Mealtime TV Use Is Associated with Higher Discretionary Food Intakes in Young Australian Children: A Two-Year Prospective Study
Abstract
:1. Introduction
2. Materials and Methods
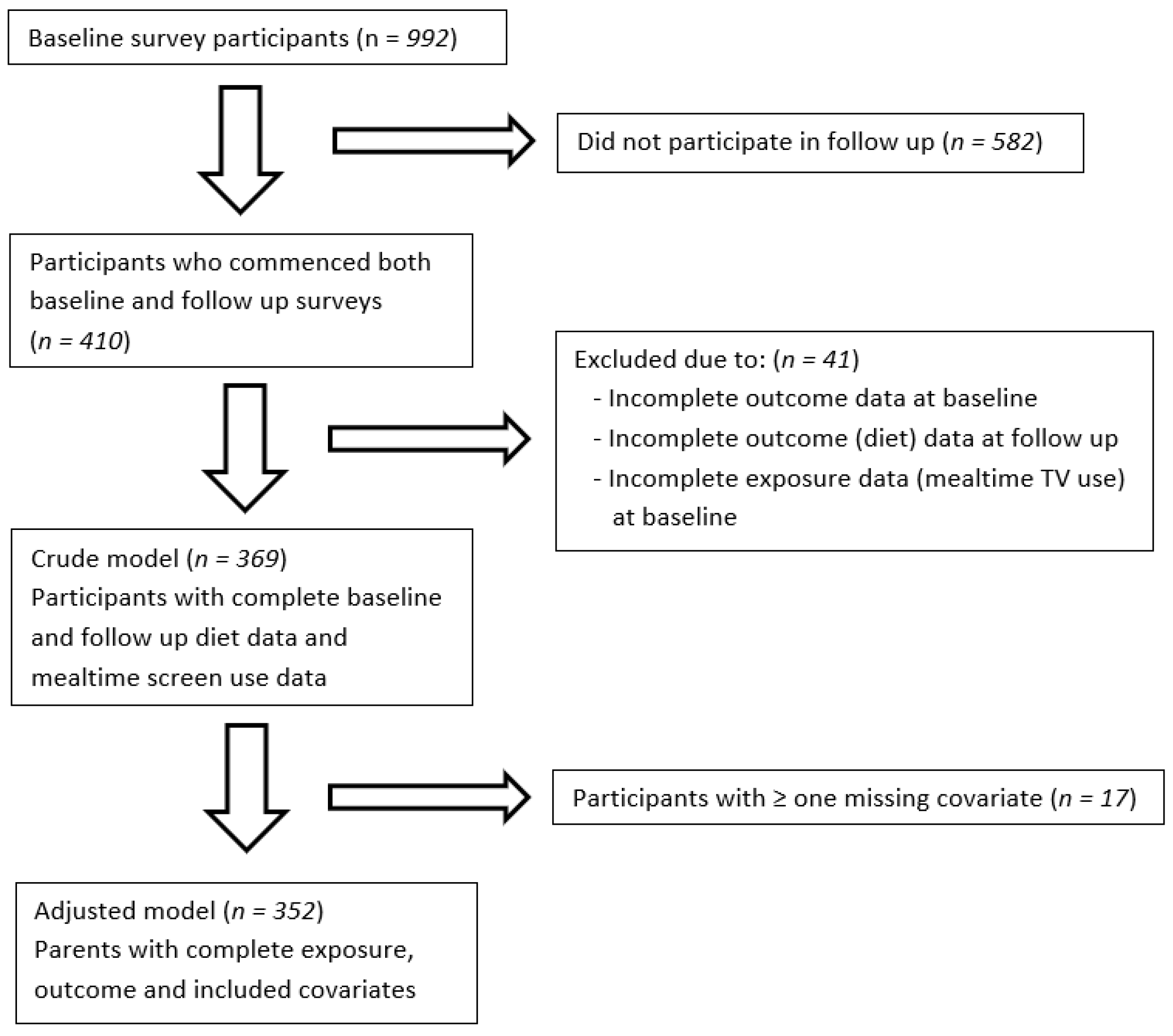
2.1. Study Participants
2.2. Mealtime TV Use
2.3. Intakes of Discretionary Foods, Fruits, and Vegetables
2.4. Covariates
2.5. Socioeconomic Position
2.6. Survey Reliability
2.7. Statistical Analysis
3. Results
3.1. Participant Demographics
3.2. Dietary Outcomes
3.3. Baseline Television Use and Prospective Dietary Outcomes
3.4. Socioeconomic Position
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
| Non-Responders (n = 406–586) | Responders (n = 398–406) | p Value | |
|---|---|---|---|
| Parent characteristics | |||
| Highest level of completed schooling n (%) | |||
| Less than university equivalent | 161 (30.4%) | 110 (27.6) | - |
| University degree equivalent or higher | 369 (69.6%) | 288 (72.4) | 0.34 |
| Child characteristics | |||
| Age mean (SD) | 2.51 (1.36) | 2.43 (1.31) | 0.37 |
| Gender (male) n (%) | 311 (53.1%) | 210 (51.7%) | 0.68 |
| Baseline diet mean (SD) | |||
| Fruit (serves/day) | 3.68 (0.56) | 3.67 (0.45) | 0.56 |
| Veg (serves/day) | 3.45 (0.69) | 3.43 (0.69) | 0.63 |
| Discretionary (occasions/day) | 0.98 (0.90) | 0.93 (0.85) | 0.41 |
| University Education (n = 219–264) | Non-University Education (n = 75–92) | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Discretionary Food | Vegetables | Fruit | Discretionary Food | Vegetables | Fruit | |||||||
| (Frequency/Day) | (Serves/Day) | (Serves/Day) | (Frequency/Day) | (Serves/day) | (Serves/Day) | |||||||
| β (95% CI) | p Value | OR (95% CI) | p Value | OR (95% CI) | p Value | β (95% CI) | p Value | OR (95% CI) | p Value | OR (95% CI) | p Value | |
| Daily | 0.21 (0.1–0.32) | <0.01 | 0.86 (0.58–1.26) | 0.43 | 0.78 (0.51–1.20) | 0.26 | 0.08 (−0.08–0.24) | 0.33 | 0.86 (0.52–1.43) | 0.57 | 0.94 (0.54–0.61) | 0.813 |
| Never or <1 day per week (reference) | ||||||||||||
| Breakfast | ||||||||||||
| 1–2 days per week | 0.39 (0.08–0.70) | 0.01 | 0.78 (0.26–2.78) | 0.65 | 0.64 (0.19–2.24) | 0.49 | 0.32 (−0.10–0.74) | 0.14 | 1.40 (0.35–5.71) | 0.47 | 1.66 (0.33–8.44) | 0.54 |
| 3–7 days per week | 0.23 (0.02–0.43) | 0.03 | 1.00 (0.49–2.05) | 0.99 | 0.61 (0.28–1.35) | 0.22 | 0.17 (−0.20–0.54) | 0.36 | 1.01 (0.31–3.22) | 0.99 | 1.08 (0.30–3.89) | 0.12 |
| Lunch | ||||||||||||
| 1–2 days per week | 0.04 (−0.23–0.31) | 0.29 | 1.02 (0.37–2.76) | 0.97 | 0.49 (0.17–1.39) | 0.18 | −0.06 (−0.50–0.37) | 0.78 | 0.31 (0.06–1.53) | 0.15 | 1.84 (0.31–10.82) | 0.50 |
| 3–7 days per week | 0.39 (0.10–0.69) | 0.01 | 0.68 (0.25–1.87) | 0.46 | 0.39 (1.33–1.11) | 0.08 | 0.21 (0.38–0.87) | 0.36 | 0.56 (0.11–2.77) | 0.48 | 0.46 (1.08–2.51) | 0.37 |
| Dinner | ||||||||||||
| 1–2 days per week | 0.24 (0.01–0.48) | 0.05 | 0.82 (0.35–1.92) | 0.65 | 0.41 (0.17–1.02) | 0.05 | 0.09 (−0.26–0.45) | 0.60 | 0.49 (0.15–1.58) | 0.23 | 0.93 (0.27–3.23) | 0.90 |
| 3–7 days per week | 0.22 (−0.02–0.46) | 0.07 | 0.56 (0.24–1.29) | 0.18 | 0.54 (0.20–1.42) | 0.21 | 0.05 (−0.34–0.45) | 0.27 | 0.61 (0.18–2.10) | 0.43 | 1.43 (0.34–6.00) | 0.63 |
| Snacks | ||||||||||||
| 1–2 days per week | 0.10 (−0.15–0.34) | 0.44 | 0.90 (0.37–2.19) | 0.81 | 0.86 (0.34–2.22) | 0.76 | −0.26 (−0.70–0.18) | 0.24 | 0.39 (0.08–1.99) | 0.26 | 0.81 (0.13–5.07) | 0.82 |
| 3–7 days per week | 0.21 (−0.03–0.44) | 0.08 | 0.82 (0.38–1.78) | 0.62 | 1.01 (0.42–2.45) | 0.98 | 0.06 (−0.35–0.46) | 0.78 | 0.38 (0.09–1.54) | 0.18 | 0.40 (0.09–1.89) | 0.25 |
Appendix B. List of Discretionary Food Items Assessed
- i.
- Hot chips, French fries, wedges, or fried potatoes?
- ii.
- Potato crisps or other salty snacks (such as Twisties, corn chips, or Barbecue Shapes)?
- iii.
- Meals or snacks such as burgers, pies, pizza, chicken, or chips from places like McDonald’s, Hungry Jack’s, Pizza Hut, KFC, Red Rooster, or local takeaway food places?
- iv.
- Cakes, muffins, scones, muesli bars, or sweet biscuits?
- v.
- Chocolate, sweets, or lollies?
- vi.
- Soft drink, cordial, sports drinks, or fruit juice drinks?
- i.
- Never or less than once a month
- ii.
- 1–3 times a month
- iii.
- Once a week
- iv.
- 2–4 times a week
- v.
- 5–6 times a week
- vi.
- Once a day
- vii.
- 2 or more times per day
References
- Australian Bureau of Statistics. Australian Health Survey: Nutrition First Results—Foods and Nutrients, 2011-12; Report Number: 4364.0.55.007. Available online: https://www.abs.gov.au/ausstats/abs@.nsf/Lookup/by%20Subject/4364.0.55.007~2011-12~Main%20Features~Discretionary%20foods~700 (accessed on 27 October 2019).
- Spence, A.C.; Campbell, K.J.; Lioret, S.; McNaughton, S.A. Early Childhood Vegetable, Fruit, and Discretionary Food Intakes Do Not Meet Dietary Guidelines, but Do Show Socioeconomic Differences and Tracking over Time. J. Acad. Nutr. Diet. 2018, 118, 1634–1643.e1. [Google Scholar] [CrossRef] [PubMed]
- Australian Bureau of Statistics. Daily intake of Fruits and Vegetables. National Health Survey: First Results, 2014-15; Report Number: 4364.0.55.001. Available online: http://www.abs.gov.au/ausstats/abs@.nsf/Lookup/by%20Subject/4364.0.55.001~2014-15~Main%20Features~Daily%20intake%20of%20fruit%20and%20vegetables~28 (accessed on 27 October 2019).
- Mihrshahi, S.; Myton, R.; Partridge, S.R.; Esdaile, E.; Hardy, L.L.; Gale, J. Sustained low consumption of fruit and vegetables in Australian children: Findings from the Australian National Health Surveys. Health Promot. J. Aust. 2019, 30, 83–87. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- UNICEF. The State of the World’s Children 2019. Children, Food and Nutrition: Growing Well in a Changing World; UNICEF: New York, NY, USA, 2019.
- Mikkilä, V.; Räsänen, L.; Raitakari, O.T.; Pietinen, P.; Viikari, J. Longitudinal changes in diet from childhood into adulthood with respect to risk of cardiovascular diseases: The Cardiovascular Risk in Young Finns Study. Eur. J. Clin. Nutr. 2004, 58, 1038–1045. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mameli, C.; Mazzantini, S.; Zuccotti, G.V. Nutrition in the First 1000 Days: The Origin of Childhood Obesity. Int. J. Environ. Res. Public Health 2016, 13, 838. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gubbels, J.S.; Raaijmakers, L.G.M.; Gerards, S.M.P.L.; Kremers, S.P.J. Dietary Intake by Dutch 1- to 3-Year-Old Children at Childcare and at Home. Nutrients 2014, 6, 304–318. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Australian Institute of Health and Welfare. Childhood Overweight and Obesity—The Impact of the Home Environment; Report Number: PHE 283; AIHW: Canberra, Australia, 2021.
- Lacy, K.E.; Spence, A.C.; McNaughton, S.A.; Crawford, D.A.; Wyse, R.J.; Wolfenden, L.; Campbell, K.J. Home environment predictors of vegetable and fruit intakes among Australian children aged 18 months. Appetite 2019, 1, 95–104. [Google Scholar] [CrossRef] [PubMed]
- Dubois, L.; Farmer, A.; Girard, M.; Burnier, D.; Porcherie, M. Demographic and socio-economic factors related to food intake and adherence to nutritional recommendations in a cohort of pre-school children. Public Health Nutr. 2011, 14, 1096–1104. [Google Scholar] [CrossRef] [Green Version]
- Bell, L.K.; Golley, R.K.; Daniels, L.; Magarey, A.M. Dietary patterns of Australian children aged 14 and 24 months, and associations with socio-demographic factors and adiposity. Eur. J. Clin. Nutr. 2013, 67, 638–645. [Google Scholar] [CrossRef] [Green Version]
- Australian Institute of Health and Welfare. Nutrition across the Life Stages. AIHW. 2018. Available online: https://www.aihw.gov.au/reports/food-nutrition/nutrition-across-the-life-stages/contents/table-of-contents (accessed on 23 October 2019).
- Manyanga, T.; Tremblay, M.S.; Chaput, J.P.; Katzmarzyk, P.T.; Fogelholm, M.; Hu, G.; Kuriyan, R.; Kurpad, A.; Lambert, E.V.; Maher, C.; et al. Socioeconomic status and dietary patterns in children from around the world: Different associations by levels of country human development? BMC Public Health 2017, 17, 457. [Google Scholar] [CrossRef] [Green Version]
- Zarnowiecki, D.M.; Dollman, J.; Parletta, N. Associations between predictors of children’s dietary intake and socioeconomic position: A systematic review of the literature. Obes. Rev. 2014, 15, 375–391. [Google Scholar] [CrossRef]
- Glanz, K.; Metcalfe, J.J.; Folta, S.C.; Brown, A.; Fiese, B. Diet and Health Benefits Associated with In-Home Eating and Sharing Meals at Home: A Systematic Review. Int. J. Environ. Res. Public Health 2021, 18, 1577. [Google Scholar] [CrossRef] [PubMed]
- Dallacker, M.; Hertwig, R.; Mata, J. The frequency of family meals and nutritional health in children: A meta-analysis. Obes. Rev. 2018, 19, 638–653. [Google Scholar] [CrossRef] [PubMed]
- Berge, J.M.; Truesdale, K.P.; Sherwood, N.E.; Mitchell, N.; Heerman, W.J.; Barkin, S.; Matheson, D.; Levers-Landis, C.E.; French, S.A. Beyond the dinner table: Who’s having breakfast, lunch and dinner family meals and which meals are associated with better diet quality and BMI in pre-school children? Public Health Nutr. 2017, 20, 3275–3284. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Litterbach, E.V.; Campbell, K.J.; Spence, A.C. Family meals with young children: An online study of family mealtime characteristics, among Australian families with children aged six months to six years. BMC Public Health 2017, 17, 111. [Google Scholar] [CrossRef] [Green Version]
- Avery, A.; Anderson, C.; McCullough, F. Associations between children’s diet quality and watching television during meal or snack consumption: A systematic review. Matern. Child Nutr. 2017, 13, e12428. [Google Scholar] [CrossRef]
- Fayet-Moore, F.; Peters, V.; McConnell, A.; Petocz, P.; Eldridge, A.L. Weekday snacking prevalence, frequency, and energy contribution have increased while foods consumed during snacking have shifted among Australian children and adolescents: 1995, 2007 and 2011-12 National Nutrition Surveys. Nutr. J. 2017, 16, 65. [Google Scholar] [CrossRef] [Green Version]
- Boylan, S.; Hardy, L.L.; Drayton, B.A.; Grunseit, A.; Mihrshahi, S. Assessing junk food consumption among Australian children: Trends and associated characteristics from a cross-sectional study. BMC Public Health 2017, 17, 299. [Google Scholar] [CrossRef] [Green Version]
- Dallacker, M.; Hertwig, R.; Mata, J. Quality matters: A meta-analysis on components of healthy family meals. Health Psychol. 2019, 38, 1137–1149. [Google Scholar] [CrossRef]
- Andaya, A.A.; Arredondo, E.M.; Alcaraz, J.E.; Lindsay, S.P.; Elder, J.P. The Association between Family Meals, TV Viewing during Meals, and Fruit, Vegetables, Soda, and Chips Intake among Latino Children. J. Nutr. Educ. Behav. 2011, 43, 308–315. [Google Scholar] [CrossRef] [Green Version]
- Blundell-Birtill, P.; Hetherington, M.M. Determinants of Portion Size in Children and Adolescents: Insights from the UK National Diet and Nutrition Survey Rolling Programme (2008–2016). Nutrients 2019, 11, 2957. [Google Scholar] [CrossRef] [Green Version]
- Wenhold, H.; Harrison, K. Television use and family mealtimes among a sample of US families with preschoolers. J. Child. Media 2017, 12, 98–115. [Google Scholar] [CrossRef]
- Mak, T.N.; Prynne, C.J.; Cole, D.; Fitt, E.; Roberts, C.; Bates, B.; Stephen, A.M. Assessing eating context and fruit and vegetable consumption in children: New methods using food diaries in the UK National Diet and Nutrition Survey Rolling Programme. Int. J. Behav. Nutr. Phys. Act. 2012, 9, 126. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Campbell, K.L.; Babiarz, A.; Wang, Y.; Tilton, N.A.; Black, M.M.; Hager, E.R. Factors in the home environment associated with toddler diet: An ecological momentary assessment study. Public Health Nutr. 2018, 21, 1855–1864. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kasper, N.; Ball, S.C.; Halverson, K.; Miller, A.L.; Appugliese, D.; Lumeng, J.C.; Peterson, K.E. Deconstructing the Family Meal: Are Characteristics of the Mealtime Environment Associated with the Healthfulness of Meals Served? J. Acad. Nutr. Diet. 2019, 119, 1296–1304. [Google Scholar] [CrossRef] [PubMed]
- Wedde, S.; Haines, J.; Ma, D.; Duncan, A.; Darlington, G. Associations between Family Meal Context and Diet Quality among Preschool-Aged Children in the Guelph Family Health Study. Can. J. Diet. Pract. Res. 2020, 81, 21–27. [Google Scholar] [CrossRef]
- Collings, P.J.; Kelly, B.; West, J.; Wright, J. Associations of TV Viewing Duration, Meals and Snacks Eaten When Watching TV, and a TV in the Bedroom with Child Adiposity. Obesity 2018, 26, 1619–1628. [Google Scholar] [CrossRef]
- Weatherspoon, L.J.; Venkatesh, S.; Horodynski, M.A.; Stommel, M.; Brophy-Herb, H.E. Food Patterns and Mealtime Behaviors in Low-Income Mothers and Toddlers. J. Community Health Nurs. 2013, 30, 1–15. [Google Scholar] [CrossRef]
- Horodynski, M.A.; Brophy-Herb, H.; Henry, M.; Smith, K.A.; Weatherspoon, L. Toddler feeding: Expectations and experiences of low-income African American mothers. Health Educ. J. 2009, 68, 14–25. [Google Scholar] [CrossRef]
- Lissner, L.; Lanfer, A.; Gwozdz, W.; Olafsdottir, S.; Eiben, G.; Moreno, L.A.; Santaliestra-Pasías, A.M.; Kovács, E.; Barba, G.; Loit, H.-M.; et al. Television habits in relation to overweight, diet and taste preferences in European children: The IDEFICS study. Eur. J. Epidemiol. 2012, 27, 705–715. [Google Scholar] [CrossRef] [Green Version]
- Cox, R.; Skouteris, H.; Rutherford, L.; Fuller-Tyszkiewicz, M.; Dell’ Aqulia, D.; Hardy, L.L. Television viewing, television content, food intake, physical activity and body mass index: A cross-sectional study of preschool children aged 2–6 years. Health Promot. J. Austr. 2012, 23, 58–62. [Google Scholar] [CrossRef]
- O′Connor, T.M.; Elias, C.; Thompson, R.R.; Arlinghaus, K.R.; Vollrath, K.; Hernandez, D.C.; Power, T.G.; Hughes, S.O. The association of TV viewing during dinner meals with quality of dietary intake and BMI z-scores among low income, ethnic minority preschool children. Appetite 2019, 140, 231–238. [Google Scholar] [CrossRef] [PubMed]
- Chan, R.; Yeung, S.; Leung, C.; Lo, S.K.; Tsang, S. Family factors and fruit and vegetable consumption in Chinese preschool children living in Hong Kong. J. Child. Serv. 2018, 13, 122–133. [Google Scholar] [CrossRef]
- Pearson, N.; Biddle, S.J.H.; Griffiths, P.; Johnston, J.P.; Haycraft, E. Clustering and correlates of screen-time and eating behaviours among young children. BMC Public Health 2018, 18, 753. [Google Scholar] [CrossRef] [PubMed]
- Zarnowiecki, D.; Ball, K.; Parletta, N.; Dollman, J. Describing socioeconomic gradients in children’s diets-does the socioeconomic indicator used matter? Int. J. Behav. Nutr. Phys. Act. 2014, 11, 44. [Google Scholar] [CrossRef] [Green Version]
- SurveyMonkey Inc.: San Mateo, CA, USA. Available online: https://www.surveymonkey.com/?ut_source=sem_lp&ut_source2=sem&ut_source3=header (accessed on 1 January 2014).
- Sweetman, C.; McGowan, L.; Croker, H.; Cooke, L. Characteristics of family mealtimes affecting children’s vegetable consumption and liking. J. Am. Diet. Assoc. 2011, 111, 269–273. [Google Scholar] [CrossRef]
- Koszewski, W.; Behrends, D.; Nichols, M.; Sehi, N.; Jones, G. Patterns of Family Meals and Food and Nutrition Intake in Limited Resource Families. Fam. Consum. Sci. Res. J. 2011, 39, 431–441. [Google Scholar] [CrossRef]
- Campbell, K.J.; Hesketh, K.D.; McNaughton, S.A.; Ball, K.; McCallum, Z.; Lynch, J.; Crawford, D.A. The extended Infant Feeding, Activity and Nutrition Trial (InFANT Extend) Program: A cluster-randomized controlled trial of an early intervention to prevent childhood obesity. BMC Public Health 2016, 16, 166. [Google Scholar] [CrossRef] [Green Version]
- Flood, V.M.; Webb, K.; Rangan, A. Recommendations for Short Questions to Assess Food Consumption in Children for the NSW Health Surveys; NSW Centre for Public Health Nutrition: Sydney, Australia, 2005.
- Riley, M.; Rutishauser, I.; Webb, K. Comparison of Short Questions with Weighed Dietary Records; Health and Aged Care: Canberra, Australia, 2001.
- Rutishauser, I.; Webb, K.; Abraham, B.; Allsopp, R. Evaluation of Short Dietary Questions from the 1995 National Nutrition Survey; Australian Government Department of Health and Ageing: Canberra, Australia, 2001.
- Golley, R.K.; Bell, L.K.; Hendrie, G.A.; Rangan, A.M.; Spence, A.; McNaughton, S.A.; Carpenter, L.; Allman-Farinelli, M.; Michelle De Silva, A.; Gill, T.; et al. Validity of short food questionnaire items to measure intake in children and adolescents: A systematic review. J. Hum. Nutr. Diet. 2017, 30, 36–50. [Google Scholar] [CrossRef]
- Cancer Council Victoria. Dietary Questionnaire for Epidemiological Studies Version 3.2 (DQES v3.2). Available online: https://www.cancervic.org.au/research/epidemiology/nutritional_assessment_services (accessed on 9 January 2020).
- Trofholz, A.C.; Telke, S.; Loth, K.; Tate, A.; Berge, J.M. Examining Predictors of Watching Television During Family Meals in a Diverse Sample. J. Nutr. Educ. Behav. 2019, 51, 1113–1120. [Google Scholar] [CrossRef]
- Collins, L.J.; Lacy, K.E.; Campbell, K.J.; McNaughton, S.A. The Predictors of Diet Quality among Australian Children Aged 3.5 Years. J. Acad. Nutr. Diet. 2016, 116, 1114–1126.e2. [Google Scholar] [CrossRef] [Green Version]
- Koo, T.K.; Li, M.Y. A Guideline of Selecting and Reporting Intraclass Correlation Coefficients for Reliability Research. J. Chiropr. Med. 2016, 15, 155–163. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Brunstrom, J.M.; Mitchell, G.L. Effects of distraction on the development of satiety. Br. J. Nutr. 2006, 96, 761–769. [Google Scholar] [PubMed]
- Wansink, B. Environmental factors that increase the food intake and consumption volume of unknowing consumers. Annu. Rev. Nutr. 2004, 24, 455–479. [Google Scholar] [CrossRef] [Green Version]
- Berge, J.M.; Rowley, S.; Trofholz, A.; Hanson, C.; Rueter, M.; MacLehose, R.F.; Neumark-Sztainer, D. Childhood Obesity and Interpersonal Dynamics During Family Meals. Pediatrics 2014, 134, 923–932. [Google Scholar] [CrossRef] [Green Version]
- Skafida, V. The family meal panacea: Exploring how different aspects of family meal occurrence, meal habits and meal enjoyment relate to young children’s diets. Soc. Health Illn. 2013, 35, 906–923. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yang-Huang, J.; van Grieken, A.; Wang, L.; Jansen, W.; Raat, H. Clustering of Sedentary Behaviours, Physical Activity, and Energy-Dense Food Intake in Six-Year-Old Children: Associations with Family Socioeconomic Status. Nutrients 2020, 12, 1722. [Google Scholar] [CrossRef] [PubMed]
- Pries, A.M.; Filteau, S.; Ferguson, E.L. Snack food and beverage consumption and young child nutrition in low- and middle-income countries: A systematic review. Matern. Child Nutr. 2019, 15, e12729. [Google Scholar] [CrossRef]
- Thimmig, L.M.; Cabana, M.D.; Bentz, M.G.; Potocka, K.; Beck, A.; Fong, L.; Chao, C.; Caughey, A.B.; Wong, A.; McKean, M. Television during Meals in the First 4 Years of Life. Clin Pediatr. 2017, 56, 659–666. [Google Scholar] [CrossRef]
- Gasser, C.E.; Mensah, F.K.; Kerr, J.A.; Wake, M. Early life socioeconomic determinants of dietary score and pattern trajectories across six waves of the Longitudinal Study of Australian Children. J. Epidemiol. Community Health 2017, 71, 1152–1160. [Google Scholar] [CrossRef]
- Australian Bureau of Statistics. Gender Indicators, Australia: Education. Available online: https://www.abs.gov.au/ausstats/abs@.nsf/Lookup/by%20Subject/4125.0~Sep%202018~Main%20Features~Education~5 (accessed on 29 May 2020).
| n (%) | ||
|---|---|---|
| Parent education | Below university equivalent | 97 (26) |
| University degree | 272 (74) | |
| Child gender | Male | 192 (52) |
| Female | 177 (48) | |
| Child age (years) mean (SD) | Baseline | 2.5 (1) |
| Follow-up | 4.3 (1) | |
| Eating location (baseline) | ||
| Breakfast (n = 359) | Sub-optimal | 83 (23) |
| Optimal | 276 (77) | |
| Lunch (n = 304) | Sub-optimal | 80 (26) |
| Optimal | 224 (74) | |
| Dinner (n = 365) | Sub-optimal | 53 (15) |
| Optimal | 312 (86) | |
| Snacks (n = 317) | Sub-optimal | 226 (71) |
| Optimal | 91 (29) | |
| Family meal frequency (baseline) | ||
| Breakfast (n = 368) | never | 22 (6) |
| 1–2 days | 46 (13) | |
| 3–7 days | 300 (82) | |
| Lunch (n = 365) | never | 15 (4) |
| 1–2 days | 58 (16) | |
| 3–7 days | 292 (80) | |
| Dinner (n = 365) | never | 19 (5) |
| 1–2 days | 26 (7) | |
| 3–7 days | 320 (88) | |
| Snacks (n = 361) | never | 28 (8) |
| 1–2 days | 69 (19) | |
| 3–7 days | 264 (73) | |
| Mealtime TV use frequency (baseline) | ||
| Breakfast (ICC 0.96) | never | 234 (63) |
| 1–2 days | 38 (10) | |
| 3–7 days | 97 (26) | |
| Lunch (ICC 0.88) | never | 254 (69) |
| 1–2 days | 57 (16) | |
| 3–7 days | 58 (16) | |
| Dinner (ICC 0.77) | never | 246 (67) |
| 1–2 days | 62 (17) | |
| 3–7 days | 61 (17) | |
| Snacks (ICC 0.77) | never | 154 (42) |
| 1–2 days | 88 (24) | |
| 3–7 days | 127 (34) | |
| Summed daily frequency | mean = 0.7 SD = 0.8 | range 1–4 |
| Discretionary Food | Daily Vegetable Intakes | Daily Fruit Intakes | ||||
|---|---|---|---|---|---|---|
| (Daily Frequency) | (≥2 Serves/Day) | (≥2 Serves/Day) | ||||
| β (95% CI) | p Value | OR (95% CI) | p Value | OR (95% CI) | p Value | |
| Daily mealtime TV use (frequency/day) | 0.16 (0.07–0.25) a | <0.01 | 0.87 (0.66–1.14) b | 0.32 | 0.79 (0.58–1.10) b | 0.11 |
| Breakfast TV use | ||||||
| <1 day per week | (REF) | |||||
| 1–2 days per week | 0.27 (0.03–0.51) | 0.03 | 1.04 (0.47–2.30) | 0.91 | 0.74 (0.30–1.86) | 0.52 |
| 3–7 days per week | 0.19 (0.01–0.36) | 0.03 | 0.87 (.51–1.49) | 0.62 | 0.58 (0.32–1.06) | 0.08 |
| Lunch TV use | ||||||
| 1–2 days per week | 0.09 (−0.11–0.30) | 0.36 | 0.79 (0.41–1.50) | 0.46 | 0.67 (0.33–1.37) | 0.27 |
| 3–7 days per week | 0.30 (0.10–0.51) | <0.01 | 0.79 (0.41–1.50) | 0.46 | 0.47 (0.24–0.95) | 0.04 |
| Dinner TV use | ||||||
| 1–2 days per week | 0.20 (0.00–0.39) | 0.05 | 0.66 (0.36–1.25) | 0.20 | 0.48 (0.24–0.95) | 0.03 |
| 3–7 days per week | 0.15 (−0.05–0.35) | 0.13 | 0.56 (0.30–1.04) | 0.07 | 0.71 (0.34–1.50) | 0.37 |
| Snack time TV use | ||||||
| 1–2 days per week | 0.00 (−0.19–0.19) | 1.00 | 0.81 (0.44–1.49) | 0.50 | 0.66 (0.32–1.37) | 0.27 |
| 3–7 days per week | 0.21 (0.03–0.39) | 0.02 | 0.84 (0.49–1.44) | 0.53 | 0.57 (0.30–1.06) | 0.08 |
| Discretionary Food | Daily Vegetable Intakes | Daily Fruit Intakes | ||||
|---|---|---|---|---|---|---|
| (Daily Frequency) | (≥2 Serves/Day) | (≥2 Serves/Day) | ||||
| β (95% CI) | p Value | OR (95% CI) | p Value | OR (95% CI) | p Value | |
| Daily mealtime TV use (frequency/day) | 0.16 (0.07–0.67) a | <0.01 | 0.84 (0.62–1.13) b | 0.24 | 0.85 (0.61–1.8) b | 0.33 |
| Breakfast TV use | ||||||
| ≤1 day per week | (REF) | |||||
| 1–2 days per week | 0.36 (0.12–0.60) | <0.01 | 0.92 (0.39–2.19) | 0.86 | 0.96 (0.35–2.58) | 0.93 |
| 3–7 days per week | 0.18 (0.02–0.37) | 0.03 | 1.00 (0.55–1.84) | 0.99 | 0.73 (0.37–1.44) | 0.37 |
| Lunch TV use | ||||||
| 1–2 days per week | 0.01 (−0.22–0.24) | 0.90 | 0.77 (0.34–1.71) | 0.52 | 0.85 (0.35–2.03) | 0.71 |
| 3–7 days per week | 0.31 (0.07–0.55) | 0.01 | 0.73 (0.33–1.63) | 0.45 | 0.46 (0.20–1.08) | 0.08 |
| Dinner TV use | ||||||
| 1–2 days per week | 0.19 (0.00–0.39) | 0.05 | 0.68 (0.35–1.33) | 0.26 | 0.58 (0.28–1.21) | 0.15 |
| 3–7 days per week | 0.15 (−0.05–0.35) | 0.13 | 0.56 (0.29–1.10) | 0.09 | 0.84 (0.37–1.90) | 0.66 |
| Snacks TV use | ||||||
| 1–2 days per week | 0.00 (−0.22–0.21) | 0.98 | 0.78 (0.36–1.70) | 0.54 | 0.85 (0.37–1.97) | 0.71 |
| 3–7 days per week | 0.16 (−0.04–0.36) | 0.13 | 0.66 (0.36–1.30) | 0.22 | 0.75 (0.36–1.59) | 0.45 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Litterbach, E.-k.; Zheng, M.; Campbell, K.J.; Laws, R.; Spence, A.C. Mealtime TV Use Is Associated with Higher Discretionary Food Intakes in Young Australian Children: A Two-Year Prospective Study. Nutrients 2022, 14, 2606. https://doi.org/10.3390/nu14132606
Litterbach E-k, Zheng M, Campbell KJ, Laws R, Spence AC. Mealtime TV Use Is Associated with Higher Discretionary Food Intakes in Young Australian Children: A Two-Year Prospective Study. Nutrients. 2022; 14(13):2606. https://doi.org/10.3390/nu14132606
Chicago/Turabian StyleLitterbach, Eloise-kate, Miaobing Zheng, Karen J. Campbell, Rachel Laws, and Alison C. Spence. 2022. "Mealtime TV Use Is Associated with Higher Discretionary Food Intakes in Young Australian Children: A Two-Year Prospective Study" Nutrients 14, no. 13: 2606. https://doi.org/10.3390/nu14132606
APA StyleLitterbach, E.-k., Zheng, M., Campbell, K. J., Laws, R., & Spence, A. C. (2022). Mealtime TV Use Is Associated with Higher Discretionary Food Intakes in Young Australian Children: A Two-Year Prospective Study. Nutrients, 14(13), 2606. https://doi.org/10.3390/nu14132606







