310, p = 0.001).
In the assessment of hydration status to predict mortality in COVID-19 patients, we performed multivariate logistic regression models with mortality as a response variable: in the first model, we evaluated the association between mortality and the presence of overhydration percentage ≥76.15% [OR 7.692; 95%CI (2.067–28.616); p = 0.002] and the second model the predictor variable tested was ECW/TBW ≥ 0.58 [OR 30.000; 95%CI (3.815–235.933); p = 0.001]. We found a significant association with mortality in both models of overhydration, which is maintained even after adjusting for confounding variables such as age, sex, and BMI, [OR 5.804; 95%CI (1.460–23.071); p = 0.013] and [OR 18.237; 95%CI (2.196–151.457); p = 0.007], respectively.
We used an 11-component model multivariate analysis (by Cox regression) to evaluate the utility of the hydration status measurements as prognostic indicators of mortality in COVID-19. We found that an increased hydration percentage value was significantly associated with a higher mortality hazards ratio [HR 2.967; 95%CI (1.459–6.032), p = 0.003). This trend was also maintained in the adjusted models by the confounding variables (Table 4).

Table 4.
Multivariate Cox regression for hydration status as predictors of mortality in COVID-19 patients.
Likewise, the ECW/TBW [HR 2.528; 95%CI (1.664–3.843), p < 0.001] was also associated with an increase in mortality HR of the crude model, with this relationship maintained in the adjusted models. These results are significantly greater than traditional clinical measures of fluid overload such as CRP/prealbumin [HR 3.057; 95% CI (0.906–10.308), p = 0.072) or BUN/creatinine [HR 1.861; 95% CI (1.375–2.520), p < 0.001)].
4. Discussion
Overhydration is a clinical finding among COVID-19 patients. Reports indicate that patients with acute respiratory distress syndrome (ARDS), to which COVID-19 frequently progresses, develop excessive fluid accumulation. Cumulative net fluid balance was significantly greater among non-survivors, compared to survivors, of ARDS during a 30 d period []. COVID-19 patients also can present with acral [] and pulmonary edema []. These observations stimulated research interest in hydration as a prognostic factor for morbidity and mortality in COVID-19.
The main finding of this study was a positive association between overhydration, assessed by BIVA, and mortality in COVID-19 patients, determining that BI-derived hydration parameters were significant 90- mortality predictors. In the Kaplan–Meyer plot of the survival curve, a hydration percentage of >79.1% (highest hydration tertile, T3) grouped most deceased patients, as a significant mortality predictor. Importantly, the present findings provide the first evidence that BIVA-related estimates of fluid overload were significantly better predictors than standard biochemical indicators of overhydration and other clinical scores. Thus, to our knowledge, this is the first report of the deleterious relationship between hydration status, COVID-19, and mortality.
Beyond these data, the survival analysis revealed an increase in hydration percentage, and ECW/TBW have more prognostic value than overhydration indicators associated with inflammation (CRP/prealbumin) or vascular overload (BUN/creatinine).
There are two fundamental lines in the pathogenesis of increased hydration, the inflammatory component of the disease and primary fluid retention due to cardiac or renal hemodynamic failure.
In more than a third of the patients in our sample, the mean hydration of FFM percentage was estimated to be 86.6% (84.1–90) and ECW/TBW was 0.67(0.61–0.74), showing a severe situation of inflammation/fluid retention associated with SARS-CoV-2 infection. In critical patients, the global effect of overhydration on mortality revealed its negative effect with OR 8.16 [1.55–6.00] []. Samoni et al. [] in the 125 critical patients cohort, described 64.8% BI-derived overhydration status with a mean hydration percentage of 80.68 ± 5.82%, while in our series we found an overhydration percentage slightly lower. The higher incidence of sepsis and multiple organ failure in critical patients constitutes inflammatory settings favorable to more fluid retention.
In the present study, patients with fluid overload showed significantly elevated levels of inflammatory parameters, CRP, and CRP/prealbumin. These findings indicate that overhydration status in COVID-19 admitted patients show a poorer outcome related to the inflammatory pattern. In ICU patients, Li et al. [] reported that an increase in CRP/prealbumin independently correlated with worse clinical outcomes. CRP/prealbumin ROC curve in predicting hospital mortality was 0.701 (0.597–0.805), p = 0.001. In our cohort, the ROC curve was similar for COVID-19 patients. To the best of our knowledge, the current study is the first time to demonstrate that CRP/prealbumin is an independent predictor of mortality in admitted COVID-19 patients. Furthermore, the prognostic value of the CRP/prealbumin for predicting mortality in COVID-19 is significantly greater than the traditional risk factor, CRP [].
COVID-19 patients with pneumonia require meticulous fluid management to avoid circulatory overload. Although fluid administration is important in patients with shock, excessive fluid administration in critical patients is associated with poor outcomes []. Based on these results, we must consider that conservative fluid management should be employed among COVID-19 patients when no evidence of shock is present. Particularly, patients with ARDS are more likely to be harmed from unnecessary fluid administration.
In the absence of specific data on the role of hyperhydration in inflammatory processes such as COVID-19, the heart failure model may be useful to see the effect of hydration on clinical outcomes. In heart failure, fluid retention caused an increased risk of mortality [OR 3.05 (1.55–6.00)] []. Hydration percentage discriminated (p = 0.001) surviving [74.00% (73.48–81.15)] and non-surviving [85.00% (74.02–87.95)] in these patients [], we also found similar differences between survivor and non-survivor patients.
We also found significant differences in BUN/creatinine, a congestion vascular marker, between surviving and non-surviving patients. A recent study revealed that BUN/creatinine may be associated with disease severity in COVID-19 with optimal thresholds of the BUN/creatinine at 51.7 had a superior possibility for mortality [AUC 0.950, (90% sensibility, 92% specificity), log-rank test, p < 0.001] [].
The predictive value of the hydration percentage depends on the choice of cut-off points, which should be developed for the specific pathology []. Using ROC analysis, Santarelli et al. [] demonstrated a similar probability of 90 d cardiovascular death [AUC 0.715; 95% CI(0.65–0.76), p < 0.04] predicted by using BIVA-derived hydration percentage. Similarly, in our study, the cut-off value of 76.15% hydration provides a clear prognostic factor with a very high risk of mortality [OR 7.692; 95%CI (2.067–28.616); p = 0.002]. Furthermore, ECW/TBW shows a higher diagnostic potency than that found in other pathologies. In chronic kidney disease, it was found an AUC = 0.64 (cut-off: 0.40, 61% sensitivity, 60% specificity, p = 0.002) []. Consequently, our results confirm a strong association between hydration status and survival in COVID-19 patients, which is more useful to use our cut-off point (0.58) since it has shown greater specificity and sensitivity in this pathology. Using 0.58 as a cut-off point, our results could more clearly establish an objective threshold for discriminating prognosis of mortality [OR 30.000; 95%CI (3.815–235.933); p = 0.001]. The cut-off value conventionally established in the literature (0.40) reaches 100% sensitivity but only 4.5% specificity.
A recent clinical COVID-19-SEIMC score [] has been validated to establish the severity prognosis of COVID-19. In our series, we found a similar relationship between score and mortality with equivalent sensitivity and specificity values to overhydration parameters. Overhydration parameters have proven to be efficient as the COVID-19 score for this purpose in our series, an easy measure could replace a multidimensional score [].
5. Conclusions
Our results identify levels of overhydration using BIVA associated with increased COVID-19 severity, 90 d mortality risk, and a hydration tertiles distribution related to the median survival time. We further demonstrate the increased prognostic value of BIVA hydration assessments compared to traditional clinical indicators of hydration.
Given its prognostic impact, these findings suggest that the evaluation of hydration status by BIA variables is adequate for bedside evaluation. It could be routinely included in COVID-19 clinical assessment at hospital admission, allowing adequate intervention to reduce mortality risk. This is recommended to maintain a restrictive fluid strategy in these patients. Therefore, careful evaluation and treatment of overhydration status are essential in COVID-19 patients, in favor of an individualized approach for restrictive fluid management providing more attention to the use of dynamic methods for evaluation of fluid change.
Whereas our findings of BI assessments are provocative, further studies are needed to validate the use of BIA in COVID-19 hydration status assessment and to incorporate this tool combined with clinical and biochemical parameters into hospitalization medical protocols.
6. Strengths–Limitations
We highlight, as strengths of our study, that is the first study that evaluated the association of overhydration—using BIVA—with mortality in COVID-19 hospitalized patients. Different BIA parameters may be useful for the early diagnosis of patients with fluid retention, allowing the provision of adequate treatment to reduce mortality risk. Overhydration assessment could be considered as an additional parameter in the clinical management of COVID-19 patients and patients with situations of acute inflammation.
The limitation in our study is the use of only admission BI assessments of hydration. There is a need for studies of serial BI measurements to monitor intra-individual variation due to COVID-induced fluid changes and the effects of clinical interventions on hydration, in order to assist in medical care and changing treatment to benefit patients.
Author Contributions
I.C.-P., A.T., D.B.-G. and J.M.G.-A. conceptualization; I.M.V.-A., I.C.-P. and A.T. methods; I.C.-P., A.T. and F.J.T. formal analysis; all authors investigation; I.C.-P., I.M.V.-A. and H.L. writing—original draft preparation; I.C.-P., F.J.T., A.T., H.L., D.B.-G. and J.M.G.-A. writing—review and editing; I.C.-P., F.J.T. and J.M.G.-A. visualization; I.C.-P., H.L., F.J.T. and J.M.G.-A. supervision. All authors know, have reviewed, and accepted the latest version of the manuscript for publication. All authors have read and agreed to the published version of the manuscript.
Funding
I.C.-P. was the recipient of a postdoctoral grant (Río Hortega CM 17/00169) and is now the recipient of a postdoctoral grant (Juan Rodes JR 19/00054) from the Instituto de Salud Carlos III and cofounded by Fondo Europeo de Desarrollo Regional-FEDER.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki and approved by the Ethics Committee of Virgen Victoria (Institutional Human Review Board).
Informed Consent Statement
Written informed consent has been obtained from the patient(s) to publish this paper.
Data Availability Statement
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Acknowledgments
We thank Marina Martínez-García for English language editing.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Huang, C.; Wang, Y.; Li, X.; Ren, L.; Zhao, J.; Hu, Y.; Zhang, L.; Fan, G.; Xu, J.; Gu, X.; et al. Clinical Features of Patients Infected with 2019 Novel Coronavirus in Wuhan, China. Lancet 2020, 395, 497–506. [Google Scholar] [CrossRef] [Green Version]
- de Bruin, S.; Bos, L.D.; van Roon, M.A.; Tuip-de Boer, A.M.; Schuurman, A.R.; Koel-Simmelinck, M.J.A.; Bogaard, H.J.; Tuinman, P.R.; van Agtmael, M.A.; Hamann, J.; et al. Clinical Features and Prognostic Factors in COVID-19: A Prospective Cohort Study. EBioMedicine 2021, 67, 103378. [Google Scholar] [CrossRef] [PubMed]
- Valtueña, J.; Ruiz-Sánchez, D.; Volo, V.; Manchado-López, P.; Garayar-Cantero, M. Acral Edema during the COVID-19 Pandemic. Int. J. Dermatol. 2020, 59, 1155–1157. [Google Scholar] [CrossRef] [PubMed]
- Cui, X.; Chen, W.; Zhou, H.; Gong, Y.; Zhu, B.; Lv, X.; Guo, H.; Duan, J.; Zhou, J.; Marcon, E.; et al. Pulmonary Edema in COVID-19 Patients: Mechanisms and Treatment Potential. Front. Pharmacol. 2021, 12, 664349. [Google Scholar] [CrossRef] [PubMed]
- Moonen, H.P.F.X.; van Zanten, F.J.L.; Driessen, L.; de Smet, V.; Slingerland-Boot, R.; Mensink, M.; van Zanten, A.R.H. Association of Bioelectric Impedance Analysis Body Composition and Disease Severity in COVID-19 Hospital Ward and ICU Patients: The BIAC-19 Study. Clin. Nutr. 2021, 40, 2328–2336. [Google Scholar] [CrossRef] [PubMed]
- Osuna-Padilla, I.A.; Rodríguez-Moguel, N.C.; Rodríguez-Llamazares, S.; Aguilar-Vargas, A.; Casas-Aparicio, G.A.; Ríos-Ayala, M.A.; Hernández-Cardenas, C.M. Low Phase Angle Is Associated with 60-Day Mortality in Critically Ill Patients with COVID-19. J. Parenter. Enter. Nutr. 2021, 46, 828–835. [Google Scholar] [CrossRef]
- Alhazzani, W.; Møller, M.H.; Arabi, Y.M.; Loeb, M.; Gong, M.N.; Fan, E.; Oczkowski, S.; Levy, M.M.; Derde, L.; Dzierba, A.; et al. Surviving Sepsis Campaign: Guidelines on the Management of Critically Ill Adults with Coronavirus Disease 2019 (COVID-19). Intensive Care Med. 2020, 46, 854–887. [Google Scholar] [CrossRef] [Green Version]
- da Silva, A.T.; Hauschild, D.B.; de Almeida Oliveira, L.D.; de Fragas Hinnig, P.; Moreno, Y.M.F.; Wazlawik, E. Association of Hyperhydration Evaluated by Bioelectrical Impedance Analysis and Mortality in Patients with Different Medical Conditions: Systematic Review and Meta-Analyses. Clin. Nutr. ESPEN 2018, 28, 12–20. [Google Scholar] [CrossRef]
- Di Somma, S.; Navarin, S.; Giordano, S.; Spadini, F.; Lippi, G.; Cervellin, G.; Dieffenbach, B.V.; Maisel, A.S. The Emerging Role of Biomarkers and Bio-Impedance in Evaluating Hydration Status in Patients with Acute Heart Failure. Clin. Chem. Lab. Med. 2012, 50, 2093–2105. [Google Scholar] [CrossRef]
- Hasanin, A.; Mostafa, M. Evaluation of Fluid Responsiveness during COVID-19 Pandemic: What Are the Remaining Choices? J. Anesth. 2020, 34, 758–764. [Google Scholar] [CrossRef]
- Lukaski, H.C.; Vega Diaz, N.; Talluri, A.; Nescolarde, L. Classification of Hydration in Clinical Conditions: Indirect and Direct Approaches Using Bioimpedance. Nutrients 2019, 11, 809. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Piccoli, A.; Rossi, B.; Pillon, L.; Bucciante, G. A New Method for Monitoring Body Fluid Variation by Bioimpedance Analysis: The RXc Graph. Kidney Int. 1994, 46, 534–539. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Talluri, A.; Liedtke, R.; Mohamed, E.I.; Maiolo, C.; Martinoli, R.; De Lorenzo, A. The Application of Body Cell Mass Index for Studying Muscle Mass Changes in Health and Disease Conditions. Acta Diabetol. 2003, 40 (Suppl. 1), S286–S289. [Google Scholar] [CrossRef] [PubMed]
- Dittmar, M.; Reber, H. Validation of Different Bioimpedance Analyzers for Predicting Cell Mass against Whole-Body Counting of Potassium (40K) as a Reference Method. Am. J. Hum. Biol. 2004, 16, 697–703. [Google Scholar] [CrossRef]
- Marini, E.; Campa, F.; Buffa, R.; Stagi, S.; Matias, C.N.; Toselli, S.; Sardinha, L.B.; Silva, A.M. Phase Angle and Bioelectrical Impedance Vector Analysis in the Evaluation of Body Composition in Athletes. Clin. Nutr. 2020, 39, 447–454. [Google Scholar] [CrossRef] [PubMed]
- Denneman, N.; Hessels, L.; Broens, B.; Gjaltema, J.; Stapel, S.N.; Stohlmann, J.; Nijsten, M.W.; Oudemans-van Straaten, H.M. Fluid Balance and Phase Angle as Assessed by Bioelectrical Impedance Analysis in Critically Ill Patients: A Multicenter Prospective Cohort Study. Eur. J. Clin. Nutr. 2020, 74, 1410–1419. [Google Scholar] [CrossRef]
- Berenguer, J.; Borobia, A.M.; Ryan, P.; Rodríguez-Baño, J.; Bellón, J.M.; Jarrín, I.; Carratalà, J.; Pachón, J.; Carcas, A.J.; Yllescas, M.; et al. Development and Validation of a Prediction Model for 30-Day Mortality in Hospitalised Patients with COVID-19: The COVID-19 SEIMC Score. Thorax 2021, 76, 920–929. [Google Scholar] [CrossRef]
- Matsue, Y.; van der Meer, P.; Damman, K.; Metra, M.; O’Connor, C.M.; Ponikowski, P.; Teerlink, J.R.; Cotter, G.; Davison, B.; Cleland, J.G.; et al. Blood Urea Nitrogen-to-Creatinine Ratio in the General Population and in Patients with Acute Heart Failure. Heart 2017, 103, 407–413. [Google Scholar] [CrossRef]
- Lu, J.; Xu, B.-B.; Zheng, Z.-F.; Xie, J.-W.; Wang, J.-B.; Lin, J.-X.; Chen, Q.-Y.; Cao, L.-L.; Lin, M.; Tu, R.-H.; et al. CRP/Prealbumin, a Novel Inflammatory Index for Predicting Recurrence after Radical Resection in Gastric Cancer Patients: Post Hoc Analysis of a Randomized Phase III Trial. Gastric. Cancer 2019, 22, 536–545. [Google Scholar] [CrossRef] [Green Version]
- Rezaie, S. COVID-19: Clinical/Therapeutic Staging Proposal and Treatment. REBEL EM Emergency Medicine Blog. 2020. Available online: https://rebelem.com/covid-19-clinical-therapeutic-staging-proposal-and-treatment/ (accessed on 12 May 2022).
- Piccoli, A.; Nigrelli, S.; Caberlotto, A.; Bottazzo, S.; Rossi, B.; Pillon, L.; Maggiore, Q. Bivariate Normal Values of the Bioelectrical Impedance Vector in Adult and Elderly Populations. Am. J. Clin. Nutr. 1995, 61, 269–270. [Google Scholar] [CrossRef]
- Evans, W.D.; McClagish, H.; Trudgett, C. Factors Affecting the in vivo Precision of Bioelectrical Impedance Analysis. Appl. Radiat. Isot. 1998, 49, 485–487. [Google Scholar] [CrossRef]
- Vettorazzi, C.; Smits, E.; Solomons, N.W. The Interobserver Reproducibility of Bioelectrical Impedance Analysis Measurements in Infants and Toddlers. J. Pediatr. Gastroenterol. Nutr. 1994, 19, 277–282. [Google Scholar] [CrossRef] [PubMed]
- Chumlea, W.C.; Schubert, C.M.; Sun, S.S.; Demerath, E.; Towne, B.; Siervogel, R.M. A Review of Body Water Status and the Effects of Age and Body Fatness in Children and Adults. J. Nutr. Health Aging 2007, 11, 111–118. [Google Scholar]
- Schutz, Y.; Kyle, U.U.G.; Pichard, C. Fat-Free Mass Index and Fat Mass Index Percentiles in Caucasians Aged 18–98 y. Int. J. Obes. Relat. Metab. Disord. 2002, 26, 953–960. [Google Scholar] [CrossRef] [Green Version]
- Moore, F.D.; Boyden, C.M. Body cell mass and limits of hydration of the fat-free body: Their relation to estimated skeletal weight. Ann. N. Y. Acad. Sci. 1963, 110, 62–71. [Google Scholar] [CrossRef]
- Selberg, O.; Selberg, D. Norms and Correlates of Bioimpedance Phase Angle in Healthy Human Subjects, Hospitalized Patients, and Patients with Liver Cirrhosis. Eur. J. Appl. Physiol. 2002, 86, 509–516. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Talluri, A.; Maggia, G. Bioimpedance Analysis (BIA) in Hemodialysis: Technical Aspects. Int. J. Artif. Organs 1995, 18, 687–692. [Google Scholar] [CrossRef]
- Lindley, E.; Devine, Y.; Hall, L.; Cullen, M.; Cuthbert, S.; Woodrow, G.; Lopot, F. A Ward-Based Procedure for Assessment of Fluid Status in Peritoneal Dialysis Patients Using Bioimpedance Spectroscopy. Perit. Dial. Int. 2005, 25 (Suppl. 3), S46–S48. [Google Scholar] [CrossRef]
- Pérez-Morales, R.; Donate-Correa, J.; Martín-Núñez, E.; Pérez-Delgado, N.; Ferri, C.; López-Montes, A.; Jiménez-Sosa, A.; Navarro-González, J.F. Extracellular Water/Total Body Water Ratio as Predictor of Mortality in Hemodialysis Patients. Ren. Fail. 2021, 43, 821–829. [Google Scholar] [CrossRef]
- Basso, F.; Berdin, G.; Virzì, G.M.; Mason, G.; Piccinni, P.; Day, S.; Cruz, D.N.; Wjewodzka, M.; Giuliani, A.; Brendolan, A.; et al. Fluid Management in the Intensive Care Unit: Bioelectrical Impedance Vector Analysis as a Tool to Assess Hydration Status and Optimal Fluid Balance in Critically Ill Patients. Blood Purif. 2013, 36, 192–199. [Google Scholar] [CrossRef]
- Rahmel, T.; Nowak, H.; Rump, K.; Siffert, W.; Peters, J.; Adamzik, M. The Aquaporin 5 -1364A/C Promoter Polymorphism Impacts on Resolution of Acute Kidney Injury in Pneumonia Evoked ARDS. PLoS ONE 2018, 13, e0208582. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Samoni, S.; Vigo, V.; Reséndiz, L.I.B.; Villa, G.; De Rosa, S.; Nalesso, F.; Ferrari, F.; Meola, M.; Brendolan, A.; Malacarne, P.; et al. Impact of Hyperhydration on the Mortality Risk in Critically Ill Patients Admitted in Intensive Care Units: Comparison between Bioelectrical Impedance Vector Analysis and Cumulative Fluid Balance Recording. Crit. Care 2016, 20, 95. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Li, L.; Dai, L.; Wang, X.; Wang, Y.; Zhou, L.; Chen, M.; Wang, H. Predictive Value of the C-Reactive Protein-to-Prealbumin Ratio in Medical ICU Patients. Biomark. Med. 2017, 11, 329–337. [Google Scholar] [CrossRef] [PubMed]
- Santarelli, S.; Russo, V.; Lalle, I.; De Berardinis, B.; Navarin, S.; Magrini, L.; Piccoli, A.; Codognotto, M.; Castello, L.M.; Avanzi, G.C.; et al. Usefulness of Combining Admission Brain Natriuretic Peptide (BNP) plus Hospital Discharge Bioelectrical Impedance Vector Analysis (BIVA) in Predicting 90 Days Cardiovascular Mortality in Patients with Acute Heart Failure. Int. Emerg. Med. 2017, 12, 445–451. [Google Scholar] [CrossRef] [Green Version]
- Ok, F.; Erdogan, O.; Durmus, E.; Carkci, S.; Canik, A. Predictive Values of Blood Urea Nitrogen/Creatinine Ratio and Other Routine Blood Parameters on Disease Severity and Survival of COVID-19 Patients. J. Med. Virol. 2021, 93, 786–793. [Google Scholar] [CrossRef]
- Guo, Q.; Lin, J.; Li, J.; Yi, C.; Mao, H.; Yang, X.; Yu, X. The Effect of Fluid Overload on Clinical Outcome in Southern Chinese Patients Undergoing Continuous Ambulatory Peritoneal Dialysis. Perit. Dial. Int. 2015, 35, 691–702. [Google Scholar] [CrossRef] [Green Version]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).