Effect of Oral Intake of Lactiplantibacillus plantarum APsulloc 331261 (GTB1TM) on Diarrhea-Predominant Irritable Bowel Syndrome: A Randomized, Double-Blind, Placebo-Controlled Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Supplement Preparation
2.2. Study Participants
2.3. Study Design and Ethics
2.4. Study Procedure
2.5. Evaluation of Efficacy Endpoints
2.6. DNA Extraction and Next-Generation Sequencing (NGS) of Fecal Microbiota
2.7. Statistical Analysis
3. Results
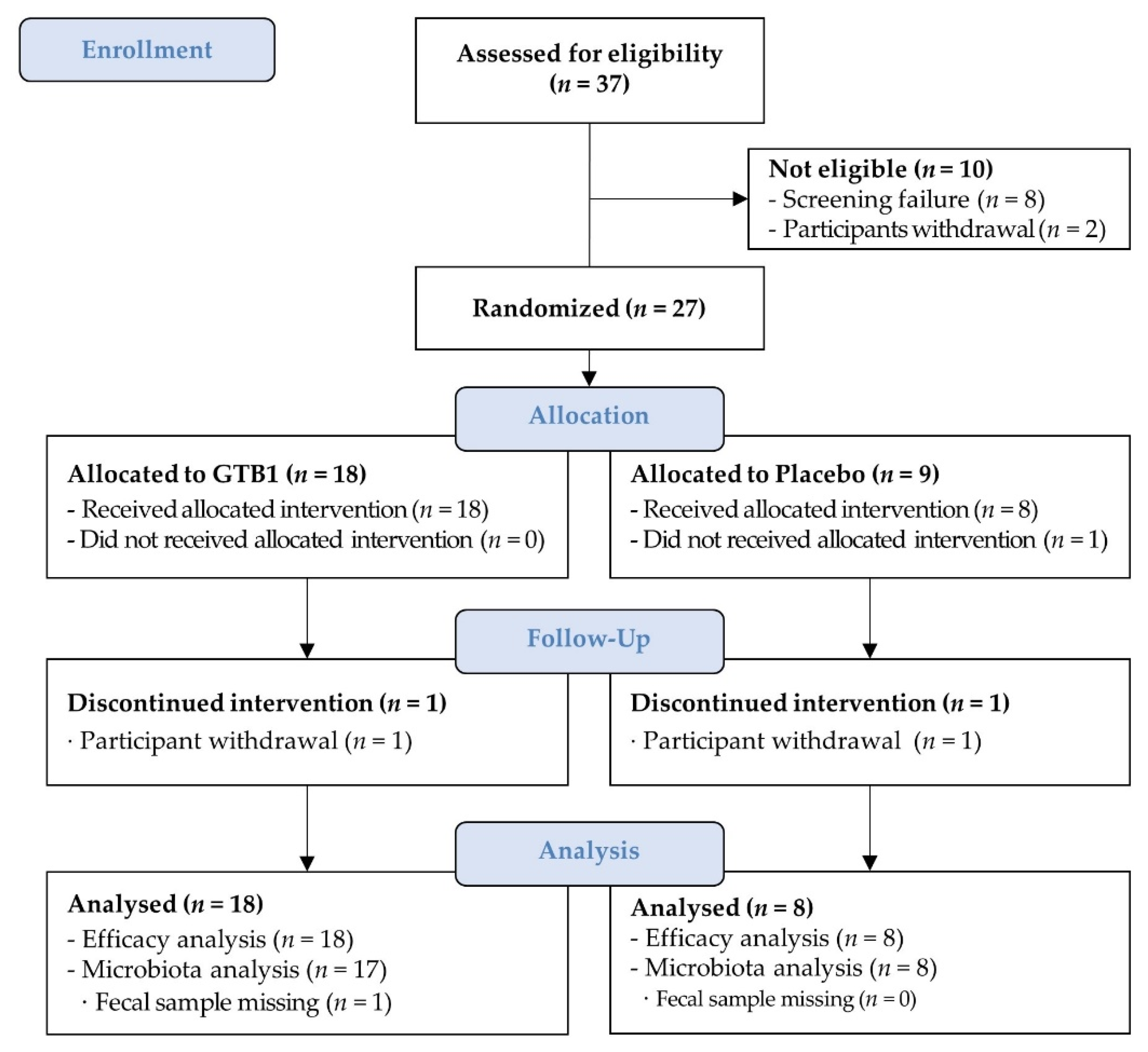
3.1. Study Participants
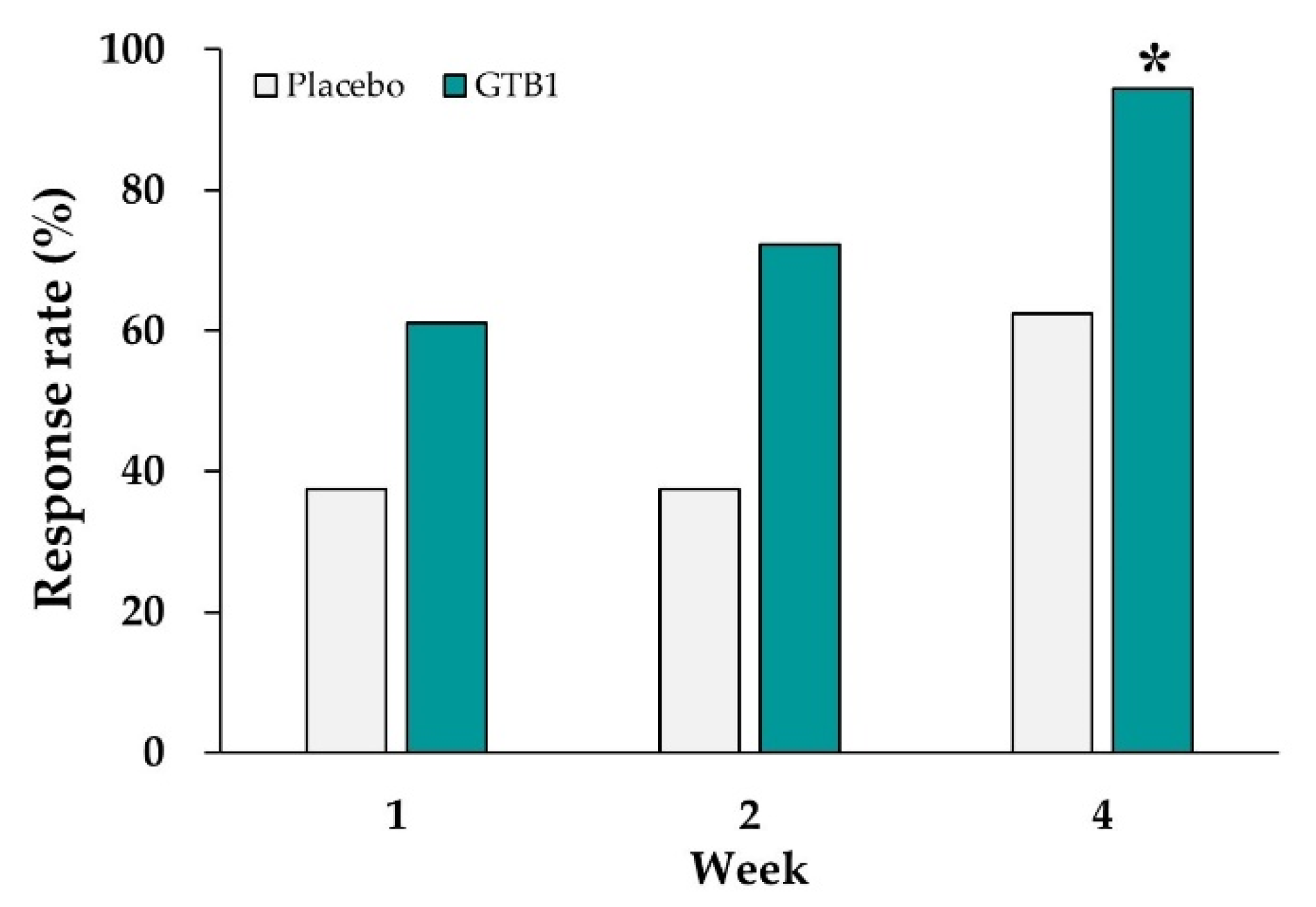
3.2. Global Relief of IBS Symptoms
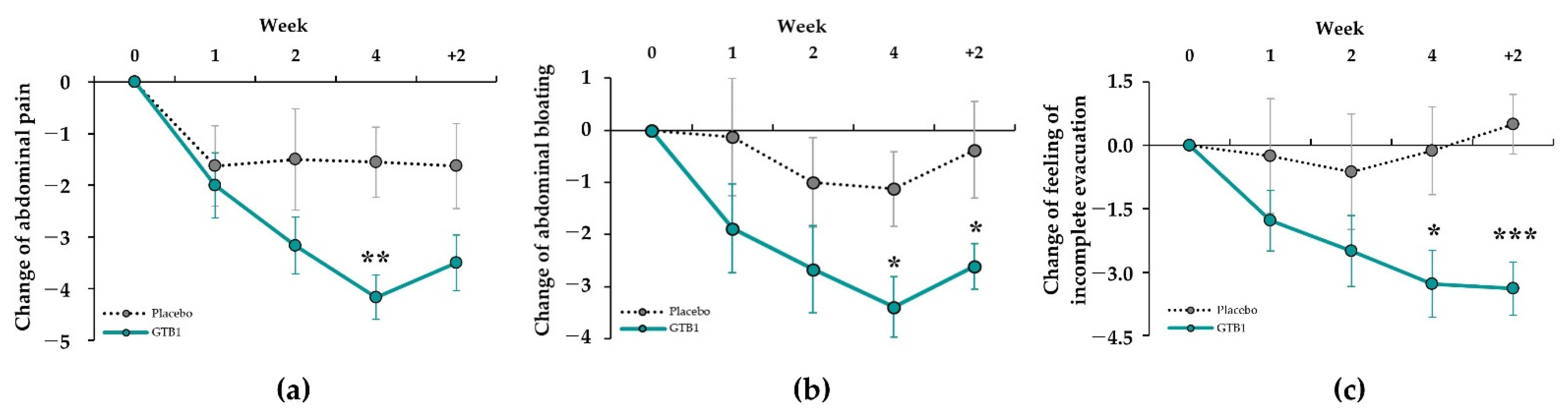
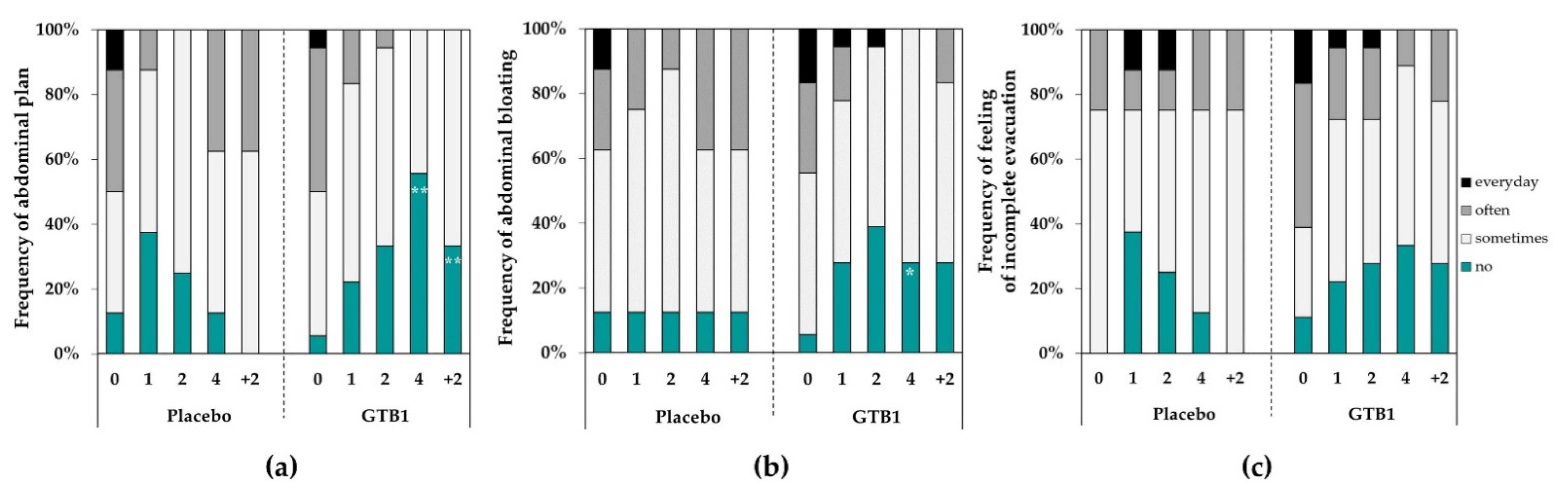
3.3. Intestinal Discomfort Symptoms
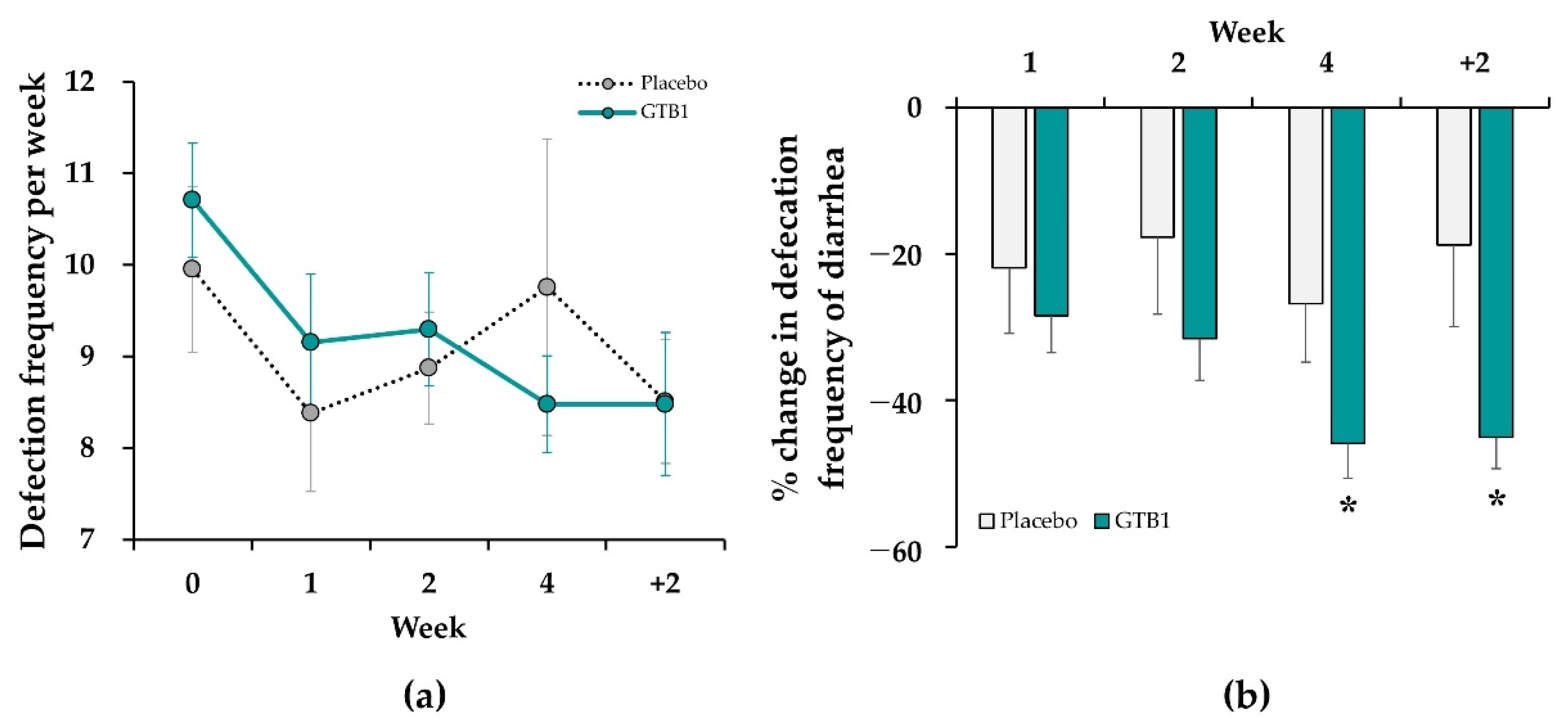
3.4. Bowel Movement
3.5. Satisfaction Assessment
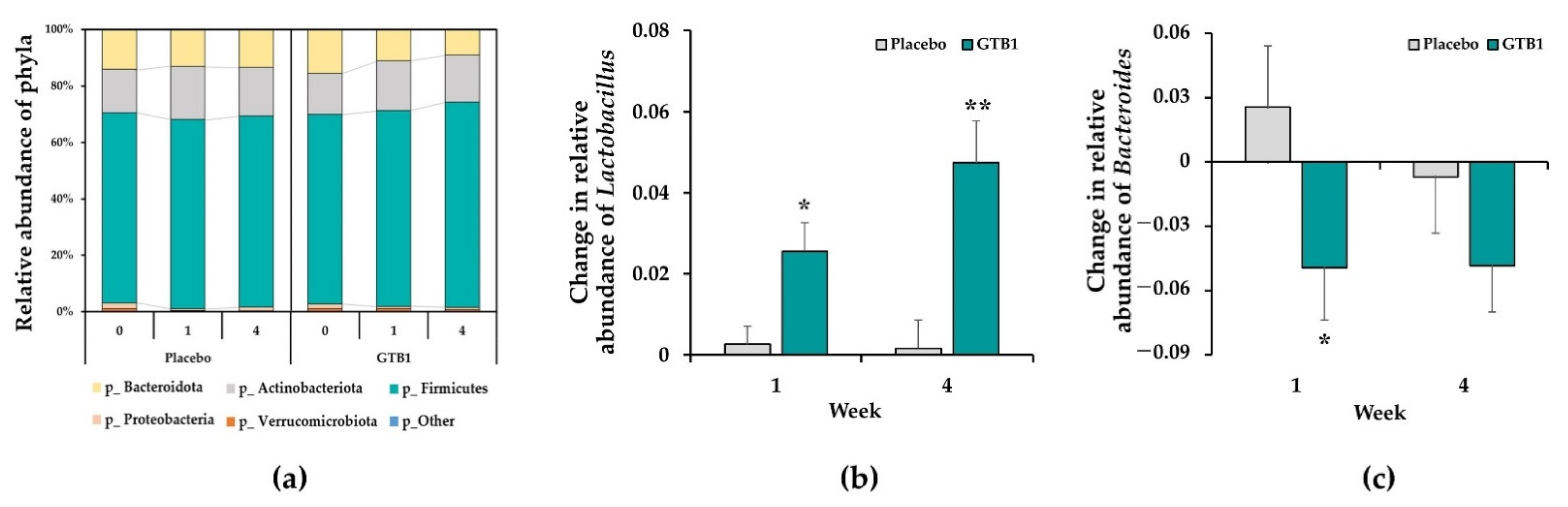
3.6. Fecal Microbiota
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Lovell, R.M.; Ford, A.C. Global prevalence of and risk factors for irritable bowel syndrome: A meta-analysis. Clin. Gastroenterol. Hepatol. 2012, 10, 712–721.e4. [Google Scholar] [CrossRef] [PubMed]
- Han, S.H.; Lee, O.Y.; Bae, S.C.; Lee, S.H.; Chang, Y.K.; Yang, S.Y.; Yoon, B.C.; Choi, H.S.; Hahm, J.S.; Lee, M.H.; et al. Prevalence of irritable bowel syndrome in Korea: Population-based survey using the Rome II criteria. J. Gastroenterol. Hepatol. 2006, 21, 1687–1692. [Google Scholar] [CrossRef] [PubMed]
- Park, K.S.; Ahn, S.H.; Hwang, J.S.; Cho, K.B.; Chung, W.J.; Jang, B.K.; Kang, Y.N.; Kwon, J.H.; Kim, Y.H. A survey about irritable bowel syndrome in South Korea: Prevalence and observable organic abnormalities in IBS patients. Dig. Dis. Sci. 2008, 53, 704–711. [Google Scholar] [CrossRef] [PubMed]
- Canavan, C.; West, J.; Card, T. The epidemiology of irritable bowel syndrome. Clin. Epidemiol. 2014, 6, 71–80. [Google Scholar]
- Enck, P.; Aziz, Q.; Barbara, G.; Farmer, A.D.; Fukudo, S.; Mayer, E.A.; Niesler, B.; Quigley, E.M.; Rajilić-Stojanović, M.; Schemann, M.; et al. Irritable bowel syndrome. Nat. Rev. Dis. Primers 2016, 24, 16014. [Google Scholar] [CrossRef] [Green Version]
- Rey, E.; García-Alonso, M.O.; Moreno-Ortega, M.; Alvarez-Sanchez, A.; Diaz-Rubio, M. Determinants of quality of life in irritable bowel syndrome. J. Clin. Gastroenterol. 2008, 42, 1003–1009. [Google Scholar] [CrossRef]
- Lacy, B.E.; Patel, N.K. Rome Criteria and a Diagnostic Approach to Irritable Bowel Syndrome. J. Clin. Med. 2017, 6, 99. [Google Scholar] [CrossRef]
- Mearin, F.; Lacy, B.E.; Chang, L.; Chey, W.D.; Lembo, A.J.; Simren, M.; Spiller, R. Bowel Disorders. Gastroenterology 2016, 150, 1393–1407. [Google Scholar]
- Drossman, D.A.; Hasler, W.L. Rome IV-Functional GI Disorders: Disorders of Gut-Brain Interaction. Gastroenterology 2016, 150, 1257–1261. [Google Scholar] [CrossRef]
- Hungin, A.P.; Chang, L.; Locke, G.R.; Dennis, E.H.; Barghout, V. Irritable bowel syndrome in the United States: Prevalence, symptom patterns and impact. Aliment. Pharm. 2005, 21, 1365–1375. [Google Scholar] [CrossRef]
- Yang, F.; Wu, J.; Ye, N.Y.; Miu, J.; Yan, J.; Liu, L.N.; Ye, B. Association of Fecal Microbiota with Irritable Bowel Syndrome-Diarrhea and Effect of Traditional Chinese Medicine for Its Management. Gastroenterol. Res. Pract. 2021, 2021, 7035557. [Google Scholar] [CrossRef] [PubMed]
- Fukudo, S.; Hahm, K.B.; Zhu, Q.; Sollano, J.D.; Rani, A.A.; Syam, A.F.; Kachintorn, U.; Suzuki, H.; Kamiya, T.; Joh, T.; et al. Survey of Clinical Practice for Irritable Bowel Syndrome in East Asian Countries. Digestion 2015, 91, 99–109. [Google Scholar] [CrossRef] [PubMed]
- Park, M.J.; Lee, K.S.; Jeong, J.S.; Kim, J.H.; Choi, J.A.; Shin, G.S.; Choe, M.A. The Prevalence, Subtypes and Risk Factors of Irritable Bowel Syndrome by ROME III among Korean University Students. J. Korean Biol. Nurs. Sci. 2011, 13, 61–71. [Google Scholar]
- Ford, A.C.; Sperber, A.D.; Corsetti, M.; Camilleri, M. Irritable bowel syndrome. Lancet 2020, 396, 1675–1688. [Google Scholar] [CrossRef]
- Ohland, C.L.; Macnaughton, W.K. Probiotic bacteria and intestinal epithelial barrier function. Am. J. Physiol. Gastrointest. Liver Physiol. 2010, 298, G807–G819. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lee, B.J.; Bak, Y.T. Irritable bowel syndrome, gut microbiota and probiotics. J. Neurogastroenterol. Motil. 2011, 17, 252–266. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ducrotté, P.; Sawant, P.; Jayanthi, V. Lactobacillus plantarum 299v (DSM 9843) improves symptoms of irritable bowel syndrome. World J. Gastroenterol. 2012, 18, 4012–4018. [Google Scholar] [CrossRef]
- Skrzydło-Radomańska, B.; Prozorow-Król, B.; Cichoż-Lach, H.; Majsiak, E.; Bierła, J.B.; Kanarek, E.; Sowińska, A.; Cukrowska, B. The effectiveness and safety of multi-strain probiotic preparation in patients with diarrhea-predominant irritable bowel syndrome: A randomized controlled study. Nutrients 2021, 13, 756. [Google Scholar] [CrossRef]
- Skrzydło-Radomańska, B.; Prozorow-Król, B.; Cichoż-Lach, H.; Majsiak, E.; Bierła, J.B.; Kosikowski, W.; Szczerbiński, M.; Gantzel, J.; Cukrowska, B. The Effectiveness of Synbiotic Preparation Containing Lactobacillus and Bifidobacterium Probiotic Strains and Short Chain Fructooligosaccharides in Patients with Diarrhea Predominant Irritable Bowel Syndrome-A Randomized Double-Blind, Placebo-Controlled Study. Nutrients 2020, 12, 1999. [Google Scholar]
- Yang, B.; Yue, Y.; Chen, Y.; Ding, M.; Li, B.; Wang, L.; Wang, Q.; Stanton, C.; Ross, R.P.; Zhao, J.; et al. Lactobacillus plantarum CCFM1143 Alleviates Chronic Diarrhea via Inflammation Regulation and Gut Microbiota Modulation: A Double-Blind, Randomized, Placebo-Controlled Study. Front. Immunol. 2021, 12, 746585. [Google Scholar] [CrossRef]
- Oh, J.H.; Jang, Y.S.; Kang, D.; Chang, D.K.; Min, Y.W. Efficacy and Safety of New Lactobacilli Probiotics for Unconstipated Irritable Bowel Syndrome: A Randomized, Double-Blind, Placebo-Controlled Trial. Nutrients 2019, 11, 2887. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Arellano, K.; Vazquez, J.; Park, H.; Lim, J.; Ji, Y.; Kang, H.J.; Cho, D.; Jeong, H.W.; Holzapfel, W.H. Safety Evaluation and Whole-Genome Annotation of Lactobacillus plantarum Strains from Different Sources with Special Focus on Isolates from Green Tea. Probiotics Antimicrob. Proteins 2020, 12, 1057–1070. [Google Scholar] [CrossRef] [PubMed]
- Park, H.; Cho, D.; Huang, E.; Seo, J.Y.; Kim, W.G.; Todorov, S.D.; Ji, Y.; Holzapfel, W.H. Amelioration of Alcohol Induced Gastric Ulcers Through the Administration of Lactobacillus plantarum APSulloc 331261 Isolated from Green Tea. Front. Microbiol. 2020, 11, 420. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Liang, D.; Longgui, N.; Guoqiang, X. Efficacy of different probiotic protocols in irritable bowel syndrome: A network meta-analysis. Medicine 2019, 98, e16068. [Google Scholar] [CrossRef]
- Thomas, S.G. Irritable bowel syndrome and mirtazapine. Am. J. Psychiatry 2000, 157, 1341–1342. [Google Scholar] [CrossRef]
- Blake, M.R.; Raker, J.M.; Whelan, K. Validity and reliability of the Bristol Stool Form Scale in healthy adults and patients with diarrhoea-predominant irritable bowel syndrome. Aliment. Pharm. 2016, 44, 693–703. [Google Scholar] [CrossRef] [Green Version]
- Gordon, S.; Ameen, V.; Bagby, B.; Shahan, B.; Jhingran, P.; Carter, E. Validation of irritable bowel syndrome Global Improvement Scale: An integrated symptom end point for assessing treatment efficacy. Dig. Dis. Sci. 2003, 48, 1317–1323. [Google Scholar] [CrossRef]
- Dong, Y.; Baumeister, D.; Berens, S.; Eich, W.; Tesarz, J. High Rates of Non-Response Across Treatment Attempts in Chronic Irritable Bowel Syndrome: Results from a Follow-Up Study in Tertiary Care. Front. Psychiatry 2019, 10, 714. [Google Scholar] [CrossRef]
- Hurst, H.; Bolton, J. Assessing the clinical significance of change scores recorded on subjective outcome measures. J. Manip. Physiol. 2004, 27, 26–35. [Google Scholar] [CrossRef]
- Singh, R.; Zogg, H.; Wei, L.; Bartlett, A.; Ghoshal, U.C.; Rajender, S.; Ro, S. Gut Microbial Dysbiosis in the Pathogenesis of Gastrointestinal Dysmotility and Metabolic Disorders. J. Neurogastroenterol. Motil. 2021, 27, 19–34. [Google Scholar] [CrossRef]
- Barbara, G.; Barbaro, M.R.; Fuschi, D.; Palombo, M.; Falangone, F.; Cremon, C.; Marasco, G.; Stanghellini, V. Inflammatory and Microbiota-Related Regulation of the Intestinal Epithelial Barrier. Front. Nutr. 2021, 8, 718356. [Google Scholar] [CrossRef] [PubMed]
- Bischoff, S.C.; Barbara, G.; Buurman, W.; Ockhuizen, T.; Schulzke, J.D.; Serino, M.; Tilg, H.; Watson, A.; Wells, J.M. Intestinal permeability—A new target for disease prevention and therapy. BMC Gastroenterol. 2014, 14, 189. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Schachtsiek, M.; Hammes, W.P.; Hertel, C. Characterization of lactobacillus coryniformis dsm 20001t surface protein cpf mediating coaggregation with and aggregation among pathogens. Appl. Environ. Microbiol. 2004, 70, 7078–7085. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Oelschlaeger, T.A. Mechanisms of probiotic actions—A review. Int. J. Med. Microbiol. 2010, 300, 57–62. [Google Scholar] [CrossRef] [PubMed]
- Isolauri, E.; Sutas, Y.; Kankaanpaa, P.; Arvilommi, H.; Salminen, S. Probiotics: Effects on immunity. Am. J. Clin. Nutr. 2001, 73, 444S–450S. [Google Scholar] [CrossRef] [Green Version]
- Barbaro, M.R.; Di Sabatino, A.; Cremon, C.; Giuffrida, P.; Fiorentino, M.; Altimari, A.; Bellacosa, L.; Stanghellini, V.; Barbara, G. Interferon-gamma is increased in the gut of patients with irritable bowel syndrome and modulates serotonin metabolism. Am. J. Physiol. Gastrointest. Liver Physiol. 2016, 310, G439–G447. [Google Scholar] [CrossRef] [Green Version]
- Liebregts, T.; Adam, B.; Bredack, C.; Röth, A.; Heinzel, S.; Lester, S.; Downie-Doyle, S.; Smith, E.; Drew, P.; Talley, N.J.; et al. Immune activation in patients with irritable bowel syndrome. Gastroenterology 2007, 132, 913–920. [Google Scholar] [CrossRef]
- Waugh, A.W.G.; Foshaug, R.; Macfarlane, S.; Doyle, J.S.G.; Churchill, T.A.; Sydora, B.C.; Fedorak, R.N. Effect of Lactobacillus plantarum 299v treatment in an animal model of irritable bowel syndrome. Microb. Ecol. Health Dis. 2009, 21, 33–37. [Google Scholar]
- Yue, Y.; He, Z.; Zhou, Y.; Ross, R.P.; Stanton, C.; Zhao, J.; Zhang, H.; Yang, B.; Chen, W. Lactobacillus plantarum relieves diarrhea caused by enterotoxin-producing Escherichia coli through inflammation modulation and gut microbiota regulation. Food Funct. 2020, 11, 10362–10374. [Google Scholar] [CrossRef]
- Zhang, M.; Hao, X.; Aziz, T.; Zhang, J.; Yang, Z. Exopolysaccharides from Lactobacillus plantarum YW11 improve immune response and ameliorate inflammatory bowel disease symptoms. Acta Biochim. Pol. 2020, 67, 485–493. [Google Scholar]
- Collado, M.C.; Gueimonde, M.; Salminem, S. Probiotics in adhesion of pathogens: Mechanisms of action. In Bioactive Foods in Promoting Health: Probiotics and Prebiotics, 1st ed.; Watson, R.R., Preedy, V.R., Eds.; Academic Press: Cambridge, MA, USA; Elsevier: London, UK, 2010; pp. 353–370. [Google Scholar]
- Mack, D.R.; Ahrne, S.; Hyde, L.; Wei, S.; Hollingsworth, M.A. Extracellular MUC3 mucin secretion follows adherence of Lactobacillus strains to intestinal epithelial cells in vitro. Gut 2003, 52, 827–833. [Google Scholar] [CrossRef] [Green Version]
- Mattar, A.F.; Teitelbaum, D.H.; Drongowski, R.A.; Yongyi, F.; Harmon, C.M.; Coran, A.G. Probiotics up-regulate MUC-2 mucin gene expression in a Caco-2 cell-culture model. Pediatr. Surg. Int. 2002, 18, 586–590. [Google Scholar] [PubMed]
- Quigley, E.M.M. Microbiota-Brain-Gut Axis and Neurodegenerative Diseases. Curr. Neurol. Neurosci. Rep. 2017, 17, 94. [Google Scholar] [CrossRef] [PubMed]
- Wullt, M.; Johansson Hagslätt, M.L.; Odenholt, I.; Berggren, A. Lactobacillus plantarum 299v enhances the concentrations of fecal short-chain fatty acids in patients with recurrent clostridium difficile-associated diarrhea. Dig. Dis. Sci. 2007, 52, 2082–2086. [Google Scholar] [CrossRef] [PubMed]
- Spiller, R.; Aziz, Q.; Creed, F.; Emmanuel, A.; Houghton, L.; Hungin, P.; Jones, R.; Kumar, D.; Rubin, G.; Trudgill, N.; et al. Guidelines on the irritable bowel syndrome: Mechanisms and practical management. Gut 2007, 56, 1770–1798. [Google Scholar] [CrossRef] [Green Version]
- Ford, A.C.; Talley, N.J. Irritable bowel syndrome. BMJ 2012, 345, e5836. [Google Scholar] [CrossRef] [Green Version]
- Lacy, B.E.; Moreau, J.C. Diarrhea-predominant irritable bowel syndrome: Diagnosis, etiology, and new treatment considerations. J. Am. Assoc. Nurse Pract. 2016, 28, 393–404. [Google Scholar] [CrossRef]
- Bearcroft, C.P.; Perrett, D.; Farthing, M.J. Postprandial plasma 5-hydroxytryptamine in diarrhoea predominant irritable bowel syndrome: A pilot study. Gut 1998, 42, 42–46. [Google Scholar] [CrossRef] [Green Version]
- Singh, P.; Staller, K.; Barshop, K.; Dai, E.; Newman, J.; Yoon, S.; Castel, S.; Kuo, B. Patients with irritable bowel syndrome-diarrhea have lower disease-specific quality of life than irritable bowel syndrome-constipation. World J. Gastroenterol. 2015, 21, 8103–8109. [Google Scholar] [CrossRef]
- Gu, Y.; Zhou, G.; Huang, S.; Wang, B.; Cao, H. The potential role of gut mycobiome in irritable bowel syndrome. Front. Microbiol. 2019, 10, 1894. [Google Scholar] [CrossRef]
- De Palma, G.; Lynch, M.D.; Lu, J.; Dang, V.T.; Deng, Y.; Jury, J.; Umeh, G.; Miranda, P.M.; Pigrau Pastor, M.; Sidani, S.; et al. Transplantation of fecal microbiota from patients with irritable bowel syndrome alters gut function and behavior in recipient mice. Sci. Transl. Med. 2017, 9, eaaf6397. [Google Scholar] [CrossRef] [PubMed]
- Pittayanon, R.; Lau, J.T.; Yuan, Y.; Leontiadis, G.I.; Tse, F.; Surette, M.; Moayyedi, P. Gut Microbiota in Patients with Irritable Bowel Syndrome-A Systematic Review. Gastroenterology 2019, 157, 97–108. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Carroll, I.M.; Ringel-Kulka, T.; Keku, T.O.; Chang, Y.H.; Packey, C.D.; Sartor, R.B.; Ringel, Y. Molecular analysis of the luminal- and mucosal-associated intestinal microbiota in diarrhea-predominant irritable bowel syndrome. Am. J. Physiol. Gastrointest. Liver Physiol. 2011, 301, G799–G807. [Google Scholar] [CrossRef]
- Liu, H.N.; Wu, H.; Chen, Y.Z.; Chen, Y.J.; Shen, X.Z.; Liu, T.T. Altered molecular signature of intestinal microbiota in irritable bowel syndrome patients compared with healthy controls: A systematic review and meta-analysis. Dig. Liver Dis. 2017, 49, 331–337. [Google Scholar] [CrossRef] [PubMed]
- Zhuang, X.; Tian, Z.; Li, L.; Zeng, Z.; Chen, M.; Xiong, L. Fecal Microbiota Alterations Associated with Diarrhea-Predominant Irritable Bowel Syndrome. Front. Microbiol. 2018, 9, 1600. [Google Scholar] [CrossRef] [PubMed]
- Kumar, M.; Dhaka, P.; Vijay, D.; Vergis, J.; Mohan, V.; Kumar, A.; Kurkure, N.V.; Barbuddhe, S.B.; Malik, S.V.; Rawool, D.B. Antimicrobial effects of Lactobacillus plantarum and Lactobacillus acidophilus against multidrug-resistant enteroaggregative Escherichia coli. Int. J. Antimicrob. Agents 2016, 48, 265–270. [Google Scholar] [CrossRef] [PubMed]
- Bermudez-Brito, M.; Plaza-Díaz, J.; Muñoz-Quezada, S.; Gómez-Llorente, C.; Gil, A. Probiotic mechanisms of action. Ann. Nutr. Metab. 2012, 61, 160–174. [Google Scholar] [CrossRef]
- Flint, H.J.; Duncan, S.H.; Scott, K.P.; Louis, P. Links between diet, gut microbiota composition and gut metabolism. Proc. Nutr. Soc. 2015, 74, 13–22. [Google Scholar] [CrossRef] [Green Version]
- Rajilić-Stojanović, M.; Biagi, E.; Heilig, H.G.; Kajander, K.; Kekkonen, R.A.; Tims, S.; de Vos, W.M. Global and deep molecular analysis of microbiota signatures in fecal samples from patients with irritable bowel syndrome. Gastroenterology 2011, 141, 1792–1801. [Google Scholar] [CrossRef]
- Verbeke, K.A.; Boesmans, L.; Boets, E. Modulating the microbiota in inflammatory bowel diseases: Prebiotics, probiotics or faecal transplantation? Proc. Nutr. Soc. 2014, 73, 490–497. [Google Scholar] [CrossRef] [Green Version]
- Liderot, K.; Ratcliffe, P.; Lüthje, P.; Thidholm, E.; Özenci, V. Microbiological Diagnosis of Eggerthella Lenta Blood Culture Isolates in a Swedish Tertiary Hospital: Rapid Identification and Antimicrobial Susceptibility Profile. Anaerobe 2016, 38, 21–24. [Google Scholar] [CrossRef] [PubMed]
- Arthur, J.C.; Perez-Chanona, E.; Mühlbauer, M.; Tomkovic, S.; Uronis, J.M.; Fan, T.J.; Campbell, B.J.; Abujamel, T.; Dogan, B.; Rogers, A.B.; et al. Intestinal inflammation targets cancer-inducing activity of the microbiota. Science 2012, 338, 120–123. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wick, E.C.; Sears, C.L. Bacteroides Spp. and Diarrhea. Curr. Opin. Infect Dis. 2010, 23, 470–474. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mariat, D.; Firmesse, O.; Levenez, F.; Guimarăes, V.; Sokol, H.; Doré, J.; Corthier, G.; Furet, J.P. The Firmicutes/Bacteroidetes ratio of the human microbiota changes with age. BMC Microbiol. 2009, 9, 123. [Google Scholar] [CrossRef]
- Lynch, S.V.; Pedersen, O. The Human Intestinal Microbiome in Health and Disease. N. Engl. J. Med. 2016, 375, 2369–2379. [Google Scholar] [CrossRef] [Green Version]
- Stojanov, S.; Berlec, A.; Štrukelj, B. The Influence of Probiotics on the Firmicutes/Bacteroidetes Ratio in the Treatment of Obesity and Inflammatory Bowel disease. Microorganisms 2020, 8, 1715. [Google Scholar] [CrossRef]
- Karlsson, C.; Ahrné, S.; Molin, G.; Berggren, A.; Palmquist, I.; Fredrikson, G.N.; Jeppsson, B. Probiotic therapy to men with incipient arteriosclerosis initiates increased bacterial diversity in colon: A randomized controlled trial. Atherosclerosis 2010, 208, 228–233. [Google Scholar] [CrossRef] [Green Version]
- Staudacher, H.M.; Whelan, K. The low FODMAP diet: Recent advances in understanding its mechanisms and efficacy in IBS. Gut 2017, 66, 1517–1527. [Google Scholar] [CrossRef] [Green Version]
- Nordström, E.A.; Teixeira, C.; Montelius, C.; Jeppsson, B.; Larsson, N. Lactiplantibacillus plantarum 299v (LP299V®): Three decades of research. Benef. Microbes 2021, 12, 441–465. [Google Scholar] [CrossRef]

| Placebo (n = 8) | GTB1 (n = 18) | p-Value 1 | ||
|---|---|---|---|---|
| Mean (SD) or n (%) | Mean (SD) or n (%) | |||
| Age (years) | 39.38 (3.16) | 39.84 (6.44) | 0.848 | |
| Female gender, n(%) | 6 (75.00%) | 12 (66.67%) | 0.568 | |
| BMI (kg/m2) | 24.40 (3.84) | 24.00 (3.44) | 0.797 | |
| Systolic blood pressure (mmHg) | 108.88 (7.16) | 110.94 (7.63) | 0.522 | |
| Diastolic blood pressure (mmHg) | 81.13 (5.74) | 79.28 (6.00) | 0.470 | |
| Rome IV | Related to defecation | 7 (87.50%) | 16 (84.21%) | 0.834 |
| Change in frequency of stool | 6 (75.00%) | 14 (73.68%) | 0.946 | |
| Change in form of stool | 8 (100.00%) | 18 (94.74%) | 0.527 | |
| Intestinal discomfort | Abdominal pain | 5.25 (1.39) | 5.83 (1.58) | 0.378 |
| Abdominal bloating | 4.75 (3.11) | 5.50 (2.87) | 0.571 | |
| Feeling of incomplete evacuation | 4.00 (2.88) | 6.17 (2.62) | 0.093 | |
| Defecation condition | Defecation frequency(/week) | 9.95 (2.56) | 10.71 (2.64) | 0.504 |
| BSFS types 6 & 7 (%) | 63.22 (21.40) | 69.07 (19.14) | 0.494 | |
| Abdominal Pain | Abdominal Bloating | Feeling of Incomplete Evacuation | ||||
|---|---|---|---|---|---|---|
| Placebo | GTB1 | Placebo | GTB1 | Placebo | GTB1 | |
| Week 0 | 5.25 ± 1.39 | 5.83 ± 1.58 | 4.75 ± 3.11 | 5.50 ± 2.87 | 4.00 ± 2.88 | 6.17 ± 2.62 |
| Week 1 | 3.63 ± 2.45 | 3.83 ± 2.73 ## | 4.63 ± 2.50 | 3.61 ± 2.52 # | 3.75 ± 1.91 | 4.39 ± 2.43 # |
| Week 2 | 3.75 ± 1.98 | 2.67 ± 1.75 ### | 3.75 ± 1.98 | 2.83 ± 2.12 ## | 3.38 ± 2.39 | 3.67 ± 2.63 ## |
| Week 4 | 3.75 ± 2.60 | 1.67 ± 1.08 ###,** | 3.63 ± 3.07 | 2.11 ± 1.49 ###,* | 3.88 ± 2.30 | 2.89 ± 2.27 ##,* |
| Week 4 + 2 | 3.63 ± 2.39 | 2.33 ± 1.81 ### | 4.38 ± 3.07 | 2.89 ± 2.05 ###,* | 4.50 ± 2.56 | 2.78 ± 2.34 ###,*** |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jung, K.; Kim, A.; Lee, J.-H.; Cho, D.; Seo, J.; Jung, E.S.; Kang, H.-j.; Roh, J.; Kim, W. Effect of Oral Intake of Lactiplantibacillus plantarum APsulloc 331261 (GTB1TM) on Diarrhea-Predominant Irritable Bowel Syndrome: A Randomized, Double-Blind, Placebo-Controlled Study. Nutrients 2022, 14, 2015. https://doi.org/10.3390/nu14102015
Jung K, Kim A, Lee J-H, Cho D, Seo J, Jung ES, Kang H-j, Roh J, Kim W. Effect of Oral Intake of Lactiplantibacillus plantarum APsulloc 331261 (GTB1TM) on Diarrhea-Predominant Irritable Bowel Syndrome: A Randomized, Double-Blind, Placebo-Controlled Study. Nutrients. 2022; 14(10):2015. https://doi.org/10.3390/nu14102015
Chicago/Turabian StyleJung, Kyoungmi, Areum Kim, Ji-Hae Lee, Donghyun Cho, Juyeon Seo, Eun Sung Jung, Hye-ji Kang, Jonghwa Roh, and Wangi Kim. 2022. "Effect of Oral Intake of Lactiplantibacillus plantarum APsulloc 331261 (GTB1TM) on Diarrhea-Predominant Irritable Bowel Syndrome: A Randomized, Double-Blind, Placebo-Controlled Study" Nutrients 14, no. 10: 2015. https://doi.org/10.3390/nu14102015
APA StyleJung, K., Kim, A., Lee, J.-H., Cho, D., Seo, J., Jung, E. S., Kang, H.-j., Roh, J., & Kim, W. (2022). Effect of Oral Intake of Lactiplantibacillus plantarum APsulloc 331261 (GTB1TM) on Diarrhea-Predominant Irritable Bowel Syndrome: A Randomized, Double-Blind, Placebo-Controlled Study. Nutrients, 14(10), 2015. https://doi.org/10.3390/nu14102015






