Methods for Assessing Willingness to Try and Vegetable Consumption among Children in Indigenous Early Childcare Settings: The FRESH Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. FRESH Study Overview
2.2. Recruitment and Study Population
2.3. Demographics, Food Security and Biometric Measures
2.4. Selection of Test Vegetables
2.5. Weighed Plate Waste
2.6. Direct Observation of Willingness-to-Try Measures
2.7. Child Food Neophobia
2.8. Validation of FR-WTT Observational Method
2.9. Statistical Analyses
3. Results
3.1. Participant Demographics, Food Security and Biometric Measures
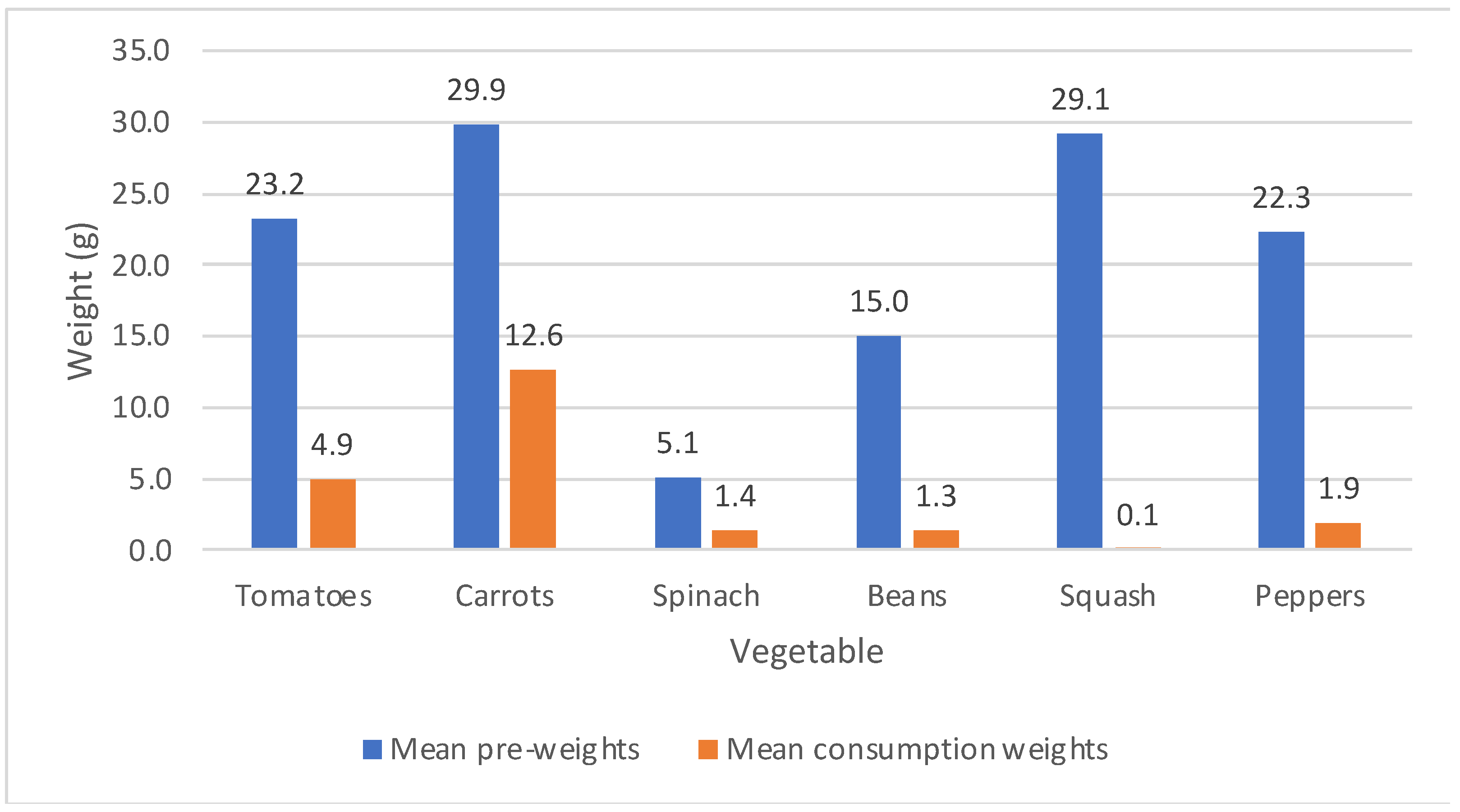
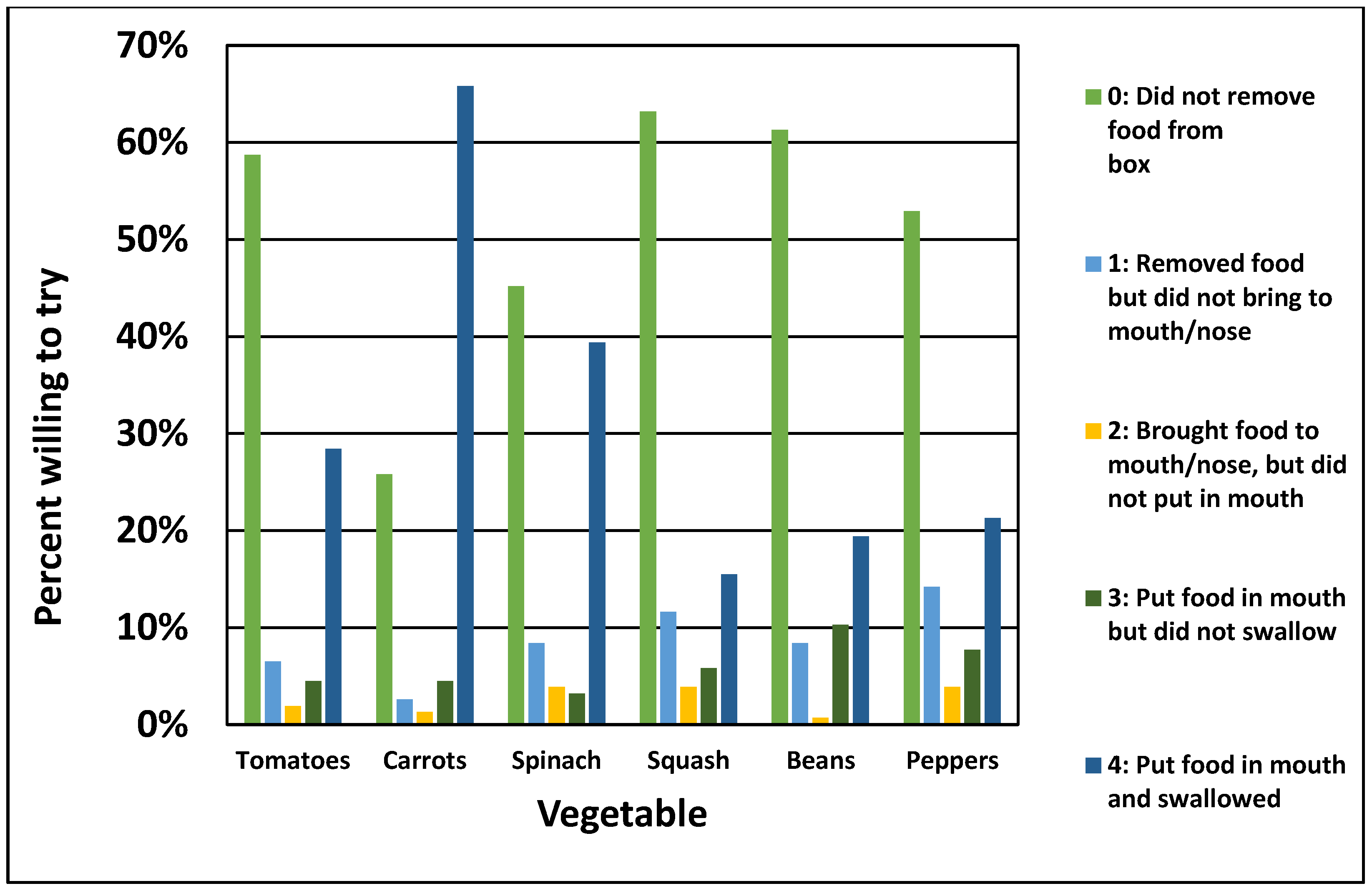
3.2. Description of Weighted Plate Waste, FR-WTT and CFNS
3.3. Criterion and Convergent Validity of Willingness-to-Try Method
3.4. Sensitivity Analysis by BMI and Food Security
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Birch, L.L. Development of food preferences. Annu. Rev. Nutr. 1999, 19, 41–62. [Google Scholar] [CrossRef] [Green Version]
- Birch, L.L. Development of food acceptance patterns in the first years of life. Proc. Nutr. Soc. 1998, 57, 617–624. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Birch, L.L.; Fisher, J.O. Development of eating behaviors among children and adolescents. Pediatrics 1998, 101, 539–549. [Google Scholar] [CrossRef] [PubMed]
- Mennella, J.A.; Bobowski, N.K. The sweetness and bitterness of childhood: Insights from basic research on taste preferences. Physiol. Behav. 2015, 152, 502–507. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Addessi, E.; Galloway, A.T.; Visalberghi, E.; Birch, L.L. Specific social influences on the acceptance of novel foods in 2–5-year-old children. Appetite 2005, 45, 264–271. [Google Scholar] [CrossRef] [PubMed]
- Cooke, L.; Wardle, J.; Gibson, E.L. Relationship between parental report of food neophobia and everyday food consumption in 2–6-year-old children. Appetite 2003, 41, 205–206. [Google Scholar] [CrossRef]
- Lafraire, J.; Rioux, C.; Giboreau, A.; Picard, D. Food rejections in children: Cognitive and social/environmental factors involved in food neophobia and picky/fussy eating behavior. Appetite 2016, 96, 347–357. [Google Scholar] [CrossRef]
- Falciglia, G.A.; Couch, S.C.; Gribble, L.S.; Pabst, S.M.; Frank, R. Food neophobia in childhood affects dietary variety. J. Am. Diet. Assoc. 2000, 100, 1474–1481. [Google Scholar] [CrossRef]
- Birch, L.L.; McPhee, L.; Shoba, B.C.; Pirok, E.; Steinberg, L. What kind of exposure reduces children’s food neophobia? Looking vs. tasting. Appetite 1987, 9, 171–178. [Google Scholar] [CrossRef]
- Wardle, J.; Cooke, L.J.; Gibson, E.L.; Sapochnik, M.; Sheiham, A.; Lawson, M. Increasing children’s acceptance of vegetables; a randomized trial of parent-led exposure. Appetite 2003, 40, 155–162. [Google Scholar] [CrossRef]
- Wardle, J.; Carnell, S.; Cooke, L. Parental control over feeding and children’s fruit and vegetable intake: How are they related? J. Am. Diet. Assoc. 2005, 105, 227–232. [Google Scholar] [CrossRef]
- Corcoran, L.; Steinley, K. Early Childhood Program Participation, From the National Household Education Surveys Program of 2016 (NCES 2017-101.REV); National Center for Education Statistics, Institute of Education Sciences, U.S. Department of Education: Washington, DC, USA, 2019. Available online: http://nces.ed.gov/pubsearch (accessed on 11 November 2021).
- Benjamin Neelon, S.E.; Briley, M.E. Position of the American Dietetic Association: Benchmarks for nutrition in child care. J. Am. Diet. Assoc. 2011, 111, 607–615. [Google Scholar] [CrossRef]
- Robson, S.M.; Khoury, J.C.; Kalkwarf, H.J.; Copeland, K. Dietary intake of children attending full-time child care: What are they eating away from the child-care center? J. Acad. Nutr. Diet. 2015, 115, 1472–1478. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sisson, S.B.; Kiger, A.C.; Anundson, K.C.; Rasbold, A.H.; Krampe, M.; Campbell, J.; DeGrace, B.; Hoffman, L. Differences in preschool-age children’s dietary intake between meals consumed at childcare and at home. Prev. Med. Rep. 2017, 6, 33–37. [Google Scholar] [CrossRef]
- Larson, N.; Story, M. Barriers to Equity in Nutritional Health for U.S. Children and Adolescents: A Review of the Literature. Curr. Nutr. Rep. 2015, 4, 102–110. [Google Scholar] [CrossRef]
- Ward, D.S.; Welker, E.; Choate, A.; Henderson, K.E.; Lott, M.; Tovar, A.; Wilson, A.; Sallis, J.F. Strength of obesity prevention interventions in early care and education settings: A systematic review. Prev. Med. 2017, 95, S37–S52. [Google Scholar] [CrossRef] [PubMed]
- Livingstone, M.B.; Robson, P.J.; Wallace, J.M. Issues in dietary intake assessment of children and adolescents. Br. J. Nutr. 2004, 92 (Suppl 2), S213–S222. [Google Scholar] [CrossRef]
- Magarey, A.; Watson, J.; Golley, R.K.; Burrows, T.; Sutherland, R.; McNaughton, S.A.; Denney-Wilson, E.; Campbell, K.; Collins, C. Assessing dietary intake in children and adolescents: Considerations and recommendations for obesity research. Int. J. Pediatr. Obes. 2011, 6, 2–11. [Google Scholar] [CrossRef] [PubMed]
- Baranowski, T. 24-Hour Recall and Diet Record Methods. In Nutritional Epidemiology; Willett, W.C., Ed.; Oxford University Press: New York, NY, USA, 2013; pp. 50–69. [Google Scholar]
- National Cancer Institute. Dietary Assessment Primer, Principles Underlying Recommendations. Available online: https://dietassessmentprimer.cancer.gov/approach/principles.html (accessed on 16 December 2019).
- Thompson, F.E.; Byers, T. Dietary assessment resource manual. J. Nutr. 1994, 124, 2245s–2317s. [Google Scholar] [CrossRef]
- Institute of Medicine Committee on Dietary Risk Assessment in the WIC Program. Dietary Risk Assessment in the WIC Program. In Food-Based Assessment of Dietary Intake; National Academies Press: Washington, DC, USA, 2002. [Google Scholar]
- Hollar, D.; Paxton-Aiken, A.; Fleming, P. Exploratory validation of the Fruit and Vegetable Neophobia Instrument among third-to fifth-grade students. Appetite 2013, 60, 226–230. [Google Scholar] [CrossRef]
- Loewen, R.; Pliner, P. The Food Situations Questionnaire: A measure of children’s willingness to try novel foods in stimulating and non-stimulating situations. Appetite 2000, 35, 239–250. [Google Scholar] [CrossRef]
- Thomson, J.L.; McCabe-Sellers, B.J.; Strickland, E.; Lovera, D.; Nuss, H.J.; Yadrick, K.; Duke, S.; Bogle, M.L. Development and evaluation of WillTry. An instrument for measuring children’s willingness to try fruits and vegetables. Appetite 2010, 54, 465–472. [Google Scholar] [CrossRef] [PubMed]
- Kaiser, L.L.; Schneider, C.; Mendoza, C.; George, G.; Neelon, M.; Roche, B.; Ginsburg, D. Development and use of an evaluation tool for taste-testing activities by school-aged children. J. Acad. Nutr. Diet. 2012, 112, 2028–2034. [Google Scholar] [CrossRef] [PubMed]
- Farfan-Ramirez, L.; Diemoz, L.; Gong, E.J.; Lagura, M.A. Curriculum intervention in preschool children: Nutrition Matters! J. Nutr. Educ. Behav. 2011, 43, S162–S165. [Google Scholar] [CrossRef]
- USDA Economic Research Service. U.S. Adult Food Security Survey Module: Three-Stage Design, with Screeners; U.S. Department of Agriculture: Honolulu, HI, USA, 2012.
- Wetherill, M.S.; Bourque, E.E.; Taniguchi, T.; Love, C.V.; Sisk, M.; Jernigan, V.B.B. Development of a Tribally-led Gardening Curriculum for Indigenous Preschool Children: The FRESH Study. J. Nutr. Educ. Behav. 2021, 53, 991–995. [Google Scholar] [CrossRef] [PubMed]
- Bollella, M.C.; Boccia, L.A.; Nicklas, T.A.; Lefkowitz, K.B.; Pittman, B.P.; Zang, E.A.; Williams, C.L. Assessing dietary intake in preschool children: The healthy start project-New York. Nutr. Res. 1999, 19, 37–48. [Google Scholar] [CrossRef]
- Cooke, L.; Carnell, S.; Wardle, J. Food neophobia and mealtime food consumption in 4–5 year old children. Int. J. Behav. Nutr. Phys. Act. 2006, 3, 14. [Google Scholar] [CrossRef] [Green Version]
- Pliner, P.; Hobden, K. Development of a scale to measure the trait of food neophobia in humans. Appetite 1992, 19, 105–120. [Google Scholar] [CrossRef]
- Johnson, S.L. Developmental and Environmental Influences on Young Children’s Vegetable Preferences and Consumption. Adv. Nutr. 2016, 7, 220S–231S. [Google Scholar] [CrossRef] [Green Version]
- Kuczmarski, R.J.; Ogden, C.L.; Guo, S.S.; Grummer-Strawn, L.M.; Flegal, K.M.; Mei, Z.; Wei, R.; Curtin, L.R.; Roche, A.F.; Johnson, C.L. 2000 CDC Growth Charts for the United States: Methods and development. Vital Health Stat. 2002, 11, 1–190. [Google Scholar] [PubMed]
- Saavedra, J.M.; Deming, D.; Dattilo, A.; Reidy, K. Lessons from the feeding infants and toddlers study in North America: What children eat, and implications for obesity prevention. Ann. Nutr. Metab. 2013, 62 (Suppl 3), 27–36. [Google Scholar] [CrossRef] [PubMed]
- Field, A.E.; Gillman, M.W.; Rosner, B.; Rockett, H.R.; Colditz, G.A. Association between fruit and vegetable intake and change in body mass index among a large sample of children and adolescents in the United States. Int. J. Obes. Relat. Metab. Disord. 2003, 27, 821–826. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Miller, P.; Moore, R.H.; Kral, T.V. Children’s daily fruit and vegetable intake: Associations with maternal intake and child weight status. J. Nutr. Educ. Behav. 2011, 43, 396–400. [Google Scholar] [CrossRef]
- Dave, J.M.; Evans, A.E.; Saunders, R.P.; Watkins, K.W.; Pfeiffer, K.A. Associations among food insecurity, acculturation, demographic factors, and fruit and vegetable intake at home in Hispanic children. J. Am. Diet. Assoc. 2009, 109, 697–701. [Google Scholar] [CrossRef]
- Fram, M.S.; Ritchie, L.D.; Rosen, N.; Frongillo, E.A. Child experience of food insecurity is associated with child diet and physical activity. J. Nutr. 2015, 145, 499–504. [Google Scholar] [CrossRef] [Green Version]
- Eicher-Miller, H.A.; Zhao, Y. Evidence for the age-specific relationship of food insecurity and key dietary outcomes among US children and adolescents. Nutr. Res. Rev. 2018, 31, 98–113. [Google Scholar] [CrossRef]
- Canter, K.S.; Roberts, M.C.; Davis, A.M. The role of health behaviors and food insecurity in predicting fruit and vegetable intake in low-income children. Child. Health Care 2017, 46, 131–150. [Google Scholar] [CrossRef]
- Dovey, T.M.; Staples, P.A.; Gibson, E.L.; Halford, J.C. Food neophobia and ’picky/fussy’ eating in children: A review. Appetite 2008, 50, 181–193. [Google Scholar] [CrossRef]
- Ahern, S.M.; Caton, S.J.; Blundell-Birtill, P.; Hetherington, M.M. The effects of repeated exposure and variety on vegetable intake in pre-school children. Appetite 2019, 132, 37–43. [Google Scholar] [CrossRef]
- Caton, S.J.; Ahern, S.M.; Remy, E.; Nicklaus, S.; Blundell, P.; Hetherington, M.M. Repetition counts: Repeated exposure increases intake of a novel vegetable in UK pre-school children compared to flavour-flavour and flavour-nutrient learning. Br. J. Nutr. 2013, 109, 2089–2097. [Google Scholar] [CrossRef] [Green Version]
- Olsho, L.E.; Klerman, J.A.; Ritchie, L.; Wakimoto, P.; Webb, K.L.; Bartlett, S. Increasing Child Fruit and Vegetable Intake: Findings from the US Department of Agriculture Fresh Fruit and Vegetable Program. J. Acad. Nutr. Diet. 2015, 115, 1283–1290. [Google Scholar] [CrossRef] [PubMed]
| Characteristic | Number (%) a |
|---|---|
| Child characteristics | |
| Age (M, SD) | 4.7 (0.8) |
| Sex | |
| Male | 75 (46) |
| Female | 87 (56) |
| Race/ethnicity | |
| Native American | 115 (71) |
| White/Caucasian only | 37 (23) |
| Other | 10 (6) |
| Body Mass Index Percentile | |
| Above 95% (Obese) | 28 (18) |
| 85–95% (Overweight) | 28 (18) |
| Below 85% (Normal or underweight) | 103 (65) |
| Child food neophobia score (M, SD) | 14.0 (5.0) |
| Adult and household characteristics | |
| Caregiver highest education | |
| Some high school/high school degree/GED | 70 (44) |
| Technical/Vocational/Associate’s degree | 50 (32) |
| Bachelor’s/Post-graduate degree | 38 (24) |
| Caregiver employment | |
| Employed b | 114 (72) |
| Not employed | 14 (9) |
| Retired/student/homemaker | 30 (19) |
| Annual household income | |
| USD 20,000 and under | 45 (29) |
| USD 20,001–35,000 | 36 (23) |
| USD 35,001–50,000 | 32 (21) |
| Over USD 50,000 | 43 (28) |
| Household food security | |
| Very low food security | 12 (8) |
| Low food security | 47 (31) |
| Marginal food security | 27 (18) |
| High food security | 65 (43) |
| Child food security | |
| Low or very low child food security | 25 (17) |
| High or marginal child food security | 126 (83) |
| Vegetable FR-WTT | n | Mean Consumption in Grams 1 (SD) | p Value |
|---|---|---|---|
| Tomatoes FR-WTT = 4 | 33 | 7.6 (7.6) | <0.001 |
| Tomatoes FR-WTT = 0, 1, 2, 3 | 131 | 0.4 (0.9) | |
| Carrots FR-WTT = 4 | 108 | 18.9 (11.4) | <0.001 |
| Carrots FR-WTT = 0, 1, 2, 3 | 56 | 0.4 (1.0) | |
| Spinach FR-WTT = 4 | 63 | 2.7 (2.2) | <0.001 |
| Spinach FR-WTT = 0, 1, 2, 3 | 101 | 0.6 (0.9) | |
| Beans FR-WTT = 4 | 31 | 4.9 (5.0) | <0.001 |
| Beans FR-WTT = 0, 1, 2, 3 | 133 | 0.5 (1.1) | |
| Squash FR-WTT = 4 | 25 | 4.1 (7.7) | <0.001 |
| Squash FR-WTT = 0, 1, 2, 3 | 139 | −0.6 (1.1) | |
| Peppers FR-WTT = 4 | 33 | 7.6 (7.6) | <0.001 |
| Peppers FR-WTT = 0, 1, 2, 3 | 131 | 0.5 (0.9) |
| Vegetable | Correlation a between FR-WTT and CFNS Scales | |
|---|---|---|
| Coefficient | p Value | |
| Tomatoes | −0.2786 | <0.01 |
| Carrots | −0.3004 | <0.01 |
| Spinach | −0.1762 | 0.03 |
| Beans | −0.0986 | 0.24 |
| Squash | −0.2454 | <0.01 |
| Peppers | −0.3259 | <0.001 |
| Total | −0.3268 | <0.001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wetherill, M.S.; Williams, M.B.; Reese, J.; Taniguchi, T.; Sisson, S.B.; Malek-Lasater, A.D.; Love, C.V.; Jernigan, V.B.B. Methods for Assessing Willingness to Try and Vegetable Consumption among Children in Indigenous Early Childcare Settings: The FRESH Study. Nutrients 2022, 14, 58. https://doi.org/10.3390/nu14010058
Wetherill MS, Williams MB, Reese J, Taniguchi T, Sisson SB, Malek-Lasater AD, Love CV, Jernigan VBB. Methods for Assessing Willingness to Try and Vegetable Consumption among Children in Indigenous Early Childcare Settings: The FRESH Study. Nutrients. 2022; 14(1):58. https://doi.org/10.3390/nu14010058
Chicago/Turabian StyleWetherill, Marianna S., Mary B. Williams, Jessica Reese, Tori Taniguchi, Susan B. Sisson, Adrien D. Malek-Lasater, Charlotte V. Love, and Valarie Blue Bird Jernigan. 2022. "Methods for Assessing Willingness to Try and Vegetable Consumption among Children in Indigenous Early Childcare Settings: The FRESH Study" Nutrients 14, no. 1: 58. https://doi.org/10.3390/nu14010058
APA StyleWetherill, M. S., Williams, M. B., Reese, J., Taniguchi, T., Sisson, S. B., Malek-Lasater, A. D., Love, C. V., & Jernigan, V. B. B. (2022). Methods for Assessing Willingness to Try and Vegetable Consumption among Children in Indigenous Early Childcare Settings: The FRESH Study. Nutrients, 14(1), 58. https://doi.org/10.3390/nu14010058







