Heart Rate Variability and Long Chain n-3 Polyunsaturated Fatty Acids in Chronic Kidney Disease Patients on Haemodialysis: A Cross-Sectional Pilot Study
Abstract
:1. Introduction
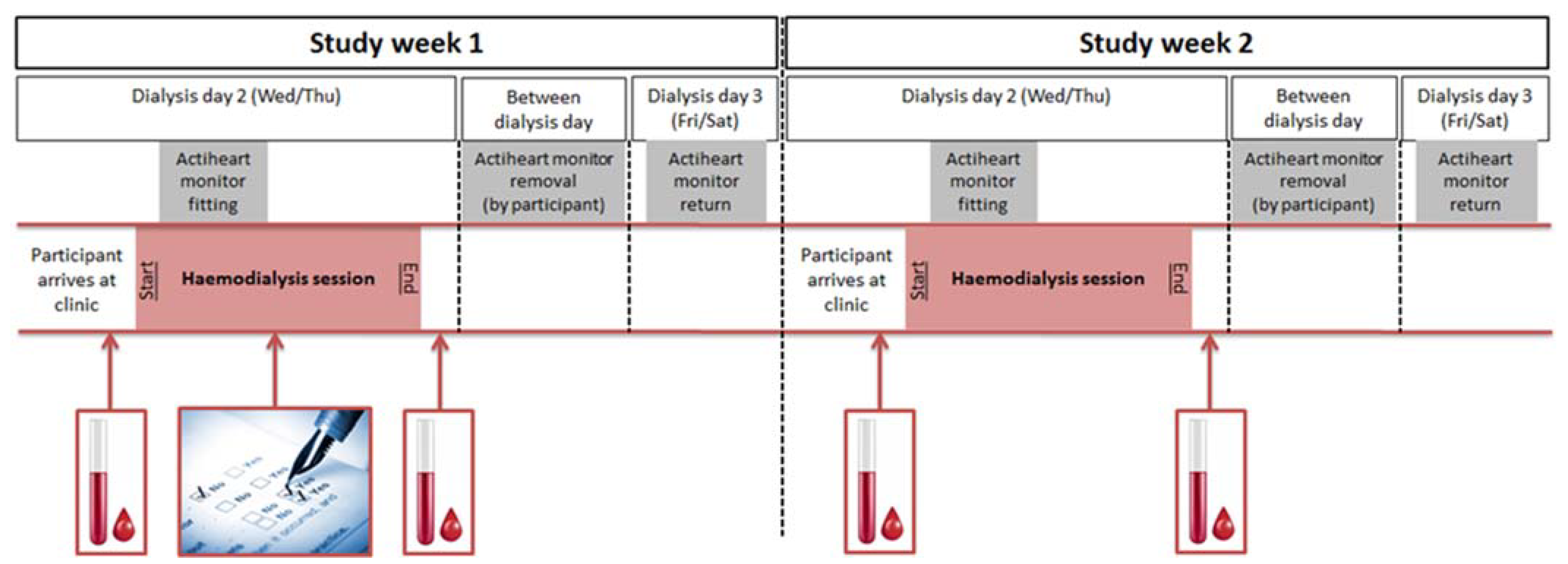
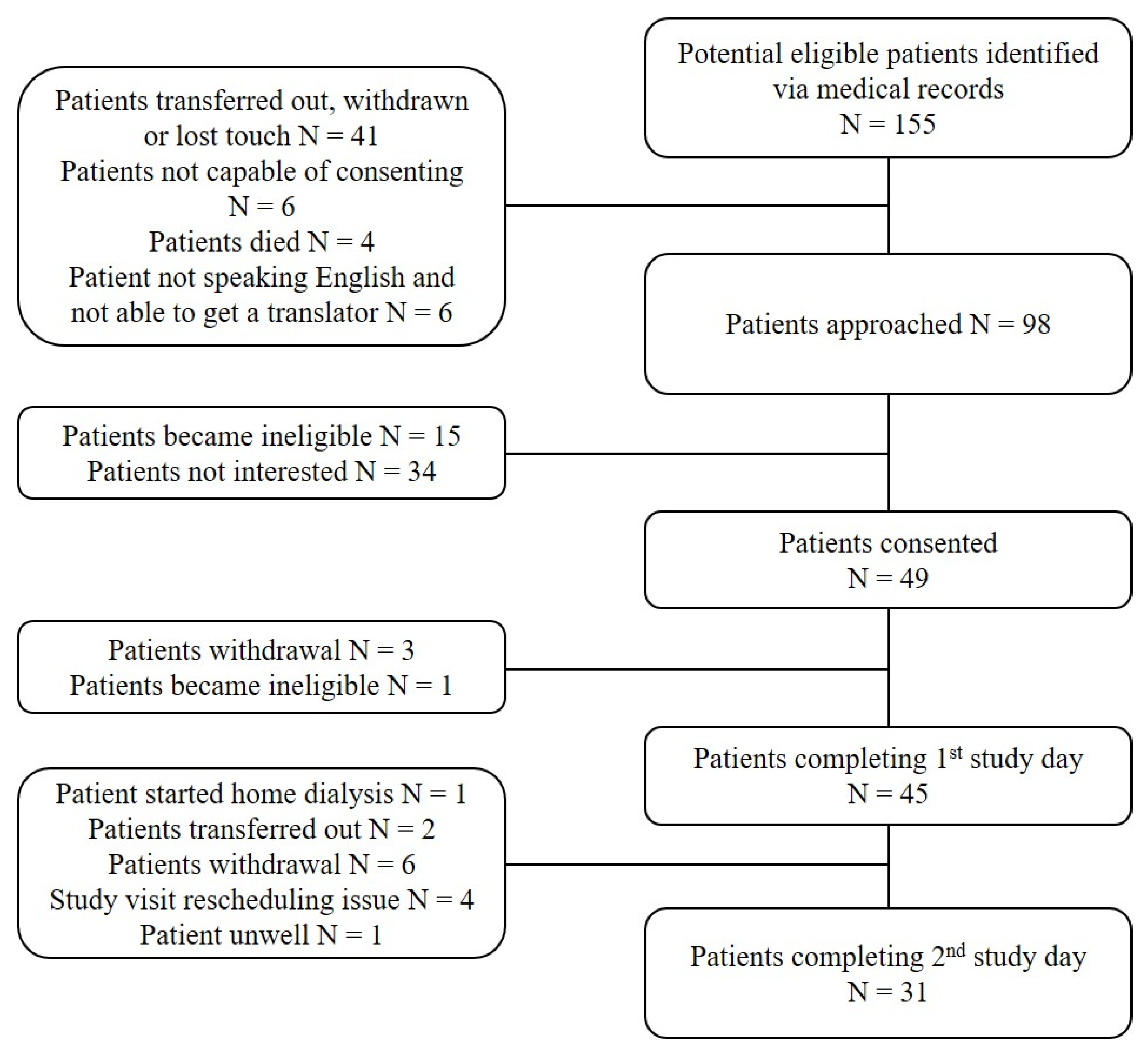
2. Materials and Methods
3. Results
3.1. Patient Characteristics
3.2. LC n-3 PUFA and 2 h Dialysis, Sleep-Time and 24 h HRV
3.3. LC n-3 PUFA and HRV in Haemodialysis vs. Reference Healthy Population
3.4. Associations between LC n-3 PUFA and HRV in Haemodialysis Patients
3.4.1. Erythrocyte Membrane LC n-3 PUFA
3.4.2. Plasma LC n-3 PUFA
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
Appendix B
| 24 h HRV Parameters | Mean | SD |
|---|---|---|
| HR (bpm) | 83.0 | 10.9 |
| IBI (ms) | 747 | 131 |
| Ti | ||
| Median | 16.8 | |
| Lower and upper quartiles | 15.0, 27.1 | |
| SDNN (ms) | 84.1 | 25.6 |
| SDANN (ms) | 76.2 | 25.6 |
| pNN50 (%) | 4.8 | 4.0 |
| RMSSD (ms) | 29.0 | 11.7 |
| LF (ms2) | ||
| Median | 92.7 | |
| Lower and upper quartiles | 40.7, 194.5 | |
| HF (ms2) | ||
| Median | 128.7 | |
| Lower and upper quartiles | 68.4, 216.8 | |
| LF:HF | ||
| Median | 0.79 | |
| Lower and upper quartiles | 0.57, 1.45 | |
| LogLF:HF | −0.22 | 0.79 |
| VLF (ms2) | 4844 | 3218 |
| SD1:SD2 | ||
| Median | 0.15 | |
| Lower and upper quartiles | 0.12, 0.24 |
References
- Foley, R.N.; Murray, A.M.; Li, S.; Herzog, C.A.; McBean, A.M.; Eggers, P.W.; Collins, A.J. Chronic Kidney Disease and the Risk for Cardiovascular Disease, Renal Replacement, and Death in the United States Medicare Population, 1998 to 1999. J. Am. Soc. Nephrol. 2004, 16, 489–495. [Google Scholar] [CrossRef]
- Herzog, C.A.; Mangrum, J.M.; Passman, R. Non-coronary heart disease in dialysis patients: Sudden cardiac death and dialysis patients. Semin. Dial. 2008, 21, 300–307. [Google Scholar] [CrossRef]
- Myerburg, R.J.; Junttila, M.J. Sudden Cardiac Death Caused by Coronary Heart Disease. Circulation 2012, 125, 1043–1052. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pun, P.H.; Smarz, T.R.; Honeycutt, E.F.; Shaw, L.K.; Al-Khatib, S.M.; Middleton, J.P. Chronic kidney disease is associated with increased risk of sudden cardiac death among patients with coronary artery disease. Kidney Int. 2009, 76, 652–658. [Google Scholar] [CrossRef] [Green Version]
- Ranpuria, R.; Hall, M.; Chan, C.T.; Unruh, M. Heart rate variability (HRV) in kidney failure: Measurement and consequences of reduced HRV. Nephrol. Dial. Transplant. 2008, 23, 444–449. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fukuta, H.; Hayano, J.; Ishihara, S.; Sakata, S.; Mukai, S.; Ohte, N.; Ojika, K.; Yagi, K.; Matsumoto, H.; Sohmiya, S.; et al. Prognostic value of heart rate variability in patients with end-stage renal disease on chronic haemodialysis. Nephrol. Dial. Transplant. 2003, 18, 318–325. [Google Scholar] [CrossRef]
- Hayano, J. Prognostic value of heart rate variability during long-term follow-up in chronic haemodialysis patients with end-stage renal disease. Nephrol. Dial. Transplant. 1999, 14, 1480–1488. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Oikawa, K.; Ishihara, R.; Maeda, T.; Yamaguchi, K.; Koike, A.; Kawaguchi, H.; Tabata, Y.; Murotani, N.; Itoh, H. Prognostic value of heart rate variability in patients with renal failure on hemodialysis. Int. J. Cardiol. 2009, 131, 370–377. [Google Scholar] [CrossRef]
- Madsen, T.; Christensen, J.H.; Svensson, M. Marine n-3 Polyunsaturated Fatty Acids in Patients With End-stage Renal Failure and in Subjects Without Kidney Disease: A Compararative Study. J. Ren. Nutr. 2011, 21, 169–175. [Google Scholar] [CrossRef]
- Shoji, T.; Kakiya, R.; Hayashi, T.; Tsujimoto, Y.; Sonoda, M.; Shima, H.; Mori, K.; Fukumoto, S.; Tahara, H.; Shioi, A.; et al. Serum n-3 and n-6 Polyunsaturated Fatty Acid Profile as an Independent Predictor of Cardiovascular Events in Hemodialysis Patients. Am. J. Kidney Dis. 2013, 62, 568–576. [Google Scholar] [CrossRef] [PubMed]
- Kutner, N.G.; Clow, P.W.; Zhang, R.; Aviles, X. Association of fish intake and survival in a cohort of incident dialysis patients. Am. J. Kidney Dis. 2002, 39, 1018–1024. [Google Scholar] [CrossRef] [PubMed]
- Friedman, A.N.; Saha, C.; Watkins, B.A. Feasibility Study of Erythrocyte Long-Chain Omega-3 Polyunsaturated Fatty Acid Content and Mortality Risk in Hemodialysis Patients. J. Ren. Nutr. 2008, 18, 509–512. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Calder, P.C. Marine omega-3 fatty acids and inflammatory processes: Effects, mechanisms and clinical relevance. Biochim. Biophys. Acta Mol. Cell Biol. Lipids 2015, 1851, 469–484. [Google Scholar] [CrossRef]
- Billman, G.E. The effects of omega-3 polyunsaturated fatty acids on cardiac rhythm: A critical reassessment. Parmacology Ther. 2013, 140, 53–80. [Google Scholar] [CrossRef] [PubMed]
- Giordano, E.; Visioli, F. Long-chain omega 3 fatty acids: Molecular bases of potential antioxidant actions. Prostaglandins Leukot. Essent. Fat. Acids 2014, 90, 1–4. [Google Scholar] [CrossRef]
- Christensen, J.H. Omega-3 Polyunsaturated Fatty Acids and Heart Rate Variability. Front. Physiol. 2011, 2, 84. [Google Scholar] [CrossRef] [Green Version]
- Christensen, J.H.; Aarøe, J.; Knudsen, N.; Dideriksen, K.; Kornerup, H.J.; Dyerberg, J.; Schmidt, E.B. Heart rate variability and n-3 fatty acids in patients with chronic renal failure-a pilot study. Clin. Nephrol. 1998, 49, 102–106. [Google Scholar]
- Svensson, M.; Schmidt, E.B.; Jørgensen, K.A.; Christensen, J.H. The effect of n-3 fatty acids on heart rate variability in patients treated with chronic hemodialysis. J. Ren. Nutr. 2007, 17, 243–249. [Google Scholar] [CrossRef]
- Malik, M.; Bigger, J.T.; Camm, A.J.; Kleiger, R.E.; Malliani, A.; Moss, A.J.; Schwartz, P.J. Heart rate variability: Standards of measurement, physiological interpretation and clinical use. Task Force of the European Society of Cardiology and the North American Society of Pacing and Electrophysiology. Eur. Heart J. 1996, 17, 354–381. [Google Scholar] [CrossRef] [Green Version]
- Lepage, G.; Roy, C.C. Direct transesterification of all classes of lipids in a one-step reaction. J. Lipid Res. 1986, 27, 114–120. [Google Scholar] [CrossRef]
- Hall, W.L.; Hay, G.; Maniou, Z.; Seed, P.T.; Chowienczyk, P.; Sanders, T. Effect of low doses of long chain n-3 polyunsaturated fatty acids on sleep-time heart rate variability: A randomized, controlled trial. Int. J. Cardiol. 2013, 168, 4439–4442. [Google Scholar] [CrossRef] [Green Version]
- Saran, R.; Li, Y.; Robinson, B.; Ayanian, J.; Balkrishnan, R.; Bragg-Gresham, J.; Chen, J.T.; Cope, E.; Gipson, D.; He, K.; et al. US Renal Data System 2014 Annual Data Report: Epidemiology of Kidney Disease in the United States. Am. J. Kidney Dis. 2015, 66, A7-305. [Google Scholar] [CrossRef] [Green Version]
- Timofte, D.; Tanasescu, M.-D.; Balan, D.G.; Tulin, A.; Stiru, O.; Vacaroiu, I.A.; Mihai, A.; Constantin, P.C.; Cosconel, C.-I.; Enyedi, M.; et al. Management of acute intradialytic cardiovascular complications: Updated overview (Review). Exp. Ther. Med. 2021, 21, 1. [Google Scholar] [CrossRef] [PubMed]
- Dessì, M.; Noce, A.; Bertucci, P.; Noce, G.; Rizza, S.; De Stefano, A.; di Villahermosa, S.M.; Bernardini, S.; de Lorenzo, A.; di Daniele, N. Plasma and erythrocyte membrane phospholipids and fatty acids in Italian general population and hemodialysis patients. Lipids Health Dis. 2014, 21, 13–54. [Google Scholar] [CrossRef] [Green Version]
- Friedman, A.N.; Yu, Z.; Tabbey, R.; Denski, C.; Tamez, H.; Wenger, J.; Thadhani, R.; Li, Y.; Watkins, B.A. Low Blood Levels of Long-Chain n–3 Polyunsaturated Fatty Acids in US Hemodialysis Patients: Clinical Implications. Am. J. Nephrol. 2012, 36, 451–458. [Google Scholar] [CrossRef] [Green Version]
- Ristić, V.; Tepsić, V.; Ristić-Medié, D.; Perunicić, G.; Rasić, Z.; Postić, M.; Arsić, A.; Blazencić-Mladenović, V.; Ristić, G. Plasma and erythrocyte phospholipid fatty acids composition in Serbian hemodialyzed patients. Ren. Fail. 2006, 28, 211–216. [Google Scholar] [CrossRef] [PubMed]
- Peck, W.; Monsen, R. Effect of three sources of long-chain fatty acids on the plasma fatty acid profile, plasma prostaglandin concentrations, and pruritus symptoms in hemodialysis. Am. J. Clin. Nutr. 1996, 64, 210–214. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gollasch, B.; Dogan, I.; Rothe, M.; Gollasch, M.; Luft, F.C. Effects of hemodialysis on blood fatty acids. Physiol. Rep. 2020, 8, 1–14. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Friedman, A.N.; Moe, S.M.; Perkins, S.M.; Li, Y.; Watkins, B.A. Fish Consumption and Omega-3 Fatty Acid Status and Determinants in Long-Term Hemodialysis. Am. J. Kidney Dis. 2006, 47, 1064–1071. [Google Scholar] [CrossRef] [PubMed]
- Harris, W.S.; Sands, S.A.; Windsor, S.L.; Ali, H.A.; Stevens, T.L.; Magalski, A.; Porter, C.B.; Borkon, A.M. Omega-3 fatty acids in cardiac biopsies from heart transplantation patients: Correlation with erythrocytes and response to supplementation. Circulation 2004, 110, 1645–1649. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Harris, W.S.; von Schacky, C. The Omega-3 Index: A new risk factor for death from coronary heart disease? Prev. Med. 2004, 39, 212–220. [Google Scholar] [CrossRef]
- Babitt, J.L.; Lin, H.Y. Mechanisms of Anemia in CKD. J. Am. Soc. Nephrol. 2012, 23, 1631–1634. [Google Scholar] [CrossRef] [Green Version]
- Serra-Majem, L.; Nissensohn, M.; Øverby, N.C.; Fekete, K. Dietary methods and biomarkers of omega 3 fatty acids: A systematic review. Br. J. Nutr. 2012, 107 (Suppl. S2), S64–S76. [Google Scholar] [CrossRef] [Green Version]
- Rantanen, J.M.; Schmidt, E.B.; Riahi, S.; Lundbye-Christensen, S.; Christensen, J.H. Marine n-3 PUFA, heart rate variability and ventricular arrhythmias in patients on chronic dialysis: A cross-sectional study. Br. J. Nutr. 2018, 120, 317–325. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hall, W.L. The future for long chain n-3 PUFA in the prevention of coronary heart disease: Do we need to target non-fish-eaters? Proc. Nutr. Soc. 2017, 76, 408–418. [Google Scholar] [CrossRef]
- Steinberg, A.A.; Mars, R.L.; Goldman, D.S.; Percy, R.F. Effect of end-stage renal disease on decreased heart rate variability. Am. J. Cardiol. 1998, 82, 1156–1158. [Google Scholar] [CrossRef]
- Tamura, K.; Tsuji, H.; Nishiue, T.; Yajima, I.; Higashi, T.; Iwasaka, T. Determinants of heart rate variability in chronic hemodialysis patients. Am. J. Kidney Dis. 1998, 31, 602–606. [Google Scholar] [CrossRef]
- Mann, M.C.; Exner, D.V.; Hemmelgarn, B.R.; Hanley, D.A.; Turin, T.C.; MacRae, J.M.; Ahmed, S.B. The VITAH Trial—Vitamin D Supplementation and Cardiac Autonomic Tone in Patients with End-Stage Kidney Disease on Haemodialysis: A Blinded, Randomized Controlled Trial. Nutrients 2016, 8, 608. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Agarwal, A.; Anand, I.S.; Sakhuja, V.; Chugh, K.S. Effect of dialysis and renal transplantation on autonomic dysfunction in chronic renal failure. Kidney Int. 1991, 40, 489–495. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tong, Y.-Q.; Hou, H.-M. Alteration of Heart Rate Variability Parameters in Nondiabetic Hemodialysis Patients. Am. J. Nephrol. 2007, 27, 63–69. [Google Scholar] [CrossRef] [PubMed]
- Poulikakos, D.; Malik, M.; Banerjee, D. Sex-Dependent Association between Heart Rate Variability and Pulse Pressure in Haemodialysis Patients. Nephron Clin. Pr. 2014, 128, 361–366. [Google Scholar] [CrossRef]
- Coquet, I.; Mousson, C.; Rifle, G.; Laurent, G.; Moreau, D.; Cottin, Y.; Zeller, M.; Touzery, C.; Wolf, J.E. Influence of Ischemia on Heart-Rate Variability in Chronic Hemodialysis Patients. Ren. Fail. 2005, 27, 7–12. [Google Scholar] [CrossRef] [PubMed]
- Chan, C.T.; Levin, N.W.; Chertow, G.M.; Larive, B.; Schulman, G.; Kotanko, P. Determinants of cardiac autonomic dysfunction in ESRD. Clin. J. Am. Soc. Nephrol. 2010, 5, 1821–1827. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sandrone, G.; Mortara, A.; Torzillo, D.; La Rovere, M.T.; Malliani, A.; Lombardi, F. Effects of beta blockers (atenolol or metoprolol) on heart rate variability after acute myocardial infarction. Am. J. Cardiol. 1994, 74, 340–345. [Google Scholar] [CrossRef]
- Wennerblom, B.; Lurje, L.; Karlsson, T.; Tygesen, H.; Vahisalo, R.; Hjalmarson, A. Circadian variation of heart rate variability and the rate of autonomic change in the morning hours in healthy subjects and angina patients. Int. J. Cardiol. 2001, 79, 61–69. [Google Scholar] [CrossRef]
- Tory, K.; Horváth, E.; Süveges, Z.; Fekete, A.; Sallay, P.; Berta, K.; Szabó, T.; Szabó, A.J.; Tulassay, T.; Reusz, G.S. Effect of propranolol on heart rate variability in patients with end-stage renal disease: A crossover pilot trial. Clin. Nephrol. 2004, 61, 316–323. [Google Scholar] [CrossRef]
- Yong, K.; Dogra, G.; Boudville, N.C.; Lim, W.H. Increased Inflammatory Response in Association with the Initiation of Hemodialysis Compared with Peritoneal Dialysis in a Prospective Study of End-Stage Kidney Disease Patients. Perit. Dial. Int. 2018, 38, 18–23. [Google Scholar] [CrossRef] [PubMed]
- Bazeley, J.; Bieber, B.; Li, Y.; Morgenstern, H.; De Sequera, P.; Combe, C.; Yamamoto, H.; Gallagher, M.; Port, F.K.; Robinson, B.M. C-Reactive Protein and Prediction of 1-Year Mortality in Prevalent Hemodialysis Patients. Clin. J. Am. Soc. Nephrol. 2011, 6, 2452–2461. [Google Scholar] [CrossRef] [Green Version]
- Psychari, S.N.; Sinos, L.; Iatrou, C.; Liakos, G.; Apostolou, T.S. Relations of inflammatory markers to lipid levels and autonomic tone in patients with moderate and severe chronic kidney disease and in patients under maintenance hemodialysis. Clin. Nephrol. 2005, 64, 419–427. [Google Scholar] [CrossRef]
- Von Känel, R.; Carney, R.M.; Zhao, S.; Whooley, M.A. Heart rate variability and biomarkers of systemic inflammation in patients with stable coronary heart disease: Findings from the Heart and Soul Study. Clin. Res. Cardiol. 2011, 100, 241–247. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Danesh, J.; Wheeler, J.G.; Hirschfield, G.; Eda, S.; Eiriksdottir, G.; Rumley, A.; Lowe, G.D.; Pepys, M.B.; Gudnason, V. C-Reactive Protein and Other Circulating Markers of Inflammation in the Prediction of Coronary Heart Disease. N. Engl. J. Med. 2004, 350, 1387–1397. [Google Scholar] [CrossRef]
- Poppitt, S.D.; Kilmartin, P.; Butler, P.; Keogh, G.F. Assessment of erythrocyte phospholipid fatty acid composition as a biomarker for dietary MUFA, PUFA or saturated fatty acid intake in a controlled cross-over intervention trial. Lipids Health Dis. 2005, 4, 30. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zong, G.; Zhu, J.; Sun, L.; Ye, X.; Lu, L.; Jin, Q.; Zheng, H.; Yu, Z.; Zhu, Z.; Li, H.; et al. Associations of erythrocyte fatty acids in the de novo lipogenesis pathway with risk of metabolic syndrome in a cohort study of middle-aged and older Chinese. Am. J. Clin. Nutr. 2013, 98, 319–326. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lemaitre, R.N.; King, I.B.; Sotoodehnia, N.; Knopp, R.H.; Mozaffarian, D.; McKnight, B.; Rea, T.D.; Rice, K.; Friedlander, Y.; Lumley, T.S.; et al. Endogenous red blood cell membrane fatty acids and sudden cardiac arrest. Metabolism 2010, 59, 1029–1034. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Browning, L.M.; Walker, C.G.; Mander, A.P.; West, A.L.; Madden, J.; Gambell, J.M.; Young, S.; Wang, L.; Jebb, S.A.; Calder, P.C. Incorporation of eicosapentaenoic and docosahexaenoic acids into lipid pools when given as supplements providing doses equivalent to typical intakes of oily fish. Am. J. Clin. Nutr. 2012, 96, 748–758. [Google Scholar] [CrossRef] [PubMed] [Green Version]
| N | % | |
| Sex | ||
| Male | 25 | 56 |
| Female | 20 | 44 |
| Ethnicity | ||
| White | 20 | 44 |
| Black | 19 | 42 |
| Other | 6 | 13 |
| Co-morbidities | ||
| Hypertension | 40 | 91 |
| Coronary artery disease | 5 | 11 |
| Peripheral vascular disease | 2 | 5 |
| Heart failure | 3 | 7 |
| Cerebrovascular disease | 3 | 7 |
| Type 2 Diabetes | 17 | 39 |
| Hyperlipidaemia | 9 | 21 |
| Anaemia | 5 | 11 |
| Medications | ||
| ACE inhibitor | 11 | 25 |
| ARB | 10 | 23 |
| β-blocker | 20 | 46 |
| α-blocker | 12 | 27 |
| Diuretic | 10 | 23 |
| Statin | 21 | 48 |
| Insulin | 11 | 25 |
| Anti-diabetic | 6 | 14 |
| Anti-depressant | 6 | 14 |
| Vitamin D | 25 | 57 |
| Calcium-based phosphate binders | 18 | 41 |
| Iron injections | 21 | 48 |
| Erythropoietin therapy | 20 | 45 |
| Subjective daytime sleepiness | ||
| Normal | 23 | 74 |
| Mild | 5 | 16 |
| Moderate | 1 | 3 |
| Severe | 2 | 7 |
| Risk of sleep apnoea | ||
| High | 20 | 65 |
| Low | 11 | 35 |
| Mean | SD | |
| Age (years) | 58 | 9 |
| Waist Circumference (cm) | ||
| Male | 105.6 | 13.2 |
| Female | 97.1 | 19.4 |
| BMI (kg/m2) | 27.8 | 7.0 |
| Average SBP (mmHg) 1 | 141 | 16 |
| Average DBP (mmHg) 1 | 76 | 9 |
| Fluid removal (L) | 2.0 | 0.8 |
| Pre- and post-dialysis measurements | ||
| Pre-dialysis creatinine (μmol/L) | 585 | 192 |
| Post-dialysis creatinine (μmol/L) | 228 | 100 |
| Pre-dialysis albumin (g/L) | ||
| Median | 38 | |
| Lower and upper quartiles | 36, 40 | |
| Post-dialysis albumin (g/L) | ||
| Median | 40 | |
| Lower and upper quartiles | 37, 44 | |
| Pre-dialysis sodium (mmol/L) | ||
| Median | 139.3 | |
| Lower and upper quartiles | 137.6, 141.0 | |
| Post-dialysis sodium (mmol/L) | ||
| Median | 138.0 | |
| Lower and upper quartiles | 137.0, 139.0 | |
| Pre-dialysis calcium (mmol/L) | 2.17 | 0.15 |
| Post-dialysis calcium (mmol/L) | 2.25 | 0.19 |
| Pre-dialysis potassium (mmol/L) | ||
| Geometric Mean | 5.1 | |
| 95% CI | 4.9, 5.4 | |
| Post-dialysis potassium (mmol/L) | ||
| Geometric Mean | 3.8 | |
| 95% CI | 3.6, 3.9 | |
| Dialysis 2 h HR and HRV 2 | ||
| HR (bpm) | 77.2 | 15.0 |
| IBI (ms) | 787 | 132 |
| Ti | 11.1 | 3.6 |
| SDNN (ms) | 45.8 | 13.9 |
| pNN50 (%) | ||
| Median | 1.86 | |
| Lower and upper quartilesRMSSD (ms) | 0.68, 5.41 | |
| Median | 21.4 | |
| Lower and upper quartiles | 17.4, 36.5 | |
| LF (ms2) | ||
| Median | 101 | |
| Lower and upper quartiles | 46, 197 | |
| HF (ms2) | ||
| Median | 114 | |
| Lower and upper quartiles | 55, 195 | |
| logLF:HF | −0.02 | 0.43 |
| SD1:SD2 | ||
| Median | 0.24 | |
| Lower and upper quartiles | 0.18, 0.42 |
| Haemodialysis Patients (n = 42) | Healthy Reference (n = 42) | p-Value | |
|---|---|---|---|
| Sex (M:F) | 22:20 | 22:20 | |
| Age (y) | 57 ± 8 | 57 ± 8 | |
| Ethnicity (White:Black:Other) | 19:18:5 | 32:7:3 | 0.013 § |
| BMI (kg/m2) | 27.6 ± 7.0 | 26.1 ± 3.4 | 0.231 |
| hs-CRP (mg/L) a | 5.0 (3.3, 7.6) | 0.6 (0.4, 0.9) | <0.001 |
| EPA dietary intake (mg/day) | 0.09 (0.06, 0.14) | 0.10 (0.07, 0.13) | 0.732 |
| DHA dietary intake (mg/day) | 0.27 (0.16, 0.45) | 0.18 (0.13, 0.25) | 0.176 |
| Erythrocyte EPA (%) a | 0.6 (0.54, 0.77) | 1.2 (1.09, 1.35) | <0.001 |
| Erythrocyte DPA (%) a | 1.5 (1.37, 1.63) | 3.3 (3.1, 3.5) | <0.001 |
| Erythrocyte DHA (%) | 2.6 ± 0.94 | 6.6 ± 1.42 | <0.001 |
| Omega-3 index (%) | 3.4 ± 1.17 | 7.9 ± 1.67 | <0.001 |
| Erythrocyte DPAn-6 (%) a | 0.23 (0.17, 0.42) | 0.45 (0.38, 0.52) | <0.001 |
| Erythrocyte AA (%) | 9.9 ± 1.29 | 17.2 ± 1.73 | <0.001 |
| Erythrocyte DGLA (%) b | 1.10 (0.88, 1.23) | 1.81 (1.63, 2.07) | <0.001 |
| Erythrocyte LA (%) | 7.6 ± 1.28 | 11.1 ± 1.61 | <0.001 |
| Erythrocyte cis-VA (%) b | 1.41 (1.36, 1.72) | 1.23 (1.11, 1.38) | <0.001 |
| Erythrocyte OA (%) | 15.7 ± 1.7 | 14.9 ± 1.04 | <0.01 |
| Erythrocyte SA (%) | 23.1 ± 1.59 | 15.7 ± 1.71 | <0.001 |
| Erythrocyte POA (%) a | 0.42 (0.32, 0.53) | 0.27 (0.23, 0.32) | <0.005 |
| Erythrocyte PA (%) b | 30.4 (29.0, 31.9) | 20.0 (18.8, 20.7) | <0.001 |
| Erythrocyte EPA:DHA ratio b | 0.31 (0.22, 0.39) | 0.18 (0.16, 0.22) | <0.001 |
| Erythrocyte PA:LA ratio b | 4.00 (3.48, 4.47) | 1.80 (1.65, 1.95) | <0.001 |
| Erythrocyte AA:EPA ratio b | 14.0 (10.4, 19.3) | 14.2 (10.7, 17.5) | 0.741 |
| Plasma EPA (%) a | 0.8 (0.63, 0.91) | 1.0 (0.91, 1.18) | 0.007 |
| Plasma DPA (%) a | 0.44 (0.40, 0.47) | 0.64 (0.60, 0.68) | <0.001 |
| Plasma DHA (%) | 1.8 ± 0.65 | 2.4 ± 0.63 | <0.001 |
| HR and HRV parameters (Sleep time) | N = 40 | N = 40 | |
| HR (bpm) | 77.4 ± 12.1 | 64.6 ± 9.7 | <0.001 |
| IBI (ms) | 800 ± 133 | 962 ± 115 | <0.001 |
| Ti | 12.2 ± 3.8 | 22.6 ± 6.3 | <0.001 |
| SDNN (ms) | 53.1 ± 16.7 | 94.3 ± 25.9 | <0.001 |
| pNN50 (%) a | 2.6 (1.7, 4.1) | 6.2 (4.1, 9.5) | 0.006 |
| RMSSD (ms) a | 23.5 (19.9, 27.8) | 34.4 (29.4, 40.4) | 0.001 |
| LF (ms2) a | 104 (79, 137) | 655 (504, 852) | <0.001 |
| HF (ms2) a | 106 (76, 148) | 316 (231, 432) | <0.001 |
| logLF:HF | −0.01 ± 0.82 | 2.64 ± 1.91 | <0.001 |
| VLF (ms2) a | 1514 (1257, 1824) | 4932 (4132, 5888) | <0.001 |
| SD1:SD2 a | 0.24 (0.21, 0.29) | 0.20 (0.17, 0.23) | 0.073 |
| EPA (wt %) a | DHA (wt %) | Omega-3 Index | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| β1 | p1 | β2 | p2 | β1 | p1 | β2 | p2 | β1 | p1 | β2 | p2 | |
| Dialysis (n = 36) | ||||||||||||
| HR (bpm) | −0.379 | 0.017 | −0.253 | 0.051 | −0.251 | 0.123 | −0.134 | 0.298 | −0.344 | 0.032 | −0.198 | 0.124 |
| IBI (ms) | 0.190 | 0.248 | 0.880 | 0.563 | 0.187 | 0.253 | 0.153 | 0.302 | 0.230 | 0.160 | 0.170 | 0.255 |
| Ti | 0.165 | 0.316 | 0.047 | 0.759 | 0.231 | 0.157 | 0.280 | 0.056 | 0.263 | 0.106 | 0.279 | 0.060 |
| SDNN (ms) | 0.136 | 0.408 | 0.023 | 0.882 | 0.101 | 0.542 | 0.142 | 0.347 | 0.133 | 0.419 | 0.141 | 0.354 |
| pNN50 (%) a | 0.053 | 0.747 | 0.012 | 0.940 | 0.090 | 0.584 | 0.127 | 0.430 | 0.100 | 0.546 | 0.124 | 0.445 |
| RMSSD (ms) a | −0.099 | 0.549 | −0.143 | 0.393 | 0.042 | 0.799 | 0.088 | 0.592 | 0.011 | 0.949 | 0.043 | 0.794 |
| LF (ms2) a | 0.225 | 0.169 | 0.088 | 0.528 | 0.095 | 0.565 | 0.151 | 0.263 | 0.154 | 0.350 | 0.167 | 0.217 |
| HF (ms2) a | −0.001 | 0.994 | −0.074 | 0.627 | 0.129 | 0.433 | 0.195 | 0.186 | 0.120 | 0.466 | 0.164 | 0.271 |
| logLF:HF | 0.250 | 0.124 | 0.195 | 0.230 | −0.092 | 0.579 | −0.101 | 0.528 | −0.013 | 0.937 | −0.041 | 0.800 |
| SDANN (ms) | 0.114 | 0.489 | 0.046 | 0.791 | 0.143 | 0.387 | 0.162 | 0.339 | 0.166 | 0.313 | 0.166 | 0.329 |
| SD1:SD2 a | −0.201 | 0.220 | −0.179 | 0.305 | −0.029 | 0.863 | −0.002 | 0.993 | −0.085 | 0.608 | −0.052 | 0.766 |
| Sleep time (n = 39) | ||||||||||||
| HR (bpm) | −0.306 | 0.062 | −0.274 | 0.110 | −0.086 | 0.608 | −0.034 | 0.840 | −0.169 | 0.304 | −0.110 | 0.522 |
| IBI (ms) | 0.309 | 0.059 | 0.270 | 0.114 | 0.079 | 0.637 | 0.032 | 0.850 | 0.154 | 0.349 | 0.106 | 0.532 |
| Ti | 0.184 | 0.268 | 0.128 | 0.469 | −0.018 | 0.915 | −0.066 | 0.701 | 0.037 | 0.825 | −0.027 | 0.879 |
| SDNN (ms) | 0.220 | 0.185 | 0.156 | 0.378 | −0.035 | 0.836 | −0.066 | 0.703 | 0.032 | 0.850 | −0.018 | 0.916 |
| pNN50 (%) a | −0.043 | 0.798 | −0.135 | 0.429 | 0.180 | 0.280 | 0.162 | 0.341 | 0.114 | 0.496 | 0.033 | 0.846 |
| RMSSD (ms) a | −0.043 | 0.797 | −0.127 | 0.466 | 0.173 | 0.300 | 0.132 | 0.435 | 0.148 | 0.376 | 0.089 | 0.602 |
| LF (ms2) a | 0.156 | 0.349 | 0.018 | 0.909 | 0.164 | 0.327 | 0.157 | 0.309 | 0.197 | 0.235 | 0.153 | 0.323 |
| HF (ms2) a | 0.096 | 0.568 | −0.013 | 0.938 | 0.230 | 0.166 | 0.202 | 0.207 | 0.241 | 0.145 | 0.187 | 0.247 |
| logLF:HF | 0.055 | 0.743 | 0.022 | 0.902 | −0.099 | 0.556 | −0.073 | 0.674 | −0.076 | 0.652 | −0.063 | 0.719 |
| VLF (ms2) a | 0.268 | 0.104 | 0.194 | 0.266 | −0.101 | 0.548 | −0.137 | 0.421 | 0.018 | 0.913 | −0.035 | 0.844 |
| SDANN (ms) a | 0.145 | 0.377 | 0.203 | 0.221 | −0.127 | 0.446 | −0.161 | 0.361 | −0.059 | 0.725 | −0.099 | 0.580 |
| SD1:SD2 a | −0.200 | 0.229 | −0.239 | 0.177 | 0.214 | 0.197 | 0.193 | 0.267 | 0.141 | 0.399 | 0.115 | 0.515 |
| 24 h (n = 35) | ||||||||||||
| HR (bpm) | −0.255 | 0.145 | −0.152 | 0.451 | −0.216 | 0.220 | −0.146 | 0.430 | −0.279 | 0.110 | −0.200 | 0.308 |
| IBI (ms) | 0.315 | 0.069 | 0.213 | 0.282 | 0.217 | 0.217 | 0.148 | 0.414 | 0.297 | 0.088 | 0.219 | 0.256 |
| Ti a | 0.430 | 0.011 | 0.334 | 0.094 | −0.008 | 0.965 | −0.078 | 0.677 | 0.109 | 0.538 | 0.001 | 0.998 |
| SDNN (ms) | 0.392 | 0.022 | 0.210 | 0.289 | −0.035 | 0.842 | −0.173 | 0.342 | 0.073 | 0.684 | −0.136 | 0.484 |
| pNN50 (%) | −0.051 | 0.775 | −0.145 | 0.508 | 0.164 | 0.355 | 0.186 | 0.351 | 0.145 | 0.414 | 0.168 | 0.432 |
| RMSSD (ms) | −0.230 | 0.190 | −0.330 | 0.130 | 0.191 | 0.279 | 0.256 | 0.201 | 0.123 | 0.489 | 0.197 | 0.359 |
| LF (ms2) a | 0.173 | 0.329 | −0.175 | 0.296 | 0.265 | 0.130 | 0.221 | 0.145 | 0.304 | 0.081 | 0.198 | 0.222 |
| HF (ms2) a | −0.090 | 0.611 | −0.311 | 0.112 | 0.286 | 0.102 | 0.323 | 0.068 | 0.252 | 0.150 | 0.276 | 0.149 |
| logLF:HF | 0.300 | 0.085 | 0.127 | 0.503 | 0.033 | 0.851 | −0.047 | 0.786 | 0.114 | 0.521 | −0.019 | 0.918 |
| VLF (ms2) | 0.412 | 0.016 | 0.293 | 0.150 | −0.050 | 0.777 | −0.168 | 0.373 | 0.063 | 0.722 | −0.109 | 0.588 |
| SDANN (ms) | 0.395 | 0.021 | 0.239 | 0.239 | −0.067 | 0.707 | −0.211 | 0.255 | 0.043 | 0.810 | −0.171 | 0.390 |
| SD1:SD2 a | −0.349 | 0.043 | −0.310 | 0.146 | 0.196 | 0.267 | 0.316 | 0.102 | 0.095 | 0.594 | 0.269 | 0.197 |
| EPA a | DPA(n-3) a | DHA | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| β1 | p1 | β2 | p2 | β1 | p1 | β2 | p2 | β1 | p1 | β2 | p2 | |
| Dialysis (n = 39) | ||||||||||||
| HR (bpm) | −0.129 | 0.435 | −0.119 | 0.347 | 0.207 | 0.207 | 0.145 | 0.253 | −0.298 | 0.065 | −0.208 | 0.101 |
| IBI (ms) | 0.151 | 0.359 | 0.159 | 0.273 | −0.178 | 0.279 | −0.111 | 0.448 | 0.239 | 0.143 | 0.223 | 0.128 |
| Ti | 0.143 | 0.386 | 0.134 | 0.362 | −0.051 | 0.759 | −0.047 | 0.752 | 0.328 | 0.042 | 0.331 | 0.022 |
| SDNN (ms) | 0.123 | 0.454 | 0.118 | 0.422 | −0.100 | 0.546 | −0.087 | 0.558 | 0.252 | 0.122 | 0.258 | 0.081 |
| pNN50 (%) a | −0.067 | 0.686 | −0.052 | 0.743 | −0.159 | 0.334 | −0.118 | 0.459 | 0.056 | 0.737 | 0.092 | 0.567 |
| RMSSD (ms) | −0.196 | 0.231 | −0.184 | 0.249 | −0.279 | 0.085 | −0.253 | 0.112 | −0.023 | 0.892 | 0.015 | 0.925 |
| LF (ms2) a | 0.095 | 0.564 | 0.081 | 0.539 | −0.147 | 0.372 | −0.153 | 0.248 | 0.239 | 0.142 | 0.235 | 0.076 |
| HF (ms2) a | −0.086 | 0.602 | −0.073 | 0.617 | −0.221 | 0.176 | −0.185 | 0.202 | 0.120 | 0.468 | 0.168 | 0.254 |
| logLF:HF | 0.196 | 0.231 | 0.166 | 0.285 | 0.095 | 0.566 | 0.042 | 0.791 | 0.100 | 0.546 | 0.044 | 0.781 |
| SDANN (ms) | 0.182 | 0.266 | 0.177 | 0.282 | −0.013 | 0.939 | −0.007 | 0.965 | 0.270 | 0.096 | 0.270 | 0.105 |
| SD1:SD2 a | −0.308 | 0.057 | −0.291 | 0.076 | −0.231 | 0.158 | −0.211 | 0.209 | −0.202 | 0.218 | −0.163 | 0.337 |
| Sleep time (n = 40) | ||||||||||||
| HR (bpm) | −0.263 | 0.106 | −0.279 | 0.080 | 0.131 | 0.427 | 0.080 | 0.626 | −0.225 | 0.168 | −0.205 | 0.210 |
| IBI (ms) | 0.280 | 0.085 | 0.296 | 0.060 | −0.100 | 0.543 | −0.046 | 0.780 | 0.218 | 0.183 | 0.201 | 0.218 |
| Ti | 0.191 | 0.244 | 0.186 | 0.264 | −0.146 | 0.375 | −0.133 | 0.431 | 0.127 | 0.441 | 0.090 | 0.599 |
| SDNN (ms) | 0.254 | 0.119 | 0.246 | 0.137 | 0.040 | 0.808 | 0.052 | 0.758 | 0.046 | 0.781 | 0.006 | 0.970 |
| pNN50 (%) a | −0.180 | 0.274 | −0.174 | 0.272 | −0.362 | 0.024 | −0.321 | 0.041 | −0.113 | 0.495 | −0.164 | 0.309 |
| RMSSD (ms) | −0.183 | 0.264 | −0.176 | 0.277 | −0.331 | 0.040 | −0.290 | 0.071 | −0.116 | 0.482 | −0.153 | 0.353 |
| LF (ms2) a | 0.031 | 0.851 | 0.025 | 0.869 | −0.142 | 0.390 | −0.110 | 0.479 | 0.068 | 0.680 | 0.035 | 0.823 |
| HF (ms2) a | −0.048 | 0.773 | −0.042 | 0.789 | −0.222 | 0.174 | −0.173 | 0.268 | −0.015 | 0.929 | −0.047 | 0.765 |
| logLF:HF | 0.088 | 0.593 | 0.075 | 0.658 | 0.098 | 0.553 | 0.079 | 0.644 | 0.086 | 0.604 | 0.087 | 0.616 |
| VLF (ms2) a | 0.285 | 0.079 | 0.277 | 0.094 | 0.078 | 0.639 | 0.085 | 0.610 | 0.099 | 0.551 | 0.053 | 0.754 |
| SDANN (ms) a | 0.320 | 0.047 | 0.308 | 0.064 | 0.181 | 0.270 | 0.172 | 0.316 | 0.039 | 0.812 | 0.004 | 0.980 |
| SD1:SD2 a | −0.354 | 0.027 | −0.340 | 0.036 | −0.364 | 0.023 | −0.330 | 0.045 | −0.159 | 0.333 | −0.172 | 0.311 |
| 24 h (n = 35) | ||||||||||||
| HR (bpm) | −0.280 | 0.109 | −0.223 | 0.195 | 0.196 | 0.266 | 0.154 | 0.369 | −0.298 | 0.087 | −0.256 | 0.170 |
| IBI (ms) | 0.352 | 0.041 | 0.296 | 0.077 | −0.144 | 0.416 | −0.097 | 0.568 | 0.335 | 0.053 | 0.297 | 0.103 |
| Ti a | 0.347 | 0.044 | 0.281 | 0.112 | −0.222 | 0.206 | −0.211 | 0.221 | 0.282 | 0.107 | 0.221 | 0.244 |
| SDNN (ms) | 0.441 | 0.009 | 0.378 | 0.022 | −0.052 | 0.769 | −0.026 | 0.879 | 0.254 | 0.147 | 0.124 | 0.506 |
| pNN50 (%) | −0.302 | 0.083 | −0.331 | 0.073 | −0.394 | 0.021 | −0.376 | 0.038 | −0.075 | 0.675 | −0.097 | 0.636 |
| RMSSD (ms) | −0.337 | 0.052 | −0.353 | 0.057 | −0.387 | 0.024 | −0.386 | 0.034 | −0.120 | 0.498 | −0.117 | 0.573 |
| LF (ms2) a | 0.062 | 0.729 | −0.017 | 0.909 | −0.134 | 0.449 | −0.108 | 0.451 | 0.219 | 0.213 | 0.089 | 0.574 |
| HF (ms2) a | −0.211 | 0.232 | −0.259 | 0.125 | −0.343 | 0.047 | −0.310 | 0.061 | 0.031 | 0.863 | 0.003 | 0.986 |
| logLF:HF | 0.298 | 0.087 | 0.258 | 0.106 | 0.210 | 0.234 | 0.205 | 0.199 | 0.240 | 0.171 | 0.125 | 0.481 |
| SDANN (ms) | 0.464 | 0.006 | 0.405 | 0.016 | −0.016 | 0.929 | −0.010 | 0.954 | 0.247 | 0.159 | 0.121 | 0.525 |
| VLF (ms2) | 0.481 | 0.004 | 0.434 | 0.010 | −0.038 | 0.829 | −0.010 | 0.956 | 0.249 | 0.155 | 0.155 | 0.422 |
| SD1:SD2 a | −0.482 | 0.004 | −0.461 | 0.009 | −0.331 | 0.056 | −0.337 | 0.060 | −0.227 | 0.197 | −0.152 | 0.453 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pinto, A.M.; MacLaughlin, H.L.; Hall, W.L. Heart Rate Variability and Long Chain n-3 Polyunsaturated Fatty Acids in Chronic Kidney Disease Patients on Haemodialysis: A Cross-Sectional Pilot Study. Nutrients 2021, 13, 2453. https://doi.org/10.3390/nu13072453
Pinto AM, MacLaughlin HL, Hall WL. Heart Rate Variability and Long Chain n-3 Polyunsaturated Fatty Acids in Chronic Kidney Disease Patients on Haemodialysis: A Cross-Sectional Pilot Study. Nutrients. 2021; 13(7):2453. https://doi.org/10.3390/nu13072453
Chicago/Turabian StylePinto, Ana M, Helen L MacLaughlin, and Wendy L Hall. 2021. "Heart Rate Variability and Long Chain n-3 Polyunsaturated Fatty Acids in Chronic Kidney Disease Patients on Haemodialysis: A Cross-Sectional Pilot Study" Nutrients 13, no. 7: 2453. https://doi.org/10.3390/nu13072453
APA StylePinto, A. M., MacLaughlin, H. L., & Hall, W. L. (2021). Heart Rate Variability and Long Chain n-3 Polyunsaturated Fatty Acids in Chronic Kidney Disease Patients on Haemodialysis: A Cross-Sectional Pilot Study. Nutrients, 13(7), 2453. https://doi.org/10.3390/nu13072453






