Effect of the Lifestyle, Exercise, and Nutrition (LEAN) Study on Long-Term Weight Loss Maintenance in Women with Breast Cancer
Abstract
:1. Introduction
2. Materials and Methods
3. Results
3.1. Baseline Characteristics of Study Participants
3.2. Post-Intervention Weight Change
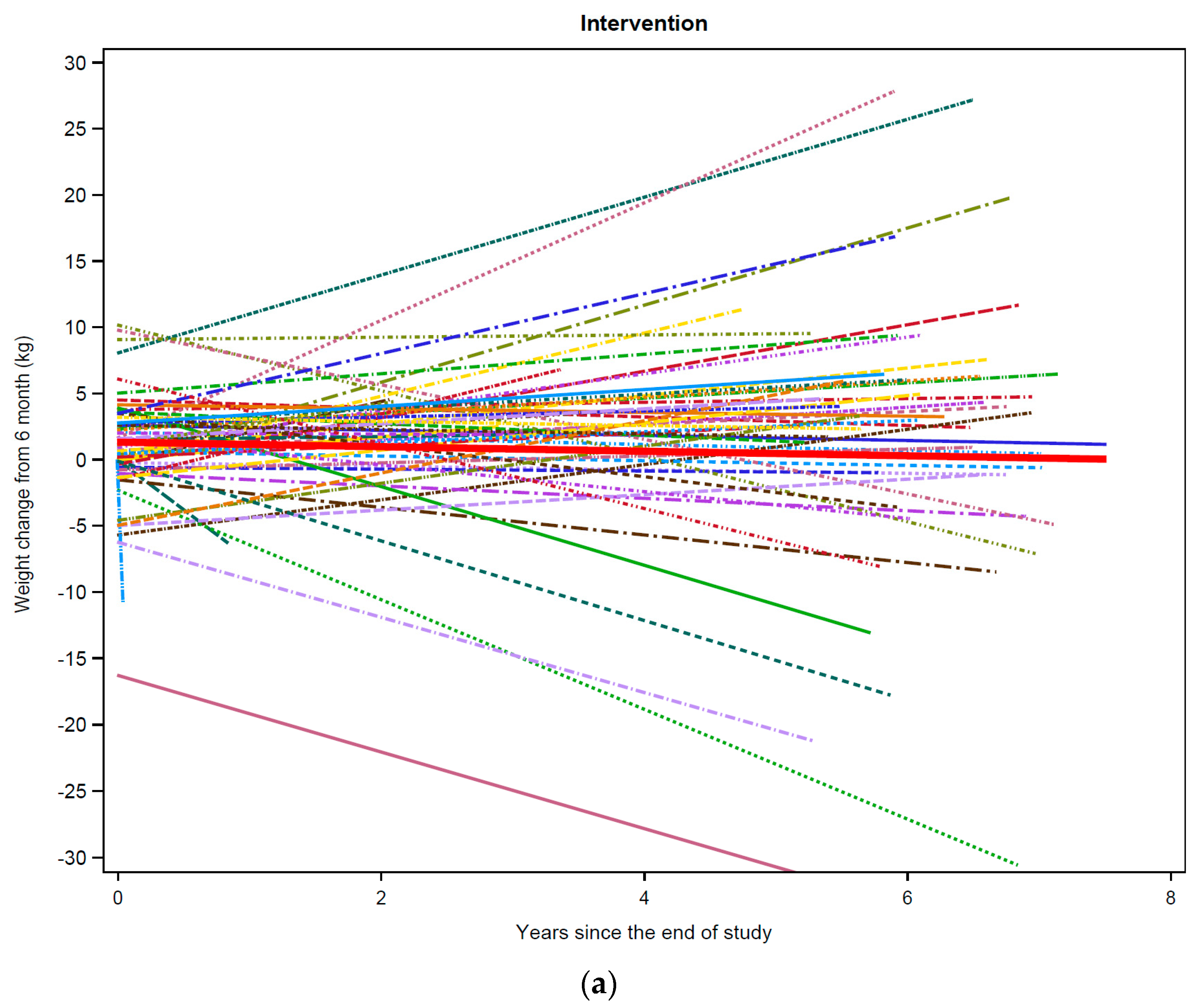
3.3. Post-Intervention Weight Change by Weight Change during LEAN
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- Siegel, R.L.; Miller, K.D.; Fuchs, H.E.; Jemal, A. Cancer Statistics. CA Cancer J. Clin. 2021, 71, 7–33. [Google Scholar] [CrossRef]
- Sheng, J.; Sharma, D.; Jerome, G.; Santa-Maria, C.A. Obese Breast Cancer Patients and Survivors: Management Considerations. Oncology 2018, 32, 410–417. [Google Scholar]
- Chan, D.S.M.; Vieira, A.R.; Aune, D.; Bandera, E.V.; Greenwood, D.C.; McTiernan, A.; Rosenblatt, D.N.; Thune, I.; Vieira, R.; Norat, T. Body mass index and survival in women with breast cancer—Systematic literature review and meta-analysis of 82 follow-up studies. Ann. Oncol. 2014, 25, 1901–1914. [Google Scholar] [CrossRef] [PubMed]
- Bradshaw, P.T.; Ibrahim, J.G.; Stevens, J.; Cleveland, R.; Abrahamson, P.E.; Satia, J.A.; Teitelbaum, S.L.; Neugut, A.I.; Gammon, M.D. Postdiagnosis Change in Bodyweight and Survival after Breast Cancer Diagnosis. Epidemiology 2012, 23, 320–327. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Maliniak, M.L.; Patel, A.V.; McCullough, M.L.; Campbell, P.T.; Leach, C.R.; Gapstur, S.M.; Gaudet, M.M. Obesity, physical activity, and breast cancer survival among older breast cancer survivors in the Cancer Prevention Study-II Nutrition Cohort. Breast Cancer Res. Treat. 2018, 167, 133–145. [Google Scholar] [CrossRef]
- Simone, V.; D’Avenia, M.; Argentiero, A.; Felici, C.; Rizzo, F.M.; De Pergola, G.; Silvestris, F. Obesity and Breast Cancer: Molecular Interconnections and Potential Clinical Applications. Oncology 2016, 21, 404–417. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chen, X.; Lu, W.; Gu, K.; Chen, Z.; Zheng, Y.; Zheng, W.; Shu, X.O. Weight Change and Its Correlates Among Breast Cancer Survivors. Nutr. Cancer 2011, 63, 538–548. [Google Scholar] [CrossRef]
- Lucas, A.R.; Levine, B.J.; Avis, N.E. Posttreatment trajectories of physical activity in breast cancer survivors. Cancer 2017, 123, 2773–2780. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Greenlee, H.; Shi, Z.; Molmenti, C.L.S.; Rundle, A.; Tsai, W.Y. Trends in Obesity Prevalence in Adults with a History of Cancer: Results from the US National Health Interview Survey, 1997 to 2014. J. Clin. Oncol. 2016, 34, 3133–3140. [Google Scholar] [CrossRef] [Green Version]
- Mozaffarian, D.; Hao, T.; Rimm, E.B.; Willett, W.C.; Hu, F.B. Changes in Diet and Lifestyle and Long-Term Weight Gain in Women and Men. N. Engl. J. Med. 2011, 364, 2392–2404. [Google Scholar] [CrossRef] [Green Version]
- Malhotra, R.; Ostbye, T.; Riley, C.M.; Finkelstein, E.A. Young adult weight trajectories through midlife by body mass category. Obesity 2013, 21, 1923–1934. [Google Scholar] [CrossRef]
- Vance, V.; Hanning, R.; Mourtzakis, M.; McCargar, L. Weight gain in breast cancer survivors: Prevalence, pattern and health consequences. Obes. Rev. 2010, 12, 282–294. [Google Scholar] [CrossRef] [PubMed]
- Caan, B.J.; Kwan, M.L.; Shu, X.O.; Pierce, J.P.; Patterson, R.E.; Nechuta, S.; Poole, E.M.; Kroenke, C.H.; Weltzien, E.K.; Flatt, S.W.; et al. Weight Change and Survival after Breast Cancer in the After Breast Cancer Pooling Project. Cancer Epidemiol. Biomark. Prev. 2012, 21, 1260–1271. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Playdon, M.C.; Bracken, M.B.; Sanft, T.B.; Ligibel, J.A.; Harrigan, M.; Irwin, M.L. Weight Gain After Breast Cancer Diagnosis and All-Cause Mortality: Systematic Review and Meta-Analysis. J. Natl. Cancer Instig. 2015, 107, djv275. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jiralerspong, S.; Goodwin, P. Obesity and Breast Cancer Prognosis: Evidence, Challenges, and Opportunities. J. Clin. Oncol. 2016, 34, 4203–4216. [Google Scholar] [CrossRef] [PubMed]
- Nyrop, K.A.; Deal, A.M.; Lee, J.T.; Muss, H.B.; Choi, S.K.; Wheless, A.; Carey, L.A.; Shachar, S.S. Weight gain in hormone receptor-positive (HR+) early-stage breast cancer: Is it menopausal status or something else? Breast Cancer Res. Treat. 2018, 167, 235–248. [Google Scholar] [CrossRef] [PubMed]
- Diet, Nutrition, Physical Activity, and Breast Cancer Survivors. 2014. Available online: www.wcrf.org/sites/default/files/Breast-Cancer-Survivors-2014-Report.pdf (accessed on 17 September 2021).
- Runowicz, C.D.; Leach, C.R.; Henry, N.L.; Henry, K.S.; Mackey, H.T.; Cowens-Alvarado, R.L.; Cannady, R.S.; Pratt-Chapman, M.; Edge, S.B.; Jacobs, L.A.; et al. American Cancer Society/American Society of Clinical Oncology Breast Cancer Survivorship Care Guideline. J. Clin. Oncol. 2016, 34, 611–635. [Google Scholar] [CrossRef] [Green Version]
- Blanchard, C.M.; Courneya, K.S.; Stein, K. Cancer survivors’ adherence to lifestyle behavior recommendations and associations with health-related quality of life: Results from the American Cancer Society’s SCS-II. J. Clin. Oncol. 2008, 26, 2198–2204. [Google Scholar] [CrossRef]
- Shaikh, H.; Bradhurst, P.; Ma, L.X.; Tan, S.Y.C.; Egger, S.J.; Vardy, J.L. Body weight management in overweight and obese breast cancer survivors. Cochrane Database Syst. Rev. 2020, 12, Cd012110. [Google Scholar]
- Playdon, M.; Thomas, G.; Sanft, T.; Harrigan, M.; Ligibel, J.A.; Irwin, M.L. Weight Loss Intervention for Breast Cancer Survivors: A Systematic Review. Curr. Breast Cancer Rep. 2013, 5, 222–246. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Greenlee, H.A.; Crew, K.D.; Mata, J.M.; McKinley, P.S.; Rundle, A.G.; Zhang, W.; Liao, Y.; Tsai, W.Y.; Hershman, D.L. A Pilot Randomized Controlled Trial of a Commercial Diet and Exercise Weight Loss Program in Minority Breast Cancer Survivors. Obesity 2012, 21, 65–76. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Harris, M.N.; Swift, D.L.; Myers, V.H.; Earnest, C.; Johannsen, N.M.; Champagne, C.M.; Parker, B.D.; Levy, E.; Cash, K.C.; Church, T.S. Cancer Survival Through Lifestyle Change (CASTLE): A Pilot Study of Weight Loss. Int. J. Behav. Med. 2012, 20, 403–412. [Google Scholar] [CrossRef]
- Rock, C.L.; Flatt, S.W.; Byers, T.E.; Colditz, G.A.; Demark-Wahnefried, W.; Ganz, P.A.; Wolin, K.Y.; Elias, A.; Krontiras, H.; Liu, J.; et al. Results of the Exercise and Nutrition to Enhance Recovery and Good Health for You (ENERGY) Trial: A Behavioral Weight Loss Intervention in Overweight or Obese Breast Cancer Survivors. J. Clin. Oncol. 2015, 33, 3169–3176. [Google Scholar] [CrossRef]
- Harrigan, M.; Cartmel, B.; Loftfield, E.; Sanft, T.; Chagpar, A.B.; Zhou, Y.; Irwin, M.L. Randomized Trial Comparing Telephone Versus In-Person Weight Loss Counseling on Body Composition and Circulating Biomarkers in Women Treated for Breast Cancer: The Lifestyle, Exercise, and Nutrition (LEAN) Study. J. Clin. Oncol. 2016, 34, 669–676. [Google Scholar] [CrossRef]
- Kimokoti, R.W.; Newby, P.; Gona, P.; Zhu, L.; McKeon-O’Malley, C.; Guzman, J.P.; D’Agostino, R.B.; Millen, B.E. Patterns of weight change and progression to overweight and obesity differ in men and women: Implications for research and interventions. Public Health Nutr. 2012, 16, 1463–1475. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chlebowski, R.T.; Reeves, M.M. Weight Loss Randomized Intervention Trials in Female Cancer Survivors. J. Clin. Oncol. 2016, 34, 4238–4248. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nyrop, K.A.; Deal, A.M.; Shachar, S.S.; Park, J.; Choi, S.K.; Lee, J.T.; O’Hare, E.A.; Wheless, A.; Carey, L.A.; Muss, H.B. Weight trajectories in women receiving systemic adjuvant therapy for breast cancer. Breast Cancer Res. Treat. 2019, 179, 709–720. [Google Scholar] [CrossRef] [PubMed]
- Vargas-Meza, A.; Chavez-Tostado, M.; Cortes-Flores, A.; Urias-Valdez, D.; Delgado-Gomez, M.; Morgan-Villela, G.; del Valle, C.J.Z.F.; Jimenez-Tornero, J.; Fuentes-Orozco, C.; García-Rentería, J.; et al. Body weight changes after adjuvant chemotherapy of patients with breast cancer: Results of a Mexican cohort study. Eur. J. Cancer Care 2016, 26, e12550. [Google Scholar] [CrossRef] [PubMed]
- Yeo, W.; Mo, F.K.F.; Pang, E.; Suen, J.J.S.; Koh, J.; Loong, H.H.F.; Yip, C.C.H.; Ng, R.Y.W.; Yip, C.H.W.; Tang, N.L.S.; et al. Profiles of lipids, blood pressure and weight changes among premenopausal Chinese breast cancer patients after adjuvant chemotherapy. BMC Women’s Health 2017, 17, 55. [Google Scholar] [CrossRef] [PubMed]
- Chaudhary, L.; Wen, S.; Xiao, J.; Swisher, A.; Kurian, S.; Abraham, J. Weight change associated with third-generation adjuvant chemotherapy in breast cancer patients. J. Community Support. Oncol. 2014, 12, 355–360. [Google Scholar] [CrossRef]
- Gu, K.; Chen, X.; Zheng, Y.; Chen, Z.; Zheng, W.; Lu, W.; Shu, X.O. Weight change patterns among breast cancer survivors: Results from the Shanghai breast cancer survival study. Cancer Causes Control 2010, 21, 621–629. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gandhi, A.; Copson, E.; Eccles, D.; Durcan, L.; Howell, A.; Morris, J.; Howell, S.; McDiarmid, S.; Sellers, K.; Evans, D.G.; et al. Predictors of weight gain in a cohort of premenopausal early breast cancer patients receiving chemotherapy. Breast 2019, 45, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Zhang, X.-M.; Dou, Q.-L.; Zeng, Y.; Yang, Y.; Cheng, A.S.K.; Zhang, W.-W. Sarcopenia as a predictor of mortality in women with breast cancer: A meta-analysis and systematic review. BMC Cancer 2020, 20, 172. [Google Scholar] [CrossRef] [PubMed]
- Ford, M.E.; Magwood, G.; Brown, E.T.; Cannady, K.D.; Gregoski, M.; Knight, K.; Peterson, L.L.; Kramer, R.; Evans-Knowell, A.; Turner, D.P. Disparities in Obesity, Physical Activity Rates, and Breast Cancer Survival. Adv. Cancer Res. 2017, 133, 23–50. [Google Scholar] [CrossRef] [PubMed]

| Characteristic | Mean (SD) or n (%) | |||
|---|---|---|---|---|
| All n = 92 | Intervention n = 60 | Usual Care n = 32 | p-Value | |
| Age, years | 58.8 (7.3) | 59.4 (7.3) | 57.6 (7.3) | 0.28 |
| BMI a, kg/m2 | 33.1 (6.6) | 32.7 (6.2) | 33.9 (7.6) | 0.42 |
| College graduate | 47 (51%) | 33 (55%) | 14 (44%) | 0.30 |
| Non-Hispanic white | 84 (91%) | 55 (92%) | 29 (91%) | 0.49 |
| Postmenopausal | 75 (82%) | 50 (83%) | 25 (78%) | 0.54 |
| Time from diagnosis to study enrollment, years | 2.7 (1.8) | 2.7 (1.5) | 2.8 (2.2) | 0.72 |
| Post study follow-up time, years | 5.9 (1.9) | 6.0 (1.8) | 5.6 (2.1) | 0.38 |
| Disease Stage | 0.94 | |||
| 0 | 15 (16%) | 9 (15%) | 6 (19%) | |
| I | 48 (52%) | 31 (52%) | 17 (53%) | |
| II | 21 (23%) | 15 (25%) | 6 (19%) | |
| III | 6 (7%) | 4 (7%) | 2 (6%) | |
| Unknown | 2 (2%) | 1 (1%) | 1 (3%) | |
| Treatment after surgery | 0.67 | |||
| None | 14 (15%) | 8 (13%) | 6 (19%) | |
| Radiation only | 34 (37%) | 21 (35%) | 13 (41%) | |
| Chemotherapy only | 17 (18%) | 13 (22%) | 4 (13%) | |
| Radiation and Chemotherapy | 27 (29%) | 18 (30%) | 9 (28%) | |
| Weight (kg) | ||||
| Baseline | 87.5 (18.1) | 86.1 (16.8) | 90.4 (20.3) | 0.27 |
| Six-month | 84.4 (19.3) | 82.4 (18.0) | 88.3 (21.2) | 0.16 |
| Weight change within study period (kg) | −3.4 (5.3) | −4.3(5.7) | −1.6 (3.7) | 0.009 |
| Yearly Mean Rate of Weight Change (kg) | SE b | 95% CI c | p-Value | |
|---|---|---|---|---|
| Intervention a (n = 60) | −0.20 | 0.07 | [−0.06, −0.33] | 0.004 |
| Usual care (n = 32) | −0.32 | 0.10 | [−0.12, −0.53] | 0.002 |
| Intervention (n = 60) | Usual Care (n = 32) | Chi-Square p-Value | |||
|---|---|---|---|---|---|
| Overall Weight Change | 0.0005 | ||||
| Weight loss (>1% loss) | 48 (80%) | 16 (50%) | |||
| Weight gain (>1% gain) | 8 (13%) | 7 (22%) | |||
| Weight maintenance (>1% change) | 4 (7%) | 9 (28%) | |||
| Weight Change (kg/yr.) | SE | Lower | Upper | p-Value | |
| Intervention | |||||
| Weight loss during LEAN | −0.09 | 0.04 | −0.15 | −0.02 | 0.02 |
| Weight gain during LEAN | −0.46 | 0.18 | −0.82 | −0.10 | 0.01 |
| Weight maintenance during LEAN | −0.07 | 0.25 | −0.57 | 0.42 | 0.78 |
| Usual Care | |||||
| Weight loss during LEAN | 0.20 | 0.15 | −0.08 | 0.49 | 0.16 |
| Weight gain during LEAN | −1.32 | 0.20 | −1.71 | −0.92 | <0.0001 |
| Weight maintenance during LEAN | −0.15 | 0.25 | −0.64 | 0.34 | 0.54 |
| Intervention vs. Usual=Care Group Comparison | |||||
| Weight loss: intervention vs. usual care | −0.39 | 0.16 | −0.71 | −0.06 | 0.02 |
| Weight gain: intervention vs. usual care | 0.85 | 0.27 | 0.32 | 1.39 | 0.002 |
| Weight maintenance: intervention vs. usual care | 0.08 | 0.35 | −0.62 | 0.78 | 0.82 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lisevick, A.; Cartmel, B.; Harrigan, M.; Li, F.; Sanft, T.; Fogarasi, M.; Irwin, M.L.; Ferrucci, L.M. Effect of the Lifestyle, Exercise, and Nutrition (LEAN) Study on Long-Term Weight Loss Maintenance in Women with Breast Cancer. Nutrients 2021, 13, 3265. https://doi.org/10.3390/nu13093265
Lisevick A, Cartmel B, Harrigan M, Li F, Sanft T, Fogarasi M, Irwin ML, Ferrucci LM. Effect of the Lifestyle, Exercise, and Nutrition (LEAN) Study on Long-Term Weight Loss Maintenance in Women with Breast Cancer. Nutrients. 2021; 13(9):3265. https://doi.org/10.3390/nu13093265
Chicago/Turabian StyleLisevick, Alexa, Brenda Cartmel, Maura Harrigan, Fangyong Li, Tara Sanft, Miklos Fogarasi, Melinda L. Irwin, and Leah M. Ferrucci. 2021. "Effect of the Lifestyle, Exercise, and Nutrition (LEAN) Study on Long-Term Weight Loss Maintenance in Women with Breast Cancer" Nutrients 13, no. 9: 3265. https://doi.org/10.3390/nu13093265
APA StyleLisevick, A., Cartmel, B., Harrigan, M., Li, F., Sanft, T., Fogarasi, M., Irwin, M. L., & Ferrucci, L. M. (2021). Effect of the Lifestyle, Exercise, and Nutrition (LEAN) Study on Long-Term Weight Loss Maintenance in Women with Breast Cancer. Nutrients, 13(9), 3265. https://doi.org/10.3390/nu13093265






