Factors Influencing the Compliance of Pregnant Women with Iron and Folic Acid Supplementation in the Philippines: 2017 Philippine Demographic and Health Survey Analysis
Abstract
1. Introduction
2. Materials and Methods
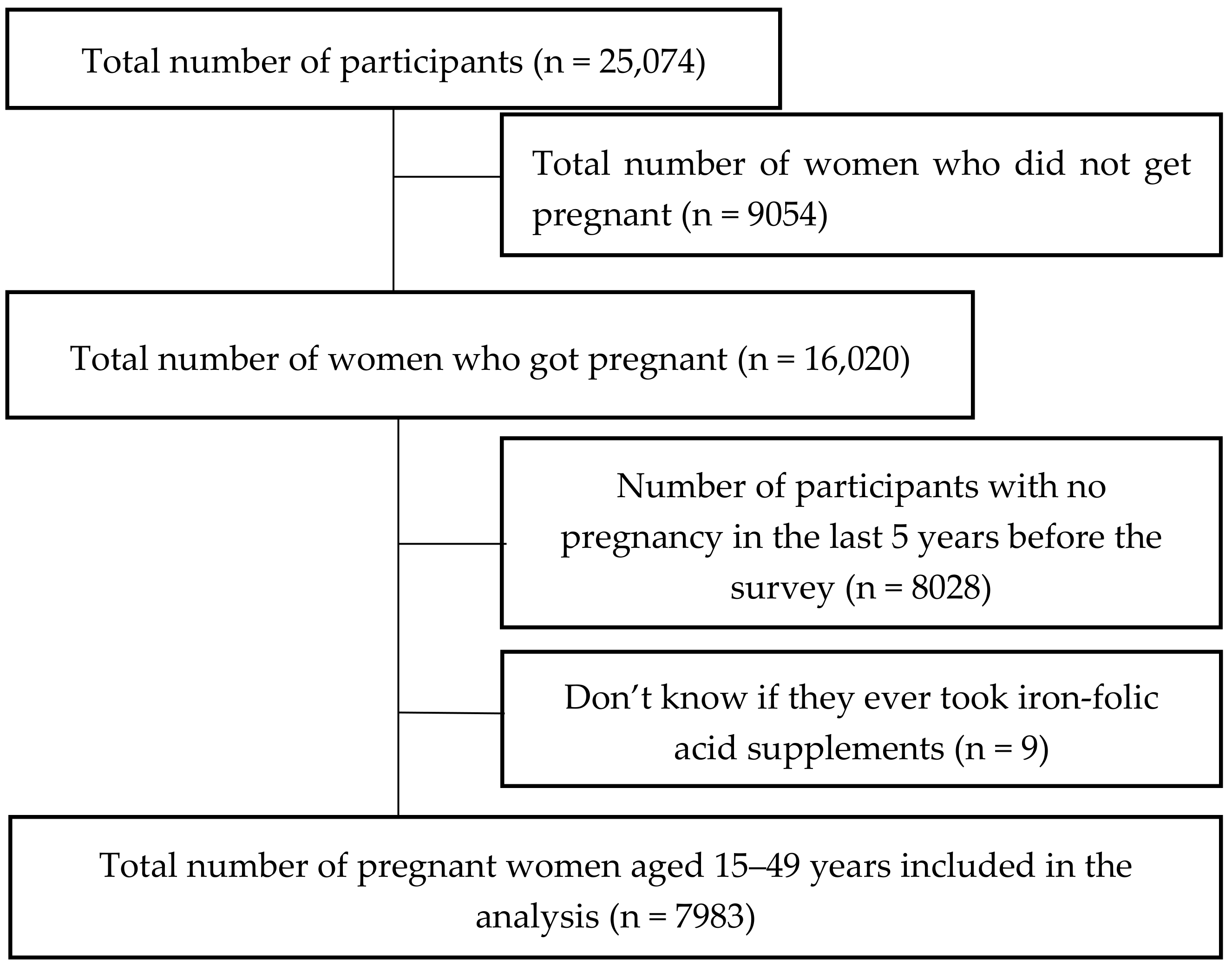
2.1. Data and Sample
2.2. Outcome Variable
2.3. Independent Variables
2.4. Data Analysis
3. Results
3.1. Characteristics of the Participants
3.2. Associations between the Characteristics of Participants and IFA Supplementation
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organization. The Global Prevalence of Anaemia in 2011; World Health Organization: Geneva, Switzerland, 2015. [Google Scholar]
- Molloy, A.M.; Kirke, P.N.; Brody, L.C.; Scott, J.M.; Mills, J.L. Effects of Folate and Vitamin B12 Deficiencies During Pregnancy on Fetal, Infant, and Child Development. Food Nutr. Bull. 2008, 29, S101–S111. [Google Scholar] [CrossRef] [PubMed]
- Philippine Department of Health. Administrative Order 2010-0010: Revised Policy on Micronutrient Supplementation to Support Achievement of 2015 MDG Targets to Reduce Underfive and Maternal Deaths and Address Micronutrient Needs of Other Population Groups. 2010. Available online: https://dmas.doh.gov.ph:8083/Search (accessed on 15 July 2021).
- Philippine Department of Health. Administrative Order No. 119 s. 2003: Updated Guidelines on Micronutrient Supplementation (Vitamin A, Iron, and Iodine). 2 December 2003. Available online: https://dmas.doh.gov.ph:8083/Search (accessed on 15 July 2021).
- Philippine Department of Health. The MNCHN Manual of Operations 2011, 2nd ed.; Philippine Department of Health: Manila, Philippines, 2011. [Google Scholar]
- World Bank. World Development Indicators. 30 July 2021. Available online: https://databank.worldbank.org/source/world-development-indicators/preview/on (accessed on 27 August 2021).
- World Health Organization. Iron Deficiency Anemia. Assessment, Prevention, and Control. In A Guide for Programme Managers; World Health Organization: Geneva, Switzerland, 2001. [Google Scholar]
- Fiedler, J.; D’Agostino, A.; Sununtnasuk, C. Nutrition Technical Brief: A Rapid Initial Assessment of the Distribution and Consumption of Iron–Folic Acid Tablets through Antenatal Care in the Phillippines. Spring Nutrition Technical Brief Series September 2014. Available online: https://www.spring-nutrition.org/publications/briefs/iron-folic-acid-assessment-philippines (accessed on 3 January 2021).
- Paulino, L.S.; Angeles-Agdeppa, I.; Etorma, U.M.M.; Ramos, A.C.; Cavalli-Sforza, T. Weekly iron-folic acid supplementation to improve iron status and prevent pregnancy anemia in Filipino women of reproductive age: The Philippine experience through government and private partnership. Nutr. Rev. 2005, 63, S109–S115. [Google Scholar] [CrossRef] [PubMed]
- Lutsey, P.L.; Dawe, D.; Villate, E.; Valencia, S.; Lopez, O. Iron supplementation compliance among pregnant women in Bicol, Philippines. Public Health Nutr. 2008, 11, 76–82. [Google Scholar] [CrossRef] [PubMed]
- Philippine Statistics Authority (PSA); ICF. Philippines National Demographic and Health Survey 2017; PSA: Quezon City, Philippines; ICF: Rockville, MD, USA, 2018. [Google Scholar]
- Reyes, C.M.; Mina, C.D.; Asis, R.D. Inequality of opportunities among ethnic groups in the Philippines. PIDS Discuss. Pap. Ser. 2017. [Google Scholar] [CrossRef]
- Tarekegn, M.; Wubshet, M.; Atenafu, A.; Derso, T.; Woretaw, A. Antenatal care and mothers’ education improved iron-folic acid adherence at Denbiya district health centers, Northwest Ethiopia: Using pills count method. Arch. Public Health 2019, 77, 30. [Google Scholar] [CrossRef] [PubMed]
- Agegnehu, G.; Atenafu, A.; Dagne, H.; Dagnew, B. Adherence to Iron and Folic Acid Supplement and Its Associated Factors among Antenatal Care Attendant Mothers in Lay Armachiho Health Centers, Northwest, Ethiopia, 2017. Int. J. Reprod. Med. 2019, 2019, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Titilayo, A.; Palamuleni, M.E.; Omisakin, O. Sociodemographic factors influencing adherence to antenatal iron supplementation recommendations among pregnant women in Malawi: Analysis of data from the 2010 Malawi Demographic and Health Survey. Malawi Med J. 2016, 28, 1–5. [Google Scholar] [CrossRef] [PubMed]
- Taye, B.; Abeje, G.; Mekonen, A. Factors associated with compliance of prenatal iron folate supplementation among women in Mecha district, Western Amhara: A cross-sectional study. Pan Afr. Med. J. 2015, 20, 43. [Google Scholar] [CrossRef] [PubMed]
- Mainuddin, A.; Begum, H.A.; Rawal, L.B.; Islam, A.; Islam, S.M.S. Women Empowerment and Its Relation with Health Seeking Behavior in Bangladesh. J. Fam. Reprod. Health 2015, 9, 65–73. [Google Scholar]
- Chourasia, A.; Pandey, C.M.; Awasthi, A. Factors influencing the consumption of iron and folic acid supplementations in high focus states of India. Clin. Epidemiol. Glob. Health 2017, 5, 180–184. [Google Scholar] [CrossRef]
- Urgessa, B.T.; Abdo, Z.A. Adherence to iron/folic acid supplementation and associated factors among pregnant women attending governmental health center in Yeka Sub City, Addis Ababa, Ethiopia. BLDE Univ. J. Health Sci. 2020, 5, 145. [Google Scholar] [CrossRef]
- Hahn, R.A.; Truman, B.I. Education Improves Public Health and Promotes Health Equity. Int. J. Health Serv. 2015, 45, 657–678. [Google Scholar] [CrossRef] [PubMed]
- Philippine Department of Health. What Are the Deployment Programs? Available online: https://doh.gov.ph/faqs/What-are-the-deployment-programs (accessed on 15 July 2021).
- An act for supporting scaling up nutrition during the first 1000 days of life by strengthening and protecting primary health care workers, in House Bill 3564. 2016.
- World Health Organization. Hidden Cities: Unmasking and Overcoming Health Inequities in Urban Settings. 14 September 2010. Available online: https://www.who.int/publications/i/item/9789241548038 (accessed on 15 July 2021).
- Desta, M.; Kassie, B.; Chanie, H.; Mulugeta, H.; Yirga, T.; Temesgen, H.; Leshargie, C.T.; Merkeb, Y. Adherence of iron and folic acid supplementation and determinants among pregnant women in Ethiopia: A systematic review and meta-analysis. Reprod. Health 2019, 16, 182. [Google Scholar] [CrossRef] [PubMed]
- Gebremichael, T.G.; Haftu, H.; Gereziher, T.A. Time to start and adherence to iron-folate supplement for pregnant women in antenatal care follow up; Northern Ethiopia. Patient Prefer. Adherence 2019, 13, 1057–1063. [Google Scholar] [CrossRef]
- Khanal, V.; Adhikari, M.; Karkee, R. Low Compliance with Iron-Folate Supplementation among Postpartum Mothers of Nepal: An Analysis of Nepal Demographic and Health Survey 2011. J. Community Health 2013, 39, 606–613. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Lyoba, W.; Mwakatoga, J.D.; Festo, C.; Mrema, J.; Elisaria, E. Adherence to Iron-Folic Acid Supplementation and Associated Factors among Pregnant Women in Kasulu Communities in North-Western Tanzania. Int. J. Reprod. Med. 2020, 2020, 3127245. [Google Scholar] [CrossRef]
- Nasir, B.B.; Fentie, A.M.; Adisu, M.K. Adherence to iron and folic acid supplementation and prevalence of anemia among pregnant women attending antenatal care clinic at Tikur Anbessa Specialized Hospital, Ethiopia. PLoS ONE 2020, 15, e0232625. [Google Scholar] [CrossRef]
- Mekonnen, B.A.; Dessie, Y.; Baraki, N.; Oumer, A.; Gebru, M. Adherence to iron and folic acid supplementation and associated factors among antenatal care attendants in Northwest Ethiopia. Int. J. Public Health Sci. 2020, 9, 20–28. [Google Scholar] [CrossRef]
| Variable/Categories | Total (N = 7983) | Non-Compliant Group (N = 5927) | Compliant Group (N = 2056) | p-Value |
|---|---|---|---|---|
| n (%) | n (%) | n (%) | ||
| Age (years) | <0.0001 | |||
| 15–24 | 1957 (24.5) | 1530 (78.2) | 427 (21.8) | |
| 25–34 | 3804 (47.7) | 2741 (72.1) | 1063 (27.9) | |
| 35–49 | 2222 (27.8) | 1656 (74.5) | 566 (25.5) | |
| Highest education attained | <0.0001 | |||
| Primary or below | 1634 (20.5) | 1378 (84.3) | 256 (15.7) | |
| Secondary | 3942 (49.4) | 2996 (76.0) | 946 (24.0) | |
| Higher | 2407 (30.1) | 1553 (64.5) | 854 (35.5) | |
| Occupation | <0.0001 | |||
| Not working | 4098 (51.3) | 3132 (76.4) | 966 (23.6) | |
| Working | 3885 (48.7) | 2795 (71.9) | 1090 (28.1) | |
| Wealth Index | <0.0001 | |||
| Poor | 4554 (57.0) | 3591 (78.9) | 963 (21.1) | |
| Middle | 1443 (18.1) | 1091 (75.6) | 352 (24.4) | |
| Rich | 1986 (24.9) | 1245 (62.7) | 741 (37.3) | |
| Ethnicity | <0.0001 | |||
| Non-Indigenous non-Muslim | 5436 (68.1) | 3941 (72.5) | 1495 (27.5) | |
| Non-Indigenous Muslim | 414 (5.2) | 392 (94.7) | 22 (5.3) | |
| Others | 2133 (26.7) | 1594 (74.7) | 539 (25.3) | |
| Religion | <0.0001 | |||
| Christianity | 7031 (88.1) | 5061 (72.0) | 1970 (28.0) | |
| Islam | 788 (9.9) | 735 (93.3) | 53 (6.7) | |
| Others or none | 164 (2.0) | 131 (79.9) | 33 (20.1) | |
| Residence | 0.534 | |||
| Urban | 2600 (32.6) | 1919 (73.8) | 681 (26.2) | |
| Rural | 5383 (67.4) | 4008 (74.5) | 1375 (25.5) | |
| Number of pregnancies | <0.0001 | |||
| 1 | 1992 (25.0) | 1422 (71.4) | 570 (28.6) | |
| 2 | 1992 (25.0) | 1441 (72.3) | 551 (27.7) | |
| 3 | 1504 (18.8) | 1111 (73.9) | 393 (26.1) | |
| ≥4 | 2495 (31.2) | 1953 (78.3) | 542 (21.7) | |
| Timing of first ANC visit | <0.0001 | |||
| Don’t know | 317 (4.0) | 306 (96.5) | 11 (3.5) | |
| First trimester | 5290 (66.3) | 3497 (66.1) | 1793 (33.9) | |
| Second or third trimester | 2376 (29.8) | 2124 (89.4) | 252 (10.6) | |
| Number of ANC visits | <0.0001 | |||
| <4 ANC visit | 1280 (16.0) | 1201 (93.8) | 79 (6.2) | |
| ≥4 ANC visits | 6703 (84.0) | 4726 (70.5) | 1977 (29.5) |
| Variables/Categories | COR (95% CI) | AOR (95% CI) |
| Age | ||
| 15–24 R | 1.00 | 1.00 |
| 25–34 | 1.39 (1.22–1.58) | 1.26 (1.08–1.46) ** |
| 35–49 | 1.22 (1.06–1.41) | 1.20 (0.99–1.44) |
| Highest education attained | ||
| Primary or below R | 1.00 | 1.00 |
| Secondary | 1.70 (1.46–1.98) | 1.26 (1.07–1.49) ** |
| Higher | 2.96 (2.53–3.46) | 1.72 (1.42–2.09) *** |
| Occupation | ||
| Not working R | 1.00 | 1.00 |
| Working | 1.26 (1.14–1.40) | 0.99 (0.88–1.10) |
| Wealth Index | ||
| Poor R | 1.00 | 1.00 |
| Middle | 1.20 (1.05–1.38) | 0.94 (0.81–1.10) |
| Rich | 2.22 (1.98–2.49) | 1.40 (1.21–1.63) *** |
| Ethnicity | ||
| Non-Indigenous non-Muslim | 1.12 (1.00–1.26) | 0.85 (0.75–0.97) * |
| Non-Indigenous Muslim | 0.17 (0.11–0.26) | 0.55 (0.31–0.95) * |
| Others R | 1.00 | 1.00 |
| Religion | ||
| Christianity R | 1.00 | 1.00 |
| Islam | 0.19 (0.14–0.25) | 0.36 (0.25–0.52) *** |
| Others or none | 0.65 (0.44–0.95) | 0.78 (0.52–1.17) |
| Residence | ||
| Urban R | 1.00 | 1.00 |
| Rural | 0.98 (0.87–1.08) | 1.30 (1.15–1.46) *** |
| Number of pregnancies | ||
| 1 R | 1.00 | 1.00 |
| 2 | 0.95 (0.83–1.10) | 0.92 (0.79–1.07) |
| 3 | 0.88 (0.76–1.03) | 0.88 (0.74–1.05) |
| ≥4 | 0.69 (0.60–0.79) | 0.88 (0.74–1.06) |
| Timing of first ANC visit | ||
| Don’t know | 0.30 (0.16–0.56) | 1.02 (0.53–1.98) |
| First trimester | 4.32 (3.75–4.98) | 3.30 (2.85–3.83) *** |
| Second or third trimester R | 1.00 | 1.00 |
| Number of ANC Visit | ||
| <4 ANC visit R | 1.00 | 1.00 |
| ≥4 ANC visits | 6.36 (5.03–8.03) | 2.71 (2.08–3.52) *** |
| Wealth Index | Non-Compliant Group | Compliant Group | AOR # | 95% CI |
|---|---|---|---|---|
| Poor, n = 4554 | ||||
| Urban R | 716 (83.4) | 142 (16.6) | 1.00 | |
| Rural | 2875 (77.8) | 821 (22.2) | 1.56 * | 1.27–1.92 |
| Middle, n = 1443 | ||||
| Urban R | 487 (77.8) | 139 (22.2) | 1.00 | |
| Rural | 604 (73.9) | 213 (26.1) | 1.17 | 0.90–1.51 |
| Rich, n = 1986 | ||||
| Urban R | 716 (64.2) | 400 (35.8) | 1.00 | |
| Rural | 529 (60.8) | 341 (39.2) | 1.22 | 0.99–1.48 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Felipe-Dimog, E.B.; Yu, C.-H.; Ho, C.-H.; Liang, F.-W. Factors Influencing the Compliance of Pregnant Women with Iron and Folic Acid Supplementation in the Philippines: 2017 Philippine Demographic and Health Survey Analysis. Nutrients 2021, 13, 3060. https://doi.org/10.3390/nu13093060
Felipe-Dimog EB, Yu C-H, Ho C-H, Liang F-W. Factors Influencing the Compliance of Pregnant Women with Iron and Folic Acid Supplementation in the Philippines: 2017 Philippine Demographic and Health Survey Analysis. Nutrients. 2021; 13(9):3060. https://doi.org/10.3390/nu13093060
Chicago/Turabian StyleFelipe-Dimog, Eva Belingon, Chia-Hung Yu, Chung-Han Ho, and Fu-Wen Liang. 2021. "Factors Influencing the Compliance of Pregnant Women with Iron and Folic Acid Supplementation in the Philippines: 2017 Philippine Demographic and Health Survey Analysis" Nutrients 13, no. 9: 3060. https://doi.org/10.3390/nu13093060
APA StyleFelipe-Dimog, E. B., Yu, C.-H., Ho, C.-H., & Liang, F.-W. (2021). Factors Influencing the Compliance of Pregnant Women with Iron and Folic Acid Supplementation in the Philippines: 2017 Philippine Demographic and Health Survey Analysis. Nutrients, 13(9), 3060. https://doi.org/10.3390/nu13093060






