Prevalence and Types of Non-Nutritive Sweeteners in the New Zealand Food Supply, 2013 and 2019
Abstract
:1. Introduction
2. Materials and Methods
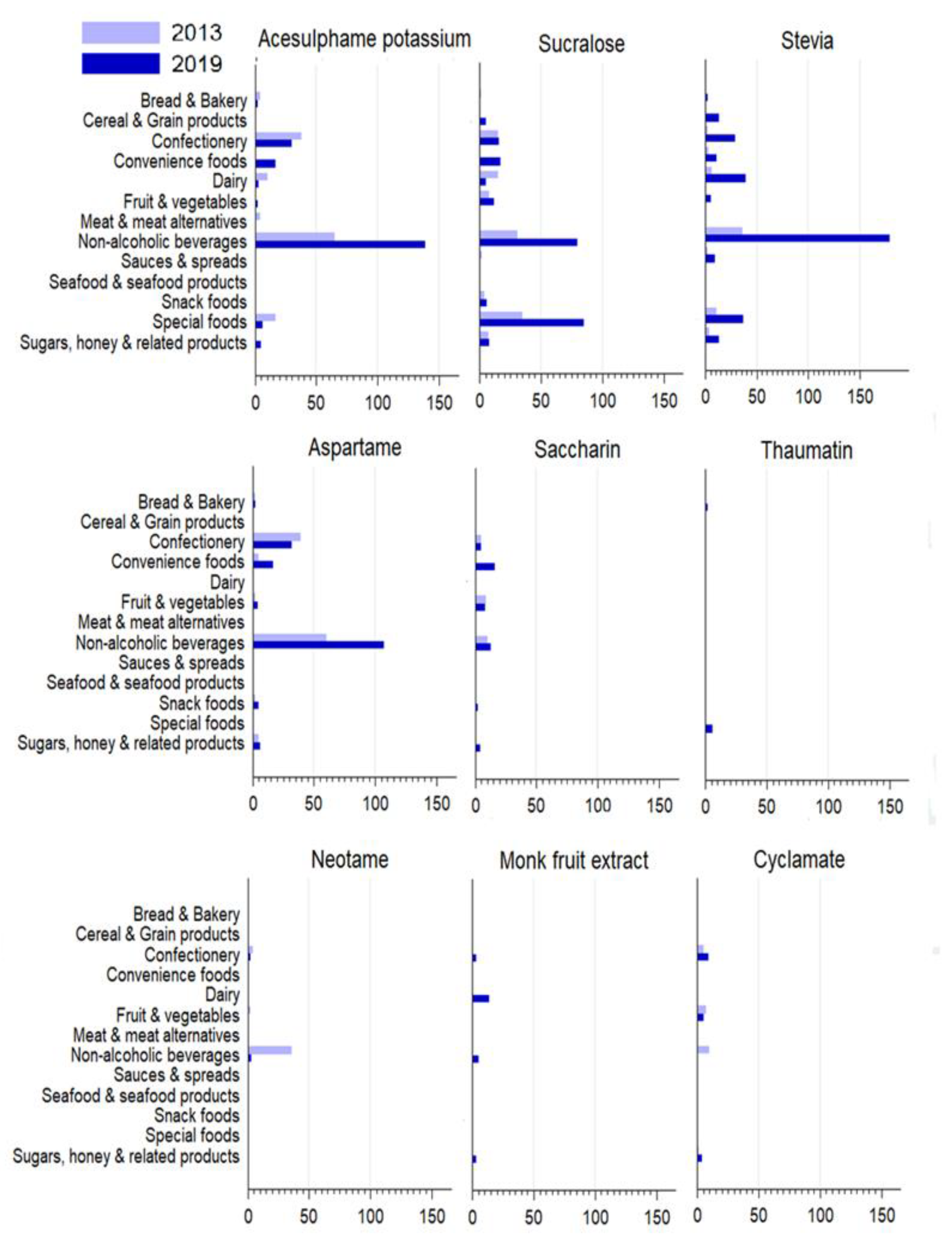
3. Results
4. Discussion
Author Contributions
Funding
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- GBD Risk Factors Collaborators. Global, regional, and national comparative risk assessment of 79 behavioural, environmental and occupational, and metabolic risks or clusters of risks, 1990–2015: A systematic analysis for the Global Burden of Disease Study 2015. Lancet 2016, 388, 1659–1724. [Google Scholar] [CrossRef] [Green Version]
- Ministry of Health. Health and Independence Report 2019: The Director-General of Health’s Annual Report on the State of Public Health; Ministry of Health: Wellington, New Zealand, 2020.
- Te Morenga, L.; Mallard, S.; Mann, J. Dietary sugars and body weight: Systematic review and meta-analyses of randomised controlled trials and cohort studies. Br. Med. J. 2013, 346, e7492. [Google Scholar] [CrossRef] [Green Version]
- Moynihan, P.J.; Kelly, S.A.M. Effect on caries of restricting sugars intake: Systematic review to inform WHO guidelines. J. Dent. Res. 2014, 93, 8–18. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Imamura, F.; O’Connor, L.; Ye, Z.; Mursu, J.; Hayashino, Y.; Bhupathiraju, S.N.; Forouhi, N.G. Consumption of sugar sweetened beverages, artificially sweetened beverages, and fruit juice and incidence of type 2 diabetes: Systematic review, meta-analysis, and estimation of population attributable fraction. Br. Med. J. 2015, 351, h3576. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Te Morenga, L.A.; Howatson, A.J.; Jones, R.M.; Mann, J. Dietary sugars and cardiometabolic risk: Systematic review and meta-analyses of randomized controlled trials of the effects on blood pressure and lipids. Am. J. Clin. Nutr. 2014, 100, 65–79. [Google Scholar] [CrossRef] [Green Version]
- Ministry of Health. Eating and Activity Guidelines for New Zealand Adults: Updated 2020; Ministry of Health: Wellington, New Zealand, 2020.
- World Health Organization. Guideline: Sugars Intake for Adults and Children; World Health Organization: Geneva, Switzerland, 2015. [Google Scholar]
- U.S. Food & Drug Administration. Added Sugars on the New Nutrition Facts Label. Available online: https://www.fda.gov/food/new-nutrition-facts-label/added-sugars-new-nutrition-facts-label (accessed on 7 September 2021).
- Erickson, J.; Slavin, J. Total, Added, and Free Sugars: Are Restrictive Guidelines Science-Based or Achievable? Nutrients 2015, 7, 2866–2878. [Google Scholar] [CrossRef] [PubMed]
- Kibblewhite, R.; Nettleton, A.; McLean, R.; Haszard, J.; Fleming, E.; Kruimer, D.; Te Morenga, L. Estimating free and added sugar intakes in New Zealand. Nutrients 2017, 9, 1292. [Google Scholar] [CrossRef] [Green Version]
- Ministry of Health. A Focus on Nutrition: Key Findings of the 2008/09 New Zealand Adult Nutrition Survey; Ministry of Health: Wellington, New Zealand, 2011.
- Public Health England. Sugar Reduction: The Evidence for Action; Public Health England: London, UK, 2015.
- Popkin, B.M.; Hawkes, C. Sweetening of the global diet, particularly beverages: Patterns, trends, and policy responses. Lancet Diabetes Endocrinol. 2016, 4, 174–186. [Google Scholar] [CrossRef] [Green Version]
- Russell, C.; Grimes, C.; Baker, P.; Sievert, K.; Lawrence, M.A. The drivers, trends and dietary impacts of non-nutritive sweeteners in the food supply: A narrative review. Nutr. Res. Rev. 2020, 1–24. [Google Scholar] [CrossRef] [PubMed]
- Sylvetsky, A.C.; Welsh, J.A.; Brown, R.J.; Vos, M.B. Low-calorie sweetener consumption is increasing in the United States. Am. J. Clin. Nutr. 2012, 96, 640–646. [Google Scholar] [CrossRef] [Green Version]
- Piernas, C.; Ng, S.W.; Popkin, B. Trends in purchases and intake of foods and beverages containing caloric and low-calorie sweeteners over the last decade in the United States. Pediatric Obes. 2013, 8, 294–306. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Coyle, D.H.; Dunford, E.K.; Wu, J.H.; Louie, J.C.Y. The use of non-nutritive and low-calorie sweeteners in 19,915 local and imported pre-packaged foods in Hong Kong. Nutrients 2021, 13, 1861. [Google Scholar] [CrossRef]
- Food Standards Australia New Zealand. Intense Sweeteners. Available online: https://www.foodstandards.gov.au/consumer/additives/pages/sweeteners.aspx (accessed on 10 February 2020).
- Food Standards Australia New Zealand. Dietary Exposure and Intake Assessments. Available online: https://www.foodstandards.govt.nz/science/exposure/pages/dietaryexposureandin4438.aspx (accessed on 6 September 2021).
- Food and Agricultural Organization of the United Nations. Scientific Advice. Available online: http://www.fao.org/food-safety/scientific-advice/en/ (accessed on 6 September 2021).
- Martyn, D.; Darch, M.; Roberts, A.; Lee, H.Y.; Yaqiong Tian, T.; Kaburagi, N.; Belmar, P. Low-/No-Calorie Sweeteners: A Review of Global Intakes. Nutrients 2018, 10, 357. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Grech, A.; Kam, C.O.; Gemming, L.; Rangan, A. Diet-quality and socio-demographic factors associated with non-nutritive sweetener use in the Australian population. Nutrients 2018, 10, 833. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Redruello-Requejo, M.; González-Rodríguez, M.; Samaniego-Vaesken, M.d.L.; Montero-Bravo, A.; Partearroyo, T.; Varela-Moreiras, G. Low- and no-calorie sweetener (LNCS) consumption patterns amongst the Spanish adult population. Nutrients 2021, 13, 1845. [Google Scholar] [CrossRef] [PubMed]
- Dunford, E.K.; Taillie, L.S.; Miles, D.R.; Eyles, H.; Tolentino-Mayo, L.; Ng, S.W. Non-nutritive sweeteners in the packaged food supply—an assessment across 4 countries. Nutrients 2018, 10, 257. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- National Institute for Health Innovation. The Nutritrack Database. Available online: https://diet.auckland.ac.nz/sites/default/files/2019-08/The_Nutritrack_Database.pdf (accessed on 23 April 2021).
- Dunford, E.; Webster, J.; Metzler, A.B.; Czernichow, S.; Mhurchu, C.N.; Wolmarans, P.; Snowdon, W.; L’Abbe, M.; Li, N.; Maulik, P.K. International collaborative project to compare and monitor the nutritional composition of processed foods. Eur. J. Prev. Cardiol. 2012, 19, 1326–1332. [Google Scholar] [CrossRef]
- Health Sponsorship Council. Shopping Behaviour of New Zealand Households; Health Sponsorship Council: Wellington, New Zealand, 2012. [Google Scholar]
- Dunford, E.K.; Miles, D.R.; Ng, S.W.; Popkin, B. Types and Amounts of Nonnutritive Sweeteners Purchased by US Households: A Comparison of 2002 and 2018 Nielsen Homescan Purchases. J. Acad. Nutr. Diet. 2020, 120, 1662–1671.e1610. [Google Scholar] [CrossRef]
- Sylvetsky, A.C.; Rother, K.I. Trends in the consumption of low-calorie sweeteners. Physiol. Behav. 2016, 164, 446–450. [Google Scholar] [CrossRef] [Green Version]
- Bolt-Evensen, K.; Vik, F.N.; Stea, T.H.; Klepp, K.-I.; Bere, E. Consumption of sugar-sweetened beverages and artificially sweetened beverages from childhood to adulthood in relation to socioeconomic status–15 years follow-up in Norway. Int. J. Behav. Nutr. Phys. Act. 2018, 15, 1–9. [Google Scholar] [CrossRef] [Green Version]
- Dhingra, R.; Sullivan, L.; Jacques, P.F.; Wang, T.J.; Fox, C.S.; Meigs, J.B.; D’Agostino, R.B.; Gaziano, J.M.; Vasan, R.S. Soft drink consumption and risk of developing cardiometabolic risk factors and the metabolic syndrome in middle-aged adults in the community. Circulation 2007, 116, 480–488. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Stanley, L. Review of data on the food additive aspartame. EFSA Supporting Publ. 2013, 10, EN-399. [Google Scholar] [CrossRef]
- Hafner, E.; Hribar, M.; Hristov, H.; Kušar, A.; Žmitek, K.; Roe, M.; Pravst, I. Trends in the Use of Low and No-Calorie Sweeteners in Non-Alcoholic Beverages in Slovenia. Foods 2021, 10, 387. [Google Scholar] [CrossRef]
- Edwards, C.H.; Rossi, M.; Corpe, C.P.; Butterworth, P.J.; Ellis, P.R. The role of sugars and sweeteners in food, diet and health: Alternatives for the future. Trends Food Sci. Technol. 2016, 56, 158–166. [Google Scholar] [CrossRef]
- Toews, I.; Lohner, S.; de Gaudry, D.K.; Sommer, H.; Meerpohl, J.J. Association between intake of non-sugar sweeteners and health outcomes: Systematic review and meta-analyses of randomised and non-randomised controlled trials and observational studies. Br. Med. J. 2019, 364, k4718. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- He, F.; Brinsden, H.; MacGregor, G. Salt reduction in the United Kingdom: A successful experiment in public health. J. Hum. Hypertens. 2014, 28, 345–352. [Google Scholar] [CrossRef]
- Wyness, L.A.; Butriss, J.L.; Stanner, S.A. Reducing the population’s sodium intake: The UK Food Standards Agency’s salt reduction programme. Public Health Nutr. 2012, 15, 254–261. [Google Scholar] [CrossRef] [Green Version]
- Public Health England. Sugar Reduction: Report on Progress between 2015 and 2019. Available online: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/984282/Sugar_reduction_progress_report_2015_to_2019-1.pdf (accessed on 8 September 2021).
| Non-Nutritive Sweeteners | Search Terms |
|---|---|
| Acesulphame potassium | 950, acesulphame potassium, acesulphame K, acesulfame potassium, acesulfame K |
| Advantame | 969, advantame |
| Alitame | 956, alitame |
| Aspartame | 951, aspartame |
| Aspartame-acesulphame salt | 962, aspartame-acesulphame salt, aspartame-acesulphame, aspartame-acesulfame salt, aspartame-acesulfame |
| Cyclamate | 952, cyclamate, cyclamic acid, calcium cyclamate, sodium cyclamate |
| Monk fruit extract | monk fruit extract, monk fruit concentrate, luo han guo extract |
| Neotame | 961, neotame |
| Saccharin | 954, saccharin, calcium saccharine, sodium saccharine, potassium saccharine |
| Stevia (steviol glycosides) | 960, steviol glycoside, stevia extract, stevia, rebaudioside |
| Sucralose | 955, sucralose |
| Thaumatin | 957, thaumatin |
| 2013 | 2019 | ||||
|---|---|---|---|---|---|
| Food Category | Number in Category | Number and Percentage of Products Containing at Least One NNS | Number in Category | Number and Percentage of Products Containing at Least One NNS | p Value |
| Bread & bakery | 1499 | 7 (0.5) | 1679 | 8 (0.5) | 1.0 |
| Cereal & cereal products | 1201 | 1 (0.1) | 1485 | 18 (1.2) | <0.001 * |
| Confectionery | 689 | 59 (8.6) | 906 | 82 (9.1) | 0.79 |
| Dairy | 1636 | 23 (1.4) | 1928 | 58 (3) | 0.001 * |
| Edible oils and emulsions | 264 | 0 | 320 | 0 | 0 |
| Eggs | 64 | 0 | 86 | 0 | 0 |
| Convenience foods | 578 | 8 (1.4) | 693 | 24 (3.5) | 0.019 * |
| Fruit & vegetables | 1570 | 19 (1.2) | 1830 | 28 (1.5) | 0.464 |
| Fish & seafood products | 441 | 0 | 414 | 1 (0.2) | 0.484 |
| Meat & meat products | 778 | 4 (0.5) | 953 | 1 (0.1) | 0.181 |
| Non-alcoholic beverages | 1104 | 175 (15.9) | 1505 | 370 (24.6) | <0.001 * |
| Sauces & spreads | 1521 | 6 (0.4) | 1757 | 10 (0.6) | 0.617 |
| Special foods | 161 | 52 (32.3) | 243 | 118 (48.6) | 0.001 * |
| Snack foods | 394 | 6 (1.5) | 547 | 13 (2.4) | 0.482 |
| Sugars, honey, and related products | 253 | 18 (7.1) | 299 | 30 (10) | 0.289 |
| Total | 12,153 | 378 | 14,645 | 761 | |
| Overall prevalence | 3.1 | 5.2 | |||
| 2013 | 2019 | |||
|---|---|---|---|---|
| Non-Nutritive Sweeteners | Number of Products Containing an NNS | Percentage of All Products (n = 12,153) | Number of Products Containing an NNS | Percentage of All Products (n = 14,645) |
| Stevia | 66 | 0.5 | 337 | 2.3 |
| Sucralose | 118 | 1 | 234 | 1.6 |
| Acesulphame-potassium | 139 | 1.1 | 206 | 1.4 |
| Aspartame | 116 | 0.95 | 174 | 1.2 |
| Saccharin | 27 | 0.2 | 49 | 0.3 |
| Cyclamate | 23 | 0.2 | 28 | 0.2 |
| Monk fruit extract | 0 | 0 | 25 | 0.2 |
| Thaumatin | 0 | 0 | 8 | 0.1 |
| Neotame | 43 | 0.4 | 5 | 0 |
| Aspartame-acesulphame salt | 1 | 0 | 1 | 0 |
| Advantame | 0 | 0 | 0 | 0 |
| Alitame | 1 | 0 | 0 | 0 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nunn, R.; Young, L.; Ni Mhurchu, C. Prevalence and Types of Non-Nutritive Sweeteners in the New Zealand Food Supply, 2013 and 2019. Nutrients 2021, 13, 3228. https://doi.org/10.3390/nu13093228
Nunn R, Young L, Ni Mhurchu C. Prevalence and Types of Non-Nutritive Sweeteners in the New Zealand Food Supply, 2013 and 2019. Nutrients. 2021; 13(9):3228. https://doi.org/10.3390/nu13093228
Chicago/Turabian StyleNunn, Rachel, Leanne Young, and Cliona Ni Mhurchu. 2021. "Prevalence and Types of Non-Nutritive Sweeteners in the New Zealand Food Supply, 2013 and 2019" Nutrients 13, no. 9: 3228. https://doi.org/10.3390/nu13093228
APA StyleNunn, R., Young, L., & Ni Mhurchu, C. (2021). Prevalence and Types of Non-Nutritive Sweeteners in the New Zealand Food Supply, 2013 and 2019. Nutrients, 13(9), 3228. https://doi.org/10.3390/nu13093228








